Abstract
Background:
Yoga and Ayurveda texts emphasize the role of cleansing the bowel as an important component of management of hypertension (HTN). Observations during our clinical experience and pilot studies on Laghu shankha prakshalana kriya (LSP), a yogic bowel cleansing technique, appeared to be safe and complimentary.
Objective:
To test the safety and effectiveness of LSP in patients with essential hypertension.
Materials and Methods:
This self control study recruited 32 patients with mild to moderate essential HTN admitted for a week long residential integrated yoga therapy program at the integrative health home in Bengaluru. Patients had a daily routine of 6 hours of integrated approach of yoga therapy (IAYT) module for HTN that included physical postures, relaxation sessions, pranayama and meditations. LSP, an additional practice, that involved drinking of luke-warm water (with or without a herbal combination, triphala) followed by a set of specific yoga postures that activates defecation reflex, was administered on 2nd (LSP without triphala) and 5th day (LSP with triphala). Assessments (sitting blood pressure and pulse rate) were done just before and after both the sessions of LSP. Secondary outcome measures such as body mass index (BMI), symptom scores, medication scores, fatigue, state and trait anxiety, general health and quality of life were assessed on 1st and 6th day of IAYT intervention.
Results:
There was significant (P < 0.001, paired t test) reduction in blood pressure (systolic and diastolic) and pulse rate immediately after both the sessions (LSP with and without triphala). There were no adverse effects reported during or after LSP. There was no significant difference between the two techniques (P < 0.505, independent samples t test), although the percentage change appeared to be higher after triphala LSP session. The number of visits to clear the bowel during the procedure was significantly (P < 0.001, independent samples t test) higher after LSP with triphala than LSP without triphalā. After weeklong IAYT, there were significant reductions in blood pressure (P < 0.001), BMI (P < 0.004), medication score (P < 0.001), symptoms score (P < 0.001), fatigue (P < 0.001), state and trait anxiety (STAI, P < 0.001), scores of general ill health (GHQ, P < 0.001), and increase in comfort level (P < 0.001) and quality of sleep (P < 0.001).
Conclusion:
LSP (a part of IAYT) is a safe and useful procedure for patients with essential hypertension. LSP with triphala is more useful.
Keywords: Bowel cleansing, hypertension, laghu shankha prakshalana kriya, triphala, yoga
INTRODUCTION
Essential hypertension is a major health burden due to its lethal complications such as cerebral, cardiac and renal events.[1] According to WHO health statistics 2012, the prevalence of hypertension in India was 23.1% in men and 22.6% in women. It was considered directly responsible for 7.5 million deaths in 2004, about 12.8 percent of the total of all global deaths.[2]
Decline in the blood pressure is the best determinant of cardiovascular risk reduction and most hypertensive patients need two or more antihypertensive drugs for the blood-pressure control. Despite the availability of effective drugs, the progression of the disease and its complications remain uncontrolled in most patients.[1] The reason appears to be a lack of holistic approach in its management, as we know that life style and psychological stresses play a major role in the genesis of hypertension and heart disease.[3,4] Sullivan et al., showed that depression and anxiety are related to increased symptom severity and functional impairment in patients with hypertension and heart diseases.[5] Complementary therapies and healing practices have been found to reduce stress, anxiety and depression. Promising therapies amongst these include imagery and hypnosis, meditation, yoga, tai chi, prayer, music, exercise, diet and use of dietary supplements.[6] Yoga offers several practices that help in mastery over the modifications of the mind (chitta vritti nirodha)[7] through the process of calmness of mind (mana prashamana upaya)[8] to reach a state of balanced functioning of the mind-body complex (samatvam yoga uchyate).[9] Integrated approach of Yoga therapy (IAYT) involves selecting physiologically acceptable and useful practices that can be grouped under four domains (raja yoga, karma yoga, bhakti yoga and jnana yoga). Raja yoga includes physical postures (asanas), breathing practices (Pranayama), cleansing techniques (kriyas) and meditation (dharana, dhyana, samadhi); karma yoga refers to stress free activity through action in relaxation; bhakti yoga is emotional mastery through nurturing pure love; jnana yoga offers cognitive correction through right knowledge.[3] Studies have found that yoga interventions are effective in reducing body weight, blood pressure, glucose level and high cholesterol.[10] Yogic relaxation leads to a state of parasympathetic dominance that promotes cardiac vagal modulation which could be beneficial in conditions (hypertension) characterized by increased sympathetic activity.[11] Meditations and yogic relaxation techniques specifically have been found to be effective in reducing blood pressure in patients with essential hypertension and preventing its complications.[12,13] Yoga and Ayurveda, the Indian systems of medicine, lay emphasis on clearing the bowel as an essential component of therapy based on its disease model.[14,15] This model of hypertension, a life style disease (adhija vyadhi),[8] proposes that these diseases begin in the mind as persitent long standing emotional responses to stressful demanding situations of life (adhi = stress); these (uncontrolled rewinding thoughts) manifest as disturbed breathing and digestive functions (poor appetite and constipation) due to prana (chi or vital energy) imbalance. As time lapses, this habituated imbalance of prana percolates to the body level (annamaya kosha) causing biochemical imbalances that shows up as hypertension.[16] Hence, IAYT aims at correcting the imbalances at all levels (the mind, prana and body). Correction of imblances in breathing (pranayama) and bowel disturbance (purgation) are considered primary requisites. Shankhaprakhsālana is a yoga practice (kriya) recommended for cleansing the bowel.[17] Laghu shankha prakshālana (LSP) is a simplified version of this kriya that is completed in a shorter time and offers lesser physical strain. Ayurveda recommends a strictly monitored procedure for purgation called virechana. Studies have observed reduction in blood pressure (BP) after virechana in patients with essential hypertension.[14,15] Mild laxatives, such as triphala, whose safety is time tested and already established in number of previous studies[18,19] may also be used instead of virechana in the management of hypertension.[20,21,22,23] Considering the amount of water consumed and physical exertion involved, it is sometimes felt that LSP may not be safe for persons with hypertension as water intake may raise blood volume (and hence the cardiac output) and strenuous exercise may further increase the heart rate. Thus, both these factors may raise the blood pressure. Therefore we conducted a pilot study to assess the safety of LSP on 8 essential hypertension patients (5 males and 3 females) in the age range of 50 ± 8.1 years. The study was conducted under the supervision of medical professionals and blood pressure and pulse rate were measured before and after the practice of LSP. The assessments were done daily early morning, empty stomach, on respective patients. We found a reduction in the blood pressure as well as pulse rate after the practice of LSP.The present study was designed based on this observation with an aim to investigate the immediate effect of LSP on blood pressure and pulse rate in patients with essential hypertension. As triphala (combination of three fruits Phyllanthus emblica, Terminalia bellerica and Terminalia chebula) is known to have a mild laxative effect it was hypothesized that LSP done with a decoction of triphala may have complementary effect in hypertension.[24] Thus, this study had two objectives: (a) to study the safety of LSP and (b) to compare the effect of LSP with and without triphala.
MATERIALS AND METHODS
Patients
This study involved thirty two patients who were diagnosed with mild to moderate hypertension as per American Heart Association criteria. Patients were diagnosed to be suffering from essential hypertension by the physician based on initial history, physical, and laboratory evaluation after ruling out all the causes of secondary hypertension. The lab evaluations included kidney functions tests (blood urea nitrogen, creatinine, and the urinalysis), USG abdomen, complete blood count, serum potassium, sodium, fasting glucose, total cholesterol, high-density cholesterol, and electrocardiogram. Both male (n = 14) and female (n = 18) patients in the age range of 30-70 years were included. Patients were selected from those who had enrolled for a holistic yoga therapy plan at a residential yoga health home.
A sample size of 32 was derived by computing (G power software) the values for alpha (0.05), effect size (0.6) and power (0.8). The effect size was calculated by considering the mean and standard deviation of blood pressure before and after the yoga intervention in hypertension patients who were treated in the same inpatient setting in our pilot study.
The inclusion criteria were: (a) those diagnosed as primary/essential hypertension by excluding renal and other causes of secondary hypertension by the physician at the time of diagnosis (checked by going through the earlier records), (b) those with mild to moderate hypertension under control with antihypertensive medication, (c) those with co-morbid conditions such as obesity or diabetes, (d) no prior experience in yoga and (e) those who were willing to participate in the study. Those with severe HTN, complications in HTN or secondary hypertension were excluded from the study. Also, patients with complications of diabetes or other major associated diseases such as coronary artery disease, psychiatric illnesses were excluded. Those on Ayurveda medication for bowel clearance, those with severe obesity (BMI > 40), and those admitted to health home for < one week were also excluded.
The study was approved by the institutional ethics committee. All patients admitted for the IAYT program at the residential integrative medical unit had an orientation session on integrated yoga therapy and LSP after the clinical evaluation by the attending physicians (modern medical and Ayurveda) before the therapy started. Written informed consent was obtained from all subjects who satisfied the inclusion criteria and were willing to participate in the study.
Design
This was a self-as-control design with assessments after two sessions of practice in the same participant on the second and fifth day after admission. All patients (with chronic illnesses) arrived between 9 am to 12 pm on a Friday for the weeklong residential facility at the Arogyadhama. The patients from all parts of India registered for the course before they arrived on Friday. They were introduced to the program by their friends (word of mouth) or the media.
After arrival, patients were allotted to different departments for holistic treatment after the basic clinical work-up by the medical team. The patients who satisfied the inclusion criteria for the present study were selected, informed consent was obtained, and all assessments were documented on the same day. In the post-lunch session there was an interactive presentation for all participants to explain the schedule of the daily routine (5 am-9 pm) during the course of next six days and clarify any doubts. Immediately after this general session, the researcher in charge addressed the group who were recruited for the study and explained the nature of the study and the procedure of LSP.
All the recruited patients practiced LSP with normal water (NWLSP) on Saturday morning under close supervision. Thursday morning was the session of LSP with triphala water (TWLSP). Primary outcome measures were recorded by the researcher before and after both the sessions in the same room where the deep relaxation session (phase 2 of LSP) was conducted after returning from the active phase of LSP practice.
Assessments
Primary outcome measures
Primary outcome measures were Blood Pressure, Pulse rate, Respiratory rate and frequency of visits to toilet for defecation during LSP. Sitting blood pressure and pulse rate was recorded by using electronic portable cardiac monitor equipment (BPL Ltd., India). Respiratory rate was manually recorded by counting the number of breaths/minute by the researcher while the attention of the patient was diverted. Total number of visits to empty the bowel during the procedure was documented.
Secondary outcome measures
All these measures were documented on the 1st and 6th day of their residential program of intervention with IAYT.
The weight was recorded using a standard electronic weighing scale.
The height was assessed using a standard scale (Stadiometer).
Body mass index (BMI): BMI was calculated by the equation: BMI = weight (kgs)/[height (m)]2
Slow Exhalation Time: This was assessed by noting the time taken (in seconds) for chanting Bhramari (making a humming sound during exhalation) after deep inhalation. This bhramari time (BHT) was considered by us to be a simplified version of SVC (slow vital capacity) that can be used in a clinical setting. The chanting of long Bhrāmari helped in ensuring the accuracy of slow and complete exhalation. Also, taking the average of three attempts helped in noting the stability of the SVC.
Symptoms score
Symptoms score was calculated by using a symptoms checklist with a four point scale (nil, Mild - symptoms do not disturb the daily routine and may not require medication for relief, moderate - disturbs the routine and needs medication and severe - needs parenteral medication or hospitalization) recorded during the semi- structured clinical interview.
Medication score
All participants were on antihypertensive drugs at the time of their admission. Medication score refers to the number of anti-hypertensive tablets/day. The standard strength of the tablet as given in the Current Index of Medical Specialities (CIMS) was checked as one tablet e.g. Amlodipine 5 mg was considered as one tablet; if the patient was taking 2.5 mg/day, it was counted as 0.5, and if it was 10 mg, it was recorded as 2 tablets. The dosage was changed only when absolutely necessary by the attending physician.
Level of fatigue
The participants were asked to mark the degree of fatigue on an eleven point (1-10) numerical analogue scale of 10 centimeters with ‘0’ at the left extreme indicating ‘nil’ fatigue and ‘10’ at the right extreme representing ‘worst possible experience of fatigue’.
Level of comfort
The participants were asked to mark the degree of comfort on an eleven point (0-10) numerical analogue scale of 10 centimeters with ‘0’ at the left extreme indicating ‘nil’ comfort and ‘10’ at the right extreme representing ‘most comfortable’.
General health questionnaire
Goldberg's GHQ designed to identify psychiatric morbidity in general practice, is a self-administered questionnaire. It has 28 items with four domains to measure somatic symptoms, anxiety and insomnia, social dysfunction and severe depression. It provides information about the recent mental status, thus distinguishing the presence of possible psychiatric disturbance. GHQ has acceptable psychometric properties and has good internal consistency and reliability with Cronbach's alpha of 0.85 and validity of 0.76 (39).
STAI inventory (State trait anxiety inventory)
STAI is a commonly used psychological inventory based on a 4-point Likert scale and consists of 40 questions on a self-report basis. STAI measures two types of anxiety i.e. state anxiety that refers to ‘how I feel now’ and trait anxiety that refers ‘how I generally feel’. Higher scores are positively correlated with higher levels of anxiety. STAI is a highly reliable test with a Chronbach's alpha of 0.6996 and validity value of 0.8027.
Quality of sleep
A checklist containing the following questions was prepared for the participants to mark their quality of sleep on the previous night on the 2nd and 6th day of their program. These were: (a) Time taken to fall asleep: measured in minutes, (b) Total duration of sleep: measured by an analogue scale, (c) Feeling of freshness on waking up: measured by an analogue scale and (d) the number of interruptions as reported by the patient on the next day.
Intervention
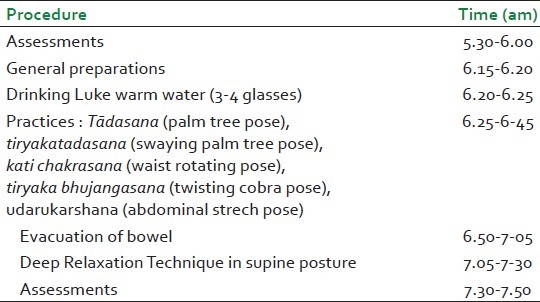
Integrated Approach of yoga Therapy (IAYT) module for Hypertension [Table 2] that has evolved over the past 20 years (by daily BP monitoring and also feedback from the patients and the teaching therapists) during our clinical experience at the center, was followed.[16] The daily routine included about 6 hours of practices selected from all four domains of yoga mentioned above. These included specific asanas for hypertension, pranayama, meditation and relaxation sessions. Yogic life style and cognitive change for stress management were discussed during individual yogic counseling sessions and daily group lectures. Table 3 shows the procedure for Laghu shankha prakshalana (LSP). The intervention was delivered by trained yoga therapists who had experience of administering LSP as well as IAYT module for hypertension for more than two years. This was done under the supervision of physicians [Tables 2 and 3].
Table 2.
IAYT module for hypertension
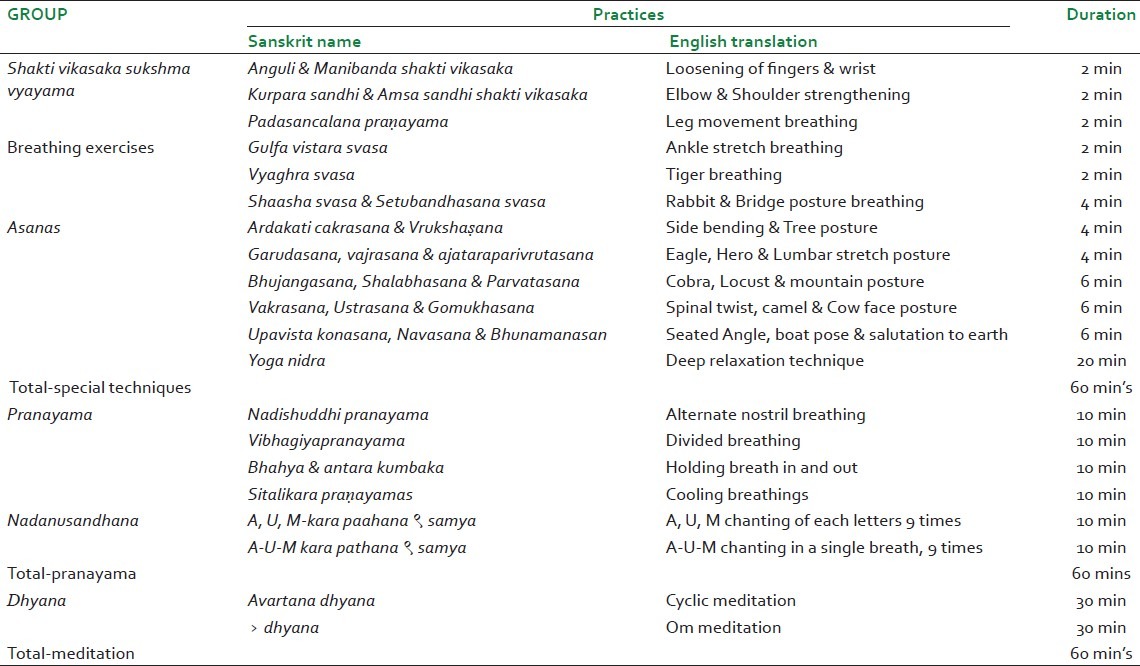
Table 3.
Procedure of laghuśankhaprakṣālana
Statistical analysis
The data were analyzed using statistical package for the Social Science (SPSS Version 10.0). Shapiro-Wilk's test was used for checking normality. Normally distributed variables (BP, Pulse, Respiratory rate, Bhramari, BMI, Comfort, STAI Anxiety level) were analyzed using Paired sample t test. Data that were not normally distributed (GHQ, Medication score, Symptom score, fatigue and quality of sleep) were analyzed using Wilcoxon's signed ranks test. The numerical variables were analyzed using Chi-square test.
RESULTS
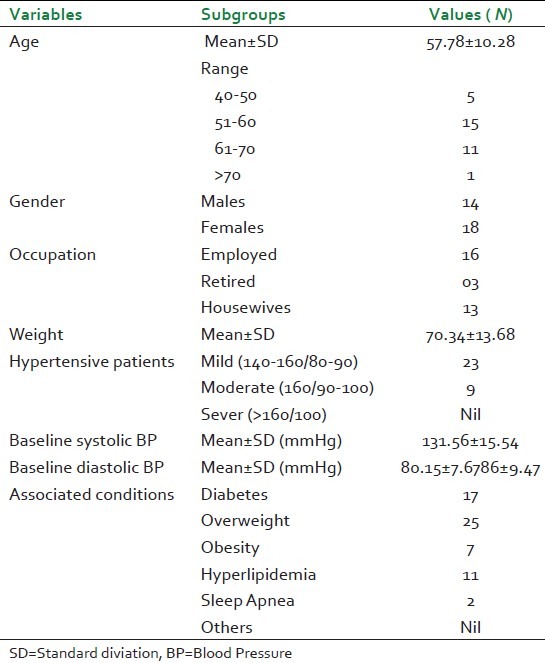
Table 1 shows the demographic details of the patients. Thirty two patients (14 males) with essential HTN were recruited for the study. The mean age was 57.78 ± 10.28 years?. The mean weight was 70.34 ± 13.68kg. Of these 17 had associated diabetes.
Table 1.
Demographic details of the subjects
Immediate Effect of LSP
There were no significant baseline differences between the values recorded before the sessions. All variables were normally distributed [Table 4].
Table 4.
Effect of NWLSP and TWLSP on blood pressure
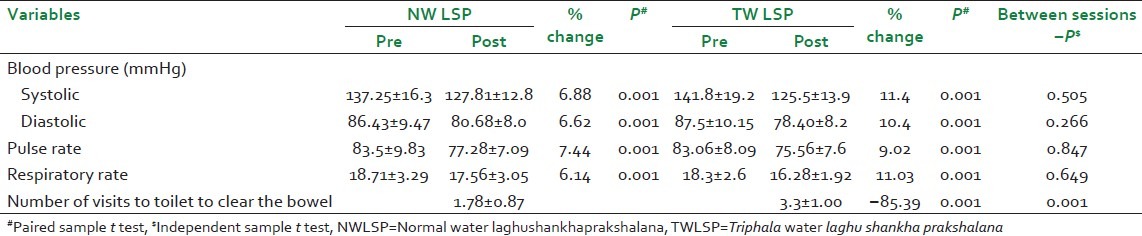
Blood Pressure
Paired samples t test showed significant reduction in systolic (P < 0.001) and diastolic blood pressure (P < 0.001) after both the sessions. The systolic blood pressure decreased by 6.8% after normal water LSP (NWLSP) session and 11.4% after LSP with triphala water (TWLSP); diastolic blood pressure decreased by 6.62% after NWLSP and 10.4% after TWLSP session. Statistically, there was no significant difference between the post values of the two sessions (P < 0.505, Independent sample t test).
Pulse rate
There was significant reduction in pulse rate in both groups (paired t test, P < 0.001), 7.4% after NWLSP and 9.02% after TWLSP. But no significant difference was found between the groups post-LSP. (P < 0.847, Independent sample t test).
Respiratory rate
The respiratory rate reduced significantly in both groups (paired t test P < 0.001), 6.14% after NWLSP and 11.03% after TWLSP. There was no significant difference between the groups (Independent samples t test, P = 0.65).
Number of visits to toilet to empty the bowel during the procedure
The mean value was 1.78 for NWLSP and 3.3 for TWLSP with significant difference between the sessions (P < 0.001, Chi-square test).
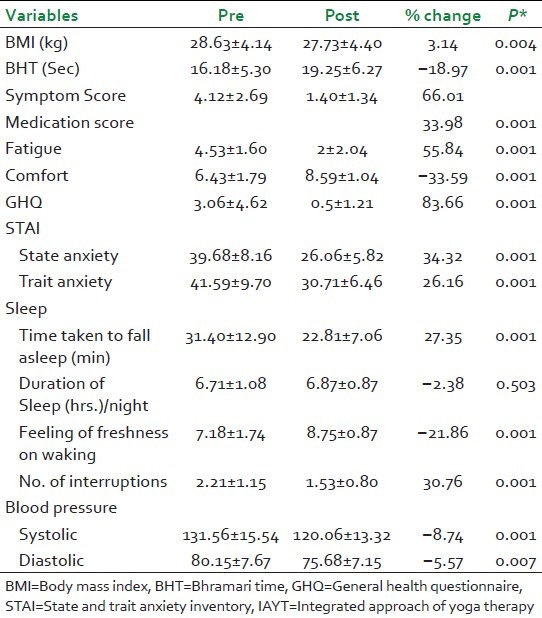
Effect of weeklong yoga therapy
There was significant reduction in systolic and diastolic blood pressure (P < 0.001), BMI (P < 0.004), medications score (P < 0.001), symptoms score (P < 0.001), fatigue (P < 0.001), state and trait anxiety scores (STAI, P < 0.001) and scores on ill health (GHQ, P < 0.001) with increase in duration of Bhramari time (P < 0.001), comfort level (P < 0.001) and quality of sleep (P < 0.001) [Table 5].
Table 5.
Weeklong IAYT therapy on secondary outcome measures
DISCUSSION
This self as control study on 32 participants with essential hypertension was aimed at looking at the safety of LSP. There were no adverse effects; there was significant (P < 0.001) reduction in blood pressure, pulse rate and respiratory rate after both sessions of LSP (NWLSP and TWLSP) with better clearance of the bowel after TWLSP. Significant changes were also observed in the comprehensive battery of tests after the weeklong program of residential IAYT.
Comparisons
Several well designed controlled studies have shown the benefits of different types of yoga based relaxation (with or without biofeedback) and meditative techniques in hypertensive patients on blood pressure and other hemodynamic variables practiced for varying periods of time. Biofeedback studies reduced systolic BP by 19.6% and the diastolic BP by 10.6% at the end of 8 weeks of meditation, which further reduced by 22.4% and 11.5% at the end of 8 months respectively.[25] This was the maximum reduction noted in BP variables by any mind-body intervention. Another effective mind-body technique, the MBSR (Mindfulness Based Stress Reduction),[26] caused reduction of systolic BP by 21.92% and diastolic BP by 16.70% after 8 weeks of the practice. Other meditations such as Transcendental meditation,[27] yogic relaxation,[28] Om meditation,[29] traditional Chinese physical and mental exercises[30] etc., caused reduction in Systolic BP ranging from 2 to 10% and the diastolic between 1.5 to 13%.
Looking at the effect of only the yoga postures on blood pressure, there appears to be mixed responses observed by different studies. Miles et al.,[31] showed a significant increase in blood pressure, heart rate and cardiac output immediately after a series of 23 hatha-based yoga postures in healthy volunteers, whereas Mizuno et al.,[32] observed significant reduction of systolic blood pressure (P < 0.05), heart and respiratory rate (P < 0.05) after 4 months of regular practice of a sequence of yoga postures in patients with hypertension. This suggests that though acute cardiovascular responses (increase in blood pressure, heart rate and cardiac output) to yoga postures are similar to those observed in isometric exercise,[31] when practiced regularly for a longer duration yoga postures actually cause reduction in blood pressure and heart rate.[32] This may be due to the modulation of autonomic nervous system which is induced by regular practice of yoga postures.[32]
There are very few studies that have looked at the immediate effects on blood pressure after the practice of selected yoga techniques. Telles et al.,[33] looked at the immediate effect of alternate nostril yoga breathing (ANYB) in a three armed randomized control study on 90 participants with essential hypertension and showed significant decrease in both systolic (4.24%, P < 0.001) and diastolic blood pressures (1.56%, P < 0.05). The immediate effect of sukha pranayama (at the rate of 6 breaths/min for 5 min) was studied by Bhavanani et al., in hypertensive patients (attending a hospital yoga outpatient dept.) which showed significant (P < 0.05) reduction in heart rate, systolic pressure, pulse pressure, mean arterial pressure and rate-pressure product, after just 5 min of the practice.[34] The effect of 10 sessions of slow abdominal breathing (six cycles/min) combined with frontal EMG biofeedback was compared with abdominal breathing without EMG feedback in postmenopausal women with pre-hypertension; significant reduction in systolic blood pressure by 8.4% and diastolic by 3.9% was observed in those with the biofeedback.[35] Palomba et al., showed reduction in blood pressure and BP emotional reactivity after a short (four sessions) Heart Rate-Biofeedback (HR-BF) protocol in unmedicated outpatients with pre- or stage 1 hypertension.[36] The present study on the immediate effect of yogic LSP in patients with moderate to mild HTN has shown reduction by 11.4% (systolic) and 6.68% (diastolic) after TWLSP, and 10.4% (systolic) and 6.62% (diastolic) after NWLSP. Thus, it seems that for immediate BP reduction, LSP is not only safe but may be more effective than ANYB, Breath Awareness or abdominal breathing with biofeedback.
Mechanisms
Improved autonomic stability with reduced stress appears to be the mechanism by which yoga helps in reducing the blood pressure in hypertensive patients. Studies point to reduction in sympathetic arousal following yoga based relaxation techniques.[37] Yoga offers mastery over the emotional surges through controlled and need based physiological responses to stressfully demanding situations instead of uncontrolled overtones of HPA axis during chronic stress.[38] Yoga changes the physiological responses to stressors by improving autonomic stability with better parasympathetic tone and reduction in sympathetic arousal with improved performance.[39]
Yoga texts clearly mention that the aim of any yoga practice, whether physical, breathing, mental or emotional, is to reach a state of control (chittavrtti nirodha) over the responses to situations (healthy stress response)[7] by the process of slowing or silencing the mind.[8] Internal awareness of the changes in the mind helps in conscious slowing down and thus offers physiological rest. Sage Gaudapada in his treatise, mandukya karika,[3] proposes a concept that one can go on deepening the level of rest by using a series of alternate stimulations (physical stretch or breath awareness or chanting) followed by relaxation technique. Stronger the stimulation (within safety limits), deeper is the rest that follows. Studies using this concept have shown the expected benefits of deep rest and autonomic stability.[40] All kriyas (procedures) including LSP seem to offer this deep stimulation by activating the basic autonomic reflexes. Thus we propose that the activated peristaltic reflex during LSP provided the strong internal awareness that could lead to deeper physiological rest during the relaxation session that followed. Another factor that may have helped in reduction of blood pressure after LSP can be - the dehydration caused due to repeated loose motions. The percent reduction of BP was higher after triphala water LSP than normal water LSP and frequency of stools was significantly more in the triphala group, this can be explained on the basis of mild laxative effect of triphala which may help in reducing blood volume further, thereby reducing the blood pressure. We are not sure whether during normal water LSP (without triphala) person loses the same amount of water that he has consumed or he loses some extra water from the body as well. Another possibility is enhanced biomechanical effects of laxation as according to the Indian systems of health, the apana vata in the GI tract influences other vatas in the body, including the vyana vayu. Blood pressure is a function of the vyana vata.
Limitations and scope of the study
This is the first controlled study on LSP with a good sample size that offers the evidence for the safety of the procedure in hypertensive patients.
It may have helped to have an additional group (as baseline control) with only IAYT practices without LSP to make the study more robust. Durability of response - short term and long term, outcomes with repeated procedures, subgroup analysis of those with a tendency to constipation may all help to bring forth the effects. Measuring serum electrolytes and stool volume would have been helpful to understand mechanisms. Blood pressure and pulse variations in supine and standing conditions for autonomic response, ankle brachial index and serum electrolytes could have enhanced the study. It would be interesting to assess the effects of LSP using more objective measures such as heart rate variability, holter blood pressure and heart rate monitoring during the entire practice in normal volunteers and hypertensive patients. Glomerular filtration rate alterations, urinary frequency and volume could have assisted in speculating extent of water absorption. There are no repeated measures were done in this study to know the carry over effect of LSP. Future studies should consider this important evaluation and try to generate a dose response curve.
Also, future studies could look into application of these non-pharmacological interventions in pre hypertensive and early hypertensive patients to assess whether these simple and safe interventions could reduce the dependence on modern anti-hypertensive drugs.
CONCLUSION
This study provides the first evidence that laghu shankha prakshalana kriya can be used safely in patients with mild to moderate essential hypertension. Addition of triphala to the water of LSP provides better cleansing. Also a weeklong practice of specific set of integrated yoga program is useful in improving the subjective and objective measures of health in patients with essential hypertension.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Messerli FH, Williams B, Ritz E. Essential hypertension. Lancet. 2007;370:591–603. doi: 10.1016/S0140-6736(07)61299-9. [DOI] [PubMed] [Google Scholar]
- 2.WHO: World health statistics. 2012. [Last accessed on 06-09-2013]. Available from: http://www.who.int/gho/publications/world_health_statistics/2012 .
- 3.Nagendra HR, Nagarthna R. New Perspective In Stress Management. 1st ed. Bangalore: Swami Vivekananda Yoga Prakashana; 2000. pp. 15–20. [Google Scholar]
- 4.Bijlani RL. Understanding medical Physiology. 2nd ed. New Delhi: Jaypee Brothers Medical Publishers; 1997. pp. 183–88. [Google Scholar]
- 5.Sullivan MD, LaCroix AZ, Spertus JA, Hecht J. Five-year prospective study of the effects of anxiety and depression in patients with coronary artery disease. Am J Cardiol. 2000;86:1135–8. doi: 10.1016/s0002-9149(00)01174-7. [DOI] [PubMed] [Google Scholar]
- 6.Kreitzer MJ, Snyder M. Healing the heart: Integrating complementary therapies and healing practices into the care of cardiovascular patients. Prog Cardiovasc Nurs. 2002;17:73–80. doi: 10.1111/j.0889-7204.2002.00626.x. [DOI] [PubMed] [Google Scholar]
- 7.Four Chapters on Freedom. 1st ed. Munger: Yoga Publication Trust; 2011. Swami Satyananda Saraswati; pp. 2–5. [Google Scholar]
- 8.Atreya BL. Vasisthadarshanam. 2nd ed. Madras: Indian Heritage Trust; 1993. pp. 105–22. [Google Scholar]
- 9.Swami Vireshwarananda. Srimad Bhagavad Gita. 2nd ed. Chennai: Sri Ramakrishna Math Printing Press Mylapore; 2000. p. 56. [Google Scholar]
- 10.Yang K. A review of Yoga programs for four leading risk factors of chronic diseases. Evid Based Complement Alternat Med. 2007;4:487–91. doi: 10.1093/ecam/nem154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kerstin K, Ahmed A, Jasmin O, Gert R, Hendrik B. Iyengar Yoga increases cardiac parasympathetic nervous modulation among healthy Yoga practitioners. Evid Based Complement Alternat Med. 2007;4:511–7. doi: 10.1093/ecam/nem087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schneider RH, Grim CE, Rainforth MV, Kotchen T, Nidich SI, Gaylord-King C, et al. Stress reduction in the secondary prevention of cardiovascular disease: Randomized, controlled trial of transcendental meditation and health education in Blacks. Circ Cardiovasc Qual Outcomes. 2012;5:750–8. doi: 10.1161/CIRCOUTCOMES.112.967406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Patel C. 12-Month follow-up of Yoga and Bio-feedback in the Management of Hypertension. Lancet. 1975;305:62–4. doi: 10.1016/s0140-6736(75)91070-3. [DOI] [PubMed] [Google Scholar]
- 14.Bhuyan G, Baghel M. A Clinical Study on Uccharaktachapa (Essential Hypertension) with Virechana and Shamana Yoga (A Herbal Compound) Ayu. 2007;28:87. [Google Scholar]
- 15.Shukla G, Bhatted S, Dave A, Shukla V. Efficacy of Virechana and Basti Karma with Shamana therapy in the management of essential hypertension: A comparative study. Ayu. 2013;34:70–6. doi: 10.4103/0974-8520.115455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nagarathna R, Nagendra HR. Yoga For Hypertension and Heart Diseases. 1st ed. Bangalore: Swami Vivekananda Yoga Prakashana; 2012. pp. 45–60. [Google Scholar]
- 17.Swami Digambarji, Gharote M. Gheranda Samhita. 1st ed. Lonavla: Kaivalyadhama SMYM Samiti; 2000. p. 38. [Google Scholar]
- 18.Munshi R, Bhalerao S, Rathi P, Kuber VV, Nipanikar SU, Kadbhane KP. An open-label, prospective clinical study to evaluate the efficacy and safety of TLPL/AY/01/2008 in the management of functional constipation. J Ayurveda Integr Med. 2011;2:144–52. doi: 10.4103/0975-9476.85554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baliga MS, Meera S, Mathai B, Rai MP, Pawar V, Palatty PL. Scientific validation of the ethnomedicinal properties of the Ayurvedic drug Triphala: A review. Chin J Integr Med. 2012;18:946–54. doi: 10.1007/s11655-012-1299-x. [DOI] [PubMed] [Google Scholar]
- 20.Munshi R, Bhalerao S, Rathi P, Kuber V. An open-label, prospective clinical study to evaluate the efficacy and safety of triphalaguggulu in the management of functional constipation. J Ayurveda Integr Med. 2011;2:144–52. doi: 10.4103/0975-9476.85554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Acharya Yadavji Trikamji. Susruta sutrasthana. 6th ed. Varanasi: Chaukhamba Surabharathi Prakashan; 1992. p. 46. [Google Scholar]
- 22.Lu K, Chakroborty D, Sarkar C, Lu T, Xie Z, Liu Z, et al. Triphalâ and its active constituent chebulinic Acid are natural inhibitors of vascular endothelial growth factor-a mediated angiogenesis. PLoS One. 2012;7:e43934. doi: 10.1371/journal.pone.0043934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pandian JD, Toor G, Arora R, Kaur P, Dheeraj KV, Bhullar RS. Complementary and alternative medicine treatments among stroke patients in India. Indian J Exp Biol. 2012;50:195–200. doi: 10.1310/tsr1905-384. [DOI] [PubMed] [Google Scholar]
- 24.Ramachandran AP, Prasad SM, Prasad UN, Jonah S. A comparative study of Kaishora Guggulu and Amrita Guggulu in the management of UtthanaVatarakta. Ayu. 2010;31:410–6. doi: 10.4103/0974-8520.82027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Patel C, Marmot M, Terry D. Controlled trial of biofeedback-aided behavioral methods in reducing mild hypertension. Br Med J (Clin Res Ed) 1981;282:2005–8. doi: 10.1136/bmj.282.6281.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Palta P, Page G, Piferi RL, Gill JM, Hayat MJ, Connolly AB, et al. Evaluation of a mindfulness-based intervention program to decrease blood pressure in low-income African-American older adults. J Urban Health. 2012;89:308–16. doi: 10.1007/s11524-011-9654-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schneider RH, Grim CE, Rainforth MV, Kotchen T, Nidich SI, Gaylord-King C, et al. Stress reduction in the secondary prevention of cardiovascular disease: Randomized, controlled trial of transcendental meditation and health education in Blacks. Circ Cardiovasc Qual Outcomes. 2012;5:750–8. doi: 10.1161/CIRCOUTCOMES.112.967406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Patel C. Twelve month follow-up of Yoga and bio-feedback in the management of hypertension. Lancet. 1975;305:62–4. doi: 10.1016/s0140-6736(75)91070-3. [DOI] [PubMed] [Google Scholar]
- 29.Telles S, Nagarathna R, Nagendra HR. Autonomic changes during “OM” meditation. Indian J Physiol Pharmacol. 1995;39:418–20. [PubMed] [Google Scholar]
- 30.Zhang Y, Li N, Sun J. Effects of combined traditional Chinese exercises on blood pressure and arterial function of adult female hypertensive patients. Res Sports Med. 2013;21:98–109. doi: 10.1080/15438627.2013.741030. [DOI] [PubMed] [Google Scholar]
- 31.Miles SC, Chun-Chung C, Hsin-Fu L, Hunter SD, Dhindsa M, Nualnim N. Arterial blood pressure and cardiovascular responses to yoga practice. Altern Ther Health Med. 2013;19:38–45. [PubMed] [Google Scholar]
- 32.Mizuno J, Monteiro H. An assessment of a sequence of yoga exercises to patients with arterial hypertension. J Bodyw Mov Ther. 2013;17:35–41. doi: 10.1016/j.jbmt.2012.10.007. [DOI] [PubMed] [Google Scholar]
- 33.Telles S, Yadav A, Kumar N, Sharma S, Naveen K, Balakrishna A. Blood pressure and purdue pegboard scores in individuals with hypertension after alternate nostril breathing, breath awareness, and no intervention. Med Sci Monit. 2013;19:61–6. doi: 10.12659/MSM.883743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bhavanani AB, Sanjay ZM, Madanmohan Immediate effect of sukhaprānāyāma on cardiovascular variables in patients of hypertension. Int J Yoga Therap. 2011;21:73–6. [PubMed] [Google Scholar]
- 35.Wang SZ, Li S, Xu XY, Lin GP, Shao L, Zhao Y. Effect of slow abdominal breathing combined with biofeedback on blood pressure and heart rate variability in prehypertension. J Altern Complement Med. 2010;16:1039–45. doi: 10.1089/acm.2009.0577. [DOI] [PubMed] [Google Scholar]
- 36.Palomba D, Ghisi M, Scozzari S, Sarlo M, Bonso E, Dorigatti F. Biofeedback-assisted cardiovascular control in hypertensive exposed to emotional stress: A pilot study. Appl Psychophysiol Biofeedback. 2011;36:185–92. doi: 10.1007/s10484-011-9160-3. [DOI] [PubMed] [Google Scholar]
- 37.Vempati RP, Telles S. Yoga based guided relaxation reduces sympathetic activity in subjects based on baseline levels. Psychol Rep. 2002;90:487–94. doi: 10.2466/pr0.2002.90.2.487. [DOI] [PubMed] [Google Scholar]
- 38.Leonard BE. HPA and immune axes in stress: Involvement of the serotonergic system. Neuroimmunomodulation. 2006;13:268–76. doi: 10.1159/000104854. [DOI] [PubMed] [Google Scholar]
- 39.Telles S, Narendran S, Raghuraj P, Nagarathna R, Nagendra HR. Comparison of changes in autonomic and respiratory parameters of girls after yoga and games at a community home. Percept Mot Skills. 1997;84:251–7. doi: 10.2466/pms.1997.84.1.251. [DOI] [PubMed] [Google Scholar]
- 40.Subramanya P, Telles S. A review of the scientific studies on cyclic meditation. Int J Yoga. 2009;2:46–8. doi: 10.4103/0973-6131.60043. [DOI] [PMC free article] [PubMed] [Google Scholar]


