Abstract
In adult periodontal patients, pathologic tooth migration can create serious functional and aesthetic problems. In such situations, a combined orthodontic and periodontal treatment is often indicated. However, the lengthy treatment time and the demanding nature of orthodontic therapy for such periodontally compromised teeth is often a challenge. In this case report, an approach combining platelet-rich fibrin for the treatment of osseous defect and a modified crown preparation technique to reposition the crown was done on a pathologically migrated right lateral incisor.
Keywords: Growth factors, interdisciplinary, periodontal bone loss, tooth migration
INTRODUCTION
Pathologic tooth migration is a common complication of moderate to severe periodontitis and is often the cause for patients to seek periodontal therapy. The physiologic tooth position is determined by interactions between the periodontal tissue and occlusal, tongue, and lip forces. Bone destruction resulting from chronic periodontal disease disturbs the equilibrium of these interactive balances, leading to pathologic tooth migration.
Spontaneous repositioning after conventional periodontal treatment is likely to occur, but only when light to moderate degrees of pathologic migration are considered.[1,2] Most cases of severe pathologic tooth migration are arduous to treat and require a team approach consisting of periodontal, endodontic, and orthodontic treatment.
The closure of space and the proper realignment of migrated tooth require orthodontic rectification. The difficulty with orthodontic realignment involves the conscientious utilization of light orthodontic forces to teeth with compromised bone support followed by a long period of retention to prevent relapse.[3] In this case report, a patient with a pathologically migrated anterior tooth with unesthetic appearance was managed without any orthodontic treatment. After controlling the periodontal disease, a modified crown preparation was done to fabricate a crown that would close the anterior space as well as reposition the crown of the migrated tooth.
CASE REPORT
The case we present here is about an 18-year-old female patient who reported to the Department of Periodontology with the chief complaint of loose and extruded right upper front tooth.
On examination, it was noticed that the right lateral incisor had extruded and moved labially giving an unesthetic appearance. There was a deep periodontal pocket distally and the tooth showed Grade II mobility [Figure 1]. Intraoral periapical radiograph showed bone loss distally reaching the apical third of the root along with periapical radiolucency [Figure 2a].
Figure 1.

Preoperative view
Figure 2.
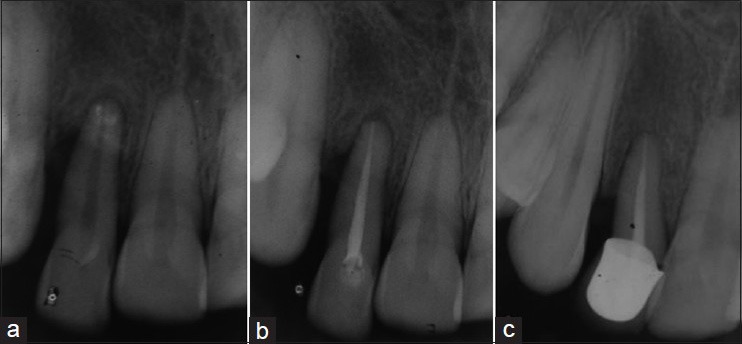
(a) Preoperative radiograph; (b) After endodontic therapy; (c) 6 months post-operative radiograph
Periodontal treatment for this patient consisted of thorough scaling and root planning followed by education on plaque control measures. This was followed by root canal treatment of the affected tooth to eliminate the periapical source of infection. The tooth was assessed after 6 weeks, the mobility had reduced to Grade I and the plaque control of the patient was found to be satisfactory [Figure 2b].
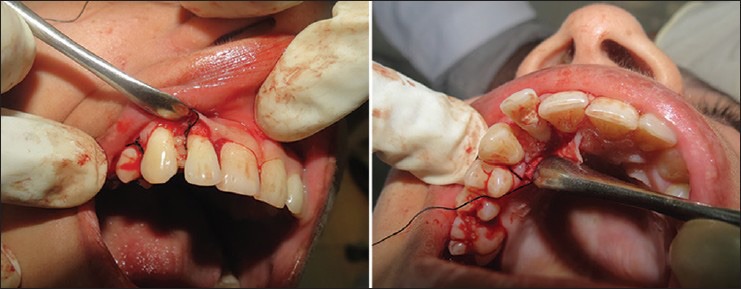
Two weeks after reassessment, periodontal flap surgery was performed in the maxillary right lateral incisor area to completely eliminate the deep periodontal infection. After thorough root planning and debridement, a deep defect distal to the lateral incisor was observed [Figure 3]. It was decided to place platelet-rich fibrin (PRF) in the defect to aid in the regeneration of bone in the area and fasten the healing process [Figure 4]. After placement of PRF, 3.0 silk sutures were placed and Coe pack dressing was given [Figures 5 and 6].
Figure 3.
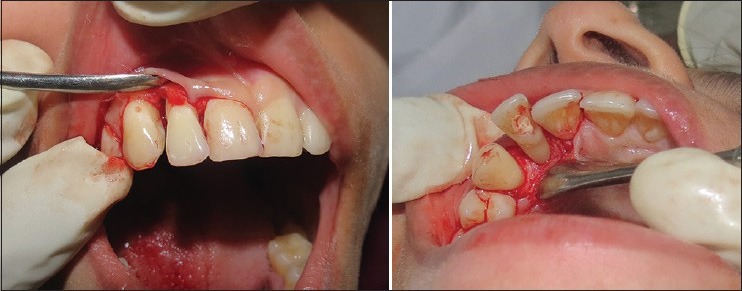
Defect exposed
Figure 4.
Platelet-rich fibrin placed in the defect
Figure 5.

Sutures placed
Figure 6.

Coe pack dressing
After 8 weeks the tooth was reassessed, the probing pocket depth had reduced to 3 mm in the distal site, but there was no spontaneous closure of the anterior space. A modified crown preparation was done on the affected tooth such that the resulting crown would close the anterior space in addition to provide long-term support to root canal treated tooth.
Six months following the treatment, the patient presented with a clinically healthy gingiva and a probing pocket depth of 3 mm [Figure 7]. On posttreatment evaluation of radiograph of the area, it was found that a significant bone fill had occurred in the defect distal to lateral incisor [Figure 2c].
Figure 7.

Six months post-operative view after crown fixation
Preparation of platelet-rich fibrin
A total volume of 10 ml blood was drawn from each patient by venipuncture of the right antecubital vein. Blood was collected in sterile glass test tubes without any anticoagulants and immediately centrifuged on a table top centrifuge (Almicro™ Instruments) at 3000 rpm for 10 min. This resulted in the separation of three basic fractions because of differential densities: The bottom red blood cells (RBCs), middle PRF, and the top layer of platelet-poor plasma (PPP). PPP was aspirated and discarded and the PRF was separated from underlying RBCs by the use of sterile stainless steel scissors.
Modified crown preparation
A triple wheel depth cutter bur (834-016, SS White, Lakewood, New Jersy) was used to prepare the depth cutting gauge at the incisal aspect of the tooth. Since the tooth was tilted mesially and labially, care was taken to reduce more tooth structure at the mesial and labial aspect. A radial shoulder finishing line configuration was prepared first by flat-end tapered diamond bur and then by end–cutting parallel side carbide finishing bur. An all ceramic coronal restoration was fabricated and fixed with light curing acrylic luting cement (Rely X luting cement, 3M ESPE, Ontario, Canada). Care was taken to keep the restoration out of occlusion with the opposite tooth.
DISCUSSION
The primary goal of periodontal treatment is the maintenance of the natural dentition in health and comfortable function. Regenerative periodontal treatments refer to the procedures that are designed to achieve the regeneration of lost periodontal tissues. Periodontal regenerative procedures include bone replacement grafts, root bio modifications, guided tissue regeneration, and their combinations. Advanced periodontal disease may result in pathological migration and intraosseous defects. The use of PRF in treating such defect may be a predictable therapeutic approach. Six months follow-up examination of this case revealed resolution of signs of periodontal disease activity, with gains in clinical attachment levels and absence of bleeding on probing.
PRF described by Choukroun et al. is a second generation platelet concentrate consisting of fibrin membrane enriched with platelets and leukocytes.[4,5] Several studies have evaluated the effectiveness of PRF in intrabony periodontal and have found a positive clinical and radiographic outcome.[6,7] Since PRF consists of a fibrin network, it leads to a more efficient cell migration and proliferation, and thus cicatrization.[8] This unique structure may act as a vehicle for carrying cells that are essential for tissue regeneration. Many growth factors, such as platelet-derived growth factor (PDGF) and transforming growth factor-β, are released from PRF.[4,5,9] Of all known growth factors, PDGF exerts a favorable effect on periodontal regeneration, as measured by gain in clinical attachment and radiographic defect fill in humans.[10]
In this case even after the periodontal disease was controlled, the unesthetic space in the anterior region remained as no spontaneous closure occurred. This may be due to the advanced nature of the lesion as spontaneous repositioning after conventional periodontal treatment is likely, only when light to moderate degrees of pathologic migration are considered.[1,2] Orthodontic repositioning was considered, but was not done for many reasons. The need for wearing fixed appliance or an orthodontic soft aligner and the long-term retention program was not acceptable for the patient.[3] The use of light orthodontic forces in such a periodontally compromised tooth was always challenging. Finally, the cost of the orthodontic therapy was a factor that had to be considered.
A radial shoulder finish line was prepared on the tooth to obtain 90° cavo-surface line angle and rounded internal line angle. This configuration results in less stress concentration on the tooth structure, which is beneficial in case of tooth with compromised bone support. The restoration was kept out of occlusion for faster wound healing and to aid in the periodontal regeneration.
As more patients with periodontal diseases are seeking advanced periodontal treatment, the need to restore the function and esthetics of pathologically migrated tooth is present more than before. Dental treatments of these patients are complex and challenging, especially if there is a need for overall short treatment time. However, interdisciplinary management including periodontal treatment using PRF, endodontic and restorative therapy may be an effective method in restoring the periodontal health and esthetics of a pathologically migrated tooth.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Gaumet PE, Brunsvold MI, McMahan CA. Spontaneous repositioning of pathologically migrated teeth. J Periodontol. 1999;70:1177–84. doi: 10.1902/jop.1999.70.10.1177. [DOI] [PubMed] [Google Scholar]
- 2.Rohatgi S, Narula SC, Sharma RK, Tewari S, Bansal P. Clinical evaluation of correction of pathologic migration with periodontal therapy. Quintessence Int. 2011;42:e22–30. [PubMed] [Google Scholar]
- 3.Kalia S, Melsen B. Interdisciplinary approaches to adult orthodontic care. J Orthod. 2001;28:191–6. doi: 10.1093/ortho/28.3.191. [DOI] [PubMed] [Google Scholar]
- 4.Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, Dohan SL, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part IV: Clinical effects on tissue healing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e56–60. doi: 10.1016/j.tripleo.2005.07.011. [DOI] [PubMed] [Google Scholar]
- 5.Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, Dohan SL, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part V: Histologic evaluations of PRF effects on bone allograft maturation in sinus lift. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:299–303. doi: 10.1016/j.tripleo.2005.07.012. [DOI] [PubMed] [Google Scholar]
- 6.Sharma A, Pradeep AR. Treatment of 3-wall intrabony defects in patients with chronic periodontitis with autologous platelet-rich fibrin: A randomized controlled clinical trial. J Periodontol. 2011;82:1705–12. doi: 10.1902/jop.2011.110075. [DOI] [PubMed] [Google Scholar]
- 7.Thorat M, Pradeep AR, Pallavi B. Clinical effect of autologous platelet-rich fibrin in the treatment of intra-bony defects: A controlled clinical trial. J Clin Periodontol. 2011;38:925–32. doi: 10.1111/j.1600-051X.2011.01760.x. [DOI] [PubMed] [Google Scholar]
- 8.Dohan Ehrenfest DM, Del Corso M, Diss A, Mouhyi J, Charrier JB. Three-dimensional architecture and cell composition of a Choukroun's platelet-rich fibrin clot and membrane. J Periodontol. 2010;81:546–55. doi: 10.1902/jop.2009.090531. [DOI] [PubMed] [Google Scholar]
- 9.Dohan Ehrenfest DM, de Peppo GM, Doglioli P, Sammartino G. Slow release of growth factors and thrombospondin-1 in Choukroun's platelet-rich fibrin (PRF): A gold standard to achieve for all surgical platelet concentrates technologies. Growth Factors. 2009;27:63–9. doi: 10.1080/08977190802636713. [DOI] [PubMed] [Google Scholar]
- 10.Cooke JW, Sarment DP, Whitesman LA, Miller SE, Jin Q, Lynch SE, et al. Effect of rhPDGF-BB delivery on mediators of periodontal wound repair. Tissue Eng. 2006;12:1441–50. doi: 10.1089/ten.2006.12.1441. [DOI] [PMC free article] [PubMed] [Google Scholar]


