Abstract
Rehabilitation service providers in rural or underserved areas are often challenged in meeting the needs of their complex patients due to limited resources in their geographical area. Recruitment and retention of the rural clinical workforce are beset by the ongoing problems associated with limited continuing education opportunities, professional isolation, and the challenges inherent to coordinating rural community healthcare. People with disabilities who live in rural communities also face challenges accessing healthcare. Traveling long distances to a specialty clinic for necessary expertise is troublesome due to inadequate or unavailable transportation, disability specific limitations, and financial limitations. Distance and lack of access are just two threats to quality of care that now being addressed by the use of videoconferencing, information exchange, and other telecommunication technologies that facilitate telerehabilitation. This white paper illustrates and summarizes clinical and vocational applications of telerehabilitation. We provide definitions related to the fields of telemedicine, telehealth, and telerehabilitation, and consider the impetus for telerehabilitation. We review the telerehabilitation literature for assistive technology applications, pressure ulcer prevention, virtual reality applications, speech-language pathology applications, seating and wheeled mobility applications, vocational rehabilitation applications, and cost-effectiveness. We then discuss external telerehabilitation influencers, such as the positions of professional organizations. Finally, we summarize clinical and policy issues in a limited context appropriate to the scope of this paper.
Keywords: Telerehabilitation, Telehealth, Telemedicine, Telepractice
Introduction
Telerehabilitation is an emerging field that is growing rapidly and becoming a significant segment of telemedicine and e-health. Advancements in Internet technologies and the availability of broadband connections in most homes and workplaces have expanded telerehabilitation services that were previously too expensive to deliver. The technologies can potentially bring a new paradigm to the way telerehabilitation is delivered and managed. This paper presents a systematic review of the nature of the emerging field of telerehabilitation from the perspective of health information management and informatics infrastructure.
Telerehabilitation (TR) is the application of telecommunication technology for supporting rehabilitation services (Russell, 2007). The nature of rehabilitation services determines the type of telecommunication technology and informatics infrastructure used to support the services. The rehabilitation process typically needs continuous and frequent monitoring of the patient’s functionality in order to test the delivered therapy and/or adapt it to the patient’s progress. This is different than the typical telemedicine service that involves a short intensive session with one or more clinicians and a patient.
Review of Science: Telerehabilitation Infrastructure
Almost all published works on TR focus on the clinical application of a technology to deliver a specific rehabilitation service over a distance. Reviewing these clinical applications will provide us with a state-of-the-art of the underlying informatics infrastructure of TR services. It is important to note that advances in health informatics are often first presented and published as conference proceedings before publication in peer-reviewed journals that usually lag about two years behind. The field of TR exists under the assumption that the barrier of distance can be minimized to enhance access that will open new possibilities for delivering intervention strategies across the continuum of care. Minimizing the barrier of distance can be accomplished through several modes of telecommunications, including voice, video, and virtual reality.
Previously, TR was viewed as a field that focuses heavily on real-time interactivity (synchronous interaction) rather than the store-and-forward approach (asynchronous interaction) (Winters, 2002). As a result, most studies and developments focus on inventing devices that can mimic face-to-face interactivity in a tele-setting. However, implementing the results of the study in a real clinical setting has proven to be difficult due to the limitation of resources and the limited availability of the devices.
A systematic approach to analyzing TR services is needed to understand the underlying infrastructure requirements to support the service. We will use a conceptual model of TR service delivery developed by Winters (2002) that is still relevant today. He proposed four conceptual models: teleconsultation, telehomecare, telemonitoring, and teletherapy. We will use this conceptual model to systematically review the current state-of-the-art of telerehabilitation services.
We reviewed papers that have been published in the past two decades in the area of TR. We conducted a search in the Medline (PubMed) database using the following keywords: telerehabilitation, telemonitoring, telehomecare, teleconsultation, and teletherapy. Aside from the keyword telerehabilitation, all other keywords can be used to find papers that are not related to TR. For example, using the keyword teleconsultation, 2,069 papers were retrieved from the PubMed database. To achieve better precision without sacrificing recall, we combined the last four keywords with the keyword rehabilitation. Then, the numbers of papers retrieved are as follows: telerehabilitation (93), teleconsultation and rehabilitation (129), telehomecare and rehabilitation (5), telemonitoring and rehabilitation (37), teletherapy and rehabilitation (4). In addition, field specific keywords, such as “teleSLP,” “telePT,” “teleophthalmology,” and “teleneuropsychology” were also used to query the database; however, we found that the search results with these keywords were already included in the broader keywords. We further refined the retrieved document to achieve perfect precision by reviewing the abstracts of the papers and included only the papers that related to rehabilitation services. We further evaluated the content of the papers to reclassify them into more accurate TR service categories. The result is 238 papers with the categories presented in Table 1.
Table 1.
TR Services in the Past Decade
| Teleconsultation |
| Number of papers: 61 |
| Prototypical example: Schein et al., (2009) |
|
|
| Telemonitoring |
| Number of papers: 36 |
| Prototypical example: Paré, Jaana, & Sicotte, (2007) |
|
|
| Telehomecare |
| Number of papers: 36 |
| Prototypical example: Hoenig et al., (2006) |
|
|
| Teletherapy |
| Number of papers: 60 |
| Prototypical example: Sugarman, Dayan, Weisel-Eichler, & Tiran, (2006) |
|
|
| Telerehabilitation Service: Other |
| Number of papers: 45 |
Teleconsultation
Winters (2002) defined teleconsultation as a standard “face-to-face” telemedicine model using interactive videoconferencing between a local provider (and client) and a remote rehabilitation expert to gain access to specialized expertise. Of 238 papers we reviewed, 61 of them are related to teleconsultation. We will use two applications to represent the teleconsultation service delivery model: Assistive Device Teleprescription and Expert Teleaccess.
Assistive Device Teleprescription is a clinical application of teleconsultation where rural clinics expand the availability of therapists by including expert therapists from the metropolitan area. The assistive device prescribed ranges from orthoses and wheelchairs to augmentative communication devices (Lemaire, Necsulescu, & Greene, 2006). In the wheelchair remote prescription system, an expert therapist can join the wheelchair assessment and fitting process via a videoconference system (Schein et al., 2009).
The second application, Expert Teleaccess is a teleconsultation service delivery where rural physical therapists can tap into the expertise of specialized therapists in other clinics or hospitals. The process is initiated by transmitting movement pictures of the client to an expert therapist in the metropolitan hospital. After analyzing the movement pictures, the expert therapist provides inputs on the treatment plan for the client. Then, the rural therapist finalizes the treatment plan by combining the input from the expert with the client’s preferences (Iwatsuki, Fujita, Maeno, & Matsuya, 2004).
Telehomecare
Telehomecare is defined as service delivery where a clinician (usually a nurse or technician) coordinates a rehabilitation service delivery from various providers to the client’s home. We will briefly review three clinical applications that represent a telehomecare service delivery model: in-home teletraining, home modification teleassessment, and a telesupport network.
In the in-home teletraining application, clients, with the help of a technician, train in activities of daily living (ADL) tasks at the client’s home. Hoenig et al., (2006) describe the protocol developed for delivering in-home teletraining for adults with mobility impairment. The training session utilizes a camera connected to a standard videophone line, allowing the therapist to monitor the process in real-time, remotely. Feedback from the therapist is carried back through the audio line. The client side utilizes a wireless headset to receive the audio feedback, allowing the clients to move freely in their training session.
Home modification teleassessment is a clinical application of telehomecare that allows an architect/accessibility expert to evaluate the accessibility of a client’s home (Sanford et al., 2006). In this application, technicians are sent to the client to capture specific images of the client’s home. The images are uploaded and analyzed remotely by an architect/accessibility expert. Kim & Brienza (2006) extended the approach further by building 3D models of the client’s home to allow virtual navigation. Based on the models, the architect/accessibility expert provides a set of recommendations to make the home more accessible.
Telesupport network is a clinical application of telehomecare that provides ongoing/lifetime support for the client via a network of healthcare resources. Generally, the network provides a web-based care coordination system that enables homecare staff to interact with providers from acute rehabilitation sites. Additionally, some networks also supplement general information about homecare, rehabilitation, and other education resources. The network is built to answer specific factors that were identified as problems for rural clients, including: medication noncompliance; social isolation and inadequate supervision; limited access to specialty services; and lack of communication between the homecare agency and hospital (Demiris, Shigaki, & Schopp, 2005). The network can also connect peers with similar rehabilitation needs (Schopp, Hales, Quetsch, Hauan, & Brown, 2004).
Telemonitoring
Telemonitoring is the clinical application wherein the rehabilitation provider sets up unobtrusive monitoring or assessment technology for the client. Some telemonitoring approaches allow a limited degree of interactivity between the client and the provider via the device. Telemonitoring is perhaps one of the biggest areas of telerehabilitation with the potential for growing even larger. This is due to the availability of inexpensive and nonintrusive environmental sensors that can be placed at home and because of the advancement of wireless networks. Two clinical applications will be used as examples: home/independent-living telemonitoring and job telecoaching.
Home and independent-living telemonitoring uses a range of devices, from a simple emergency call button to sophisticated home sensors. The goal of this telemonitoring application is to allow clients to live independently while their health and safety are monitored remotely by health-care providers (Paré, Jaana, & Sicotte, 2007).
In job telecoaching, an automated agent that is capable of providing instant feedback is coupled with the client as a partner. The device is programmed to identify missing steps or false movements of the client. By creating a model of the client’s movement and comparing the model with the correct movement model stored inside the device, instant feedback can be produced to remind the client of the missing or false movement.
Teletherapy
Arguably the most visible application of TR services, teletherapy is defined as a model of TR service delivery wherein the client conducts therapeutic activities in the home setting using the course of therapy managed by a therapist remotely. The therapist generally has the ability to modify the therapy setting. The process of modification can be done synchronously or asynchronously. Three clinical applications are reviewed to represent teletherapy: teleneuro/orthopedic-rehabilitation, teleaudiology/teleSLP, and postsurgical teletraining.
Teleneuro/orthopedic-rehabilitation is the clinical application where neural/orthopedic-related rehabilitation therapy is delivered remotely. This clinical application category includes post-stroke TR service, traumatic brain injury (TBI) TR service, and orthopedic TR service. Feng & Winters (2007) combined an off-the-shelf force feedback joystick with instant messaging and videoconferencing to create computer-based assessment tools for neurorehabilitation. Computer-based assessment tools have the advantage of providing instant evaluations of therapy performance that is useful for therapy optimization purposes. Goals of the computer-based tools (such as game achievements and targets) can serve as a key motivational tool for conducting the therapy consistently over time. Moreover, computer based tools can provide digital metrics with a higher sensitivity to a client’s subtle changes (including range of motion and pressure strength) compared to traditional clinical assessment scales. Virtual reality is also utilized as tools to provide TR service. Virtual gloves (Placidi, 2007) and haptic devices are used to provide force-feedback, allowing a client to interact with an immersive virtual reality environment in the therapy session.
Teleaudiology/TeleSpeech-Language-Pathology (TeleSLP) is the clinical application to provide speech-language therapy and audiology services over a distance. TeleSLP can utilize both synchronous and asynchronous communication modes. Real-time interaction is used to identify facial gestures and expressions while the store-and-forward method is used to send numerical data to the therapist. Additionally, video can be stored and forwarded to provide a higher-quality video recording without the need for high bandwidth (Hill et al., 2006). By using the store-and forward method, metrics of data can be aggregated and analyzed to deliver personalized therapy for the client.
Postsurgical teletraining is the clinical application to deliver remote rehabilitation after a surgical process. Rehabilitation for postsurgery interventions concentrates on regaining range-of-motion, strength, and relieving sensitivity in the surgical area (Heuser et al., 2007). Similar to the Teleneuro/orthopedic-rehabilitation, virtual reality is utilized in providing remote training for the client. However, postsurgical teletraining generally focuses more on the continuity of self-training and requires less real-time interactivity with the therapist. Data can be uploaded periodically and aggregated in the server for the therapist.
Telerehabilitation from an Informatics Perspective
Defining the relationships between telemedicine and other related areas is important in order to design an optimal IT infrastructure. In stricter terms, telemedicine is usually defined as the delivery of clinical services. Since TR may involve the delivery of clinical services such as in teletherapy, TR intersects with telemedicine. The rest of the TR models fall under telehealthcare or e-health, the term used to refer to the management of disability and health.
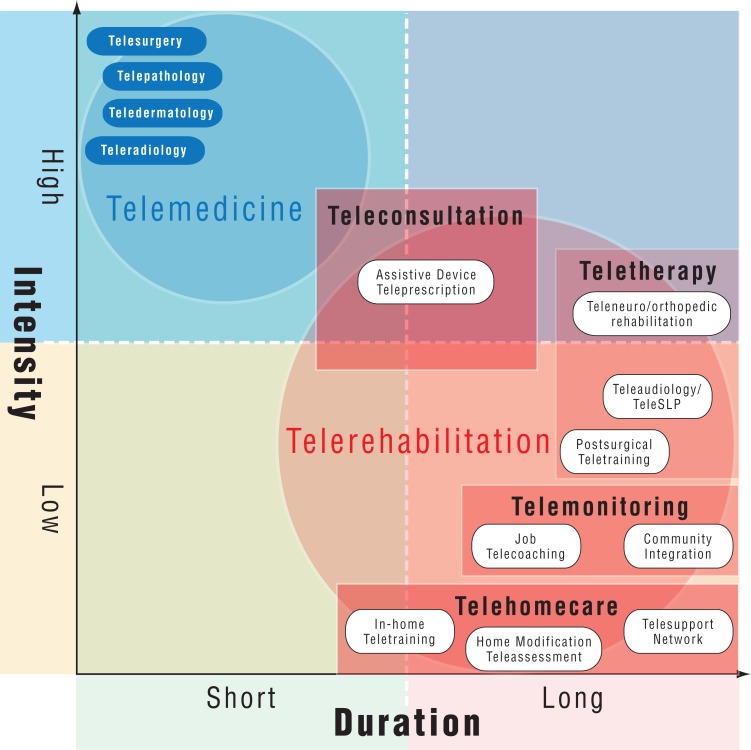
The field of telemedicine can be mapped into four quadrants based on the axes of intensity and duration of the clinical service delivery. The intensity is the amount of information exchanged (usually measured by the size of the files used, speed/resolution of the video required, etc.) among the participants in the telemedicine process. The intensity ranges from high intensity, such as the case with tele-surgery, to low intensity, such as in-home rehabilitation. The high intensity services such as telesurgery usually require a very high-quality real-time video connection between two sides and an extremely high-speed connection between two sides to allow real-time manipulation of commands or objects on the remote side. Low intensity telemedicine services can be delivered by using a plain old telephone service (POTS). On the duration axis, the service ranges from short duration service to long term or lifetime service. An example of a short duration service is tele-radiology that typically consists of a one-time diagnosis by a remote radiologist on the images sent by a hospital. An example of long duration service is community integration of persons with disabilities or the management of stroke/SCI recovery.
Figure 1 illustrates many telemedicine services mapped into the intensity-duration axes. Traditional telemedicine such as teleradiology and telepathology mostly falls into the high intensity – short duration quadrant. These services require very high-speed and very reliable connections between two sides. These services usually involve a short, one-time encounter that either does not repeat or only repeats a few times. Telerehabilitation services are mostly in the low intensity – long duration quadrant. For example, rehabilitative retraining after surgery usually involves low intensity monitoring and a course of therapy prescribed by healthcare providers. Telerehabilitation services, however, usually require repetitive encounters over a long period of time.
Figure 1.
Map of telemedicine services in Intensity-Duration quadrant model
The quadrant model is used to analyze the service delivery, not the mode of data transmission (store-forward or synchronous) nor the data transmission speed. Intuitively, low-intensity services can be delivered via low-speed connections such as the POTS (Plain Old Telephone System). However, more and more low-intensity services are delivered via high-speed connections to achieve better quality of service. On the other hand, limitations on bandwidth may require high-intensity services to be delivered using low-speed connections, such as the store-and-forward method that does not require live interactivity. Teleradiology is an example of high-intensity service that doesn’t require synchronous communication and often can be conducted via the store-and-forward method.
Telerehabilitation shares many features of chronic disease management. In chronic disease management, the service focuses on monitoring the patient over long periods of time. Similarly, the client in telerehabilitation needs the service for a long period of time, with many requiring a lifetime service. The interaction and communication in both chronic disease management and telerehabilitation are usually of low intensity. Therefore, chronic disease management can be categorized into the low intensity – long duration quadrant. In contrast, traditional telemedicine shares the characteristic of acute disease management: intense, but short.
Most telerehabilitation services share many similarities with chronic disease management, thus placing them into the low intensity – long duration quadrant. However, unlike chronic disease management, telerehabilitation services may move around in the quadrant based on the availability of informatics resources (such as technology, bandwidth, and human resources) and the need for the services. For example, prior to the Internet boom, most telerehabilitation services were delivered via POTS because POTS was the only available network of telecommunication in many areas. However, the very same telerehabilitation services may now be delivered in two modes: simple telemonitoring can be conducted over low-speed connections, while intensive assessment sessions can be conducted over high-speed connections to provide real-time interactivity between provider and client.
There is a dynamic interaction between infrastructure and services in TR: the availability of infrastructure affords new services and the need for services can stimulate the development of new infrastructure. Developing a conceptual model of TR services is important because unlike telemedicine, TR is an emerging field and is much more diverse. This model will allow us to define the difference and the relationships among TR, telemedicine, telehealth, e-health, etc. From the information technology (IT) standpoint, a systematic review of the advances in IT is important in order to understand the optimal IT infrastructure for TR and to project what TR services will look like in the future.
The service deliveries in each of the four quadrants demand different types of IT infrastructure and bandwidth requirements. A typical infrastructure for a teleconsultation is a videoconferencing over a high-bandwidth network, while telehomecare typically requires only low to moderate bandwidth. Telemonitoring and teletherapy usually require moderate to high bandwidth. The long duration of service for telerehabilitation requires an informatics infrastructure that allows the management of the client’s data over a long period of time. For example, the informatics requirement for telerehabilitation services includes maintaining a longitudinal health record and supporting a course of treatment over time.
The telemedicine quadrant model can be used to analyze many issues in telemedicine. For example, the quadrant can be used to analyze similarities among telemedicine services and to analyze how certain technologies can be used across different telemedicine services. The quadrant model can also be used to explain why certain TR services that have been developed in research are difficult to deploy. For example, the telecoaching service is difficult to implement because it is a high-intensity, high-bandwidth service. We can identify the IT infrastructure requirements for the four models of service based on the Intensity-Duration Quadrant model of TR.
Low Intensity - Long Duration (LI-LD) Quadrant
Most TR services fall into the LI-LD quadrant. The services in this quadrant are characterized by low-intensity interaction between client and healthcare provider/therapist, but are conducted over a long period of time. Telehomecare and Telemonitoring are two typical TR service delivery models that fit into this quadrant. Services with low-intensity interactions do not require high-bandwith and can be delivered directly to clients at home.
The requirement for this quadrant is an infrastructure that allows retention of rehabilitation data over a long period of time on a low- to medium-bandwidth connection (common household connection).
Asynchronous IT infrastructure is used by a significant number of rehabilitation service deliveries in the LI-LD quadrant. Asynchronous communication stores and forwards rehabilitation data to therapists, which allows data retention over a long period of time. In asynchronous communication models that have been used in the past for at-home TR projects, large data files are transmitted in small chunks over low to medium bandwidth channels, allowing the infrastructure to be deployed over a common household connection.
A wide array of devices is utilized to capture the data at the client’s side in the LI-LD quadrant, ranging from a simple emergency call button to automated monitoring robots. Therefore, the asynchronous IT infrastructure also requires a network that supports multimodal data and can be interfaced easily with the devices. Almost all networks can support asynchronous communication. POTS, wireless networks, and the Internet are great candidates to deploy the asynchronous IT infrastructure. POTS has the advantage of availability and simplicity. Wireless networks can be accessed from anywhere, thus having the advantage of accessibility. The Internet has the advantage of multimodal sophistication and access to web-based health resources.
High Intensity - Short Duration (HI-SD) Quadrant
The services in this quadrant are characterized by a very intensive interaction between client and provider, conducted over a short period of time. From the information flow perspective, it flows in a burst. In essence, the TR services in this quadrant are similar to the traditional telemedicine services. We identified one service delivery model that falls into this quadrant: intensive teleconsultation. Most of the services in this quadrant are conducted at clinical settings, connecting rural and metropolitan area clinics. Therefore, the requirement for this quadrant is an infrastructure that allows high intensity, interactive communication over a short period of time. Due to the setting, the bandwidth needed can range from medium to high speed connections.
Synchronous IT infrastructure fits with the requirements of the HI-SD quadrant. High-quality videoconference systems combined with interaction tools are necessary to allow effective communication in a teleconsultation. The level of interaction needed varies between clinical applications. Assistive device teleprescription generally requires a high level of interactivity such as high-quality videoconferencing, which allows a real-time assessment of the client remotely. On the other hand, depending on the field, expert teleaccess can be built over an infrastructure with less level of interactivity.
High quality video and audio systems are a necessity for the HI-SD quadrant. The video/audio systems are utilized to show detailed aspects either of the client or the therapy materials. Additionally, the video/audio systems are also used as communication tools allowing feedback from therapists to be given in a timely manner. Therefore, a very high-speed and reliable network is required for the IT infrastructure to support services in this quadrant. A dedicated network (ATM, ISDN) and the Internet are great candidates for the IT infrastructure in this quadrant. A dedicated network has the advantage of reliability and can support all types of communication. The main disadvantages of a dedicated network are the cost of the device and the network, and the proprietary nature of the technology. The Internet has the advantage of low cost and an open system that can be easily integrated with other components of IT infrastructure. However, reliability and security issues require that Internet deployment be conducted with extra precautions.
High Intensity - Long Duration (HI-LD) Quadrant
The services in this quadrant are characterized by an intense interaction between client and healthcare provider/therapist, and, although the sessions are generally short, the service consists of many sessions conducted over a long period of time. We identified one service delivery model for this quadrant: teletherapy. The settings of TR services for the HI-LD quadrant can range from a client’s home to a clinical setting. Most TR services in the HI-LD quadrant utilize both modes of communication. Therefore, the requirement of this quadrant varies based on the type of therapy. Therapies relying on videoconferences generally need a high intensity infrastructure with medium to high bandwidth, while therapies relying on the store-and-forward approach can often make use of a low intensity infrastructure with medium to low bandwidth.
A flexible computer network that allows integration of systems is necessary to support the HI-LD quadrant as most of the services utilize both modes of communication. Any network that has the capability of integrating synchronous and asynchronous applications is required to implement the HI-LD quadrant infrastructure. The Internet becomes a great candidate to deploy the HI-LD quadrant. Although it requires certain measures to ensure reliability and security, the Internet has the advantage of flexibility and scalability, allowing modules to be integrated seamlessly in a computer-based solution.
EMERGING ISSUES AND CHALLENGES
As telerehabilitation and homecare become popular due to the availability of technologies and the economic potential of reducing the cost of services, TR can potentially increase access to care. Access is increasingly important in light of the shortage of clinicians and the increased aging population. TR also brings emerging issues and challenges that need to be recognized and addressed. We will review four notable challenges: the management of complex health information, privacy/confidentiality issues, the need to design a consumer-centered system, the need for evidence-based practice.
Complex health information
Rehabilitation service is characterized by repetitive encounters over a long period of time. In some cases, a stream of videos is recorded for every encounter. In a face-to-face rehabilitation session, this type of information is not recorded. For example, during a neuropsychological assessment, the entire session between patient and therapist is not recorded; only the assessment from the therapist will be recorded. During a wheelchair prescription session, the session between ATP and the prospective wheelchair users are not recorded. However, in telerehabilitation, the entire session, including the detailed activities, is captured by the video system that links the therapist with the remote patient.
Since TR encounters are repetitive over long periods of time, the information accumulated from every encounter needs to be stored and organized to allow the therapists to view the information easily. Managing a wealth of information in a complex form (such as video, sound, text, and still images) poses a new challenge in telerehabilitation. Determining which information is most important will determine the success of future telerehabilitation. The field of visualization and human-computer interface will be very useful to solve these challenges.
The recording of entire sessions might also create opportunities that previously did not exist. For example, currently students have to shadow therapists to learn how to perform clinical sessions. The availability of the sessions in video can be used to educate future therapists and as an educational repository to enhance and supplement the current clinical education of therapists. There is also a potential for bringing the field of data mining to characterize the wealth of data that previously has not been available.
Privacy/Confidentiality Issues
Imagine a video of psychological therapy from a telerehabilitation session is stolen and posted on the Internet. The results will be very damaging to the patient and to the credibility of telerehabilitation services. Telerehabilitation services bring more challenges to privacy and confidentiality issues compared to face-to-face rehabilitation due to the fact that, in the future, it will be more common to have the entire session of rehabilitation therapy either recorded or captured over the Internet, while such sessions in face-to-face therapy leave no trail beyond the therapy room. The availability of digital versions of the detailed therapy session can potentially bring opportunities for research and education, but also can create more challenges in terms of privacy/confidentiality. As all medical fields begin to move toward electronic medical records, consumers will gradually become more comfortable with technology-enabled healthcare. However, it is important that TR systems be developed in such a way that all users feel as comfortable and secure using them as they do when seeing a clinician in person.
Consumer-Centered Telerehabilitation Services
The convergence of TR services with the Internet will bring TR services closer to the consumer. Unlike telemedicine in the past, the users of future TR systems will be the public, rather than healthcare professionals. That is, clients will independently use the system to access the course of treatment or to record data. This will bring new challenges to the design and development of TR infrastructure. Unlike healthcare professionals, public users may be more dynamic, moving from one healthcare system to another according to their needs and personal preferences. Therefore, the client’s data has to be able to follow the individual. The need for health data to follow individuals will force different systems to interface with each other. The client’s data and information will have to flow from one system to another in order to ensure the integrity and the completeness of the client’s health status.
The Need for Evidence-based Practice in Telerehabilitation
Although TR has been used to deliver rehabilitation services to many underserved areas, the evidence of TR’s effectiveness still does not reflect the reality of current practices. A quick search of popular Internet-search engines reveals hundreds of different rehabilitation centers across the world that acknowledges the use of TR in their practices. However, most centers still focus on developing the technology to deliver TR instead of performing studies to measure the efficacy and effectiveness of TR. The lack of evidence results in slow adoption of TR by healthcare administrators and policy makers, which limits the reimbursment available for TR. In addition, most technologies are developed without great consideration of the human factors, which hampers the translation of technologies from a research project into a consumer product.
Emerging Technologies And Opportunities
Similar to other industries, advancements in Internet technologies provide potential and opportunities for changing the landscape of telerehabilitation services in the future. Among notable advancements that can potentially be a considerable force are: the availability of very high-bandwidth in most households and offices; the advent of Web 2.0 technologies that can bring integration to TR services; and, the push toward consumer empowerment and ownership of personal health information. These forces will shape the development of telerehabilitation services and infrastructure in the next decade.
The advent of Web 2.0 provides potential technologies to build a platform to deliver TR services. Through the use of these technologies, multiple information and collaboration features can be integrated into a single application built on top of the Internet. In addition, the increasing availability of bandwidth allows heavy, high-bandwidth applications to be developed and delivered through the Internet. With the high rate of Internet penetration in rural areas, building the application over the Internet also increases the accessibility of the solution to both metropolitan and rural areas.
Following this advancement, there is a growing trend that all the branches of telehealth (telemedicine, telehealthcare, and e-health) be integrated into a single mode of service. The concept of providing “single-entry” to the system that supports the service has been viewed as an efficient way to provide complete information about the client to healthcare providers. The current sophistication of Internet services and the speed of networks allow this integration where it was not afforded in the past decade. For example, real-time videoconferencing can be integrated with clinical information systems or other information management systems, allowing healthcare providers to get real-time feedback on the client’s condition while assessing and making decisions about the client’s therapy.
Availability of High-bandwidth, High-Definition Technologies
By the end of 2006, the penetration of broadband connections among Internet users in the United States was estimated to reach 80%, while more than 90% of US workers used broadband (Madden, 2006). Extrapolating the current trend, as the broadband penetration among Internet users is almost universal, the category for future bandwidth may no longer be between broadband (56Kbit or higher) and regular telephone lines (56 Kbps or less), but between many forms of broadband. Already, the current speed of broadband access in the US is 384 Kbps or higher, with Cable providing connections with a speed between 384 Kbps - 1.5 Mbps (both downstream and upstream) and a Digital Subscriber Line (DSL) providing a speed between 768 Kbps -5 Mbps (downstream) and 384–768 Kbps (upstream). New DSL technology on top of fiber optics (e.g. Verizon FiOS) connections can provide a speed between 5–15 Mbps (downstream) and 2–15 Mbps (upstream).
The availability of high-bandwidth infrastructure provides a channel for various types of data to be transmitted among TR sites. The advancement of haptic controls and personal monitoring devices allows higher quality client data to be gathered. With proper optimization, this data can be transferred efficiently through the high-bandwidth infrastructure, providing more complete information about the client to therapists in their assessments.
The increase in high bandwidth availability also drives most video conference developers to incorporate high-definition (HD) content into their systems, allowing higher quality of multimedia files to be transmitted over the network. Although the use of HD content in TR is currently limited, this technology has the potential for increasing the quality of TR assessment, especially in assessment that relies on visual cues and information.
Telerehabilitation and the Internet
Prior to the mid-1990s, the unavailability of high-speed and reliable connections over the Internet forced telemedicine and telerehabilitation services that required video to be delivered over proprietary systems and ISDN lines. The result was a proprietary environment with little potential for integration of informatics support across workflow. For example, videoconferencing was usually a separate service, while a database or health records were supported by a different system. The Internet gradually became suitable as a platform for demanding interactive services, such as videoconferencing, due to the advancement of broadband speeds. The drawbacks of the Internet in the past (e.g. potentially higher packet loss and low quality of service) have become less of a factor as the speed and quality of the Internet increased. Currently, most developers of videoconferencing systems have adopted the concept of communication over IP in addition to the traditional ISDN channel. Ever since being introduced in the mid 1990s, the percentage of video calls hosted over IP networks has continued to grow, with an estimation of IP networks becoming the most common network used for hosting videoconferences in 2004 (Wainhouse Research, 2006).
The future of the TR infrastructure points toward multimodal services delivered over multimodal telecommunication applications. The Internet has tremendous potential as the standard platform for future multimodal telecommunications. An integrated TR service that includes teleconsultation, e-health, and teletherapy can be delivered using multimodal applications (videoconferencing, personal health record access, personalized consumer health information, remote monitoring, etc.) over a single communication channel. The massive investment on the collaboration software by the computer industry will also provide a boost to this convergence.
The Internet’s advantage over other networks is that it is accessible, expandable, scalable, and inexpensive. The advent of the Web 2.0 technologies that are characterized by advanced networking and collaborations, as well as technology for service delivery, makes the Internet more attractive as a platform for TR applications. Deploying Web 2.0 technologies on top of the Internet allows the development of sophisticated applications that integrate videoconferencing, stimuli presentations, electronic medical records, online collaboration, and other services into a single multimodal system. Employing this approach and open-source technologies enable the rapid development of an integrated multimodal TR service in a low cost fashion.
The dynamics of Internet-based communities also allows for a product to be disseminated and tested by millions of users in a short period of time. In open-source, the Internet has become a resource that can help the polishing process of a product. Using similar methods, the Internet-based community may become a resource to help put human factors into the IT product to support TR. This approach may allow the product to be polished, modified to be free from errors and bugs, and made ready to use in a short development time.
Toward Evidence-based Telerehabilitation Services
To ensure the flow of data, a standardized data exchange protocol for TR has to be established. Following the telemedicine trend, we believe it is imperative for the TR field to create a standardized protocol to ensure the continuity of care for the client across their rehabilitation providers. This area is still in infancy both in terms of research and in the development of informatics infrastructure. Some preliminary work in this area has started to emerge. For example, Demiris (Demiris, Shigaki, & Schopp, 2005) identified the set of clinical data to assess the impact of clinical applications, including:
- Patient demographic information
- Outcome and Assessment Information Set (OASIS) data set
- Short Form (SF)-36 Health Survey data set
- Functional Independence Measure (FIM)
- Data on hospitalizations, emergency room, and medical office visits
- Geriatric Depression Scale (GDS) for older adult populations
- Secondary Conditions Questionnaire, an instrument designed to assess secondary conditions for persons with rehabilitation conditions
Providing complete information about the client will help the client track the progress of the therapy and invite the client to be more involved in the therapy. The complete information will also help the therapist make better informed decisions about the client in order to customize the therapy to fit the client’s needs.
Summary Of Findings
TR offers opportunities for providing equitable access to underserved areas and populations in both rural and urban settings to advanced rehabilitation services that are otherwise unavailable. TR also has the potential of allowing small community clinics to expand their services to include specialized services. In light of the aging population and shortage of healthcare providers, TR will play a greater role in delivering rehabilitation services to reach more individuals in both rural and metropolitan areas.
The keys to providing TR infrastructure are affordability, reachability, and scalability. The Internet has the potential to become the backbone for TR because it allows us to develop TR that is cost-effective, can reach most computers and mobile devices, and is scalable all over the world. The Internet has attractive features for developers, including being open, highly scalable, capable of handling multiple types of data, and flexible to customization. The trend toward portable monitoring devices and smart-home technologies also provides TR with new opportunities to bring specialized services closer to the clients.
These potential benefits, however, will not be realized unless the system can be adopted easily by the stakeholders of the healthcare service. Usability is a key factor in adoption of technology, therefore, development of a usable IT infrastructure to support TR is crucial for clinical and consumer entities to accept TR. The use of evidence-based practice will also be crucial in promoting the benefits of TR in limited condition settings.
Acknowledgments
This paper was presented at the Telerehabilitation State of the Science Virtual Conference held by the Rehabilitation Engineering Research Center (RERC) on Telerehabilitation at the University of Pittsburgh. The authors would like to thank David M. Brennan for helpful comments and discussions. The work is funded by the National Institute on Disability and Rehabilitation Research, grant #H133E040012.
References
- Demiris G, Shigaki CL, Schopp LH. An evaluation framework for a rural home-based telerehabilitation network. Journal of Medical Systems. 2005;29(6):595–603. doi: 10.1007/s10916-005-6127-z. [DOI] [PubMed] [Google Scholar]
- Feng X, Winters J. An interactive framework for personalized computer-assisted neurorehabilitation. IEEE Transactions on Information Technology in Biomedicine. 2007;11(5):518–526. doi: 10.1109/titb.2006.889700. [DOI] [PubMed] [Google Scholar]
- Heuser A, Kourtev H, Winter S, Fensterheim D, Burdea G, Hentz V, et al. Telerehabilitation using the Rutgers Master II Glove following carpal tunnel release Surgery: Proof-of-concept. IEEE Transactions on Neural Systems and Rehabilitation Engineering. 2007;15(1):43–49. doi: 10.1109/TNSRE.2007.891393. [DOI] [PubMed] [Google Scholar]
- Hill AJ, Theodoros DG, Russell TG, Cahill LM, Ward EC, Clark KM. An Internet-based telerehabilitation system for the assessment of motor speech disorders: a pilot study. American Journal of Speech-Language Pathology. 2006;15(1):45–56. doi: 10.1044/1058-0360(2006/006). [DOI] [PubMed] [Google Scholar]
- Hoenig H, Sanford JA, Butterfield T, Griffiths PC, Richardson P, Hargraves K. Development of a teletechnology protocol for in-home rehabilitation. Journal of Rehabilitation Research & Development. 2006;43(2):287–298. doi: 10.1682/jrrd.2004.07.0089. [DOI] [PubMed] [Google Scholar]
- Iwatsuki H, Fujita C, Maeno R, Matsuya A. Development of a telerehabilitation system for training physiotherapists in rural areas. J Telemed Telecare. 2004;10(Suppl 1):51–52. doi: 10.1258/1357633042614401. [DOI] [PubMed] [Google Scholar]
- Kim J, Brienza DM. Development of a virtual reality telerehabilitation system for analyzing accessibility of the built environment. Journal of Rehabilitation Research & Development. 2006;43(2):11–26. [Google Scholar]
- Lemaire E, Necsulescu L, Greene G. Service delivery trends for a physical rehabilitation outreach program. Disability & Rehabilitation. 2006;28(21):1349–1359. doi: 10.1080/09638280600638166. [DOI] [PubMed] [Google Scholar]
- Madden M. Internet penetration and impact. PEW Internet and American Life Project 2006 [Google Scholar]
- Paré G, Jaana M, Sicotte C. Systematic review of home telemonitoring for chronic diseases: the evidence base. J Am Med Inform Assoc. 2007 May-Jun;14(3):269–77. doi: 10.1197/jamia.M2270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Placidi G. A smart virtual glove for the hand telerehabilitation. Computers in Biology and Medicine. 2007;37(8):1100–1107. doi: 10.1016/j.compbiomed.2006.09.011. [DOI] [PubMed] [Google Scholar]
- Russell TG, Buttrum P, Wootton R, Jull GA. Low-bandwidth telerehabilitation for patients who have undergone total knee replacement: preliminary results. Journal of Telemedicine & Telecare. 2003;9(2):S44–S47. doi: 10.1258/135763303322596246. [DOI] [PubMed] [Google Scholar]
- Russell TG. Physical rehabilitation using telemedicine. Journal of Telemedicine & Telecare. 2007;13(5):217–220. doi: 10.1258/135763307781458886. [DOI] [PubMed] [Google Scholar]
- Sanford JA, Griffiths PC, Richardson P, Hargraves K, Butterfield T, Hoenig H. The effects of in-home rehabilitation on task self-efficacy in mobility-impaired adults: A randomized clinical trial. J Am Geriatr Soc. 2006;54(11):1641–1648. doi: 10.1111/j.1532-5415.2006.00913.x. [DOI] [PubMed] [Google Scholar]
- Schein RM, Schmeler MR, Brienza D, Saptono A, Parmanto B. Development of a service delivery protocol used for remote wheelchair consultation via telerehabilitation. Telemed J E Health. 2008;14(9):932–8. doi: 10.1089/tmj.2008.0010. [DOI] [PubMed] [Google Scholar]
- Schopp LH, Hales JW, Quetsch JL, Hauan MJ, Brown GD. Design of a peer-to-peer telerehabilitation model. Telemedicine Journal and e-Health. 2004;10(2):243–251. doi: 10.1089/tmj.2004.10.243. [DOI] [PubMed] [Google Scholar]
- Sugarman H, Dayan E, Weisel-Eichler A, Tiran J. The Jerusalem Telerehabilitation System, a new low-cost, haptic rehabilitation approach. Cyberpsychol Behav. 2006;9(2):178–182. doi: 10.1089/cpb.2006.9.178. [DOI] [PubMed] [Google Scholar]
- Wainhouse Research . The ISDN to IP Migration for Videoconferencing. Duxbury, MA: Weinstein, I. M; 2006. [Google Scholar]
- Winters JM. Telerehabilitation research: Emerging opportunities. Annual Review of Biomedical Engineering. 2002;4:287–320. doi: 10.1146/annurev.bioeng.4.112801.121923. [DOI] [PubMed] [Google Scholar]