When specially trained pharmacy technicians took patients’ medication histories in a hospital emergency department, the histories they conducted were accurate 88% of the time compared with 57% of those conducted by nurses, who had other duties.
Abstract
Purpose:
To evaluate the percentage, frequency, and types of medication history errors made by pharmacy technicians compared with nurses in the emergency department (ED) to determine if patient safety and care can be improved while reducing nurses’ workloads.
Methods:
Medication history errors were evaluated in a pre-post study comparing a historical control group (nurses) prior to the implementation of a pharmacy technician program in the ED to a prospective cohort group (pharmacy technicians). Two certified pharmacy technicians were trained by the post-graduate year one (PGY1) pharmacy practice resident to conduct medication history interviews in a systematic fashion, with outside resources (i.e., assisted living facility, pharmacy, physician’s office, or family members) being consulted if any portion of the medication history was unclear or lacking information. The primary outcome compared the percentage of patients with accurate medication histories in each group. Secondary outcomes included differences between groups regarding total medication errors, types of errors, documentation of patient allergies and drug reactions, and documentation of last administration times for high-risk anticoagulant/antiplatelet medications. Accuracy was determined by reviewing each documented medication history for identifiable errors, including review of electronic generated prescriptions within the hospital system as well as physician notes or histories documented on the same day (for potential discrepancies). This review was performed by the pharmacy resident. The categories of errors included a drug omission, a drug commission, an incorrect or missing drug, an incorrect or missing dose, or an incorrect or missing frequency. Anonymous surveys were distributed to ED nurses to assess their feedback on the new medication reconciliation program using pharmacy technicians.
Results:
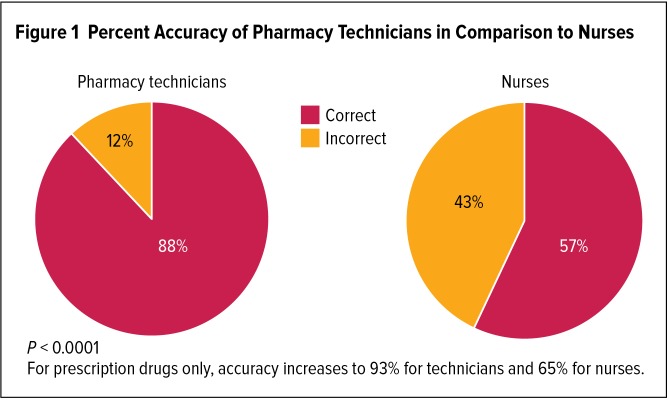
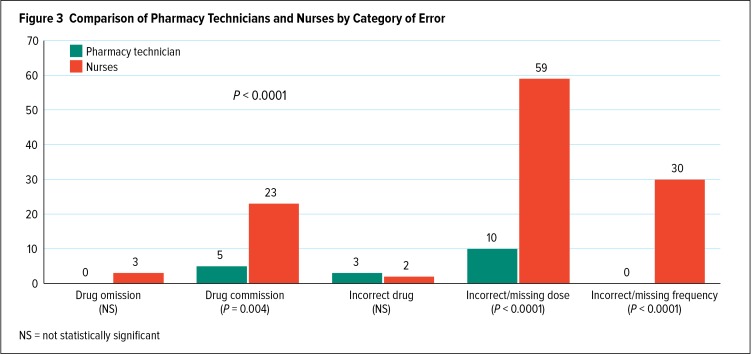
A total of 300 medication histories from the ED were evaluated (150 in each group). Medication histories conducted by pharmacy technicians were accurate 88% of the time compared with 57% of those conducted by nurses (P < 0.0001). Nineteen errors (1.1%) were made by pharmacy technicians versus 117 (8.3%) by nurses (relative risk [RR], 7.5; P < 0.0001). The most common type of error was an incorrect or missing dose (10 versus 59, P < 0.001), followed by an incorrect or missing frequency (0 versus 30, P < 0.0001), and a drug commission (5 versus 23, P = 0.004). There were no differences between groups regarding the documentation of patient allergies. Documentation rates of high-risk anticoagulant and antiplatelet administration times were greater for pharmacy technicians than for nurses (76% versus 13%, P < 0.001).
Conclusion:
This study demonstrates that trained pharmacy technicians can assist prescribers and nurses by improving the accuracy of medication histories obtained in the ED.
BACKGROUND
ADEs (adverse drug events, or injuries due to drug-related interventions) occur far too often in our society and, in many instances, are preventable.1 For example, a 2006 report brief from the Institute of Medicine concluded that at least 1.5 million preventable ADEs occur each year in the U.S.2 Frequently, such errors arise during medication reconciliation processes, where transitions in patient care often involve multiple personnel, leading to a noteworthy potential for discrepancies. For instance, more than 40% of medication errors are believed to result from inadequate reconciliation in handoffs during admission, transfer, and discharge of patients. Of these errors, approximately 20% are believed to result in patient harm.3
Other research found that each preventable ADE that took place in a hospital added approximately $8,750 to the cost of the hospital stay.2 Furthermore, a systematic review of 22 studies (involving more than 3,500 patients) found errors in medication histories for up to 67% of patients at the time of hospital admission. With the inclusion of patient allergies in this assessment, the incidence of errors rose to as much as 95% of patients, and up to 39% of errors had the potential to cause moderate or severe patient discomfort or deterioration in the patient’s condition.4 Similarly, the “Medications at Transitions and Clinical Handoffs” (MATCH) study found medication errors in more than one-third of patients studied; 85% of the errors originated with medication histories.5
Acquisition of a patient’s medication history is the first step in the medication reconciliation process, in which there is direct comparison of the medications that a patient was previously taking to the current medication regimen and any discrepancies or problems are resolved. A comprehensive, accurate medication history is necessary for the practitioner’s proper evaluation and clinical assessment of the patient, as medication histories provide insight into potential medical problems and facilitate the continuity of treatment. Although it is an integral component of patient care, obtaining an accurate medication history is often challenging. Potential barriers include patient confusion or impaired memory, clinical status (i.e., fatigue, decreased alertness, distraction due to pain), outdated information in hospital records, polypharmacy use, limited access to patient records, time constraints, and language or cultural differences. In some instances, it is necessary to consult outside resources, such as a patient’s pharmacy or assisted living facility, to attain accurate and comprehensive information.
Traditionally, nurses and physicians have collected patient medication histories. However, their ability to obtain complete and accurate records may be limited by heavy workloads and increasing patient-care responsibilities. Physicians often ask what medications a patient is taking during their initial assessment, but this time period is limited and a small component of their documentation process. Nurses are usually assigned to multiple patients at a time and are often preoccupied with direct patient-care activities (including patient assessments and documentation, medication administration, taking physician orders, and reporting to other health care practitioners during transitions in patient care).
Recent literature demonstrates clear advantages in utilizing skilled pharmacy technicians to complete medication histories. Additionally, pharmacy technicians can be employed to devote the majority of their efforts to documenting accurate and comprehensive information. Well-trained pharmacy technicians are proficient in communication techniques and problem-solving abilities, and they possess a fundamental understanding of medication use. To illustrate, a Dutch study of preoperative surgical patients found a significant decrease in the number of medication discrepancies after medication reconciliation was performed by a pharmacy technician in comparison to an anesthesiologist (a 5% error rate by pharmacy technicians versus 38% by anesthesiologists; RR, 0.29; 95% confidence interval [CI], 0.12–0.71).6 In another study, more than half of the medication histories recorded by physicians differed from those obtained by pharmacy staff, with a total of 5,963 discrepancies in 3,594 medication histories.7 Furthermore, results of a Canadian study indicate that pharmacy technicians are able to obtain medication histories in the ED with as much accuracy and completeness as pharmacists (the differences between groups for prescription and over-the-counter [OTC] medications were P = 0.47 and P = 0.77, respectively).8
The Society of Hospital Medicine has called attention to the need for research to identify best medication-reconciliation practices, and the goals of the American Society of Health-System Pharmacists (ASHP) include incorporating pharmacy involvement in managing the acquisition of medication histories (part of its 2015 Initiative) and expanding the responsibilities of the pharmacy technician (part of its Pharmacy Practice Model Initiative).9,10,11 Additionally, the Joint Commission includes risk points of medication reconciliation in its National Patient Safety Goals.12 In this study, we evaluated medication history errors before and after implementation of a pharmacy-technician-based medication reconciliation program in the ED.
METHODS
Study Setting
This study was conducted between November 2011 and February 2012 at Morton Plant Hospital in Clearwater, Florida, after receiving approval from its institutional review board. Morton Plant Hospital is a 687-bed, community-owned facility with an average daily ED census of 140 to 150 persons. Approximately 60% of the hospital’s admissions come directly from the ED.
Inclusion and Exclusion Criteria
Patients were included in the study if they were more than 18 years old, were admitted to the hospital directly from the ED, took at least three medications upon arrival (to minimize variations between groups, since the pharmacy technicians were asked to complete medication histories for patients with several medications), and presented to the ED between 1 p.m. and 9:30 p.m. (coinciding with the hours of the ED pharmacy technician). Patients were excluded if they were incapable of providing a medication history. A computer-generated admissions report was used to identify and select eligible patients during the specified period. Patients were assigned a numerical identifier for data collection to protect anonymity.
Study Design
This was a pre-post study design comparing a historical control group (nurses) prior to the implementation of a pharmacy technician program in the ED to a prospective cohort group (pharmacy technicians). Two certified pharmacy technicians were hired to participate in the ED medication reconciliation process. They were selected based on their ability to communicate effectively, desire to interact with patients, problem-solving abilities, and display of initiative. They received on-site training by the PGY1 pharmacy practice resident over a period of two weeks. First, the technicians were given a series of educational lectures (developed in-house) pertaining to patient communication, high-risk medications, and the medication reconciliation process. Subsequently, they were taught a systematic approach to collecting medication histories consisting of a patient interview, utilization of a checklist, asking prompting questions, reviewing and updating old records, and contacting the patient’s pharmacy (or other sources such as the physician, nursing home, or family) if there were any uncertainties. The technicians were also trained to update patient allergies (with associated reactions) and to document the last date and time that each medication was administered (if known). They practiced using the computer software program on a “dummy patient” before working in the ED. The pharmacy technicians then worked directly with the pharmacy resident to collect patient medication histories in the ED until they felt prepared to work on their own (approximately one week). A pharmacy technician was then assigned to work in the ED from 1 p.m. to 9:30 p.m. (including a 30-minute break), seven days a week. The pharmacy technicians worked with the ED staff without any direct supervision by a pharmacist.
Data Collection/Objectives
The PGY1 pharmacy resident collected data by reviewing each electronically documented medication history for identifiable errors. Electronic prescriptions generated by the health care system and physician notations made on the same day were reviewed for potential discrepancies. The primary objective was to determine any differences in the percentage of patients with accurate medication histories prepared by nurses compared with pharmacy technicians. Secondary objectives included any differences in the total number of medication errors, types of medication errors, documentation of patient allergies and reactions, and documentation of the last administration date and time of high-risk anticoagulant and antiplatelet medications. Accuracy was determined and quantified by using only those errors that were discoverable using electronic documented information.
Baseline characteristics were recorded for both groups, and medication history errors were classified into the following types: A drug omission (failure to document a drug that the patient is taking), a drug commission (a notation adding a drug that the patient is not actually taking), an incorrect or missing drug, an incorrect or missing dose, and/or an incorrect or missing frequency. Nonprescription vitamins and herbal preparations were excluded from all analyses because patients are often unaware of the dose(s), it is not feasible to clarify this information, and these substances are generally held during the hospital stay if not part of the hospital formulary. Finally, optional and anonymous surveys were distributed to nurses in the ED to determine their perspectives and obtain feedback regarding this interventional program. A one-month lapse occurred between the pre- and post-intervention data collection periods to allow for adequate training of pharmacy technicians and implementation of the new program.
Statistical Analysis
Sample-size considerations were determined using previously published literature and a pilot study conducted at Morton Plant Hospital.13–15 We estimated that a total sample size of 102 patients would be necessary to reach a power of 90% with an anticipated effect size of 30% (α = 0.05) (PS Version 3.0, Vanderbilt University, Nashville, Tennessee). For statistical testing methods, we used chi square analyses for all nominal data and student’s t-tests for continuous or discrete data. Two-proportion analyses were run on continuous or discrete data insufficient to perform student’s t-tests (Minitab 16 Plus, Minitab, Inc., State College, Pennsylvania). All descriptive statistics were calculated using Microsoft Windows Excel (version 2007).
RESULTS
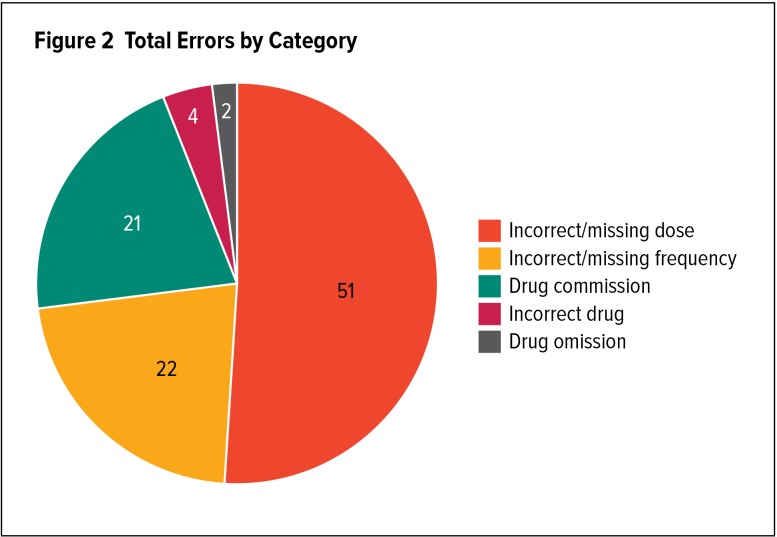
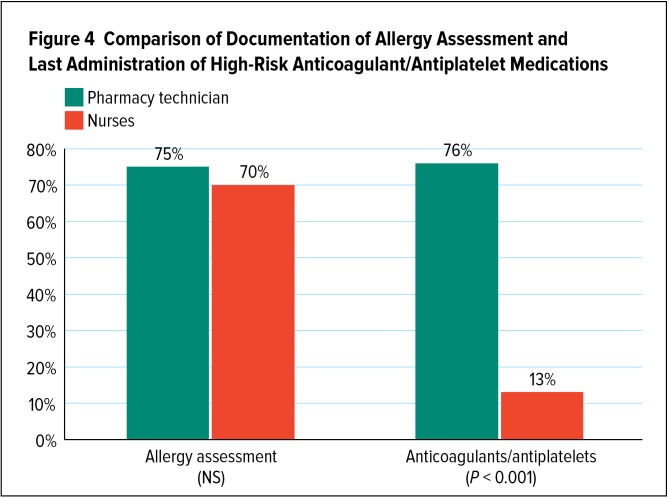
A total of 300 medication histories (150 in each group) were included in the study. Baseline characteristics were similar between groups, with the exception of the pharmacy technician group having a greater average number of medications per patient (P = 0.003) and comorbidities per patient (P = 0.001) (Table 1). For the primary outcome, medication histories conducted by pharmacy technicians were accurate without any identifiable errors 88% of the time compared with 57% of medication histories conducted by nurses (P < 0.0001) (Figure 1). We also conducted a subanalysis excluding all OTC medication errors, and accuracy increased to 93% versus 65%, respectively (P < 0.0001). Nineteen errors out of 1,727 entries (1.1%) were made by pharmacy technicians compared with 117 errors out of 1,410 entries (8.3%) by nurses (RR, 7.5; P < 0.0001) (Table 2). For both groups, the most common category of error was an incorrect or missing dose (51%), followed by an incorrect or missing frequency (22%), drug commission (21%), incorrect or missing drug (4%), and drug omission (2%) (Figure 2, Table 3). When comparing the categories of errors between pharmacy technicians and nurses, there was a significant difference for the three most common types of errors: An incorrect or missing dose (10 versus 59, P < 0.0001), incorrect or missing frequency (0 versus 30, P < 0.0001), and drug commission (5 versus 23, P = 0.004) (Figure 3). There were no differences between groups with regard to the documentation of patient allergies and reactions (P = 0.366). High-risk anticoagulant and antiplatelet administration times were documented 76% of the time by pharmacy technicians compared with 13% of the time by nurses (P < 0.001) (Figure 4).
Table 1.
Baseline Characteristics
| Technician (N = 150) | Nurse (N = 150) | Statistical Significance | |
|---|---|---|---|
| Male | 62 | 61 | NS (P = 0.928) |
| Female | 88 | 89 | NS (P = 0.940) |
| Age (mean ± SD) | 70 ± 17.32 | 67 ± 19.38 | NS (P = 0.144) |
| Comorbidities (mean ± SD) | 6.1 ± 3.49 | 4.8 ± 2.58 | Difference = 1.22 95% CI (0.522–1.918) (P = 0.001) |
| Medications* (mean ± SD) | 12.3 ± 6.16 | 10.3 ± 5.58 | Difference = 2.04 95% CI (0.704–3.376)(P = 0.003) |
CI = confidence interval; NS = not statistically significant; SD = standard deviation
Mean number of patient medications at time of ED presentation
Figure 1.
Percent Accuracy of Pharmacy Technicians in Comparison to Nurses
P < 0.0001
For prescription drugs only, accuracy increases to 93% for technicians and 65% for nurses.
Table 2.
Total Errors by Group
| Technician (N = 150) | Nurse (N = 150) | Statistical Significance | |
|---|---|---|---|
| Total errors (%)* | 19 / 1,727(1.1%) | 117 / 1,410 (8.3%) | Difference = −0.07 (7%) 95% CI, −0.086 to −0.055 P < 0.0001 |
Percent error per medication entry
Figure 2.
Total Errors by Category
Table 3.
Examples of Errors by Category
| Incorrect/missing dose |
|
| Incorrect/missing frequency |
|
| Incorrect/missing drug | • “Muscle relaxant, new heart medicine” (vague description, drugs not identified) |
| Drug commission |
|
| Drug omission |
|
MD = physician
Figure 3.
Comparison of Pharmacy Technicians and Nurses by Category of Error
NS = not statistically significant
Figure 4.
Comparison of Documentation of Allergy Assessment and Last Administration of High-Risk Anticoagulant/Antiplatelet Medications
Twenty-two ED nurses responded to our first anonymous survey, which included the following results: 95% felt that they did not have enough time to complete accurate medication histories and 90% believed that medication reconciliation tasks interfere with their ability to perform other nursing duties. Three months after our program was initiated, a second anonymous survey was administered to 27 ED nurses and found the following: 100% of respondents felt positive about having pharmacy technicians conduct medication histories in the ED, 85% definitely had additional time to tend to their patients, and 100% felt they would benefit if the pharmacy technicians conducted all of the medication histories in the ED.
DISCUSSION
Prior to the initiation of this study, we anticipated that this interventional program could improve the accuracy of patient information that was collected during the medication history process. Subsequently, the ability for health care providers to make appropriate assessments and interventions would be enhanced, and the incidence of adverse drug events should decrease. The results of this study support our initial goals, with findings of significant improvements in documentation accuracy through utilization of trained pharmacy technicians whose primary job responsibility is obtaining thorough medication histories in the ED.
There are several notable limitations to our study. First, the design was not randomized and did not contain a prospective control group, and the data was collected unblinded by investigators. We also assumed that medication histories acquired by skilled pharmacy technicians using standardized procedures would lead to an accurate assessment of a patient’s current medication regimen. In support of this assumption, previous literature indicates that investigation of a patient’s documented medication history by a pharmacy technician results in increased accuracy, and trained pharmacy technicians are capable of obtaining medication histories with as much accuracy as pharmacists.6,8
Baseline characteristics were similar between groups, with the exception of the pharmacy technician group having a greater average number of medications and comorbidities per patient. As a result, we should expect the technician group to make more errors. However, despite having more complicated patients, the accuracy of pharmacy technicians exceeded that of nurses by 31 percentage points, with medication history entries by nurses being 7.5 times more likely to contain an error. We might also expect a greater number of errors to occur during our busiest season, the winter months (corresponding to the period of data collection for our interventional technician group).
There is also the possibility of potential errors in both groups that may have been undiscoverable during our study, since we only included errors that could be ascertained through documented electronic records. We attempted to minimize undiscoverable errors in the pharmacy technician group by having them follow precise and thorough methods to obtain comprehensive medication history information. In contrast, the nurses were trained previously, and their methods of collecting medication histories may have varied. They did not always use a checklist, and it is not known if they updated old records, interviewed the patient, or contacted outside resources. Thus, we would expect that the undiscovered errors made by nurses might be greater in comparison to the technician group.
Lastly, our facility is a nontrauma hospital with a significant elderly population—therefore the results cannot necessarily be generalized to all institutions or patient populations.
Medication history errors may occur for a variety of reasons during the documentation process, with the most notable being limitations due to time constraints or heavy workloads (prohibiting additional clarification steps). Errors may also occur due to incorrect interpretation or transcription (i.e., mispronunciation by the patient or improper spelling on a written drug list leading to documentation of the wrong drug, dose, and/or frequency). In addition, inadequate information may be provided without further inquiry, or the documenter may have limited familiarity with drug products, dosages, and use of available pharmacological resources.
We did not perform a cost analysis in our study, although we expect that there would be significant cost savings as a result of avoiding potential adverse medication errors or events. Such errors could potentially lengthen the patient stay or even contribute to future hospitalizations (i.e., a prior study found drug-related adverse events to be a cause of more than one in nine ED visits).16 Our study does illustrate that it is reasonable to hire and train pharmacy technicians to perform medication histories in the ED, rather than using pharmacists, which allows a significant cost savings to the department and institution. Further studies are warranted to investigate the potential cost savings of using pharmacist technicians to conduct medication histories.
During the training period of the pharmacy technician group, we emphasized the importance of obtaining and documenting patient allergies (including reactions) and the last date and time that each medication was taken (if it is feasible to obtain this information). It is important and helpful to the practitioner and health care team to obtain a record of patient allergy information— primarily to prevent a potential adverse drug event, but also to ascertain the severity of reaction(s) and to determine if a true allergy is present (versus an intolerance or side effect). This helps to promote safe medication prescribing practices, including use of the most appropriate antibiotic(s) for site and severity of infection.
It is also prudent to determine the date and approximate time that each medication was last administered (if known). This helps to avoid patients either missing a dose or accidentally receiving an extra dose. Furthermore, computer software programs used in institutional settings often default to the next “standard administration time,” which doesn’t take into account whether the patient has recently received a dose. If it is known when the next dose is due, then the practitioner or pharmacist can appropriately enter the timing of the next dose. Having knowledge of the last approximate time that a medication was administered may also help to prevent an adverse drug event. This is especially important for medications pertinent to preventing a disease relapse (such as epilepsy or organ rejection) or other high-risk medications such as anticoagulants and antiplatelets. For example, if it were necessary to have an emergency surgical procedure and it had been too soon since the last anticoagulant dose was administered, a patient could be at risk for severe or life-threatening bleeding.
During our study, we found a considerable difference between groups when reviewing the last administration dates and times for high-risk anticoagulant and antiplatelet medications. This information was documented 76% of the time by the technician group and only 13% of the time by nurses. No differences were found between groups for the documentation of patient allergies and reactions. We suspect the marked difference may be due to the fact that nurses have many additional duties and do not always have time to obtain this information in such detail. For example, 95% of the 22 ED nurses who responded to our first survey felt that they did not have enough time to complete accurate medication histories. It is also not known if documentation of the last administration time was emphasized during their training. Further improvements in the documentation of patient allergies and reactions could be made through additional education and training for both groups.
Our objectives are not to minimize or criticize the performance and abilities of nurses, but rather to investigate new ways to assist them (as well as other team members) in improving the quality of patient care, service, and safety. We also aim to raise awareness regarding the value of obtaining the best accuracy in medication history documentation and the capacity to use trained pharmacy technicians successfully for this process. Nurses in the ED are often assigned to multiple patients at once and are required to fulfill a variety of patient-care tasks in a limited amount of time. By creating a position that is devoted primarily to the medication-history process, this position can be utilized to investigate and obtain the most accurate medication histories possible. We believe that skilled pharmacy technicians are appropriate candidates for this process, as they have baseline knowledge of prescription medications, including brand and generic names and dosage strengths. Good interpersonal communication skills, the ability to work independently, and problem-solving abilities are also important characteristics for this position.
Ideally, it would be most beneficial to have a pharmacist review each medication history that the pharmacy technician obtains. This would provide a second check against documented lists (or medication administration records) if available. Also, the pharmacist can have the technician double-check anything that does not appear appropriate. The pharmacist would be readily available to answer any questions that the technician may have or to clarify any uncertainties. It may be feasible to relocate a current pharmacy workstation to the ED, which would minimize costs to the department.
Due to the success of this investigation and receipt of positive feedback from ED nursing personnel, we have expanded this program to additional sites within our health system since the time of this study. We have also relocated a pharmacy workstation to the ED. This permits pharmacists to attend to their usual duties as well as reviewing medication histories obtained by the pharmacy technician and answering drug questions from the ED staff.
CONCLUSION
The results of this interventional program indicate that skilled pharmacy technicians are suitable candidates to collect medication histories, and also demonstrate that trained pharmacy technicians can improve the accuracy of medication histories obtained in the ED as compared with relying solely on nurses. This in turn leads to improvements in patient care and safety, and also supports multidisciplinary collaboration and the expansion of pharmacy technician roles.
Footnotes
Disclosure: The authors report no commercial or financial relationships in regard to this article.
REFERENCES
- 1.Mark SM, Little JD, Geller S, Weber RJ. Principles and practices of medication safety. In: Dipiro JT, Talbert RL, Yee GC, et al., editors. Pharmacotherapy: A Pathophysiologic Approach. 8th ed. New York, New York: McGraw-Hill, Education, LLC; 2011. Available at: http://accesspharmacy.mhmedical.com/content.aspx?bookid=462§ionid=41100771. Accessed July 13, 2014. [Google Scholar]
- 2.Institute of Medicine. Preventing medication errors. Report brief. Jul, 2006. Available at: http://www.iom.edu/~/media/Files/Report%20Files/2006/Preventing-Medication-Errors-Quality-Chasm-Series/medicationerrorsnew.ashx. Accessed December 8, 2014.
- 3.Barnsteiner JH. Medication reconciliation. In: Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville, Maryland: Agency for Healthcare Research and Quality; Apr, 2008. Available at: http://www.ncbi.nlm.nih.gov/books/NBK2648/. Accessed July 13, 2014. [PubMed] [Google Scholar]
- 4.Tam VC, Knowles SR, Cornish PL, et al. Frequency, type and clinical importance of medication history errors at admission to hospital: a systematic review. JAMC. 2005;173(5):510–515. doi: 10.1503/cmaj.045311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gleason KM, McDaniel MR, Feinglass J, et al. Results of the Medications at Transitions and Clinical Handoffs (MATCH) study: an analysis of medication reconciliation errors and risk factors at hospital admission. J Gen Intern Med. 2010;25(5):441–447. doi: 10.1007/s11606-010-1256-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Van den Bemt PM, Van den Broek S, Van Nuner AK, et al. Medication reconciliation performed by pharmacy technicians at the time of preoperative screening. Ann Pharmacother. 2009;43(5):868–874. doi: 10.1345/aph.1L579. [DOI] [PubMed] [Google Scholar]
- 7.De Winter S, Spriet I, Indevuyst C, et al. Pharmacist- versus physician-acquired medication history: a prospective study at the emergency department. Qual Saf Health Care. 2010;19(5):371–375. doi: 10.1136/qshc.2009.035014. [DOI] [PubMed] [Google Scholar]
- 8.Johnston R, Saulnier L, Gould O. Best possible medication history in the emergency department: comparing pharmacy technicians and pharmacists. Can J Hosp Pharm. 2010;63(5):359–365. doi: 10.4212/cjhp.v63i5.947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greenwald JL, Halasyamani L, Greene J, et al. Making inpatient medication reconciliation patient centered, clinically relevant and implementable: A consensus statement on key principles and necessary first steps. J Hosp Med. 2010;5(8):477–585. doi: 10.1002/jhm.849. [DOI] [PubMed] [Google Scholar]
- 10.Lindsey K. Medication reconciliation: physician-driven and pharmacy-managed by med rec techs. Michigan Pharmacists Association; Lansing, Michigan: May 4, 2009. [Google Scholar]
- 11.The consensus of the Pharmacy Practice Model Summit. Am J Health-Syst Pharm. 2011;68:1148–1152. doi: 10.2146/ajhp110060. [DOI] [PubMed] [Google Scholar]
- 12. Joint Commission. Hospital national patient safety goals. Elements of performance for NPSG.03.06.01. Available at: http://www.jointcommission.org/assets/1/6/HAP_NPSG_Chapter_2014.pdf. Accessed December 8, 2014.
- 13.Ruble M. Service outcome cost report of pharmacist interventions in the emergency department. Feb, 2010. Conducted at Morton Plant Hospital, Clearwater, Florida.
- 14.Michels RD, Meisel SB. Program using pharmacy technicians to obtain medication histories. Am J Health-Syst Pharm. 2003;60(19):1982–1986. doi: 10.1093/ajhp/60.19.1982. [DOI] [PubMed] [Google Scholar]
- 15.Knight H, Edgerton L, Foster R. Pharmacy technicians obtaining medication histories within the emergency department. Am J Health-Syst Pharm. 2010;67(7):512–514. doi: 10.2146/ajhp090367. [DOI] [PubMed] [Google Scholar]
- 16.Zed PJ, Abu-Laban RB, Balen RM, et al. Incidence, severity and preventability of medication-related visits to the emergency department: a prospective study. CMAJ. 2008;178(12):1563–1569. doi: 10.1503/cmaj.071594. [DOI] [PMC free article] [PubMed] [Google Scholar]