Abstract
After the World Health Organization officially declared the end of the first pandemic of the XXI century in August 2010, the influenza A(H1N1)pdm09 virus has been disseminated in the human population. In spite of its sustained circulation, very little on phylogenetic data or oseltamivir (OST) resistance is available for the virus in equatorial regions of South America. In order to shed more light on this topic, we analysed the haemagglutinin (HA) and neuraminidase (NA) genes of influenza A(H1N1)pdm09 positive samples collected during the pandemic period in the Pernambuco (PE), a northeastern Brazilian state. Complete HA sequences were compared and amino acid changes were related to clinical outcome. In addition, the H275Y substitution in NA, associated with OST resistance, was investigated by pyrosequencing. Samples from PE were grouped in phylogenetic clades 6 and 7, being clustered together with sequences from South and Southeast Brazil. The D222N/G HA gene mutation, associated with severity, was found in one deceased patient that was pregnant. Additionally, the HA mutation K308E, which appeared in Brazil in 2010 and was only detected worldwide the following year, was identified in samples from hospitalised cases. The resistance marker H275Y was not identified in samples tested. However, broader studies are needed to establish the real frequency of resistance in this Brazilian region.
Keywords: influenza A(H1N1)pdm09, haemagglutinin, oseltamivir resistance, pyrosequencing
Influenza viruses are well recognised for their viral properties such as sialic-acid receptor specificity, glycosylation, virulence, pathogenicity and development of resistance to drug therapy as well as for their high mutation rates, with the ability to generate antigenically distinct variants (Kilander et al. 2010, Ghedin et al. 2011, Sun et al. 2011). The haemagglutinin (HA) gene presents the highest mutation rates in the influenza genome and its encoded glycoprotein is responsible for the initial steps of successful infection (Wagner et al. 2002). In April 2009, the World Health Organization (WHO) identified the occurrence of novel human influenza cases in Mexico and the United States of America (USA), which were caused by influenza A(H1N1) of swine origin (Garten et al. 2009), thereafter referred to as A(H1N1)pdm09. Within months, the virus had spread worldwide, provoking the first pandemic of the XXI century, accounting for more than 18,000 deaths (WHO 2010). In Brazil, the first cases were confirmed by sequencing and real-time reverse transcription-polymerase chain reaction (RT-PCR) on 7 May 2009 in the Southeast Region from travellers arriving from Mexico. Three weeks later, the local transmission of A(H1N1)pdm09 influenza virus was announced by the Brazilian Ministry of Health. In Pernambuco (PE), a northeast state located in an equatorial region (geographic coordinates of Recife municipality, the state’s capital: 08º03’14’’S 34º52’52’’W), the first case was confirmed at the beginning of June 2009.
Since its establishment in the human population, many authors have monitored polymorphisms of the influenza A(H1N1)pdm09 HA gene, which allowed early phylogenetic classification of the virus into seven distinct clades (Potdar et al. 2010), with clades 6 and 7 being the most prevalent in Brazil and worldwide (Nelson et al. 2009). Mixed viral populations bearing the D222G/N change have been more frequently reported among severe/fatal cases (Ledesma et al. 2011, Wedde et al. 2013, Resende et al. 2014). The changes in this residue are associated with an expansion in viral tropism, allowing linkage of the particles to both α2,6 and α2,3 sialic-acid cell receptors, with the latter being found in the majority in the lower respiratory tract of humans (Liu et al. 2010). In addition, mutations in the neuraminidase (NA) can lead to a loss of sensitivity to oseltamivir (OST), as observed for seasonal A(H1N1) viruses in different countries before the emergency of the 2009 pandemic virus (Dharan et al. 2009, Eshaghi et al. 2009, Moscona 2009). The worldwide dissemination of A(H1N1)pdm09 influenza virus associated with the broad use of OST has demanded increasing surveillance of viral resistance to NA inhibitors. To our knowledge, data published from Brazil’s equatorial region are mainly clinical and epidemiological surveys (Barrau et al. 2012, Schuck-Paim et al. 2012, Pires Neto et al. 2013, Silva et al. 2014), without molecular or phylogenetic data. Taking into account the impact of influenza A(H1N1)pdm09, the unique characteristics of influenza viruses circulating worldwide and the lack of published data on molecular features of the virus from this equatorial region, we seek to investigate the presence of the H275Y change in NA gene and carry out the molecular characterisation of the HA gene from circulating influenza A(H1N1)pdm09 viruses in PE.
SUBJECTS, MATERIALS AND METHODS
Clinical samples and molecular diagnosis - Clinical specimens (combined nose and throat swabs or lung tissue fragments of deceased subjects) were collected from outpatients and hospitalised patients in Recife and its metropolitan area from April 2009-April 2010. These samples were collected in the scope of the Brazilian Influenza Surveillance Network within seven days of onset of influenza-like illness. In hospitalised cases where OST was used, the sample collection was performed before drug administration. After collection, both swabs and tissue fragments were placed in standard virus transport medium at the Pernambuco State Central Laboratory. The samples were then sent frozen to the Evandro Chagas Institute, in PA, for influenza A(H1N1)pdm09 detection by a real-time RT-PCR protocol developed by Centers for Disease Control and Prevention (USA) (WHO 2009b). The samples confirmed positive for influenza A(H1N1)pdm09 were sent to the Respiratory Viruses Reference Laboratory at Oswaldo Cruz Foundation, Rio de Janeiro, for further molecular characterisation. This study was approved by the Ethics in Research Committee of the Federal University of Pernambuco (protocol CEP/CCS/UFPE 219/10).
Sequencing of HA genes - The genetic characterisation of the HA gene from 30 samples from June 2009-April 2010 was performed by the Sanger method. In summary, the HA gene was amplified by RT-PCR using SuperScript III One-step RT-PCR with Platinum Taq-DNA Polymerase (Invitrogen, USA) following the protocol released by WHO (2009a). The amplicons were directly sequenced using Big Dye Terminator Cycle Sequencing Ready Reaction v.3.1 (Applied Biosystems, USA), purified (Motta et al. 2006) and run on an ABI 3130XL Capillary Automatic DNA Analyzer, as established by the manufacturer. Sequences of complete HA genes were edited using the Sequencher software, v.5.1 (Gene Codes, USA).
Phylogenetic analysis - The data set used for phylogenetic analysis was composed of the 30 HA sequences obtained in this study as well as other Brazilian and worldwide sequences available at GenBank (ncbi.nlm.nih.gov) collected over the period of this study. The complete dataset (5,471 sequences) was split in Brazilian (157, 2.87%) and non-Brazilian small ones. The CD-HIT software (weizhong-lab.ucsd.edu/cd-hit/) was used to select representative sequences of each data set, reducing then to a reasonable size. The identity cut-offs were 99.9% and 99.5% for Brazilian and non-Brazilian groups, respectively. The final data set contained 70 sequences, including two egg-isolated vaccine strains A/California/07/09 (FJ969540) and A/California/04/09 (FJ966082). The complete HA gene sequences were aligned using the CLUSTALW tool integrated within the MEGA 5.2 software (Tamura et al. 2011). A maximum-likelihood (ML) phylogenetic tree was inferred with the PhyML program (atcg-montpellier.fr/phyml/), using the best-fitting nucleotide substitution model, Hasegawa-Kishino-Yano plus gamma distribution among the sites, which was estimated by means of jModelTest v.2.1.1 software. ML reliability of branches was evaluated using approximate likelihood-ratio test and an interior branch cut-off value was ≥ 0.9. The tree was rooted with two vaccine representative sequences, which fell outside all clades, being used as a basis for comparison.
Pyrosequencing analysis of NA gene - A total of 118 influenza A(H1N1)pdm09 positive samples (65 hospitalised and 53 outpatients) were pyrosequenced in order to check for the presence of the resistance marker H275Y in the NA gene, according to a protocol developed previously (Deyde et al. 2010). After purification, the amplicons were analysed on the Pyromark Q-96 ID (Qiagen, Germany), using the single nucleotide polymorphism (SNP) mode. To carry out the quantitative analysis of H275Y mutation, we investigated the codon change CAC-TAC by pyrosequencing. All samples presenting less than 10% of “T” at the first position of the codon were considered wild type. Conversely, all values above 10% were considered as a mixture of wild and mutant types, with potentially reduced sensitivity to OST treatment.
RESULTS
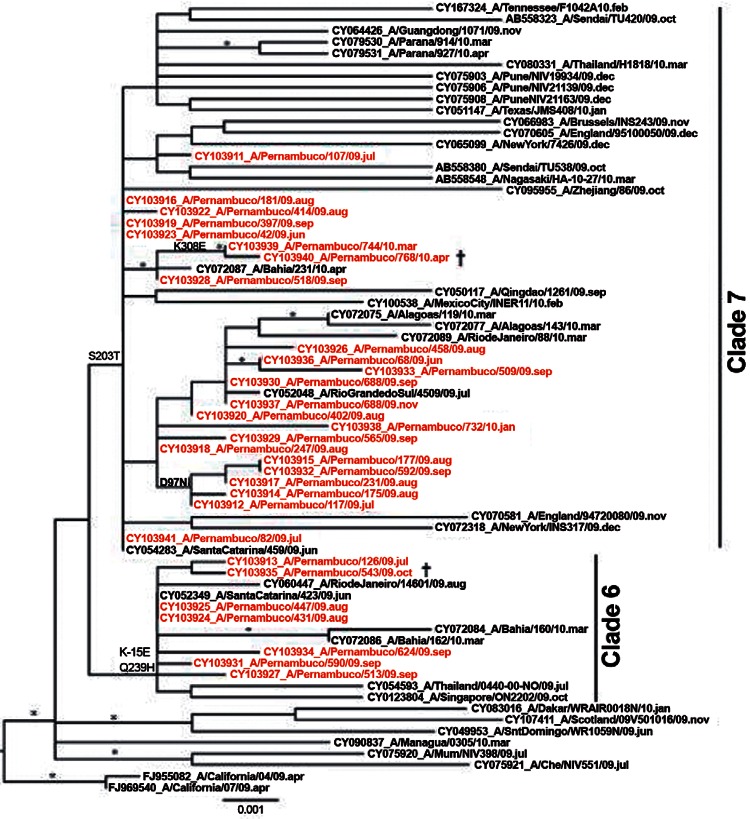
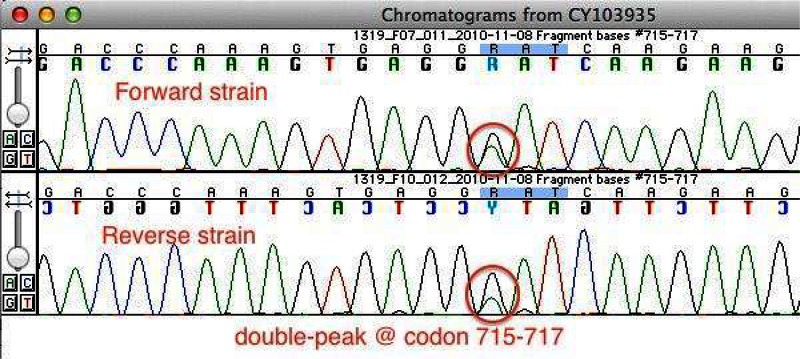
The details of the 30 samples sequenced in this study, namely strain name, GenBank accession, date and epidemiologic week (EW) of collection and patient type, are summarised in Table I. The samples sequenced covered the beginning of the regional circulation of the pandemic virus in PE in June 2009-April 2010. The period with the largest amount of sequences was August-September, between EW 31-38, accounting for 19 sequences. Twenty out of 30 HA sequences came from hospitalised patients, with two fatal cases. Theoretically translated amino acid sequences obtained from these patients held a total of 16 changes in comparison to A/California/07/2009. The changes stratified by patient type and their association to HA epitope regions are listed in Table II. The changes P83S and I321V were identified immediately after the introduction of the virus in the human population, being common to all samples outside phylogenetic clade 1 (Nelson et al. 2009). The second most frequent change was S203T, the signature residue of phylogenetic clade 7 (Potdar et al. 2010). This change was found in 23 samples (77%) collected from both outpatients or hospitalised subjects and only seven samples were similar to the vaccine prototype for this residue. Out of 30 samples, the Q293H change, characteristic of clade 6, was found in eight sequences in this study; three in outpatient subjects and five in samples from hospitalised patients. This change was combined with a K-15E mutation (in the HA signal peptide) in seven out of eight samples, the unique exception being A/Pernambuco/175/2009 (CY103914) from the outpatient group. Residue changes S84N, D97N and P182Q were found both in outpatient and hospitalised groups and the mutation K308E was identified in one sample from 2009 (CY103928) and three from 2010 (CY103938, CY103939 and CY103940), all from hospitalised patients. A further six changes were identified once or twice in this study, also in hospitalised or deceased patients, namely: G39E, S71F, D222N/G, N260K, Y351F and D472G. The sequences in this study were also analysed for the presence of putative HA virulence markers D222G (WHO 2009c) and Q293H (Glinsky 2010). A mixed viral population D222N/G, presenting as a double peak on the Sanger electropherogram (Supplementary data), was identified in sample A/Pernambuco/643/2009 (CY103935) from a deceased patient. On the other hand, the change Q239H was detected in eight samples, all from 2009, including a sample from a deceased pregnant woman bearing the mixture N/G at residue 222. The ML phylogenetic analysis of complete HA sequences from PE was carried out along with global representative sequences available in GenBank (Figure). PE sequences were divided in two major groups on the ML tree, represented by red branches and the most frequent amino acid changes are represented at the branches. Seven samples were allocated to clade 6 and 23 to clade 7. No chronological or geographic segregation was detected between PE and south-southeastern Brazilian samples, being clustered altogether in both clades. The pyrosequencing assay was performed in order to detect for the anti-viral resistance genetic marker H275Y of the NA gene. A total of 118 samples from hospitalised and outpatients patients positive for influenza A(H1N1)pdm09 by RT-PCR were assayed using pyrosequencing methodology and none presented a tyrosine at residue 275.
TABLE I. Influenza A(H1N1)pdm09 positive samples sequenced in this study.
| Strain identification | GenBank accession | EW collection | Collection date | Patient type |
|---|---|---|---|---|
| A/Pernambuco/42/2009 | CY103923 | 25 | 27 June 2009 | O |
| A/Pernambuco/66/2009 | CY103936 | 26 | 29 June 2009 | H |
| A/Pernambuco/82/2009 | CY103941 | 26 | 2 July 2009 | O |
| A/Pernambuco/107/2009 | CY103911 | 28 | 17 July 2009 | O |
| A/Pernambuco/117/2009 | CY103912 | 29 | 23 July 2009 | O |
| A/Pernambuco/126/2009 | CY103913 | 29 | 25 July 2009 | O |
| A/Pernambuco/175/2009 | CY103914 | 31 | 5 August 2009 | O |
| A/Pernambuco/177/2009 | CY103915 | 31 | 5 August 2009 | O |
| A/Pernambuco/181/2009 | CY103916 | 31 | 5 August 2009 | O |
| A/Pernambuco/231/2009 | CY103917 | 31 | 9 August 2009 | H |
| A/Pernambuco/247/2009 | CY103918 | 32 | 11 August 2009 | H |
| A/Pernambuco/402/2009 | CY103920 | 33 | 19 August 2009 | H |
| A/Pernambuco/397/2009 | CY103919 | 34 | 24 September 2009 | H |
| A/Pernambuco/414/2009 | CY103922 | 34 | 25 August 2009 | H |
| A/Pernambuco/431/2009 | CY103924 | 34 | 27 August 2009 | O |
| A/Pernambuco/447/2009 | CY103925 | 34 | 30 August 2009 | H |
| A/Pernambuco/458/2009 | CY103926 | 34 | 28 August 2009 | H |
| A/Pernambuco/513/2009 | CY103927 | 35 | 3 September 2009 | H |
| A/Pernambuco/518/2009 | CY103928 | 35 | 4 September 2009 | H |
| A/Pernambuco/565/2009 | CY103929 | 36 | 11 September 2009 | H |
| A/Pernambuco/567/2009 | CY103930 | 36 | 12 September 2009 | H |
| A/Pernambuco/590/2009 | CY103931 | 37 | 18 September 2009 | H |
| A/Pernambuco/592/2009 | CY103932 | 37 | 18 September 2009 | H |
| A/Pernambuco/609/2009 | CY103933 | 37 | 22 September 2009 | H |
| A/Pernambuco/624/2009 | CY103934 | 38 | 24 September 2009 | H |
| A/Pernambuco/643/2009 | CY103935 | 39 | 3 October 2009 | D |
| A/Pernambuco/688/2009 | CY103937 | 44 | 4 November 2009 | O |
| A/Pernambuco/732/2010 | CY103938 | 2 | 14 January 2010 | H |
| A/Pernambuco/744/2010 | CY103939 | 9 | 6 March 2010 | H |
| A/Pernambuco/768/2010 | CY103940 | 15 | 15 April 2010 | D |
D: deceased; EW: epidemiologic week; H: hospitalised; O: outpatient.
TABLE II. Mutations in complete neuraminidase gene segments associated with patient characteristics and antigenic sites.
| Amino acid changesa | HA epitope | Patient type (n)
|
Total (n) | ||
|---|---|---|---|---|---|
| Outpatient (n = 10) | Hospitalised (n = 18) | Deceased (n = 2) | |||
| K-15E | - | 2 | 4 | 1 | 7 |
| G39E | - | - | 1 | - | 1 |
| S71F | Cb | - | 1 | - | 1 |
| S74N | Cb | 1 | 2 | - | 3 |
| P83S | - | 10 | 18 | 2 | 30 |
| S84N | - | 1 | 1 | - | 2 |
| D97N | - | 3 | 2 | - | 5 |
| P182Q | - | 1 | 4 | - | 5 |
| S203T | Ca1 | 8 | 14 | 1 | 23 |
| D222N/Gb | Ca2 | - | - | 1 | 1 |
| N260K | - | - | 1 | - | 1 |
| Q293H | - | 3 | 4 | 1 | 8 |
| K308E | - | - | 3 | 1 | 4 |
| I321V | - | 10 | 18 | 2 | 30 |
| Y351Fc | - | - | - | 1 | 1 |
| D472Gc | - | - | 1 | 1 | 7 |
a: numbering according to H1 subtype without the signal peptide; b: N/G: a double peak (A/G) at the first base of the 222 codon; c: HA2 region; HA: haemagglutinin.
Maximum-likelihood (ML) phylogenetic tree of complete neuraminidase gene representing influenza A(H1N1)pdm09 viruses circulating in the state of Pernambuco (PE) from June 2009-April 2010. PE sequence names are in red to differentiate from other representative sequences from the equivalent period available in the GenBank database. ML reliability of branches was evaluated using an approximate likelihood-ratio test and the interior branch cut-off value was ≥ 0.9 indicated by an asterisk. All samples sequenced in this study are classified in clades 6 and 7 that co-circulate. Major associated amino acid changes are indicated in the branches using H1 numbering without signal peptide. The tree is rooted with egg-isolated vaccine strain A/California/07/09 (FJ969540). †: deceased patients.
DISCUSSION
It is noteworthy that whereas HA mutations S84N, D97N and P182Q were found in both outpatient and hospitalised groups, the change K308E was found only in severe cases. The K308E change was detected in one sample collected on 4 September 2009 from a hospitalised patient (CY103928) and thereafter in three other samples from the beginning of 2010, collected from two hospitalised (CY103938, CY103939) and a deceased patient (CY103940) (Table II). Based on sequences available in GenBank for this period, the K308E change first appeared in the Brazilian equatorial area and only in the next year in other tropical and temperate countries such as Singapore, England, Spain and USA. It is also worth noting that for Brazilian samples this change was not associated with V47I or E172K as observed in samples from the genetic group represented by A/Madrid/SO8171/10 identified in Spain (Ledesma et al. 2012). It remains to be seen if such changes are responsible for the severity of the cases and conversely if these changes were provoked by a longer period of viral replication in the lower respiratory tract. Scattered residue changes have been identified in severely immunosuppressed cancer patients and were associated to long shedding periods (Souza et al. 2010). In our study the patients were sampled once therefore it was not possible follow the evolution of the virus during the course of illness. Nevertheless, a greater diversity in the HA gene was distinguished in the hospitalised group when compared with the outpatient group, as observed by the amount of single mutations in hospitalised subject sequences.
In addition, we studied the possible association between the patient’s clinical status and the presence of HA virulence markers D222G and Q293H. A mixed viral population D222N/G (a double peak on the Sanger electropherogram) was identified in one sample only from this study. The amino acid residue 222 is located in the receptor binding site of HA and alterations in this site can affect the cellular tropism of the virus, rendering particles more prone to infecting the lower respiratory tract, thus, provoking severe disease. This hypothesis is in agreement with a fatal outcome from a pregnant woman that developed pneumonia with pulmonary condensation on chest radiography. The other putative virulence marker Q293H was detected in a similar proportion both in outpatient samples as well in hospitalised samples; therefore, we could not associate this mutation with more severe or fatal cases. Such findings corroborate the results previously reported from Brazilian and Indian samples (Lee et al. 2010, Potdar et al. 2010). Phylogenetic relationships between PE HA sequences, south-southeastern Brazilian and other worldwide isolates can be seen in Figure. PE sequences were classified in co-circulating clades 6 and 7, as observed in distinct regions of the world (Nelson et al. 2009). The majority of PE sequences are in clade 7, grouped together with other sequences from the same period from the states of Santa Catarina and Rio Grande do Sul, in southern Brazil, geographically distant from PE. Both clusters enclosed minor sub-clusters, most of them characterised by single amino acid changes, however, all samples were similar to the vaccine prototype, as observed by other authors (Barr et al. 2010, Ikonen et al. 2010). All samples in clade 6 presented the signature mutation Q293H, whereas this mutation was found only in two samples in clade 7: A/Pernambuco/175/09 (CY103914) and A/Pernambuco/414/09 (CY103922).
The H275Y marker was not detected in the 118 samples evaluated in this study. This finding is in agreement with previous data, that suggest a very low frequency of resistance in influenza A(H1N1)pdm09 in comparison to seasonal viruses (Souza et al. 2010, Yang et al. 2013) during the period the samples were collected. However, the expected levels of resistance detected in south-southeastern states in Brazil (Souza et al. 2013) and in Argentina (Barrero et al. 2011) since 2011, as well as the increasing number of resistant strains reported worldwide (Hurt et al. 2012, Souza et al. 2013) indicate the need for broader monitoring of resistance in equatorial areas of Brazil.
In this study, some important features of influenza A(H1N1)pdm09 HA and NA genes were described from samples collected in PE during the 2009-2010 biennium. There was no significant difference in PE HA sequences when compared with those from other Brazilian regions as samples from distinct regions were extensively grouped together in the phylogenetic tree. These regional sub-clusters, formed by samples collected between July/2009-April/2010, are indicative of co-circulation of lineages, as previously observed (Galiano et al. 2011). In addition, the NA resistance marker H275Y was not identified by pyrosequencing in any of the 118 samples tested, confirming the stability of the NA of the pandemic virus during the pandemic year. However, continuous monitoring of viral evolution and the emergence of OST resistance are pivotal for worldwide influenza surveillance and the findings depicted here contribute to a better understanding of the genetic characteristics of the influenza A(H1N1)pdm09 virus that circulated during the pandemic period in the Northeast Brazil.
Supplementary data. Sanger sequencing electropherogram showing the double peak at the first base of codon 715-717 of the neuraminidase gene resulting in a H275Y mutation. This mixed virus population was identified only in patient CY103935 and the presence of A/G peaks was confirmed both in sense and anti-sense strains.
Footnotes
Financial support: DECIT/MoH, CNPq
REFERENCES
- Barr IG, Cui L, Komadina N, Lee RT, Lin RT, Deng Y, Caldwell N, Shaw R, Maurer-Stroh S. A new pandemic influenza A(H1N1) genetic variant predominated in the winter 2010 influenza season in Australia, New Zealand and Singapore. Euro Surveill. 2010;15: doi: 10.2807/ese.15.42.19692-en. [DOI] [PubMed] [Google Scholar]
- Barrau M, Larrieu S, Cassadou S, Chappert JL, Dussart P, Najioullah F, Matheus S, Renner J, Gasc C, Quenel P, Ledrans M. Hospitalized cases of influenza A(H1N1)pdm09 in the French territories of the Americas, July 2009-March 2010. Rev Panam Salud Publica. 2012;32:124–130. doi: 10.1590/s1020-49892012000800006. [DOI] [PubMed] [Google Scholar]
- Barrero PR, Viegas M, Valinotto LE, Mistchenko AS. Genetic and phylogenetic analyses of influenza A(H1N1)pdm virus in Buenos Aires, Argentina. J Virol. 2011;85:1058–1066. doi: 10.1128/JVI.00936-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deyde VM, Sheu TG, Trujillo AA, Okomo-Adhiambo M, Garten R, Klimov AI, Gubareva LV. Detection of molecular markers of drug resistance in 2009 pandemic influenza A(H1N1) viruses by pyrosequencing. Antimicrob Agents Chemother. 2010;54:1102–1110. doi: 10.1128/AAC.01417-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dharan NJ, Gubareva LV, Meyer JJ, Okomo-Adhiambo M, McClinton RC, Marshall SA, St George K, Epperson S, Brammer L, Klimov AI, Bresee JS, Fry AM, Oseltamivir-Resistance Working G Infections with oseltamivir-resistant influenza A(H1N1) virus in the United States. JAMA. 2009;301:1034–1041. doi: 10.1001/jama.2009.294. [DOI] [PubMed] [Google Scholar]
- Eshaghi A, Bolotin S, Burton L, Low DE, Mazzulli T, Drews SJ. Genetic microheterogeneity of emerging H275Y influenza virus A(H1N1) in Toronto, Ontario, Canada from the 2007-2008 respiratory season. J Clin Virol. 2009;45:142–145. doi: 10.1016/j.jcv.2009.04.010. [DOI] [PubMed] [Google Scholar]
- Galiano M, Agapow PM, Thompson C, Platt S, Underwood A, Ellis J, Myers R, Green J, Zambon M. Evolutionary pathways of the pandemic influenza A(H1N1) 2009 in the UK. PLoS ONE. 2011;6: doi: 10.1371/journal.pone.0023779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garten RJ, Davis CT, Russell CA, Shu B, Lindstrom S, Balish A, Sessions WM, Xu X, Skepner E, Deyde V, Okomo-Adhiambo M, Gubareva L, Barnes J, Smith CB, Emery SL, Hillman MJ, Rivailler P, Smagala J, Graaf M, Burke DF, Fouchier RA, Pappas C, Alpuche-Aranda CM, Lopez-Gatell H, Olivera H, Lopez I, Myers CA, Faix D, Blair PJ, Yu C, Keene KM, Dotson PD, Jr, Boxrud D, Sambol AR, Abid SH, St George K, Bannerman T, Moore AL, Stringer DJ, Blevins P, Demmler-Harrison GJ, Ginsberg M, Kriner P, Waterman S, Smole S, Guevara HF, Belongia EA, Clark PA, Beatrice ST, Donis R, Katz J, Finelli L, Bridges CB, Shaw M, Jernigan DB, Uyeki TM, Smith DJ, Klimov AI, Cox NJ. Antigenic and genetic characteristics of swine-origin 2009 A(H1N1) influenza viruses circulating in humans. Science. 2009;325:197–201. doi: 10.1126/science.1176225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghedin E, Laplante J, DePasse J, Wentworth DE, Santos RP, Lepow ML, Porter J, Stellrecht K, Lin X, Operario D, Griesemer S, Fitch A, Halpin RA, Stockwell TB, Spiro DJ, Holmes EC, St George K. Deep sequencing reveals mixed infection with 2009 pandemic influenza A(H1N1) virus strains and the emergence of oseltamivir resistance. J Infect Dis. 2011;203:168–174. doi: 10.1093/infdis/jiq040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glinsky GV. Genomic analysis of pandemic (H1N1) 2009 reveals association of increasing disease severity with emergence of novel hemagglutinin mutations. Cell Cycle. 2010;9:958–970. doi: 10.4161/cc.9.5.10913. [DOI] [PubMed] [Google Scholar]
- Hurt AC, Hardie K, Wilson NJ, Deng YM, Osbourn M, Leang SK, Lee RT, Iannello P, Gehrig N, Shaw R, Wark P, Caldwell N, Givney RC, Xue L, Maurer-Stroh S, Dwyer DE, Wang B, Smith DW, Levy A, Booy R, Dixit R, Merritt T, Kelso A, Dalton C, Durrheim D, Barr IG. Characteristics of a widespread community cluster of H275Y oseltamivir-resistant A(H1N1)pdm09 influenza in Australia. J Infect Dis. 2012;206:148–157. doi: 10.1093/infdis/jis337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikonen N, Haanpaa M, Ronkko E, Lyytikainen O, Kuusi M, Ruutu P, Kallio-Kokko H, Mannonen L, Lappalainen M, Ziegler T, Julkunen I. Genetic diversity of the 2009 pandemic influenza A(H1N1) viruses in Finland. PLoS ONE. 2010;5: doi: 10.1371/journal.pone.0013329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilander A, Rykkvin R, Dudman SG, Hungnes O. Observed association between the HA1 mutation D222G in the 2009 pandemic influenza A(H1N1) virus and severe clinical outcome, Norway 2009-2010. Euro Surveill. 2010;15: doi: 10.2807/ese.15.09.19498-en. [DOI] [PubMed] [Google Scholar]
- Ledesma J, Pozo F, Perez Ruiz M, Navarro JM, Pineiro L, Montes M, Perez Castro S, Suarez Fernandez J, Garcia Costa J, Fernandez M, Galan JC, Cuevas MT, Casas I, Perez Brena P. Substitutions in position 222 of haemagglutinin of pandemic influenza A(H1N1) 2009 viruses in Spain. J Clin Virol. 2011;51:75–78. doi: 10.1016/j.jcv.2011.01.020. [DOI] [PubMed] [Google Scholar]
- Ledesma J, Pozo F, Reina G, Blasco M, Rodriguez G, Montes M, Lopez-Miragaya I, Salvador C, Reina J, Ortiz de Lejarazu R, Egido P, Lopez Barba J, Delgado C, Cuevas MT, Casas I, Spanish Influenza Surveillance S Genetic diversity of influenza A(H1N1) 2009 virus circulating during the season 2010-2011 in Spain. J Clin Virol. 2012;53:16–21. doi: 10.1016/j.jcv.2011.09.032. [DOI] [PubMed] [Google Scholar]
- Lee RT, Santos CL, Paiva TM, Cui L, Sirota FL, Eisenhaber F, Maurer-Stroh S. All that glitters is not gold - founder effects complicate associations of flu mutations to disease severity. 297Virol J. 2010;7 doi: 10.1186/1743-422X-7-297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y, Childs RA, Matrosovich T, Wharton S, Palma AS, Chai W, Daniels R, Gregory V, Uhlendorff J, Kiso M, Klenk HD, Hay A, Feizi T, Matrosovich M. Altered receptor specificity and cell tropism of D222G hemagglutinin mutants isolated from fatal cases of pandemic A(H1N1) 2009 influenza virus. J Virol. 2010;84:12069–12074. doi: 10.1128/JVI.01639-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moscona A. Global transmission of oseltamivir-resistant influenza. N Engl J Med. 2009;360:953–956. doi: 10.1056/NEJMp0900648. [DOI] [PubMed] [Google Scholar]
- Motta FC, Siqueira MM, Lugon AK, Straliotto SM, Fernandes SB, Krawczuk MM. The reappearance of Victoria lineage influenza B virus in Brazil, antigenic and molecular analysis. J Clin Virol. 2006;36:208–214. doi: 10.1016/j.jcv.2006.03.008. [DOI] [PubMed] [Google Scholar]
- Nelson M, Spiro D, Wentworth D, Beck E, Fan J, Ghedin E, Halpin R, Bera J, Hine E, Proudfoot K, Stockwell T, Lin X, Griesemer S, Kumar S, Bose M, Viboud C, Holmes E, Henrickson K. The early diversification of influenza A/H1N1pdm. RRN1126PLoS Curr. 2009;1 doi: 10.1371/currents.RRN1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pires RJ, Neto, Lemos DR, Cavalcanti LP, Ramos AN, Junior, Alencar CH, Facanha MC, Barroso MI, Vilar DC, Fonseca MD., Neto Pandemic influenza A(H1N1) 2009: epidemiological analysis of cases in a tropical/semi-arid region of Brazil. Rev Soc Bras Med Trop. 2013;46:141–146. doi: 10.1590/0037-8682-0016-2012. [DOI] [PubMed] [Google Scholar]
- Potdar VA, Chadha MS, Jadhav SM, Mullick J, Cherian SS, Mishra AC. Genetic characterization of the influenza A pandemic (H1N1) 2009 virus isolates from India. PLoS ONE. 2010;5: doi: 10.1371/journal.pone.0009693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resende PC, Motta FC, Oliveira ML, Gregianini TS, Fernandes SB, Cury AL, do Carmo DRM, Souza TM, Siqueira MM. Polymorphisms at residue 222 of the hemagglutinin of pandemic influenza A(H1N1)pdm09: association of quasi-species to morbidity and mortality in different risk categories. PLoS ONE. 2014;9: doi: 10.1371/journal.pone.0092789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuck-Paim C, Viboud C, Simonsen L, Miller MA, Moura FE, Fernandes RM, Carvalho ML, Alonso WJ. Were equatorial regions less affected by the 2009 influenza pandemic? The Brazilian experience. PLoS ONE. 2012;7: doi: 10.1371/journal.pone.0041918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva RC, Siqueira MAM, Martins Netto E, Bastos JS, Nascimento-Carvalho CM, Vilas-Boas AL, Bouzas ML, Motta FC, Brites C. Epidemiological aspects of influenza A related to climatic conditions during and after a pandemic period in the city of Salvador, northeastern Brazil. Mem Inst Oswaldo Cruz. 2014;109:229–235. doi: 10.1590/0074-0276140273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Souza TM, Resende PC, Fintelman-Rodrigues N, Gregianini TS, Ikuta N, Fernandes SB, Cury AL, Rosa MC, Siqueira MM. Detection of oseltamivir-resistant pandemic influenza A(H1N1)pdm2009 in Brazil: can community transmission be ruled out? PloS ONE. 2013;8: doi: 10.1371/journal.pone.0080081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Souza TM, Salluh JI, Bozza FA, Mesquita M, Soares M, Motta FC, Pitrowsky MT, Oliveira ML, Mishin VP, Gubareva LV, Whitney A, Rocco SA, Gonçalves VM, Marques VP, Velasco E, Siqueira MM. H1N1pdm influenza infection in hospitalized cancer patients: clinical evolution and viral analysis. PLoS ONE. 2010;5: doi: 10.1371/journal.pone.0014158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun S, Wang Q, Zhao F, Chen W, Li Z. Glycosylation site alteration in the evolution of influenza A(H1N1) viruses. PLoS ONE. 2011;6: doi: 10.1371/journal.pone.0022844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamura K, Peterson D, Peterson N, Stecher G, Nei M, Kumar S. MEGA5: molecular evolutionary genetics analysis using maximum likelihood, evolutionary distance and maximum parsimony methods. Mol Biol Evol. 2011;28:2731–2739. doi: 10.1093/molbev/msr121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner R, Matrosovich M, Klenk HD. Functional balance between haemagglutinin and neuraminidase in influenza virus infections. Rev Med Virol. 2002;12:159–166. doi: 10.1002/rmv.352. [DOI] [PubMed] [Google Scholar]
- Wedde M, Wahlisch S, Wolff T, Schweiger B. Predominance of HA-222D/G polymorphism in influenza A(H1N1)pdm09 viruses associated with fatal and severe outcomes recently circulating in Germany. PLoS ONE. 2013;8: doi: 10.1371/journal.pone.0057059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO - World Health Organization WHO CDC protocol for influenza A(H1N1) genome sequencing. 2009a who.int/csr/resources/publications/swineflu/GenomePrimers_20090512.pdf
- WHO - World Health Organization WHO CDC protocol of real-time RT-PCR for influenza A(H1N1) 2009. 2009b who.int/csr/resources/publications/swineflu/CDCRealtimeRTPCR_SwineH1Assay2009_20090430.pdf
- WHO - World Health Organization Preliminary review of D222G amino acid substitution in the haemagglutinin of pandemic influenza A(H1N1) 2009 viruses. 2009c who.int/csr/resources/publications/swineflu/h1n1_d222g/en/ [PubMed]
- WHO - World Health Organization WHO pandemic (H1N1) 2009. 2010 who.int/csr/don/2010_08_06/en/index.html
- Yang JR, Huang YP, Chang FY, Hsu LC, Huang HY, Pan YT, Lin YC, Wu HS, Liu MT. Characterization of oseltamivir-resistant influenza A(H1N1)pdm09 viruses in Taiwan in 2009-2011. J Med Virol. 2013;85:379–387. doi: 10.1002/jmv.23482. [DOI] [PubMed] [Google Scholar]