Abstract
The desire for improved esthetics has increased tremendously over the years. Periodontal plastic surgery deals with regenerative procedures designed to restore form, function and enhance esthetics. The aim of this study was to evaluate the effectiveness of subepithelial connective tissue graft using pouch and tunnel technique as root coverage procedure. Three patients corresponding to a total of 8 sites participated in the study. Maxillary teeth with miller's class I gingival recession were included in the study. All the sites were treated using subepithelial connective tissue graft using pouch and tunneling technique. Patients were followed up for a period of 6 months and 1 year. All the treated teeth showed 100% root coverage at the end of 6 months and 1 year. Gingival recession is a common occurrence and its prevalence increases with age. It can lead to clinical problems, diminished cosmetic appeal and hence esthetic concern. There are various techniques for root coverage. Subepithelial connective tissue graft has shown the best predictability (95%) of root coverage in Millers class I & II cases. This technique preserves the intermediate papilla, accelerates the initial wound healing & also applies less traction. Due to minimal trauma at the recipient site, this procedure may be advantageous in treatment of recession as compared to other treatment modalities.
Keywords: Gingival recession, periodontal plastic surgery, subepithelial connective tissue graft
INTRODUCTION
Periodontal plastic surgery is defined as the surgical procedures performed to correct or eliminate anatomic, developmental or traumatic deformities of the gingiva or alveolar mucosa.[1] Gingival recession is defined as the displacement of the gingival margin apical to the cemento-enamel junction (CEJ) with the loss of periodontal connective tissue fibers along with root cementum and alveolar bone.[2] Studies by Murray and Gorman et al. have shown that recession increases with increasing age. A survey revealed that 88% of people above 65 years of age and 50% of people between 18 and 64 years of age have one or more sites with recession (Serino G, Wennstrom JL, Lindhe J, Eneroth L).[3] The main indications for root coverage procedure are esthetic demands, root hypersensitivity, root caries lesions and cervical abrasions. Thus, it is essential to carry out root coverage surgery for the aforementioned conditions.[4] If untreated, gingival recession may progress to the point that it can compromise the prognosis of the tooth in question.
The amount of recession is assessed clinically by measuring in millimeters the distance from the CEJ and the soft tissue margin. The recession of gingiva, either localized or generalized, may be associated with one or more surfaces, resulting in attachment loss and root exposure. Marginal gingival recession, therefore should not be viewed as merely a soft tissue defect, but as the destruction of both the soft and hard tissue.[5]
CAUSES OF GINGIVAL RECESSION
-
Predisposing factors:
- Minimal attached gingiva
- Aberrant frenal pull
- Tooth malposition (fenestration and dehiscence).
-
Precipitating factors:
- Inflammation related to plaque
- Improper tooth brushing
- Iatrogenic factors such as crown preparations extending subgingivally, impression techniques involving gingival retraction
- Poor orthodontic treatment where the teeth are moved outside the labial or lingual plate
Anatomical factors include abnormal tooth position in the arch, aberrant path of eruption, individual tooth shape
Pathological factors such as bone resorption due to periodontal disease.[6]
Accepted procedures for multiple root coverage include coronally advanced flap with/without free mucosal graft, subepithelial connective tissue graft (SCTG) and guided tissue regeneration. Other materials like Emdogain (EMD), acellular dermal matrix have also been tried. Connective tissue grafts are an important treatment options for periodontal and implant reconstructive plastic surgery. Connective tissue graft was first used by Edel (1974), Broome and Taggart (1976) and Donn (1978), to increase the width of keratinized gingiva. The use of connective tissue grafts for treatment of gingival recession began in 1985 when Langer and Langer described SCTG technique for covering gingival recession of both single and multiple adjacent teeth.[7] They described a technique in which the graft is covered by the overlying partial thickness flap. Nelson proposed the use of full thickness flap to cover the SCTG.[8]
In 1985 Raetzke, described a different version of connective tissue graft called “Envelope technique.”[9] Allen in 1994, in a modification of Raetzke's technique, described the “Tunnel or supraperiosteal envelope technique,” for treatment of multiple adjacent gingival recession.[10] Santarelli et al.[11] adapted the tunnel technique using a single vertical incision. Mahn adapted the tunnel approach for acellular dermal connective tissue grafting by using full thickness procedure with vertical incisions.[12]
Indications for pouch and tunnel technique include:
Miller's Class I and Class II gingival recession
Lack of adequate donor tissue for lateral sliding flap
Presence of multiple and wide recessions in maxillary teeth
Increased recession in areas where esthetic concerns is of great concern
Exposed root sensitivity.
This case series outlines the advantages of SCTG using pouch and tunnel procedure, as outlined by Allen in 1994, for treatment of multiple gingival recessions over other treatment modalities.
MATERIALS AND METHODS
The patients for this study were taken from the patient pool of Department of Periodontics, Oxford Dental College, Hospital and Research center, Bangalore. Three patients aged between 20 and 25 years participated in this study.
Inclusion criteria
Maxillary anterior teeth and premolars with Miller's Class I recession
Normal alignment of teeth in the arch
Patient not undergone any periodontal surgery in the past 1 year.
Exclusion criteria
Root surface restorations
Root caries
Smoking
Trauma from occlusion
Abnormal frenal attachment
Medically compromised patients.
Case 1
A 21-year-old male patient reported with the complaint of sensitivity in upper left anterior teeth region. On examination, Miller's Class I gingival recession was present in relation to 23 and 24. The width of attached gingiva was found to be adequate in the region of 23 and 24. A pouch and tunnel technique utilizing palatal connective tissue graft for root coverage was planned based on the indications stated above [Figure 1].
Figure 1.

Miller's Class I gingival recession with respect to 23 and 24
Case 2
A 25-year-old male patient complained of longer teeth in relation to upper left anterior region. On examination there was Miller's Class I gingival recession in relation to 21, 22 and 23.
Case 3
A 20-year-old female patient came with the chief complaint of sensitivity in her upper right anterior teeth. On examination, there was Miller's Class I recession in relation to 12, 13 and 14.
PRESURGICAL PROTOCOL
The treatment protocol was explained to all three patients and an informed consent was obtained. Routine periodontal therapy, including scaling and root planning was done. Oral hygiene instructions were given. Patients recalled after 4 weeks for the surgical procedure.
SURGICAL TECHNIQUE
Recipient site preparation
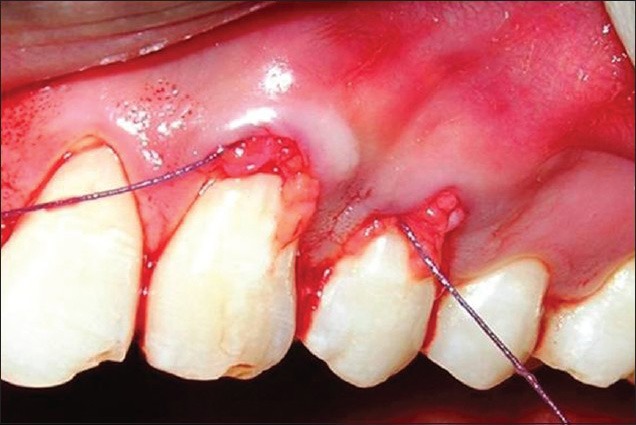
Following administration of local anesthesia, i.e., local infiltration of 2% lidocaine with a concentration of 1:200000 epinephrine, sulcular incisions through each recession area were given with a number 15 blade. Care was taken not to extend the incisions till the tip of the interdental papilla. A full thickness mucoperiosteal flap was reflected, extending beyond the mucogingival junction. This was done so as to reduce the tension on the flap to facilitate coronal displacement following placement of the graft. Each pedicle adjacent to the recession was undermined gently, without detaching it completely to prepare a tunnel. The undermining of tissues to prepare the tunnel was done by extending it laterally about 3-5 mm [Figure 2].
Figure 2.

Crevicular incisions given and pouch and tunnel prepared
Donor site preparation
SCTG was harvested using Lui's Class I incision from the palate.[13] The incision was placed between distal aspect of canine and mesial aspect of first molar area. After the graft was harvested, pressure was applied to the donor area with gauze soaked in saline, to control bleeding. The palatal flap was then sutured with 4-0 direct interrupted suture [Figures 3 and 4].
Figure 3.

Incisions given on the palate
Figure 4.

Subepithelial connective tissue graft harvested
Graft placement
The graft was stabilized using a 5-0 silk suture. The mesial aspect of the graft was pierced with the needle, and the needle was passed passively underneath the tunnel created between the adjacent recessions. The suture was passed from the mesial aspect of the tunnel and pushed gently to the distal direction with a periosteal elevator so that the graft could slide underneath the tunnel. The graft was positioned coronal to CEJ. After positioning, the graft was secured to the mesial and distal aspect with sling sutures in order to prevent movement of the graft [Figures 5 and 6].
Figure 5.
Graft stabilized with 5-0 sutures
Figure 6.

Sutures placed
Dry tin foil was applied to the recipient site. A periodontal dressing (Coe Pak) was placed over the foil to stabilize and protect the donor tissue [Figure 7].
Figure 7.

Periodontal dressing placed
Post-operative instructions
The patients were advised to use 0.2% chlorhexidine gluconate mouth rinse twice daily for 2 weeks. Post-operative home care instructions were given and they were prescribed analgesic to reduce post-operative pain and discomfort. Sutures were removed after 10 days. The patients were further followed up at 3 and 6 months intervals for supportive periodontal therapy. All the sites healed uneventfully. The donor site appeared normal in color and healthy after 4 weeks and the recipient site was healthy with excellent color match with adjacent tissues. After 1 year, complete root coverage achieved, remained so without any adverse effects. The patient reported satisfactory esthetic results and loss of hypersensitivity [Figure 8].
Figure 8.

At 1 year post-operative follow-up
DISCUSSION
Gingival recession is a very common occurrence nowadays and requires treatment to prevent further complications. In the past, periodontal treatment procedures were mainly aimed at preventing and treating the existing periodontal diseases. However, with increasing esthetic demands these surgical procedures are modified so as to preserve and enhance esthetics by various periodontal plastic surgical procedures. Periodontal plastic surgery deals with procedures that are designed to enhance esthetics, restore form, function and also include regenerative modalities too.
Obtaining predictable root coverage has become an important part of periodontal therapy. Many surgical procedures have been attempted to obtain root coverage. Some techniques when attempted produce unsatisfactory results. The reasons could be; poor case selection, improper technique selection, inadequate root preparation, insufficient height of interdental bone and soft tissue, poor surgical technique, insufficient blood supply from the surrounding tissues due to in adequate recipient site preparation, flap penetration.
There have been a number of treatment modalities for managing gingival recession such as free gingival graft, coronally advanced flap, use of barrier membranes, EMD, various growth factors etc., SCTG has become a popular treatment modality for coverage of denuded roots because of its high degree of success. It has shown the best predictability (95%) of root coverage in Millers Class I and II cases.[14] The clinical advantage of SCTG is apparent not only at the recipient site, where there is good tissue blending, but also at the palatal donor site, as it uses a more conservative approach to harvest the graft causing reduced degree of discomfort to the patient.
Langer and Langer[7] published an article that introduced and outlined the indications and procedures necessary for achieving success with the SCTG. They indicated that their technique had “the advantage of a closer color blend of the graft with adjacent tissue avoiding the “Keloid” healing present with free gingival grafts. The success of these grafts has been attributed to the double blood supply at the recipient site from the underlying connective tissue base and the overlying recipient flap. It can be used to gain total root coverage in isolated and multiple sites. When histologically evaluated, use of SCTG over recession defects results in periodontal regeneration.[15]
In this study, all the sites treated with pouch and tunnel technique showed 100% root coverage. The pre-operative recession height ranged from 3 to 4 mm and width around 2-4 mm. At the end of 1 year, all the sites showed complete root coverage. The tunnel technique was developed as a modification of the envelope technique. This technique was designed specifically for the wide multiple recessions frequently found in the maxilla where root coverage seems to be most difficult to obtain. The results of the tunnel procedure demonstrated favorable root coverage. The use of the tunnel technique not only preserves the papillary height between two mucogingival defects, but also helps maintain adequate blood supply to the underlying graft. It also provides excellent adaptation of the graft to the recipient site. Produces highly esthetic results and also increase the thickness of keratinized gingiva.
CONCLUSION
Gingival recession is a serious concern both functionally and esthetically. The surgical technique of choice depends on several factors, each having their advantages, disadvantages, indications and contraindications. The clinician should choose from among the different surgical protocols available, selecting the least traumatic technique for the patient. Success of any root coverage procedure is determined by various factors that are critical at each step of the procedure starting from case selection to long-term maintenance (supportive periodontal therapy) and patient compliance. SCTG with pouch and tunnel technique produces significantly superior and predictable results with greater advantages.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.American Academy of Periodontology: Proceedings of the world workshop in periodontics. Ann Periodontol. 1996;1:37–215. [Google Scholar]
- 2.Wennstrom JL, Zucchelli G, Pini Prato GP. Mucogingival surgery. In: Lang NP, Karring T, editors. Clinical Periodontology and Implant Dentistry. 5th ed. Oxford, UK: Blackwell Munksgaard; 2008. pp. 955–1011. [Google Scholar]
- 3.Serino G, Wennström JL, Lindhe J, Eneroth L. The prevalence and distribution of gingival recession in subjects with a high standard of oral hygiene. J Clin Periodontol. 1994;21:57–63. doi: 10.1111/j.1600-051x.1994.tb00278.x. [DOI] [PubMed] [Google Scholar]
- 4.Goldstein M, Brayer L, Schwartz Z. A critical evaluation of methods for root coverage. Crit Rev Oral Biol Med. 1996;7:87–98. doi: 10.1177/10454411960070010601. [DOI] [PubMed] [Google Scholar]
- 5.Ahathya RS, Deepalakshmi D, Ramakrishnan T, Ambalavanan N, Emmadi P. Subepithelial connective tissue grafts for the coverage of denuded root surfaces: A clinical report. Indian J Dent Res. 2008;19:134–40. doi: 10.4103/0970-9290.40468. [DOI] [PubMed] [Google Scholar]
- 6.Leong DJ, Wang HL. A decision tree for soft tissue grafting. Int J Periodontics Restorative Dent. 2011;31:307–13. [PubMed] [Google Scholar]
- 7.Langer B, Langer L. Subepithelial connective tissue graft technique for root coverage. J Periodontol. 1985;56:715–20. doi: 10.1902/jop.1985.56.12.715. [DOI] [PubMed] [Google Scholar]
- 8.Nelson SW. The subpedicle connective tissue graft. A bilaminar reconstructive procedure for the coverage of denuded root surfaces. J Periodontol. 1987;58:95–102. doi: 10.1902/jop.1987.58.2.95. [DOI] [PubMed] [Google Scholar]
- 9.Raetzke PB. Covering localized areas of root exposure employing the “envelope” technique. J Periodontol. 1985;56:397–402. doi: 10.1902/jop.1985.56.7.397. [DOI] [PubMed] [Google Scholar]
- 10.Allen AL. Use of the supraperiosteal envelope in soft tissue grafting for root coverage. I. Rationale and technique. Int J Periodontics Restorative Dent. 1994;14:216–27. [PubMed] [Google Scholar]
- 11.Santarelli GA, Ciancaglini R, Campanari F, Dinoi C, Ferraris S. Connective tissue grafting employing the tunnel technique. A case report of complete root coverage in anterior maxilla. Int J Periodontics Restorative Dent. 2001;21:77–83. [PubMed] [Google Scholar]
- 12.Tözüm TF, Dini FM. Treatment of adjacent gingival recessions with subepithelial connective tissue grafts and the modified tunnel technique. Quintessence Int. 2003;34:7–13. [PubMed] [Google Scholar]
- 13.Liu CL, Weisgold AS. Connective tissue graft: A classification for incision design from the palatal site and clinical case reports. Int J Periodontics Restorative Dent. 2002;22:373–9. [PubMed] [Google Scholar]
- 14.Miller PD., Jr A classification of marginal tissue recession. Int J Periodontics Restorative Dent. 1985;5:8–13. [PubMed] [Google Scholar]
- 15.Bruno JF, Bowers GM. Histology of a human biopsy section following the placement of a subepithelial connective tissue graft. Int J Periodontics Restorative Dent. 2000;20:225–31. [PubMed] [Google Scholar]


