Abstract
Introduction:
Nowadays we are facing a steep increase in non-operative management throughout the injured body areas, with a continuous increase in the injuries' grade.
Objective:
To evaluate the safety and applicability of non-operative management in major trauma patients.
Methods:
Prospective observational study, in a level I trauma center, during 30 months. Inclusion criteria: major trauma patients with abdominal visceral lesions.
Results:
There were 207 major trauma patients whose average age was 35.8 ± 17.2 years, male being 69.6%. The most severe abdominal injuries were in the spleen (32.9%), the liver (19.2%) and the small bowel (11.6%). For the spleen lesions, the non-operative management was successful in 57.9% cases , with a failure rate of 11.6%. Non operative management was successful in 50% of liver injuries, its rate of success being independent of the hepatic injury grade.
Conclusions:
Selective non operative management of abdominal visceral injuries is safe and effective in major trauma patients. Nevertheless, we should stress that this type of protocol should be applied only by highly trained surgeons, able to early convert this management to difficult surgical strategies.
Keywords: trauma, non-operative management, polytrauma, abdominal injuries
INTRODUCTION
Nowadays, trauma meets the pandemic criteria, with a daily worldwide mortality as high as 16000 (1). While the mechanism and frequency of different specific injuries has changed during millennia, trauma remains an important cause of mortality and morbidity in modern society (2). Selective non operative management of significant abdominal injuries has represented one of the most important changes in the trauma patient care over the last decades (3). Starting with isolated pediatric splenic lesions (2), current literature states that one third of all abdominal gunshot wounds, including selected isolated liver and kidney gunshot injuries, can be successfully managed in a non-operative way (4). Khan et al. present a case of contained retrohepatical injury, after a single gunshot wound, in a hemodinamically stable patient, successfully managed in a non-operative way (5). For these torso gunshot wounds, clinical examination is essential for selecting patients with a need for emergency laparotomy. Due to the fact that all failures of non-operative management occur within 24 hours since hospital arrival, this seems to be the minimum required observation period before discharge (6). For high grade renal trauma, conservative management comes with a consistently decreased rate of nephrectomy, regardless of injury characteristics (7). Nevertheless, the trauma surgeons should be very skillful and trained to perform difficult surgeries because emergency laparotomy may be lifesaving, even with a similar mortality and morbidity rate as with non-operative management. Li Petri et al. present a mortality of 2% and a morbidity of 15.3% for complex liver resection, with a mortality of 2% for non-operative treatment and a morbidity of 17% (8). Paul et al. demonstrate that almost one-third of their blunt aortic injuries were safely managed non operatively, so they recommend selective non operative management for minimal aortic injuries (9). Publishing their institutional experience and reviewing the literature, Hamidian et al. conclude that non operative management is equally effective for traumatic major pancreatic duct transection, assuming that the management is individually based on clinical conditions (10). ❑
METHODS
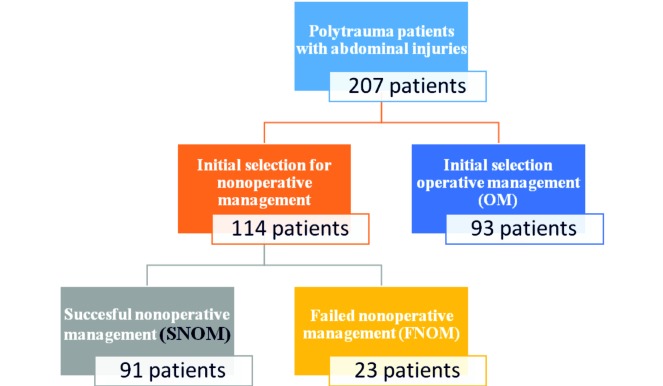
During 30 months (September 2008 – March 2011), we have prospectively included for the current study 207 major trauma patients. The inclusion criteria are: (1) Injury Severity Score ≥17 or two injuries with Abbreviated Injury Scale >2; (2) abdominal trauma revealed by clinical exam, abdominal ultrasonography or Computed Tomography. The only exclusion was: previous surgical procedures in another trauma center and subsequent referral. The main purpose was to define the safety of selective non operative management of abdominal visceral injuries in polytrauma patients. After the secondary survey the patients were divided into two groups: Non operative Management and Operative Management. During the in-hospital stay the patients were further divided in: Group 1 – Successful non operative management, Group 2 – Failed non operative management, Group 3 – Therapeutic laparotomy, Group 4 – Unnecessary/ Non-therapeutic laparotomy.
The statistical analysis was performed with IBM SPSS Statistics 19.0 software. The continuous variables are presented as mean ± standard deviation, and the categorical variables as percentage. We have used independent sample T-test or ANOVA for normal distributed data and Mann-Whitney or Kruskal-Wallis for nonparametric data. The statistical significance was declared when p <0.05. ❑
RESULTS
Out of 19806 trauma patients admitted in our level I trauma center during the study period, there were 207 (1%) major trauma patients. The mean age was 35.8±17.2 years, male patients being especially involved in all age groups (69.6%). The most frequent were blunt injuries (92.8%), assuming that penetrating trauma rarely fulfils the polytrauma criterion. The injuries were traffic related in 62% of cases, in 2% motorcycle related cases fall in 15%, human aggressions in 15.6%, occupational in 4.8% and self-inflicted injuries in 0.7%. Although all patients had abdominal trauma, the region with the highest Abbreviated Injury Scale was the abdomen in 57%, the head in 13.6%, the thorax in 13.6%, the extremity in 12.1% and the vertebral column in 3%. The most severe abdominal injury was the spleen – 32.9%, the liver – 19.2%, the small bowel – 11.6%, abdominal vascular – 11%, the diaphragm – 4.8%, the urinary bladder – 4.8%, the mesentery – 4.1%, the kidney – 3.4%, the duodenum – 3.4%, the colon – 2.7%, the rectum – 0.7%, the stomach – 0.7% and the gallbladder – 0.7%.
Figure 1. Study design.
The Glasgow Coma Scale (11) was strongly correlated with mortality and Intensive Care Unit admission (p = 0.000), but there was no correlation with the failure rate of non operative management (p = 0.47).
We have observed a higher Injury Severity Score for OM group than for SNOM and FNOM patents (p = 0.027).
Table 1
Table 1.
Injury Severity Score in study groups
| Injury Severity Score | ||||||
|---|---|---|---|---|---|---|
| Mean | Std. Deviation | 95% Confidence Interval for Mean | Minimum | Maximum | ||
| Lower Bound | Upper Bound | |||||
| SNOM | 27.76 | 10.781 | 25.50 | 30.01 | 17 | 57 |
| OM | 32.32 | 15.377 | 29.06 | 35.58 | 17 | 75 |
| FNOM | 25.96 | 11.933 | 20.80 | 31.12 | 17 | 57 |
| Total | 29.55 | 13.287 | 27.70 | 31.40 | 17 | 75 |
Liver trauma
There were 38 patients with liver injuries: 10 grade I, 12 grade II, 11 grade III and 5 grade IV, according to Organ Injury Scale of the American Association for the Surgery of Trauma (AAST). Non operative management was successful in 50%, 47.4% were surgically approached and a failed non operative management only in 2.6%. It is important to note that the non operative management was equally successful, independent of the hepatic injury grade.
Splenic trauma
Spleen was injured in 63.3% of patients, in 46.1% being the most severe abdominal trauma. There were 14.7% grade I, 44.2% grade II, 24.2% grade III, 15.8 grade IV and 1.1% grade V splenic injuries. The non-operative management was successful in 57.9%, with a failure rate of 11.6%. ❑
DISCUSSION
The polytrauma patients represent the ultimate challenge for trauma care, due to their broad spectrum of injured organs and clinical scenarios. Although the "polytrauma" term is frequently used, especially in European literature, there is no universally accepted and evidence based definition (12). According to Trentz, the definition for "polytrauma" used for the current study was: "a syndrome secondary to multiple trauma, exceeding a defined severity (Injury Severity Score ≥27), with a consecutive systemic inflammatory response syndrome for at least 24 hours, generating dysfunction or failure of remote, uninjured organs or systems" (13). According to Butcher and Balogh the practicability of including SIRS into the definition of polytrauma as a surrogate for physiological derangement appears questionable (14). The same authors conclude that the "Abbreviated Injury Score >2 in at least two body regions" definition for polytrauma captures the greatest percentage of the worst outcomes and has a higher accuracy and precision in defining polytrauma than Injury Severity Score >15 or >17 (15). In polytrauma patients, Zwingmann et al. found the following distribution of the regions with an Abbreviated Injury Scale greater than 2: severe cranial trauma – 37%, severe thoracic trauma – 54%, abdominal trauma – 31%, pelvic trauma – 28%, upper limbs – 43% and lower limbs – 33% (16). In the current study, the mechanism of injury was by blunt trauma, but the trauma surgeon should actively search the trauma scenario because only a high suspicion for potential injuries may increase their early diagnosis and consequent treatment (17). An important difference between liver and splenic injuries is that liver injury grade does not correlate with the failure rate of the non-operative management. Navsaria et al. concluded the same thing regarding non operative management of liver gunshot injuries (18). The indication for non-operative management are continuously evolving, Liu et al. present 12 patients with delayed splenic rupture managed non surgically, with a success rate of 83% (19). Petrowsky et al. analyzing 468 patients with liver trauma conclude that the integration of Computed Tomography in early trauma-room management and the shift to non-operative management in hemodynamically stable patients resulted in an improved survival rate and should be the gold standard for liver trauma (20). Van der Wilden et al. present a success rate of 91.3% for non-operative management in grade 4 and 5 liver injuries, only 6.5% of patients requiring delayed operation, without experiencing life-threatening complications because of delay (21).
For splenic injuries, the benefits of non-operative management seem to be: lower morbidity and mortality, lower early infections rate, the avoidance of a non-therapeutic laparotomy, the avoidance of early or late complications related to laparotomy, decreased blood transfusions, decreased in hospital stay and the maintenance of the immunological function and prevention overwhelming postsplenectomy infection (22). According to our results, Bhullar et al. did not find any correlation between people over 55 years and the outcomes of non-operative management of blunt splenic injuries (23). ❑
CONCLUSIONS
Selective non operative management of abdominal visceral injuries is safe and effective in major trauma patients. Nevertheless, we should stress that this type of protocol should be applied only by highly trained surgeons, able to early convert this management to difficult surgical strategies. An equally important role is occupied in the trauma team by an imagist and a dedicated interventional radiologist. Due to a steep increase in non-operative management throughout the injured body areas, we feel that the trauma education program should vary the methodology of learning for emergency surgical procedures.
CONFLICT OF INTEREST
none declared.
FINANCIAL SUPPORT
none declared.
References
- 1.Paun S, Beuran M, Negoi I, et al. Trauma--epidemiology: where are we today? Chirurgia (Bucur) 2011;106:439–443. [PubMed] [Google Scholar]
- 2.Beuran M, Negoi I, Paun S, et al. History of trauma care. Chirurgia (Bucur) 2011;106:573–580. [PubMed] [Google Scholar]
- 3.Beuran M, Negoi I, Paun S, et al. Selective nonoperative management of solid abdominal visceral lesions. Chirurgia (Bucur) 2010;105:317–326. [PubMed] [Google Scholar]
- 4.Navsaria PH, Edu S, Nicol AJ. Nonoperative management of pelvic gunshot wounds. Am J Surg. 2011;201:784–788. doi: 10.1016/j.amjsurg.2010.03.014. [DOI] [PubMed] [Google Scholar]
- 5.Khan IR, Hamidian Jahromi A, Khan FM, et al. Nonoperative management of contained retrohepatic caval injury. Ann Vasc Surg. 2012;26:420e429–412. doi: 10.1016/j.avsg.2011.05.042. [DOI] [PubMed] [Google Scholar]
- 6.Inaba K, Branco BC, Moe D, et al. Prospective evaluation of selective nonoperative management of torso gunshot wounds: when is it safe to discharge? J Trauma Acute Care Surg. 2012;72:884–891. doi: 10.1097/TA.0b013e31824d1068. [DOI] [PubMed] [Google Scholar]
- 7.Jacobs MA, Hotaling JM, Mueller BA, et al. Conservative management vs early surgery for high grade pediatric renal trauma--do nephrectomy rates differ? J Urol. 2012;187:1817–1822. doi: 10.1016/j.juro.2011.12.095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li Petri S, Gruttadauria S, Pagano D, et al. Surgical management of complex liver trauma: a single liver transplant center experience. Am Surg. 2012;78:20–25. [PubMed] [Google Scholar]
- 9.Paul JS, Neideen T, Tutton S, et al. Minimal aortic injury after blunt trauma: selective nonoperative management is safe. J Trauma. 2011;71:1519–1523. doi: 10.1097/TA.0b013e31823b9811. [DOI] [PubMed] [Google Scholar]
- 10.Hamidian Jahromi A, D'Agostino HR, Zibari GB, et al. Surgical Versus Nonsurgical Management of Traumatic Major Pancreatic Duct Transection: Institutional Experience and Review of the Literature. Pancreas. 2013;42:76–87. doi: 10.1097/MPA.0b013e3182575cf9. [DOI] [PubMed] [Google Scholar]
- 11.Beuran M, Negoi I, Paun S, et al. Trauma scores: a review of the literature. Chirurgia (Bucur) 2012;107:291–297. [PubMed] [Google Scholar]
- 12.Butcher N, Balogh ZJ. The definition of polytrauma: the need for international consensus. Injury. 2009;40(Suppl4):S12–22. doi: 10.1016/j.injury.2009.10.032. [DOI] [PubMed] [Google Scholar]
- 13.Trentz O. In: AO Principles of Fracture Management. edn. Edited by Ruedi T, Buckley R, Moran C. Stuttgart. New York Thieme; 2007. Polytrauma: pathophysiology, priorities and management. pp. 337–347. [Google Scholar]
- 14.Butcher NE, Balogh ZJ. The practicality of including the systemic inflammatory response syndrome in the definition of polytrauma: Experience of a level one trauma centre. Injury. 2013;44:12–7. doi: 10.1016/j.injury.2012.04.019. [DOI] [PubMed] [Google Scholar]
- 15.Butcher N, Balogh ZJ. AIS>2 in at least two body regions: a potential new anatomical definition of polytrauma. Injury. 2012;43:196–199. doi: 10.1016/j.injury.2011.06.029. [DOI] [PubMed] [Google Scholar]
- 16.Zwingmann J, Schmal H, Südkamp NP, et al. Verletzungsschwere und -lokalisationen polytraumatisierter Kinder im Vergleich zu Erwachsenen und deren Bedeutung für das Schockraummanagement. Zentralbl Chir. 2008;133:68–75. doi: 10.1055/s-2008-1004661. [DOI] [PubMed] [Google Scholar]
- 17.Beuran M, Negoi I, Paun S, et al. (Mechanism of injury--trauma kinetics. What happened? How?). Chirurgia (Bucur) 2012;107:7–14. [PubMed] [Google Scholar]
- 18.Navsaria PH, Nicol AJ, Krige JE, et al. Selective nonoperative management of liver gunshot injuries. Ann Surg. 2009;249:653–656. doi: 10.1097/SLA.0b013e31819ed98d. [DOI] [PubMed] [Google Scholar]
- 19.Liu PP, Liu HT, Hsieh TM, et al. Nonsurgical management of delayed splenic rupture after blunt trauma. J Trauma Acute Care Surg. 2012;72:1019–1023. doi: 10.1097/TA.0b013e3182464c9e. [DOI] [PubMed] [Google Scholar]
- 20.Petrowsky H, Raeder S, Zuercher L, et al. A quarter century experience in liver trauma: a plea for early computed tomography and conservative management for all hemodynamically stable patients. World J Surg. 2012;36:247–254. doi: 10.1007/s00268-011-1384-0. [DOI] [PubMed] [Google Scholar]
- 21.van der Wilden GM, Velmahos GC, Emhoff T, et al. Successful nonoperative management of the most severe blunt liver injuries: a multicenter study of the research consortium of new England centers for trauma. Arch Surg. 2012;147:423–428. doi: 10.1001/archsurg.2012.147. [DOI] [PubMed] [Google Scholar]
- 22.Beuran M, Gheju I, Venter MD, et al. Non-operative management of splenic trauma. J Med Life. 2012;5:47–58. [PMC free article] [PubMed] [Google Scholar]
- 23.Bhullar IS, Frykberg ER, Siragusa D, et al. Age does not affect outcomes of nonoperative management of blunt splenic trauma. J Am Coll Surg. 2012;214:958–964. doi: 10.1016/j.jamcollsurg.2012.03.007. [DOI] [PubMed] [Google Scholar]