Abstract
Multiple sclerosis (MS) and neuromyelitis optica (NMO) are the most prevalent neuroinflammatory diseases of the central nervous system (CNS). The immunological cascade of these disorders is complex, and the exact spatial and temporal role of different immune cells is not fully understood. Although MS has been considered for many years to be primarily T cell driven, it is well established that B cells and the humoral immune response play an important role in its pathogenesis. This has long been evident from laboratory findings that include the presence of oligoclonal bands in the CSF. In NMO the importance of the humoral immune system appears even more obvious as evidenced by pathogenic antibodies against aquaporin 4 (AQP4). Besides their capacity to mature into antibody-producing plasma cells, B cells are potent antigen presenting cells to T lymphocytes and they can provide soluble factors for cell activation and differentiation to other immune-competent cells.
In MS and NMO, there are substantial data from clinical trials that B cell depletion with CD20-directed agents is effective and relatively safe. Plasma cells, which produce antibodies against molecular targets expressed by the host, but which also provide humeral immune responses against pathogens, are not targeted by anti-CD20 therapies. Therefore the depletion of CD19-expressing cells would offer potential advantages with regard to efficacy, but potentially higher risks with regard to infectious complications.
This review will outline the rationale for CD19 as a molecular target in CNS autoimmunity. The current stage of drug development is illustrated. Potential safety concerns will be discussed.
The putative role of B cells in inflammation
In addition to presenting antigen to T cells, B cells are also a major source of regulatory cytokines (Figure 1). Not unlike T cells, B lymphocytes can be divided into distinct phenotypes based on the cytokines they express. Regulatory B cells (Breg) secrete high levels of interleukin (IL)-10 or transforming growth factor-beta (TGF-β). Plasma cells have recently been described as expressing the highest levels of IL-10 and IL-35 within the B cell population during acute bacterial infection. In the same study, B cell derived IL-35 was also found to be required for recovery from experimental autoimmune encephalomyelitis (EAE), a mouse model for MS [1]. B effector cells (Be) however, produce distinct arrays of cytokines depending on maturation and environmental factors. Analogous to helper T cell (Th) polarization, Be cells were initially classified as expressing either the Th1 signature cytokine interferon gamma (IFNγ) (Be1), or the Th2 cytokines IL-4, IL-5, and IL-13 (Be2), thus regulating leukocyte migration and inflammatory cell infiltration [2]. The exact mechanisms that drive B cell development toward Be1 or Be2 remain mostly unknown. Be1 polarization appears to be the default developmental pathway and absolutely dependent on expression of the IFNγ receptor and the T-box transcription factor T-bet. [3]. In contrast, differentiation towards a Be2 phenotype is promoted by IL-4. The Be 1 phenotype is dynamic, and IL-4 signaling leads to a switch from Be1 to Be2 cells [4].
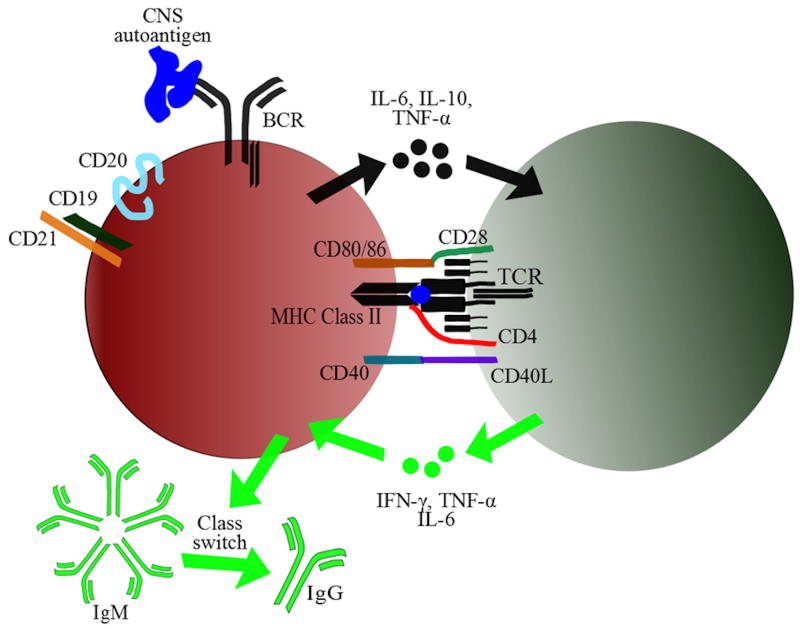
Figure 1. The triple role of B lymphocytes – Antigen presentation, cytokine expression, and antibody secretion.
B lymphocytes are capable of presenting antigen to T cells. They recognize pathogens via the B cell receptor (BCR), and then endocytose the antibody-fixed antigen. Like dendritic cells, B cells constitutively express MHC class II molecules. Upon antigen engagement via the BCR, B cells initiate the expression of various cytokines, including interleukin (IL)-6, IL-10, and tumor necrosis factor alpha (TNFα). These cytokines affect CD4+ T cell activation and differentiation. CD4+ T cells, once activated and differentiated into a specific T helper (Th) cell phenotype, cross-activate B cells via cytokines and co-stimulatory molecules, including cluster of differentiation (CD)40-CD40 ligand and CD80/CD86-CD28. In addition, the class switch from immunoglobulin (Ig) M to IgG requires CD4+ T cell help via cytokines and co-stimulation.
The recognition that B cell subsets may be pro- or anti-inflammatory, and that some of the B cell phenotypes are dynamic in their development is important in the context of any pharmacological intervention, as B cell-depleting therapies should ideally not indiscriminately target Breg and Be subsets. The complexity of B cell biology and their role as putative cellular targets for therapeutic interventions is further illustrated by the fact that Be subsets are only a subset of a larger category, so-called B 2 cells with very diverse surface markers, anatomical distribution, and cellular functions (Table 1).
Table 1.
B cell phenotypes by surface markers, primary anatomical locations, and biological functions.
| B1 B cells | B2 B cells | Regulatory B cells | |
|---|---|---|---|
| Surface Markers | Mice: CD19+ CD20+ CD5+/- CD11+ Humans: CD19+ CD20+ CD27+ CD43+ CD70- |
Mice: CD19+ CD20+ B220+ CD5- Humans: CD19+ CD20+ B220+ CD24lo CD27-CD43- |
Mice:CD19+ CD20+ CD5+ CD1dhi Humans: CD19+ CD20+ CD24hi CD38hiCD27+ |
| Primary Anatomical Locations |
|
|
|
| Biological Functions |
|
|
|
B cells in multiple sclerosis
It has taken neurologists and neuroimmunologists the better part of the 20th century to develop a true appreciation for the pathogenic role of B cells in multiple sclerosis (MS). While a clear understanding of B cell function in MS is still only incompletely understood, the results of recent clinical trials that employed B cell-targeted therapies has made cells of the B cell lineage prime cellular targets in this disorder.
Until recently, B cells were primarily thought of as (auto) antibody producing lymphocytes (Figure 1). In 1942, Elvin Kabat identified monoclonal spikes of immunoglobulin (Ig), or oligoclonal bands (OCBs), by electrophoresis in the cerebrospinal fluid (CSF) of MS patients [5]. Subsequently, Astrid Fagraeus identified the function of plasma cells as antibody-producing cells in 1948 [6]. When John Simpson discovered that antibodies of patients with myasthenia gravis bind the acetylcholine receptor at the neuromuscular junction, their functional role was rightfully interpreted as autoimmune [7]. Given that the presence of OCBs in MS indicate an exaggerated Ig synthesis in the brain and spinal cord, it has been assumed by many that these antibodies may initiate and perpetuate disease activity. The molecular and cellular targets of OCBs in MS have not (yet) been identified despite the fact that plausible candidates, including myelin oligodendroycte glycoprotein (MOG), were investigated extensively. Thus, it cannot be entirely ruled-out that they are an epiphenomenon. However, given the abundance of Ig in some MS lesions, an aberrant humeral immune response against CNS molecular targets cannot be ruled-out [8]. Srivastava and colleagues used a proteomic approach focusing on membrane proteins, and they identified the ATP-sensitive inward rectifying potassium channel KIR4.1 as the target of serum IgG of MS patients, but not controls [9]. Serum antibodies to KIR4.1 were also detectable in the majority of children with acquired demyelinating CNS disorders [10], and the same group reported on a differential loss of KIR4.1 immuno-reactivity in multiple sclerosis lesions [11]. The data has not yet been confirmed by independent groups [12].
The histopathology of MS lesions shows heterogeneity, and one group of investigators identified four fundamentally different patterns of demyelination defined by myelin protein loss, the location and extension of plaques, the patterns of oligodendrocyte destruction, and the immunopathological evidence of complement activation [8]. Two patterns resembled T cell-mediated or T-cell plus antibody–mediated autoimmune encephalomyelitis. The other two patterns suggested a primary oligodendrocyte dystrophy. In contrast to NMO lesions, no eosinophilic infiltrates have been identified in MS lesions. The molecular analyses of B cells in CNS lesions provided evidence for hypermutations and support a view for a pivotal role of compartmentalized antigen-specific B cell expansions [13].
It is now recognized that B cells play additional roles in inflammation in general, and in central nervous system (CNS) inflammation in particular. In a seminal observation, John Prineas described lymphoid tissue in cerebral perivascular spaces in autopsy tissue of patients with MS [14]. In some patients the lymphoid structures within the cerebral perivascular regions resemble the germinal centers in secondary lymphoid organs, where B cells proliferate, differentiate, and mutate the B cell receptor (BCR) through somatic hypermutation [15]. However, cerebral perivascular spaces, also known as “Virchow-Robin spaces”, also constitute a compartment that plays a critical role in antigen presentation within the brain. Hematopoetically-derived myeloid cell subsets and B cells reside in these spaces. It has long been shown that B lymphocytes are very capable of presenting antigen to T cells (Figure 1). Li and colleagues recently demonstrated that B lymphocytes of basal vertebrates are capable of phagocytosis [16]. In humans and other vertebrates, B cells are not capable of engulfing proteins like DC and other phagocytes in order to digest them within the phagosome. However, in these species, B cells do endocytose antibody-fixed pathogens. Like DCs, B cells constitutively express MHC class II molecules. The unique role of B lymphocytes as antigen presenting cells (APC) results from the expression of the high-affinity BCR, which recognizes soluble antigens. This endows them with superior antigen presenting ability for antigens that are present at very small concentrations. Thus, in contrast to myeloid APCs, B cells can selectively present antigens. In addition, B cells can endow antigen-selectivity to DCs by marking pathogens or other antigens, through Fc receptor-binding antibodies (opsonization) for uptake by the phagocyte.
Results from rituximab clinical trials have shown that the role of B cells as APCs and secretors or cytokines and chemokines is very likely more important than their antibody production in the pathogenesis of MS. The deletion or substantial reduction in the number of CD20+ B cells with rituximab also was associated with a significant decrease (>50% of pretreatment levels) in CD3+ T cells within the CSF of patients after a minimum rituximab exposure of 24 weeks. This decrease was attributed to decreases in the chemokines CXCL13 and CCL19 [17]. The efficacy of rituximab on magnetic resonance imaging (MRI) outcomes was studied in a phase II clinical trial. By the 12th week post infusion the total number of gadolinium-enhancing lesions was significantly decreased as compared to the placebo arm, with no new lesions forming from 12 weeks to 48 weeks (end-point for the study) post-infusion [18]. The decreased number of gadolinium-enhancing lesions, along with a lack of newly formed lesions, combined with no significant change in the IgG levels found in the CSF of rituximab treated patients suggests that the APC function of B cells, along with their creation and maintenance of specific cytokine and chemokine networks is more important than their antibody secretion in the pathogenesis of MS.
Twenty-five years after Prineas' initial observation, other investigators re-discovered lymphoid tissue in the CNS, and were able to characterize them in more detail [19],[20]. Serafina and colleagues showed that B cell follicles in the cerebral meninges of patients with MS are sites of Epstein-Barr virus (EBV) latency [21]. In their study, B cells and plasma cells were EBV-infected in all MS cerebral tissues that were evaluated. This observation is potentially interesting since immune responses against EBV have recently been associated with MS [22]. However, other investigators were unable to reproduce the findings by Serfina et al. Willis and colleagues could not detect EBV in any of the examined MS specimens containing white matter lesions by in situ hybridization, immunohistochemistry and two independent real-time polymerase chain reaction (PCR) methodologies that detect genomic EBV or the abundant EBV encoded RNA (EBER) 1, respectively [23].
B cells in neuromyelitis optica
NMO is a recurrent inflammatory disorder of the central nervous system (CNS) that targets predominantly the optic nerves and the spinal cord. Consequently, patients with NMO are primarily afflicted with complete or incomplete vision loss, paraparesis, tetraparesis, sensory loss, and sphincter dysfunction [24]. Specifically, unilateral or bilateral vision loss is the most common initial presentation, followed by recurrent episodes of transverse myelitis, usually presenting as longitudinal extensive transverse myelitis (LETM). The diagnosis of NMO is made mainly on clinical grounds: Current diagnostic criteria require optic neuritis, myelitis, and at least two of three supportive criteria: (1) MRI evidence of a contiguous spinal cord lesion three or more segments in length, (2) onset brain MRI non-diagnostic for multiple sclerosis (MS), or (3) NMO-IgG seropositivity [25]. Importantly, CNS involvement beyond the optic nerves and spinal cord is compatible with a diagnosis of NMO. Once the diagnosis of NMO is established, disease exacerbations are identified clinically, and confirmed by MRI.
Similar to RRMS, the disease course of NMO is typically relapsing-remitting. Also, there is a strong female preponderance. However, a secondary-progressive disease course has also been described but is relatively rare [26]. Instead, disability accumulates almost exclusively as a result of incomplete recovery of relapses.
Lennon and co-workers first identified NMO-IgG, an autoantibody that binds to human aquaporin-4 (hAQP4) [27],[28]. In initial case series, NMO-IgG was detectable in the serum of 33-91% of NMO patients [29]. These discrepancies are explained by differences in study populations and detection assays. More refined methods, including fluorescence-activated cell sorting assays, cell-based assays, and enzyme-linked immunosorbet assays (ELISA) result in a seropositivity of about 90% [30]. Chihara and coworkers discovered that the number of CD20- CD19int CD27high CD38high CD180- peripheral blood plasma blasts correlates directly with serum AQP4 antibody titers in NMO and NMO spectrum disorder seropositive patients [31]. The percentage of peripheral blood plasma blasts also directly correlated to disease relapses. Interestingly, in vitro experiments suggest that IL-6 promotes the production of AQP4 antibody from these peripheral blood plasma blasts, as well as their survival. Remarkably, OCBs within the CSF are only detectable in approximately 30% of patients with NMO [32].
The pathogenicity of NMO-IgG has been clearly demonstrated in animal models [33],[34],[35]. AQP4 plays an important role in the transportation of water across the cell membrane of numerous cell types. Within the CNS, it is highly expressed in the foot processes of astrocytes [36],[37]. There are two isoforms of hAQP4: M1 and the shorter M23 isoform, which lacks the first 22 amino acids but is otherwise identical in sequence [38].
All NMO lesions, regardless of age, disease stage, and disease activity show extensive loss of AQP4 immunoreactivity, which is seen in MS lesions [39],[40],[41]. Interesting, early NMO lesions reveal preserved myelin despite a prominent loss of the astrocytes, which suggests the astrocyte as an early cellular target of an immunological attack [42]. Perivascular IgM, IgG, and C9neo depositions are abundantly present, and immune cell infiltrate, composed primarily of neutrophils, eosinophils, and macrophages are detectable [43]. CD3+ and CD8+ T-cells and natural killer cells are somewhat less prevalent [44].
It is currently not entirely clear how seronegative and seropositive NMO patients differ. A recent retrospective study of 175 Caucasian patients determined that seropositive patients are predominantly female, more often have signs of co-existing autoimmunity, and experience more severe clinical attacks. Seropositive patients and seronegative patients did not differ significantly with regard to age at onset, time to relapse, annualized relapse rates, outcome from relapse (complete, partial, no recovery), annualized EDSS increase, mortality rate, supratentorial brain lesions, brainstem lesions, history of carcinoma, frequency of preceding infections, oligoclonal bands, or CSF pleocytosis [45].
Interestingly, some patients with NMO who are NMO-Ig negative are seropositive for anti-myelin oligodendrocyte glycoprotein (MOG) antibodies. Sato et al recently showed that 7.4% of patients within a cohort of 215 individuals were positive for MOG antibodies [46]. No patients were positive for antibodies against both molecular targets. Furthermore, compared with NMO-Ig-positive patients or patients who were seronegative for either antibody in this study, patients with MOG antibodies showed a male preponderance, presented with optic neuritis more frequently than with transverse myelitis, more frequently had bilateral simultaneous optic neuritis, more often had monophasic disease, and better clinical recovery. Kitley and colleagues reported similar observations in an independent cohort of 29 patients [47].
B cell specific therapies in CNS autoimmune disorders
Perhaps the best evidence to date supporting a role for B-cell involvement in MS pathogenesis comes from clinical trials with rituximab in MS. Rituximab is a chimeric IgG1 monoclonal antibody (mAb) that targets the B-lymphocyte surface antigen CD20 [48]. CD20 is a transmembrane protein involved in B cell activation, differentiation, and calcium transport. It is generally thought that rituximab depletes B lymphocytes via antibody-dependent cell mediated cytotoxicity (ADCC) and complement-dependent cytolysis (CDC). Interestingly, a more recent study by Montalvao and coworkers suggested Ab-dependent cellular phagocytosis of Kupffer cells in the liver as the main mechanism for B cell depletion [49].
Similar results were recently shown with ocrelizumab, a humanized recombinant anti-CD20 mAb [50]. In contrast to rituximab, a chimeric antibody, ocrelizumab is a humanized IgG1 mAb [51]. Thus, its immunogenicity is decreased. Also, its efficacy appears to be mediated primarily by ADCC rather than CDC [52]. A phase II, randomized, placebo-controlled, multicenter trial in patients with RRMS tested low dose ocrelizumab (600mg) on day 1 and 15, high dose ocrelizumab (2000mg) on day 1 and 15 or interferon beta (IFNβ)-1a once a week versus placebo [50]. At week 24 of therapy, the number of gadolinium-enhancing lesions was decreased by 89 % in the low dose and by 96 % in the high dose ocrelizumab group. Both groups significantly outperformed IFNβ-1a. The annualized relapse rate was significantly lower in both ocrelizumab treatment groups than in the placebo or IFNβ-1a groups]. There were no detectable gadolinium-enhancing lesions in either ocrelizumab group at week 96.
Ofatumumab is a fully human IgG1 anti-CD20 mAb [51]. It appears to deplete B cells primarily through CDC. Ofatumumab appears to dissociate from CD20 at a slower rate than rituximab, and binds an additional antigenic determinant [53]. In a phase II trial that enrolled 38 RRMS patients, participants received two doses of either 100 mg, 300 mg, or 700 mg ofatumumab, or placebo. After 24 weeks, there was a significant reduction of gadolinium-enhancing lesions on MRI in the treatment groups [54].
However, not all B cell-modulating therapies investigated in patients with MS showed the desired treatment effect. A phase II trial with atacicept, a recombinant fusion protein targeted to block the activity of BLyS and APRIL, TNF family cytokines that promote B cell proliferation, maturation and survival, was terminated early when patients in the treatment group showed increased disease activity as compared to placebo [55],[56]. Atacicept's failure may be explained by the differing requirements for BLyS and APRIL amongst the various B cell subtypes. Marginal zone B cells and innate-like B1 B cells highly express the APRIL receptor transmembrane activator and calcium-modulator and cytophilin ligand interactor (TACI) due to their higher requirement for APRIL during immune responses. Marginal zone B cells have been suggested to have a regulatory-like function, and they express high levels of IL-10. Regulatory B cells appear to be positioned between marginal zone B cells and B1 B cells based on their surface markers, IL-10 secretion, and increased localization to the peritoneal cavity. Although there is no evidence to suggest absolute requirements for APRIL or BLyS by regulatory B cells, it is likely that a reduced availability of BLyS and APRIL due to atacicept may negatively impact them. As atacicept impairs memory B cells the least of all subgroups, it could also be hypothesized that atacicept blocks the ability of regulatory B cells to control autoreactive memory B cells that may serve as potent APC to T cells. All major B cell phenotypes are described in Table 1.
The presence of hAQP4 as a potential autoantigen that triggers the secretion of NMO-IgG by plasma cells provides a rationale for immunotherapy in patients with NMO. NMO-IgG has been clearly demonstrated to be pathogenic, and not an epiphenomenon [34],[35],[57]. The mainstay of treatment of acute exacerbations centers on high dose steroids and plasma exchange. Interestingly, immunomodulatory drugs approved for treatment of MS have not shown benefit in patients with NMO and may actually be detrimental, including interferon beta [58] and natalizumab [59]. In contrast, immunosuppressive regimens have been shown to be efficacious. Currently accepted treatment regimens for NMO in the US include azathioprine plus prednisone, mycophenolate +/- prednisone, and the anti-CD20 monoclonal antibody, rituximab.
The rationale for utilizing rituximab as a pharmacotherapy in patients with NMO was initially derived from histopathological evaluations of biopsy and autopsy material, where IgM and IgG deposition were abundantly present [43]. To date, no class I evidence from placebo controlled treatment trials support the use of rituximab or other B cell depleting agents in patients with NMO. Data from relatively small, uncontrolled retrospective, and prospective studies show that rituximab appears to have a substantial effect on the relapse rates in NMO, which has been used as a clinical outcome [60],[61],[62],[63]. In these studies, rituximab therapy resulted in a substantial reduction in the annualized relapse rate. However, the treatment response is heterogeneous in that a subset of patients continues to have frequent and severe relapses, possibly due to the inability of rituximab to target pathogenic CD20- plasma blasts and plasma cells within the tissues, as has been seen in primary immune thrombocytopenia (ITP) rituximab treated patients [31],[64]. A second possible reason for treatment failures with rituximab may be due to distinct cytokine networks within patients. IL-10 is typically viewed as an important regulatory cytokine, in regards to autoimmunity, due to its ability to modulate inflammatory T cell and B cell responses. Plasma cells have recently been described as high producers of IL-10 [65],[1]. This would, initially, make rituximab seem like an ideal choice for therapy as it would allow for the potentially regulatory IL-10 secreted from plasma cells to modulate autoreactive effector T cells without interference from autoreactive, pro-inflammatory memory B cells. However, it has been shown in vitro that IL-10 induces B cell differentiation to CD20-CD38+ plasma cells [66]. This suggests that rituximab's failure in some NMO patients may be a result of incomplete depletion of B cells combined with plasma cells furthering the disease process by increasing the development of long-lived, anti-AQP4, plasma cells. This is supported by Uzawa et al finding of increased levels of IL-10 within the CSF of NMO patients [67].
It is currently incompletely understood what factors separate responders and non-responders to rituximab. However, some observations have been made that may guide the design of future clinical studies: (1) A partial repopulation with CD19+20+ B cells prior to the next rituximab dose appears to create a window of vulnerability. Approximately one-third of treatment failures in rituximab trials occur immediately prior to a scheduled rituximab infusion. The absolute number of CD19+20+ B cells in peripheral blood or CSF was not determined in the above mentioned studies. However, Greenberg et al. recently demonstrated that low doses of rituximab showed a high rate of early B-cell repopulation and clinical disease activity [68]. (2) The absolute number of CD27+ memory B cells in peripheral blood may be a better biological marker to monitor NMO disease activity than absolute CD19+20+ B cell numbers [63]. A recent study of 30 NMO patients on rituximab therapy found that treatment failures occurred in all 4 patients who did not achieve suppression of CD27 counts (below 0.05%) with rituximab, while only 2 treatment failures occurred among 26 patients in whom CD27 cells were adequately suppressed [63]. (3) Rituximab therapy leads to an increased expression of B-cell activating factor (BAFF), a potent inducer of antibody production by plasma cells. Nakashima et al. showed that approximately half of NMO patients who received rituximab in the context of a prospective study developed a transient increase in the NMO-IgG titer within 2 weeks of rituximab infusion that correlated with increased BAFF levels [69]. Treatment failures with rituximab in the above mentioned trials have disproportionately occurred within the first 3 weeks of rituximab therapy.
Anti-CD20 therapy is potentially immunosuppressive. The U.S. Food and Drug Administration (FDA) recently approved changes to the prescribing information of ofatumumab and rituximab to add new Boxed Warning information about the risk of reactivation of hepatitis B virus (HBV) infection [70]. The FDA also issued a warning that two patients have died after being treated with rituximab for systemic lupus erythematosus (SLE) [71]. While these patients had previously been treated with immunosuppressant agents and glucocorticosteroids, these observations strongly suggest that depletion of CD20+ cells has potential immunosuppressive effects in recipients.
CD 19 as a molecular target in CNS autoimmunity
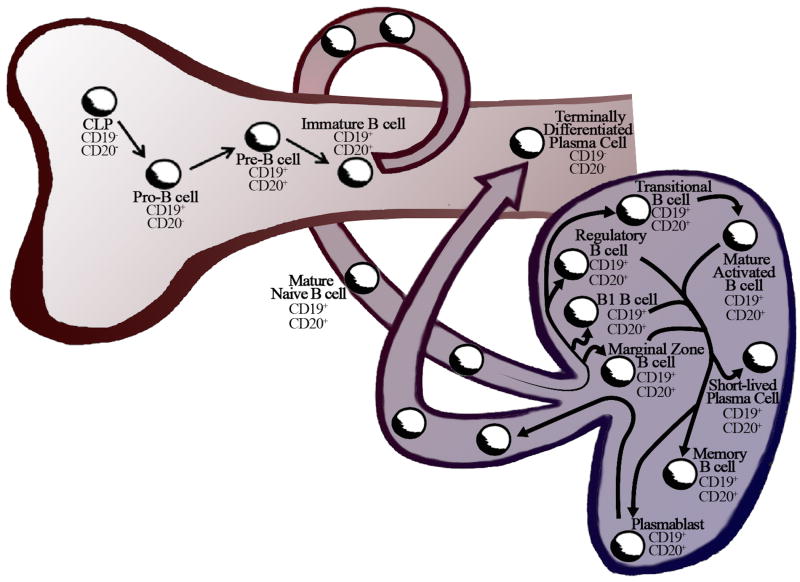
Antibody producing plasma cells are the source of protective, highly target specific antibodies, but also might be the key players in antibody-mediated chronic autoimmune diseases. One potential concern with anti-CD20 immunotherapies is the expression profile of CD20 on human B cells. CD20 can be detected on large pre-B cells, small pre-B cells, immature B cells, naïve B cells, and mature B cells [72],[73],[74],[75],[76] (Figure 2). Thus, the main biological rationale for anti-CD20 interventions is the depletion of the vast majority of cells belonging to the B cell lineage, and to prevent the de novo generation of plasma cells from their precursors. While this appears to be a viable approach, specifically with long-term anti-CD20 therapy, memory B cells that are already situated within target tissues are less affected. Thus, autoimmune events that were already initiated prior to treatment may perpetuate. One potential advantage of this approach is that B cell-mediated immunological memory is not lost, providing one mechanism of host defense against pathogens.
Figure 2. B lymphocyte compartmentalization, development, and differentiation.
In adult mammals, B lymphocytes common lymphocytes progenitors (CLP) originate in the bone marrow, where they develop into Pro-B cells, Pre-B cells, and immature B cells. As part of their life cycle, immature B cells that possess a mature B cell receptor (BCR) and chemokine receptors, egress from the bone marrow into lymphatic vessels. Once within the afferent lymphatics, these cells by definition are considered mature naïve B cells. In the lymph node, there a very heterogeneous groups of B lymphocytes, including marginal zone B cells, B1 cells, B regulatory cells, transitional B cells, mature B cells, memory B cells, as well as short-lived plasma cells, and plasmablasts. The CD19 antigen is a type I transmembrane glycoprotein that belongs to the immunoglobulin Ig superfamily. It is expressed throughout B-cell development, including early pro-B cells and late pro-B cells, as well as in memory B cells, plasmablasts, and a proportion of plasma cells. The overall expression increases approximately threefold as B cells mature. In terminally differentiated plasma cells, which are highly prevalent in the bone marrow, CD19 can no longer be detected.
The CD19 antigen is a type I transmembrane glycoprotein that belongs to the immunoglobulin Ig superfamily. It is expressed throughout B-cell development, including early pro-B cells and late pro-B cells, as well as in memory B cells, plasmablasts, and a proportion of plasma cells [77],[78],[79,80] (Figure 2). The overall expression increases approximately threefold as B cells mature. In terminally differentiated plasma cells, CD19 can no longer be detected [81] (Figure 2).
During lymphopoiesis, B-cell development and differentiation is influenced by CD19 through modulation of B-cell receptor signaling. It appears to be a crucial component in establishing optimal immune responses by modulating antigen-independent B cell development, and immunoglobulin-induced B cell activation. CD19-deficiency in humans and mice leads to an overall impaired humoral response with increased susceptibility to infection [80],[82],[83]. In contrast, overexpression of a human (h)CD19 transgene by its endogenous promoter [84],[85], which recapitulates the developmental pattern of hCD19 surface expression, results in autoimmune disease in the tight skin (TSK/+) mouse, an animal model for human systemic sclerosis (SSc) [86]. In these mice, chronic B cell activation through enhanced CD19-mediated signaling led to skin sclerosis possibly through IL-6 overexpression as well as auto-antibodies.
The hCD19 transgenic mouse model has also been utilized to evaluate CD19-directed immunotherapies. Two weeks after a single injection of anti-CD19 mAb, serum IgM, IgG, and IgA Ab levels were significantly decreased [87]. This effect was sustained for a minimum of 10 weeks. In addition, anti-CD19 therapy decreased autoantibody production in hCD19TG mice.
As such, due to the differential expression of surface markers during B cell maturation, targeting CD19 instead of CD20 in autoimmune diseases might more dramatically affect antibody-secreting plasma cells in the bone marrow [88]. Protective, as well as potentially pathogenic immunoglobulin levels appeared to be only mildly affected by anti-CD20 therapeutics [89],[90],[91]. In contrast, anti-CD19 therapeutics possibly could allow resetting of the immune repertoire of antibody-secreting plasma cells. Hence, therapeutic long-term efficacy of anti-CD19 drugs could possibly exceed the efficacy of anti-CD20 antibodies in NMO, where NMO-Ig is pathogenic. This may also be true in MS.
While the above data provide solid evidence for a potential role of CD19-directed agents in the treatment of human CNS autoimmune disorders, there are other observations that give reason for caution. Blair and colleagues recently described a subset of human CD19+CD24hiCD38hi regulatory B cells [92]. These cells were capable of suppressing Th 1 cell differentiation in vitro. CD138high plasma cells have been shown to express high levels of the cytokines IL-35 and IL-10, which aids in tissue repair as well as in suppressing T and B cell memory responses in vivo [1]. A depletion of all B cells might disrupt B cell homeostasis towards autoimmunity in some individuals in some settings.
Anti-CD19 therapies
Several recombinant CD19 mAbs are currently being developed for clinical trials. The most advanced compound is MEDI-551, an affinity-optimized and afucosylated humanized IgG1 kappa anti-CD19 mAb. Its effect on B cell depletion is primarily mediated by ADCC [93]. The mechanism of depletion requires the presence of FcγRIIIA-bearing effector cells, including natural killer cells, neutrophil polymorphonuclear cells, monocytes, and macrophages. The absence of fucose from MEDI-551 results in a 10-fold enhanced affinity of the mAb to FcγR IIIA (CD16), and enhanced ADCC effector function. Reduced cell surface dissociation and antigen internalization was observed with MEDI-551 as compared to the anti-CD20 mAb rituximab. MEDI-551 demonstrated a robust ADCC activity against B-cell leukemia and lymphoma cell lines in vitro, as well as against chronic lymphocytic leukemia (CLL), and acute lymphoblastic leukemia (ALL) samples.
The safety pharmacokinetics, immunogenicity, and clinical activity of MEDI-551 in patients with B-cell malignancies, including diffuse large B cell lymphoma (DLBCL), CLL, follicular lymphoma (FL), or multiple myeloma (MM) was recently evaluated in a phase 1/2 study [94]. A total of 25 subjects were enrolled. Study participants received MEDI-551 monotherapy at doses of 0.5, 1.0, 2.0, 4.0, 8.0, or 12.0 mg/kg in 28-day cycles using standard 3+3 dose escalation. Results from prior pharmacokinetic studies suggested maximal saturation of CD19 sites at the 12-mg/kg dose. Dose escalation continued until one of the following doses was reached: (1) The maximum tolerated dose (MTD) (if ≤ 12 mg/kg), (2) the 12 mg/kg maximum dose, or the optimal biological dose (OBD) as defined by a composite of safety, pharmacokinetic, pharmacodynamic, and efficacy data. In the event that a MTD was not reached and an OBD was not determined, the protocol allowed for expansion using the highest dose investigated with a pre-defined acceptable risk-benefit profile. Therapy with MEDI-551 was continued until patients achieved a complete response, sustained toxicity, or progression of disease. Subjects with a complete response were permitted 2 additional cycles of MEDI-551 therapy. Patient safety was assessed through 60 days after the last dosing. Responses were assessed using the following criteria: FL and DLBCL: Revised Response Criteria for Malignant Lymphoma update to the International Working Group (IWG) response criteria [95]; CLL: National Cancer Institute–IWG criteria [96]; MM: International Multiple Myeloma Working Group criteria [97]. Immunogenicity against MEDI-551 was assessed on day 1 of each cycle, at the end of therapy, at 30 days and at 60 days post-therapy, and every 3 months thereafter until B cell reconstitution occurred.
An MTD of MEDI-551 was not reached in this trial, and an OBD was not identified. Consequently, in the absence of an MTD or an OBD, the study was expanded using the highest investigated dose (12 mg/kg). As of April 2012, a total of 59 patients were enrolled and received ≥1 dose of MEDI-551. During the dose-escalation phase of the trial, the MTD of MEDI-551 was not reached.
Although this trial was not designed to determine efficacy, antitumor activity of MEDI-551 is suggested by the responses achieved across all dose levels: Objective response rate 26.5%; complete remission 8.8%; partial remission 17.6%; and disease control rate 76.5%.
The majority of treatment-related adverse events was grade 1 or 2 in severity, and included 7 infusion reactions that resolved with appropriate medical interventions. A total of 24 subjects discontinued treatment: 2 due to adverse events (1 grade 2 infusion reaction, 1 grade 2 decreased neutrophil count) and 17 had progressive disease. Six study participants experienced reversible ≥grade 3 treatment-related toxicities, including infusion reaction (in 1 subject), thrombocytopenia, increased blood triglycerides, hyponatremia, and grade 4 neutropenia in 2 patients. Four deaths occurred: 1 due to pneumonia, 1 due to subarachnoid hemorrhage, and 2 due to general physical health deterioration. None of the deaths were considered related to MEDI-551 treatment. No evidence of immunogenicity was observed.
Study MI-CP200 is a Phase I, randomized, double-blind, placebo-controlled clinical trial that was developed to evaluate the safety and tolerability of escalating single intravenous doses of MEDI-551 in 28 adult patients with systemic sclerosis (SSc) [98]. Participants were required to have at least moderate skin thickening in an area suitable for repeat biopsy. Compared to baseline, there was a significant, durable, and dose-dependent depletion of B cells in peripheral blood.
Animal models were utilized to study the pharmacodynamic properties of MEDI-551 in CNS autoimmunity. SLE1 x hCD19 Tg mice (H-2s) spontaneously produce autoreactive Abs as they age. In these mice, MEDI-551 rapidly and effectively depletes B cells in the blood, and bone marrow [98]. Splenic germinal center B cells are also susceptible to MEDI-551 depletion. After B cell depletion with MEDI-551, total IgM and IgG titers decreased significantly. Also, autoimmune antibodies in serum, including anti-nuclear (IgG), anti-histone (IgG), anti-double stranded DNA (IgM and IgG), and anti-single stranded DNA (IgG and IgM) were significantly reduced. It was also observed that the ability of MEDI-551 to decrease the number of antibody-secreting cells is greater in the spleen than in bone marrow. This might be due to the higher prevalence of terminally differentiated CD19- plasma cells in bone marrow. Another possible explanation is the requirement of MEDI-551 for FcγRIIIA-bearing effector cells, including natural killer cells, neutrophil polymorphonuclear cells, monocytes, and macrophages to fully deplete CD19-bearing cells. Thus, the decreased depletion in the bone marrow that was observed could be the result of a relatively low prevalence of FcγRIIIA-expressing effector cells to mediate ADCC.
To identify potential cellular targets of MEDI-551, the expression of CD19 and CD20 on plasma cells from human tissues was assessed by flow cytometry [98]. Plasma blasts and early plasma cells in human blood, tonsil, spleen, and bone marrow were found to be CD19+CD20-. Given that plasma blasts make up over 30% of the CSF B cell compartment in MS patients, and appear to play an important role in MS pathogenesis, the broader expression of CD19 as a molecular target for cell-depleting therapies may be considered advantageous [99].
To determine the feasibility of parallel or sequential combination therapy involving MEDI-551 in patients with MS, one experiment was designed to rule out antagonizing effects between FDA-approved agents or commonly utilized agents and MEDI-551. The ability of MEDI-551 monotherapy to mediate ADCC of B cells was compared to combination therapy with glatiramer acetate, interferon beta, or prednisolone. None of the aforementioned drugs affected the ability of MEDI-551 to deplete B cells. MEDI-551 is currently being tested in Phase 1 clinical trial in RRMS patients [100]. Other anti-CD19 compounds are the aforementioned humanized mouse anti-hCD19 mAb [84], an Fc-engineered, affinity-matured humanized anti-hCD19 mAb that possesses increased FcγR binding avidity, improved ADCC, and which is currently being tested in chronic lymphocytic leukemia (CLL) [101], as well as MDX-1342, a fully humanized recombinant mAB that resulted in substantial B-cell reduction after a single-dose (10 or 30 mg) in patients with rheumatoid arthritis (RA) [80].
In summary, CD19 has been identified as a putative molecular target in human disease. Early clinical data on pharmacodynamics and pharmacokinetic properties of therapeutic mAb are currently gathered and show that this treatment approach might provide and acceptable benefit-risk ratio in human patients.
Weighing potential risks against potential benefits
The role of B cells in MS pathogenesis, the efficacy of anti-CD20 therapies in MS and NMO, and the cellular distribution of CD19 on cells of the B cell lineage provide compelling arguments for CD19-directed therapeutics in CNS autoimmunity. Ultimately, clinical trials will determine whether these agents will provide substantial advantages over approved therapies, and which patient population will be the ideal recipients. As with any intervention, patient safety is the primary concern, and there are currently insufficient data points and certainly no long term safety assessments to fully understand the implications of long-term CD19-mediated cell depletion. Some of the potential concerns are [88]:
Targeting CD19+ B lymphocytes and plasma cells may result in a biologically meaningful weakening of protective adaptive humoral immune responses and host defense. This may include, but not be restricted to, immune surveillance of the CNS.
Acquired adaptive immunity through vaccinations may be impaired or lost. There may be a requirement for revaccination, at least in some individuals.
As stated above, it is currently no known to what extend anti-CD19 therapies affect effector cells and regulatory cells. While it appears that there are beneficial treatment effects during cell depletion in autoimmunity, it is not known how different cell types will reconstitute after cessation of therapy. Also, compartmental effects of anti-CD19 mAbs are not fully understood. Thus, there remain conceptual concerns that inflammation could be exacerbated in some patients.
There are concerns about the potential effects of long-term immunosuppression after anti-CD19 therapy on increased opportunistic infections and neoplastic growth.
In summary, it appears feasible to have any clinical development of CD19-directed pharmacotherapy accompanied by a pharmacovigilance program that assesses the risk of infections, malignancies, and T cell-dependent and independent vaccine responses. Also, from currently available data it appears feasible - after proof of efficacy and safety in ongoing and future clinical trial - to utilize anti-CD19 therapies as a treatment induction: Patients with very active disease could receive CD19-depleting interventions early after failing less aggressive interventions, and for a limited time to reset an aberrant immune response against CNS autoantigens. Then, patients could be maintained on immunomodulatory, relatively safe agents.
Summary
The development of CD19-directed therapies for MS and NMO is exciting. It will offer a more aggressive approach against cells of the B cell lineage than agents that are currently in phase III clinical trial programs. There is no question that these agents have the potential to teach us about the pathogenesis of MS and NMO. Hopefully, neurologists will also learn who amongst their patients would benefit from anti-CD19 therapies: Patients with early disease, patients who do not respond to more T cell-directed interventions, or perhaps even patients with progressive disease phenotypes for whom treatment options are currently limited? Also, how will CD 19-directed therapies compare in efficacy and safety against currently approved drugs and agents that are further along in clinical development? How long will patients need to be treated? As stated above, there are safety concerns regarding long term immunosuppression. However, depletion of CD19+ cells as a monotherapeutic approach, but more likely in combination with other immunoactive agents, might potentially establish immunological tolerance in individuals afflicted with CNS autoimmunity.
There is a long, intriguing road ahead in the development of CD19-directed therapies. Clinical studies will have to be accompanied by thorough assessments of immunological events, other disease biomarkers, and a rigorous pharmacovigilance program.
Reference List
- 1.Shen P, Roch T, Lampropoulou V, O'Connor RA, Stervbo U, Hilgenberg E, Ries S, Dang VD, Jaimes Y, Daridon C, Li R, Jouneau L, Boudinot P, Wilantri S, Sakwa I, Miyazaki Y, Leech MD, McPherson RC, Wirtz S, Neurath M, Hoehlig K, Meinl E, Grutzkau A, Grun JR, Horn K, Kuhl AA, Dorner T, Bar-Or A, Kaufmann SH, Anderton SM, Fillatreau S. IL-35-producing B cells are critical regulators of immunity during autoimmune and infectious diseases. Nature. 2014;507(7492):366–370. doi: 10.1038/nature12979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pistoia V. Production of cytokines by human B cells in health and disease. Immunol Today. 1997;18(7):343–350. doi: 10.1016/s0167-5699(97)01080-3. [DOI] [PubMed] [Google Scholar]
- 3.Harris DP, Goodrich S, Gerth AJ, Peng SL, Lund FE. Regulation of IFN-gamma production by B effector 1 cells: essential roles for T-bet and the IFN-gamma receptor. J Immunol. 2005;174(11):6781–6790. doi: 10.4049/jimmunol.174.11.6781. [DOI] [PubMed] [Google Scholar]
- 4.Harris DP, Goodrich S, Mohrs K, Mohrs M, Lund FE. Cutting edge: the development of IL-4-producing B cells (B effector 2 cells) is controlled by IL-4, IL-4 receptor alpha, and Th2 cells. Journal of immunology. 2005;175(11):7103–7107. doi: 10.4049/jimmunol.175.11.7103. [DOI] [PubMed] [Google Scholar]
- 5.Kabat EA, Moore DH, Landow H. An Electrophoretic Study of the Protein Components in Cerebrospinal Fluid and Their Relationship to the Serum Proteins. The Journal of clinical investigation. 1942;21(5):571–577. doi: 10.1172/JCI101335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fagraeus A. The plasma cellular reaction and its relation to the formation of antibodies in vitro. Journal of immunology. 1948;58(1):1–13. [PubMed] [Google Scholar]
- 7.Simpson JA. Myasthenia gravis: a new hypothesis. ScotMedJ. 1960;5:419–436. [Google Scholar]
- 8.Lucchinetti C, Bruck W, Parisi J, Scheithauer B, Rodriguez M, Lassmann H. Heterogeneity of multiple sclerosis lesions: implications for the pathogenesis of demyelination. Annals of neurology. 2000;47(6):707–717. doi: 10.1002/1531-8249(200006)47:6<707::aid-ana3>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 9.Srivastava R, Aslam M, Kalluri SR, Schirmer L, Buck D, Tackenberg B, Rothhammer V, Chan A, Gold R, Berthele A, Bennett JL, Korn T, Hemmer B. Potassium channel KIR4.1 as an immune target in multiple sclerosis. The New England journal of medicine. 2012;367(2):115–123. doi: 10.1056/NEJMoa1110740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kraus V, Srivastava R, Kalluri SR, Seidel U, Schuelke M, Schimmel M, Rostasy K, Leiz S, Hosie S, Grummel V, Hemmer B. Potassium channel KIR4.1-specific antibodies in children with acquired demyelinating CNS disease. Neurology. 2014;82(6):470–473. doi: 10.1212/WNL.0000000000000097. [DOI] [PubMed] [Google Scholar]
- 11.Schirmer L, Srivastava R, Kalluri SR, Bottinger S, Herwerth M, Carassiti D, Srivastava B, Gempt J, Schlegel J, Kuhlmann T, Korn T, Reynolds R, Hemmer B. Differential loss of KIR4.1 immunoreactivity in multiple sclerosis lesions. Annals of neurology. 2014 doi: 10.1002/ana.24168. [DOI] [PubMed] [Google Scholar]
- 12.Nerrant E, Salsac C, Charif M, Ayrignac X, Carra-Dalliere C, Castelnovo G, Goulabchand R, Tisseyre J, Raoul C, Eliaou JF, Labauge P, Vincent T. Lack of confirmation of anti-inward rectifying potassium channel 4.1 antibodies as reliable markers of multiple sclerosis. Multiple sclerosis. 2014 doi: 10.1177/1352458514531086. [DOI] [PubMed] [Google Scholar]
- 13.Lehmann-Horn K, Kronsbein HC, Weber MS. Targeting B cells in the treatment of multiple sclerosis: recent advances and remaining challenges. Therapeutic advances in neurological disorders. 2013;6(3):161–173. doi: 10.1177/1756285612474333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prineas JW, Wright RG. Macrophages, lymphocytes, and plasma cells in the perivascular compartment in chronic multiple sclerosis. Lab Invest. 1978;38(4):409–421. [PubMed] [Google Scholar]
- 15.Kim S, Davis M, Sinn E, Patten P, Hood L. Antibody diversity: somatic hypermutation of rearranged VH genes. Cell. 1981;27(3 Pt 2):573–581. doi: 10.1016/0092-8674(81)90399-8. [DOI] [PubMed] [Google Scholar]
- 16.Li J, Barreda DR, Zhang YA, Boshra H, Gelman AE, Lapatra S, Tort L, Sunyer JO. B lymphocytes from early vertebrates have potent phagocytic and microbicidal abilities. Nature immunology. 2006;7(10):1116–1124. doi: 10.1038/ni1389. [DOI] [PubMed] [Google Scholar]
- 17.Cross AH, Klein RS, Piccio L. Rituximab combination therapy in relapsing multiple sclerosis. Therapeutic advances in neurological disorders. 2012;5(6):311–319. doi: 10.1177/1756285612461165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hauser SL, Waubant E, Arnold DL, Vollmer T, Antel J, Fox RJ, Bar-Or A, Panzara M, Sarkar N, Agarwal S, Langer-Gould A, Smith CH, Group HT. B-cell depletion with rituximab in relapsing-remitting multiple sclerosis. The New England journal of medicine. 2008;358(7):676–688. doi: 10.1056/NEJMoa0706383. [DOI] [PubMed] [Google Scholar]
- 19.Serafini B, Rosicarelli B, Magliozzi R, Stigliano E, Aloisi F. Detection of ectopic B-cell follicles with germinal centers in the meninges of patients with secondary progressive multiple sclerosis. Brain pathology. 2004;14(2):164–174. doi: 10.1111/j.1750-3639.2004.tb00049.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Magliozzi R, Howell O, Vora A, Serafini B, Nicholas R, Puopolo M, Reynolds R, Aloisi F. Meningeal B-cell follicles in secondary progressive multiple sclerosis associate with early onset of disease and severe cortical pathology. Brain. 2007;130(Pt 4):1089–1104. doi: 10.1093/brain/awm038. [DOI] [PubMed] [Google Scholar]
- 21.Serafini B, Rosicarelli B, Franciotta D, Magliozzi R, Reynolds R, Cinque P, Andreoni L, Trivedi P, Salvetti M, Faggioni A, Aloisi F. Dysregulated Epstein-Barr virus infection in the multiple sclerosis brain. The Journal of experimental medicine. 2007;204(12):2899–2912. doi: 10.1084/jem.20071030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ascherio A, Munger KL. 99th Dahlem conference on infection, inflammation and chronic inflammatory disorders: Epstein-Barr virus and multiple sclerosis: epidemiological evidence. Clinical and experimental immunology. 2010;160(1):120–124. doi: 10.1111/j.1365-2249.2010.04121.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Willis SN, Stadelmann C, Rodig SJ, Caron T, Gattenloehner S, Mallozzi SS, Roughan JE, Almendinger SE, Blewett MM, Bruck W, Hafler DA, O'Connor KC. Epstein-Barr virus infection is not a characteristic feature of multiple sclerosis brain. Brain. 2009;132(Pt 12):3318–3328. doi: 10.1093/brain/awp200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cree BA, Goodin DS, Hauser SL. Neuromyelitis optica. Seminars in neurology. 2002;22(2):105–122. doi: 10.1055/s-2002-36534. [DOI] [PubMed] [Google Scholar]
- 25.Wingerchuk DM, Lennon VA, Pittock SJ, Lucchinetti CF, Weinshenker BG. Revised diagnostic criteria for neuromyelitis optica. Neurology. 2006;66(10):1485–1489. doi: 10.1212/01.wnl.0000216139.44259.74. [DOI] [PubMed] [Google Scholar]
- 26.Wingerchuk DM, Pittock SJ, Lucchinetti CF, Lennon VA, Weinshenker BG. A secondary progressive clinical course is uncommon in neuromyelitis optica. Neurology. 2007;68(8):603–605. doi: 10.1212/01.wnl.0000254502.87233.9a. [DOI] [PubMed] [Google Scholar]
- 27.Lennon VA, Wingerchuk DM, Kryzer TJ, Pittock SJ, Lucchinetti CF, Fujihara K, Nakashima I, Weinshenker BG. A serum autoantibody marker of neuromyelitis optica: distinction from multiple sclerosis. Lancet. 2004;364(9451):2106–2112. doi: 10.1016/S0140-6736(04)17551-X. [DOI] [PubMed] [Google Scholar]
- 28.Lennon VA, Kryzer TJ, Pittock SJ, Verkman AS, Hinson SR. IgG marker of optic-spinal multiple sclerosis binds to the aquaporin-4 water channel. The Journal of experimental medicine. 2005;202(4):473–477. doi: 10.1084/jem.20050304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jarius S, Franciotta D, Bergamaschi R, Wright H, Littleton E, Palace J, Hohlfeld R, Vincent A. NMO-IgG in the diagnosis of neuromyelitis optica. Neurology. 2007;68(13):1076–1077. doi: 10.1212/01.wnl.0000256822.01222.bd. [DOI] [PubMed] [Google Scholar]
- 30.Jiao Y, Fryer JP, Lennon VA, Jenkins SM, Quek AM, Smith CY, McKeon A, Costanzi C, Iorio R, Weinshenker BG, Wingerchuk DM, Shuster EA, Lucchinetti CF, Pittock SJ. Updated estimate of AQP4-IgG serostatus and disability outcome in neuromyelitis optica. Neurology. 2013;81(14):1197–1204. doi: 10.1212/WNL.0b013e3182a6cb5c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chihara N, Aranami T, Sato W, Miyazaki Y, Miyake S, Okamoto T, Ogawa M, Toda T, Yamamura T. Interleukin 6 signaling promotes anti-aquaporin 4 autoantibody production from plasmablasts in neuromyelitis optica. Proceedings of the National Academy of Sciences of the United States of America. 2011;108(9):3701–3706. doi: 10.1073/pnas.1017385108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jarius S, Paul F, Franciotta D, Ruprecht K, Ringelstein M, Bergamaschi R, Rommer P, Kleiter I, Stich O, Reuss R, Rauer S, Zettl UK, Wandinger KP, Melms A, Aktas O, Kristoferitsch W, Wildemann B. Cerebrospinal fluid findings in aquaporin-4 antibody positive neuromyelitis optica: results from 211 lumbar punctures. Journal of the neurological sciences. 2011;306(1-2):82–90. doi: 10.1016/j.jns.2011.03.038. [DOI] [PubMed] [Google Scholar]
- 33.Bradl M, Misu T, Takahashi T, Watanabe M, Mader S, Reindl M, Adzemovic M, Bauer J, Berger T, Fujihara K, Itoyama Y, Lassmann H. Neuromyelitis optica: pathogenicity of patient immunoglobulin in vivo. Annals of neurology. 2009;66(5):630–643. doi: 10.1002/ana.21837. [DOI] [PubMed] [Google Scholar]
- 34.Bennett JL, Lam C, Kalluri SR, Saikali P, Bautista K, Dupree C, Glogowska M, Case D, Antel JP, Owens GP, Gilden D, Nessler S, Stadelmann C, Hemmer B. Intrathecal pathogenic anti-aquaporin-4 antibodies in early neuromyelitis optica. Annals of neurology. 2009;66(5):617–629. doi: 10.1002/ana.21802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Asavapanumas N, Ratelade J, Papadopoulos MC, Bennett JL, Levin MH, Verkman AS. Experimental mouse model of optic neuritis with inflammatory demyelination produced by passive transfer of neuromyelitis optica-immunoglobulin G. Journal of neuroinflammation. 2014;11:16. doi: 10.1186/1742-2094-11-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Connolly DL, Shanahan CM, Weissberg PL. The aquaporins. A family of water channel proteins. The international journal of biochemistry & cell biology. 1998;30(2):169–172. doi: 10.1016/s1357-2725(97)00124-6. [DOI] [PubMed] [Google Scholar]
- 37.Pittock SJ, Weinshenker BG, Lucchinetti CF, Wingerchuk DM, Corboy JR, Lennon VA. Neuromyelitis optica brain lesions localized at sites of high aquaporin 4 expression. Archives of neurology. 2006;63(7):964–968. doi: 10.1001/archneur.63.7.964. [DOI] [PubMed] [Google Scholar]
- 38.Furman CS, Gorelick-Feldman DA, Davidson KG, Yasumura T, Neely JD, Agre P, Rash JE. Aquaporin-4 square array assembly: opposing actions of M1 and M23 isoforms. Proceedings of the National Academy of Sciences of the United States of America. 2003;100(23):13609–13614. doi: 10.1073/pnas.2235843100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Misu T, Fujihara K, Kakita A, Konno H, Nakamura M, Watanabe S, Takahashi T, Nakashima I, Takahashi H, Itoyama Y. Loss of aquaporin 4 in lesions of neuromyelitis optica: distinction from multiple sclerosis. Brain. 2007;130(Pt 5):1224–1234. doi: 10.1093/brain/awm047. [DOI] [PubMed] [Google Scholar]
- 40.Roemer SF, Parisi JE, Lennon VA, Benarroch EE, Lassmann H, Bruck W, Mandler RN, Weinshenker BG, Pittock SJ, Wingerchuk DM, Lucchinetti CF. Pattern-specific loss of aquaporin-4 immunoreactivity distinguishes neuromyelitis optica from multiple sclerosis. Brain. 2007;130(Pt 5):1194–1205. doi: 10.1093/brain/awl371. [DOI] [PubMed] [Google Scholar]
- 41.Sinclair C, Kirk J, Herron B, Fitzgerald U, McQuaid S. Absence of aquaporin-4 expression in lesions of neuromyelitis optica but increased expression in multiple sclerosis lesions and normal-appearing white matter. Acta neuropathologica. 2007;113(2):187–194. doi: 10.1007/s00401-006-0169-2. [DOI] [PubMed] [Google Scholar]
- 42.Parratt JD, Prineas JW. Neuromyelitis optica: a demyelinating disease characterized by acute destruction and regeneration of perivascular astrocytes. Mult Scler. 2010;16(10):1156–1172. doi: 10.1177/1352458510382324. [DOI] [PubMed] [Google Scholar]
- 43.Lucchinetti CF, Mandler RN, McGavern D, Bruck W, Gleich G, Ransohoff RM, Trebst C, Weinshenker B, Wingerchuk D, Parisi JE, Lassmann H. A role for humoral mechanisms in the pathogenesis of Devic's neuromyelitis optica. Brain. 2002;125(Pt 7):1450–1461. doi: 10.1093/brain/awf151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Saadoun S, Bridges LR, Verkman AS, Papadopoulos MC. Paucity of natural killer and cytotoxic T cells in human neuromyelitis optica lesions. Neuroreport. 2012;23(18):1044–1047. doi: 10.1097/WNR.0b013e32835ab480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jarius S, Ruprecht K, Wildemann B, Kuempfel T, Ringelstein M, Geis C, Kleiter I, Kleinschnitz C, Berthele A, Brettschneider J, Hellwig K, Hemmer B, Linker RA, Lauda F, Mayer CA, Tumani H, Melms A, Trebst C, Stangel M, Marziniak M, Hoffmann F, Schippling S, Faiss JH, Neuhaus O, Ettrich B, Zentner C, Guthke K, Hofstadt-van Oy U, Reuss R, Pellkofer H, Ziemann U, Kern P, Wandinger KP, Bergh FT, Boettcher T, Langel S, Liebetrau M, Rommer PS, Niehaus S, Munch C, Winkelmann A, Zettl UU, Metz I, Veauthier C, Sieb JP, Wilke C, Hartung HP, Aktas O, Paul F. Contrasting disease patterns in seropositive and seronegative neuromyelitis optica: A multicentre study of 175 patients. Journal of neuroinflammation. 2012;9:14. doi: 10.1186/1742-2094-9-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sato DK, Callegaro D, Lana-Peixoto MA, Waters PJ, de Haidar Jorge FM, Takahashi T, Nakashima I, Apostolos-Pereira SL, Talim N, Simm RF, Lino AM, Misu T, Leite MI, Aoki M, Fujihara K. Distinction between MOG antibody-positive and AQP4 antibody-positive NMO spectrum disorders. Neurology. 2014;82(6):474–481. doi: 10.1212/WNL.0000000000000101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kitley J, Waters P, Woodhall M, Leite MI, Murchison A, George J, Kuker W, Chandratre S, Vincent A, Palace J. Neuromyelitis optica spectrum disorders with aquaporin-4 and myelin-oligodendrocyte glycoprotein antibodies: a comparative study. JAMA neurology. 2014;71(3):276–283. doi: 10.1001/jamaneurol.2013.5857. [DOI] [PubMed] [Google Scholar]
- 48.Stuve O, Cepok S, Elias B, Saleh A, Hartung HP, Hemmer B, Kieseier BC. Clinical stabilization and effective B-lymphocyte depletion in the cerebrospinal fluid and peripheral blood of a patient with fulminant relapsing-remitting multiple sclerosis. Archives of neurology. 2005;62(10):1620–1623. doi: 10.1001/archneur.62.10.1620. [DOI] [PubMed] [Google Scholar]
- 49.Montalvao F, Garcia Z, Celli S, Breart B, Deguine J, Van Rooijen N, Bousso P. The mechanism of anti-CD20-mediated B cell depletion revealed by intravital imaging. The Journal of clinical investigation. 2013;123(12):5098–5103. doi: 10.1172/JCI70972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kappos L, Li D, Calabresi PA, O'Connor P, Bar-Or A, Barkhof F, Yin M, Leppert D, Glanzman R, Tinbergen J, Hauser SL. Ocrelizumab in relapsing-remitting multiple sclerosis: a phase 2, randomised, placebo-controlled, multicentre trial. Lancet. 2011;378(9805):1779–1787. doi: 10.1016/S0140-6736(11)61649-8. [DOI] [PubMed] [Google Scholar]
- 51.Rommer PS, Dudesek A, Stuve O, Zettl UK. Monoclonal antibodies in treatment of multiple sclerosis. Clinical and experimental immunology. 2014;175(3):373–384. doi: 10.1111/cei.12197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kausar F, Mustafa K, Sweis G, Sawaqed R, Alawneh K, Salloum R, Badaracco M, Niewold TB, Sweiss NJ. Ocrelizumab: a step forward in the evolution of B-cell therapy. Expert opinion on biological therapy. 2009;9(7):889–895. doi: 10.1517/14712590903018837. [DOI] [PubMed] [Google Scholar]
- 53.Zhang B. Ofatumumab. mAbs. 2009;1(4):326–331. doi: 10.4161/mabs.1.4.8895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sorensen PS, Lisby S, Grove R, Derosier F, Shackelford S, Havrdova E, Drulovic J, Filippi M. Safety and efficacy of ofatumumab in relapsing-remitting multiple sclerosis: a phase 2 study. Neurology. 2014;82(7):573–581. doi: 10.1212/WNL.0000000000000125. [DOI] [PubMed] [Google Scholar]
- 55.Hartung HP, Kieseier BC. Atacicept: targeting B cells in multiple sclerosis. Therapeutic advances in neurological disorders. 2010;3(4):205–216. doi: 10.1177/1756285610371146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kappos L, Hartung HP, Freedman MS, Boyko A, Radu EW, Mikol DD, Lamarine M, Hyvert Y, Freudensprung U, Plitz T, van Beek J, Group AS. Atacicept in multiple sclerosis (ATAMS): a randomised, placebo-controlled, double-blind, phase 2 trial. Lancet neurology. 2014;13(4):353–363. doi: 10.1016/S1474-4422(14)70028-6. [DOI] [PubMed] [Google Scholar]
- 57.Ratelade J, Asavapanumas N, Ritchie AM, Wemlinger S, Bennett JL, Verkman AS. Involvement of antibody-dependent cell-mediated cytotoxicity in inflammatory demyelination in a mouse model of neuromyelitis optica. Acta neuropathologica. 2013;126(5):699–709. doi: 10.1007/s00401-013-1172-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Shimizu J, Hatanaka Y, Hasegawa M, Iwata A, Sugimoto I, Date H, Goto J, Shimizu T, Takatsu M, Sakurai Y, Nakase H, Uesaka Y, Hashida H, Hashimoto K, Komiya T, Tsuji S. IFNbeta-1b may severely exacerbate Japanese optic-spinal MS in neuromyelitis optica spectrum. Neurology. 2010;75(16):1423–1427. doi: 10.1212/WNL.0b013e3181f8832e. [DOI] [PubMed] [Google Scholar]
- 59.Kleiter I, Hellwig K, Berthele A, Kumpfel T, Linker RA, Hartung HP, Paul F, Aktas O Neuromyelitis Optica Study G. Failure of natalizumab to prevent relapses in neuromyelitis optica. Archives of neurology. 2012;69(2):239–245. doi: 10.1001/archneurol.2011.216. [DOI] [PubMed] [Google Scholar]
- 60.Cree BA, Lamb S, Morgan K, Chen A, Waubant E, Genain C. An open label study of the effects of rituximab in neuromyelitis optica. Neurology. 2005;64(7):1270–1272. doi: 10.1212/01.WNL.0000159399.81861.D5. [DOI] [PubMed] [Google Scholar]
- 61.Jacob A, Weinshenker BG, Violich I, McLinskey N, Krupp L, Fox RJ, Wingerchuk DM, Boggild M, Constantinescu CS, Miller A, De Angelis T, Matiello M, Cree BA. Treatment of neuromyelitis optica with rituximab: retrospective analysis of 25 patients. Archives of neurology. 2008;65(11):1443–1448. doi: 10.1001/archneur.65.11.noc80069. [DOI] [PubMed] [Google Scholar]
- 62.Pellkofer HL, Krumbholz M, Berthele A, Hemmer B, Gerdes LA, Havla J, Bittner R, Canis M, Meinl E, Hohlfeld R, Kuempfel T. Long-term follow-up of patients with neuromyelitis optica after repeated therapy with rituximab. Neurology. 2011;76(15):1310–1315. doi: 10.1212/WNL.0b013e3182152881. [DOI] [PubMed] [Google Scholar]
- 63.Kim SH, Kim W, Li XF, Jung IJ, Kim HJ. Repeated treatment with rituximab based on the assessment of peripheral circulating memory B cells in patients with relapsing neuromyelitis optica over 2 years. Archives of neurology. 2011;68(11):1412–1420. doi: 10.1001/archneurol.2011.154. [DOI] [PubMed] [Google Scholar]
- 64.Mahevas M, Patin P, Huetz F, Descatoire M, Cagnard N, Bole-Feysot C, Le Gallou S, Khellaf M, Fain O, Boutboul D, Galicier L, Ebbo M, Lambotte O, Hamidou M, Bierling P, Godeau B, Michel M, Weill JC, Reynaud CA. B cell depletion in immune thrombocytopenia reveals splenic long-lived plasma cells. The Journal of clinical investigation. 2013;123(1):432–442. doi: 10.1172/JCI65689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Madan R, Demircik F, Surianarayanan S, Allen JL, Divanovic S, Trompette A, Yogev N, Gu Y, Khodoun M, Hildeman D, Boespflug N, Fogolin MB, Grobe L, Greweling M, Finkelman FD, Cardin R, Mohrs M, Muller W, Waisman A, Roers A, Karp CL. Nonredundant roles for B cell-derived IL-10 in immune counter-regulation. J Immunol. 2009;183(4):2312–2320. doi: 10.4049/jimmunol.0900185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Choe J, Choi YS. IL-10 interrupts memory B cell expansion in the germinal center by inducing differentiation into plasma cells. European journal of immunology. 1998;28(2):508–515. doi: 10.1002/(SICI)1521-4141(199802)28:02<508::AID-IMMU508>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 67.Uzawa A, Mori M, Arai K, Sato Y, Hayakawa S, Masuda S, Taniguchi J, Kuwabara S. Cytokine and chemokine profiles in neuromyelitis optica: significance of interleukin-6. Mult Scler. 2010;16(12):1443–1452. doi: 10.1177/1352458510379247. [DOI] [PubMed] [Google Scholar]
- 68.Greenberg BM, Graves D, Remington G, Hardeman P, Mann M, Karandikar N, Stuve O, Monson N, Frohman E. Rituximab dosing and monitoring strategies in neuromyelitis optica patients: creating strategies for therapeutic success. Multiple sclerosis. 2012;18(7):1022–1026. doi: 10.1177/1352458511432896. [DOI] [PubMed] [Google Scholar]
- 69.Nakashima I, Takahashi T, Cree BA, Kim HJ, Suzuki C, Genain CP, Vincent T, Fujihara K, Itoyama Y, Bar-Or A. Transient increases in anti-aquaporin-4 antibody titers following rituximab treatment in neuromyelitis optica, in association with elevated serum BAFF levels. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2011;18(7):997–998. doi: 10.1016/j.jocn.2010.12.011. [DOI] [PubMed] [Google Scholar]
- 70.http://www.fda.gov/Drugs/DrugSafety/ucm366406.htm.
- 71.http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm126519.htm.
- 72.Stashenko P, Nadler LM, Hardy R, Schlossman SF. Characterization of a human B lymphocyte-specific antigen. J Immunol. 1980;125(4):1678–1685. [PubMed] [Google Scholar]
- 73.Stashenko P, Nadler LM, Hardy R, Schlossman SF. Expression of cell surface markers after human B lymphocyte activation. Proceedings of the National Academy of Sciences of the United States of America. 1981;78(6):3848–3852. doi: 10.1073/pnas.78.6.3848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Loken MR, Shah VO, Dattilio KL, Civin CI. Flow cytometric analysis of human bone marrow. II. Normal B lymphocyte development. Blood. 1987;70(5):1316–1324. [PubMed] [Google Scholar]
- 75.Uchida J, Lee Y, Hasegawa M, Liang Y, Bradney A, Oliver JA, Bowen K, Steeber DA, Haas KM, Poe JC, Tedder TF. Mouse CD20 expression and function. International immunology. 2004;16(1):119–129. doi: 10.1093/intimm/dxh009. [DOI] [PubMed] [Google Scholar]
- 76.Pieper K, Grimbacher B, Eibel H. B-cell biology and development. The Journal of allergy and clinical immunology. 2013;131(4):959–971. doi: 10.1016/j.jaci.2013.01.046. [DOI] [PubMed] [Google Scholar]
- 77.Bradbury LE, Kansas GS, Levy S, Evans RL, Tedder TF. The CD19/CD21 signal transducing complex of human B lymphocytes includes the target of antiproliferative antibody-1 and Leu-13 molecules. J Immunol. 1992;149(9):2841–2850. [PubMed] [Google Scholar]
- 78.Haas KM, Tedder TF. Role of the CD19 and CD21/35 receptor complex in innate immunity, host defense and autoimmunity. Advances in experimental medicine and biology. 2005;560:125–139. doi: 10.1007/0-387-24180-9_16. [DOI] [PubMed] [Google Scholar]
- 79.Otero DC, Anzelon AN, Rickert RC. CD19 function in early and late B cell development: I. Maintenance of follicular and marginal zone B cells requires CD19-dependent survival signals. J Immunol. 2003;170(1):73–83. doi: 10.4049/jimmunol.170.1.73. [DOI] [PubMed] [Google Scholar]
- 80.Tedder TF. CD19: a promising B cell target for rheumatoid arthritis. Nature reviews Rheumatology. 2009;5(10):572–577. doi: 10.1038/nrrheum.2009.184. [DOI] [PubMed] [Google Scholar]
- 81.Cooper LJ, Al-Kadhimi Z, DiGiusto D, Kalos M, Colcher D, Raubitschek A, Forman SJ, Jensen MC. Development and application of CD19-specific T cells for adoptive immunotherapy of B cell malignancies. Blood cells, molecules & diseases. 2004;33(1):83–89. doi: 10.1016/j.bcmd.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 82.Poe JC, Minard-Colin V, Kountikov EI, Haas KM, Tedder TF. A c-Myc and surface CD19 signaling amplification loop promotes B cell lymphoma development and progression in mice. J Immunol. 2012;189(5):2318–2325. doi: 10.4049/jimmunol.1201000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.van Zelm MC, Reisli I, van der Burg M, Castano D, van Noesel CJ, van Tol MJ, Woellner C, Grimbacher B, Patino PJ, van Dongen JJ, Franco JL. An antibody-deficiency syndrome due to mutations in the CD19 gene. The New England journal of medicine. 2006;354(18):1901–1912. doi: 10.1056/NEJMoa051568. [DOI] [PubMed] [Google Scholar]
- 84.Zhou LJ, Smith HM, Waldschmidt TJ, Schwarting R, Daley J, Tedder TF. Tissue-specific expression of the human CD19 gene in transgenic mice inhibits antigen-independent B-lymphocyte development. Molecular and cellular biology. 1994;14(6):3884–3894. doi: 10.1128/mcb.14.6.3884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Engel P, Zhou LJ, Ord DC, Sato S, Koller B, Tedder TF. Abnormal B lymphocyte development, activation, and differentiation in mice that lack or overexpress the CD19 signal transduction molecule. Immunity. 1995;3(1):39–50. doi: 10.1016/1074-7613(95)90157-4. [DOI] [PubMed] [Google Scholar]
- 86.Saito E, Fujimoto MIuuCmaiam, Hasegawa M, Komura K, Hamaguchi Y, Kaburagi Y, Nagaoka T, Takehara K, Tedder TF, Sato S. CD19-dependent B lymphocyte signaling thresholds influence skin fibrosis and autoimmunity in the tight-skin mouse. The Journal of clinical investigation. 2002;109(11):1453–1462. doi: 10.1172/JCI15078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Yazawa N, Hamaguchi Y, Poe JC, Tedder TF. Immunotherapy using unconjugated CD19 monoclonal antibodies in animal models for B lymphocyte malignancies and autoimmune disease. Proceedings of the National Academy of Sciences of the United States of America. 2005;102(42):15178–15183. doi: 10.1073/pnas.0505539102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Mei HE, Schmidt S, Dorner T. Rationale of anti-CD19 immunotherapy: an option to target autoreactive plasma cells in autoimmunity. Arthritis research & therapy. 2012;14(Suppl 5):S1. doi: 10.1186/ar3909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Cambridge G, Leandro MJ, Edwards JC, Ehrenstein MR, Salden M, Bodman-Smith M, Webster AD. Serologic changes following B lymphocyte depletion therapy for rheumatoid arthritis. Arthritis and rheumatism. 2003;48(8):2146–2154. doi: 10.1002/art.11181. [DOI] [PubMed] [Google Scholar]
- 90.Vallerskog T, Gunnarsson I, Widhe M, Risselada A, Klareskog L, van Vollenhoven R, Malmstrom V, Trollmo C. Treatment with rituximab affects both the cellular and the humoral arm of the immune system in patients with SLE. Clinical immunology. 2007;122(1):62–74. doi: 10.1016/j.clim.2006.08.016. [DOI] [PubMed] [Google Scholar]
- 91.Stohl W, Gomez-Reino J, Olech E, Dudler J, Fleischmann RM, Zerbini CA, Ashrafzadeh A, Grzeschik S, Bieraugel R, Green J, Francom S, Dummer W. Safety and efficacy of ocrelizumab in combination with methotrexate in MTX-naive subjects with rheumatoid arthritis: the phase III FILM trial. Annals of the rheumatic diseases. 2012;71(8):1289–1296. doi: 10.1136/annrheumdis-2011-200706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Blair PA, Norena LY, Flores-Borja F, Rawlings DJ, Isenberg DA, Ehrenstein MR, Mauri C. CD19(+)CD24(hi)CD38(hi) B cells exhibit regulatory capacity in healthy individuals but are functionally impaired in systemic Lupus Erythematosus patients. Immunity. 2010;32(1):129–140. doi: 10.1016/j.immuni.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 93.Herbst R, Wang Y, Gallagher S, Mittereder N, Kuta E, Damschroder M, Woods R, Rowe DC, Cheng L, Cook K, Evans K, Sims GP, Pfarr DS, Bowen MA, Dall'Acqua W, Shlomchik M, Tedder TF, Kiener P, Jallal B, Wu H, Coyle AJ. B-cell depletion in vitro and in vivo with an afucosylated anti-CD19 antibody. The Journal of pharmacology and experimental therapeutics. 2010;335(1):213–222. doi: 10.1124/jpet.110.168062. [DOI] [PubMed] [Google Scholar]
- 94.Forero-Torres A, Hamadani M, Sonet A, Verhoef G, Fanale M, Bello C, Goswami T, Huang W, Yao Z, Ibrahim R, Herbst R, Cheson BD. Phase 1/2 Study of MEDI-551, a Humanized Monoclonal Antibody Targeting CD19, in Subjects With Relapsed or Refractory Advanced B-cell Malignancies. ASCO Annual Meeting; Chicago. 2012. [Google Scholar]
- 95.Cheson BD, Pfistner B, Juweid ME, Gascoyne RD, Specht L, Horning SJ, Coiffier B, Fisher RI, Hagenbeek A, Zucca E, Rosen ST, Stroobants S, Lister TA, Hoppe RT, Dreyling M, Tobinai K, Vose JM, Connors JM, Federico M, Diehl V International Harmonization Project on L. Revised response criteria for malignant lymphoma. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2007;25(5):579–586. doi: 10.1200/JCO.2006.09.2403. [DOI] [PubMed] [Google Scholar]
- 96.Hallek M, Cheson BD, Catovsky D, Caligaris-Cappio F, Dighiero G, Dohner H, Hillmen P, Keating MJ, Montserrat E, Rai KR, Kipps TJ International Workshop on Chronic Lymphocytic L. Guidelines for the diagnosis and treatment of chronic lymphocytic leukemia: a report from the International Workshop on Chronic Lymphocytic Leukemia updating the National Cancer Institute-Working Group 1996 guidelines. Blood. 2008;111(12):5446–5456. doi: 10.1182/blood-2007-06-093906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Durie BG, Harousseau JL, Miguel JS, Blade J, Barlogie B, Anderson K, Gertz M, Dimopoulos M, Westin J, Sonneveld P, Ludwig H, Gahrton G, Beksac M, Crowley J, Belch A, Boccadaro M, Cavo M, Turesson I, Joshua D, Vesole D, Kyle R, Alexanian R, Tricot G, Attal M, Merlini G, Powles R, Richardson P, Shimizu K, Tosi P, Morgan G, Rajkumar SV International Myeloma Working G. International uniform response criteria for multiple myeloma. Leukemia. 2006;20(9):1467–1473. doi: 10.1038/sj.leu.2404284. [DOI] [PubMed] [Google Scholar]
- 98.Carter L, Knappertz V, Wang Y, Groves C, Ward E, Gallagher S, Yusuf I, Karnell J, Ettinger R, Rajan B, Herbst R. MEDI-551, A Novel Antibody That Depletes CD19+ B Cells: Rationale For Clinical Development In Multiple Sclerosis. ECTRIMS; Lyon: 2012. [Google Scholar]
- 99.Cepok S, Rosche B, Grummel V, Vogel F, Zhou D, Sayn J, Sommer N, Hartung HP, Hemmer B. Short-lived plasma blasts are the main B cell effector subset during the course of multiple sclerosis. Brain. 2005;128(Pt 7):1667–1676. doi: 10.1093/brain/awh486. [DOI] [PubMed] [Google Scholar]
- 100.http://clinicaltrials.gov/show/NCT01585766 N.
- 101.http://www.xencor.com/2010/12/xencor-and-morphosys-initiate-phase-1-study-of-anti-cd19-antibody-in-chronic-lymphocytic-leukemia/.