Abstract
The purpose of this study was to evaluate the usability of telerehabilitation as a method of teaching self-management for chronic swelling of the lower limbs in persons with limited mobility. An in-home telerehabilitation self-management education protocol for chronic swelling of the lower limbs, termed Telerehabilitation to Empower You to Manage and Prevent Swelling (TR-PUMPS), was implemented using the Versatile and Integrated System for Telerehabilitation (VISYTER) software platform. Participants (n=11) were 36–79 years old, predominately female (72.7%) and diagnosed with a variety of health conditions. Participants’ perceived usability scores of the remote delivery of TR-PUMPS was high with a median score of 6.67 (range 4.90 – 7.00) on a Likert scale: 1= disagree to 7= agree. There was no correlation between participants’ familiarity with information technology and their perception of telerehabilitation usability. These results support telerehabilitation as a viable method for teaching a home-based, self-management protocol for chronic swelling.
Keywords: Telerehabilitation, telehealth, lower limb swelling, self-management, usability, chronic disease management and mobility limitation
An estimated 18.6 million persons in the United States have mobility limitations (Iezzonni, McCarthy, Davis & Siebens, 2000). Individuals who rely on wheelchairs for mobility are at higher risk for chronic swelling due to limited or absent calf-pump function (Cavorsi, 2000). In addition, the negative effect of sitting for long periods of time, e.g., limb dependency, impedes venous and lymphatic flow (Geyer, 2010). If untreated, chronic swelling may lead to lymphedema, a chronic debilitating disease that requires life-long management. Without proper management, lymphedema can progress, resulting in the proliferation of fibrotic tissue, an increase in size of affected limb and increased risk for wounds and infections (Baddour, 2006; Dupuy et al., 1999; Foldi, Foldi, & Clodius, 1989; ISL, 2009). The standard of care for chronic swelling generally involves a regimen of hygiene, meticulous skin and nail care, and some form of compression to reduce the limb swelling and maintain the reduction. In the case of lymphedema, exercise, deep breathing and lymphatic massage are added to provide complete decongestive therapy (CDT). Therapy is provided in two phases. Specialized lymphedema therapists provide Phase 1 of the therapy within the clinical setting. Phase 2 involves the patients’ self-management of their chronic swelling in which they maintain this multi-modal regimen for life. The objective of therapy is to stop lymphedema progression, decrease swelling and fibrotic changes in the tissue and prevent infections and other complications (Foldi, 1998; Kerchner, Fleischer, & Yosipovitch, 2008; Ko. 1998; Mayrovitz, 2009; NLN, 2011; Rockson, 2001).
Self-management programs for chronic conditions have been shown to improve healthcare outcomes and increase health-related quality of life (Bourbeau et al., 2003; DeWalt et al., 2004; Lorig, Sobel, Ritter, Laurent, & Hobbs, 2001; Lorig, Ritter, Laurent, & Plant, 2006). However, research on self-management of lymphedema is minimal. A systematic review of literature on self-management of lymphedema from 2004–2011 indicated that Phase 2 CDT, which includes compression therapy, lymphatic massage, exercise and skin care, was likely to be effective but this conclusion was based on expert opinion only. Further research on self-management of lymphedema, particularly randomized controlled trials, was recommended based on results of the review (Ridner et al., 2012). Studies have identified that delay in appropriate treatment due to lack of healthcare professionals’ knowledge regarding lymphedema and inadequate specialized therapy resources can negatively impact quality of life in people with lymphedema. Delay in treatment may lead to progression of the disease, resulting in an increase in swelling, infections, pain and a decrease in mobility of an effected extremity, negative self-image, depression and social isolation (Bogan, Powell, & Dudgeon, 2007; Morgan, Frank, & Moffatt, 2005; William, Moffatt, & Franks, 2004). Access to specialized lymphedema therapists in the US is limited due to the small number of therapists and inequitable distribution (more urban than rural) (Lymphology Association of North America, n.d.). These issues compound existing transportation barriers frequently encountered by persons with limited mobility (Drainoni et al., 2006; Kaye, Kang, & LaPlante, 2000). Transportation barriers are escalated for people who live in rural areas resulting in long commutes to urban medical centers. Barriers identified include inadequate or nonexistent public transportation, difficulty coordinating time with caregivers, lack of assessable restrooms in route, difficulty sitting for prolong periods of time, and delayed pick-ups by transportation services resulting in missed appointments (Drainoni et al, 2006; Iezzoni, Killeen, & O’Day, 2006). Results of the U.S 2002 National Health Interview Survey found that, within a one year time frame, approximately 3.7 million people delayed obtaining medical care due to transportation difficulties (Wallace, Hughes-Cromwick, Mull, & Khasnabis, 2005). Few studies have attempted to identify solutions to the challenges faced by persons with chronic swelling/ lymphedema and mobility limitations in accessing treatment for this chronic condition. Telerehabilitation (TR) has the potential to overcome the barriers to access for treatment for this population and has recently been shown to be effective in the delivery of in-home therapy (Finkelstein, Lapshin, Castro, Cha, & Provance, 2008; Holden, Dyar, & Dyan-Cimadoro, 2007; Tousignant, Boissy, Corriveau, Moffett, & Cabana, 2009). Therefore, this study aimed to examine the usability of TR as a method of teaching self-management for chronic swelling of the lower limbs in persons with limited mobility.
Method
Design
The parent study was a prospective longitudinal single cohort study funded by the National Institute on Disability and Rehabilitation Research, United States Department of Education (Grant # H133E090002). Data used to measure outcomes for the present study were obtained prior to and at the end of the six week TR intervention.
Sample Population
Inclusion criteria for the study were: 1) aged 18–80; 2) swelling or lymphedema for > 3 months that did not resolve overnight; and 3) used a scooter or wheelchair for mobility within the community. Exclusion criteria were: 1) visual acuity less than 20/100; 2) inability to apply and remove socks and pants or unavailability of a caregiver who could perform such tasks; and 3) contraindications for compression therapy (Brennan & Miller, 1998; Kunimoto et al., 2001; NLN, 2011; Tiwara, Cheng, Button, Myint, & Hamilton, 2003).
Participants were recruited from lymphedema clinics, wound clinics and physical medicine and rehabilitation departments in southwestern Pennsylvania, the Western Pennsylvania Lymphedema Therapists Network and the Research Participant Registry of an academic medical center. The study goal was to recruit a sample of 11 participants. This sample size was determined using a power analysis with the alpha level of 0.05, a power of 0.80 and was based on a literature review of the effect size of an instrument (Canadian Occupational Performance Measure) used in the parent study. The study received Institutional Review Board approval and all participants provided informed consent.
Self-Management Protocol
The process used to develop the standardized self-management protocol, TR-PUMPS, used in the present study was described in a previous article (Faett, Geyer, Hoffman, & Brienza, 2012). The self-management protocol was developed using expert consultation. It incorporated 10 validated patient education modules at the 5th grade reading level designed to teach principles of CDT in a manner suitable for the targeted population and a TR platform tailored to effectively deliver the program (Faett et al., 2012). The resulting protocol incorporated face-to-face TR educational sessions and educational material supplied in both video and written format.
TR Technology
When defining the type of technology needed to effectively and efficiently implement the self-management program, the following features were evaluated: 1) potential to provide face-to-face telecommunication between the TR clinician and study participant; 2) potential to allow media sharing of educational videos during teleconferencing sessions; 3) video capability that allowed performance of skin assessments and observations of return demonstrations of self-management skills; 4) system characteristics that were intuitive or required minimal training for the TR clinician and study participants; 5) system requirements that allowed use of participants current home computers; 6) proven reliability and minimal requirements for Information Technology support; 7) ability to customize the system with off-the-shelf audio and video equipment; and 8) ability to archive TR sessions for educational purposes and to evaluate the self-management program. Based on these features, the Versatile and Integrated System for Telerehabilitation (VISYTER) software platform (Parmanto et al., 2010) was selected to remotely deliver the self-management program. VISYTER is a secure system that provides real-time videoconferencing and sharing of media. The system allows use of multiple cameras, includes the ability to archive sessions (Parmanto et al., 2010) and has been shown to be effective in conducting remote clinical evaluations (Schein, Schmeler, Holm, Saptono, & Brienza, 2010). Laboratory testing of VISYTER to tailor it for optimal delivery of the protocol was performed prior to implementation. Results of testing to establish broadband speed requirements and a detailed description of the audio and video equipment used to deliver the protocol were described in a previous article (Faett et al., 2012).
TR Implementation
The TR intervention was provided to the participants within their home setting. After initial testing to confirm adequate broadband speed, VISYTER software was downloaded onto the participant’s computer or a loaned laptop. During the TR set-up, the co-investigator setting up the TR platform first connected with a TR clinician via a virtual clinic room to evaluate the video and audio connection. The participant was provided with instructions on how to connect to VISYTER. During TR sessions, the clinician and participants connected via VISYTER’s virtual clinic rooms at pre-determined times. Educational videos were accessed via the media sharing capabilities of VISYTER and used as a teaching tool during the teleconferencing sessions. Skin assessments and skill performance were viewed using a remotely controlled camera with zoom capabilities. Videoconferencing with each participant took place a minimum of once a week for six weeks.
Outcome Measures
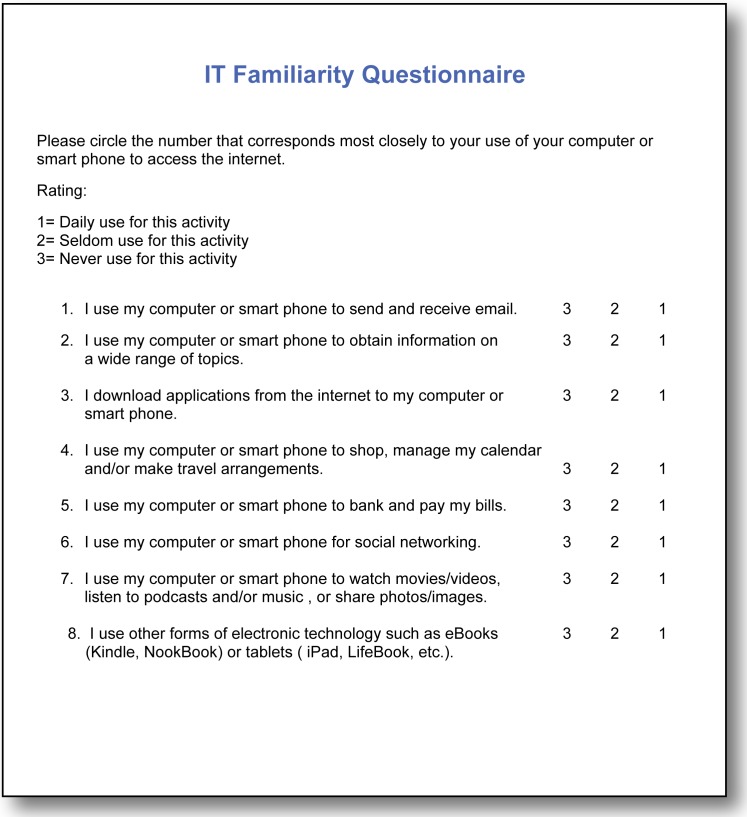
The Information Technology (IT) Familiarity Questionnaire, developed by Geyer, M. J., was utilized to evaluate the participants’ familiarity with Information Technology, as no relevant validated tool could be located that was appropriate for use in this study. The tool consisted of eight questions on frequency of use of IT which participants rated using a Likert scale (1= daily use to 3= never used). The total score was the average of the scores of the eight questions. The tool was evaluated by researchers with experience conducting TR and found to have face validity. IT familiarity was viewed as a potential barrier to success using the TR educational intervention and satisfaction with TR.
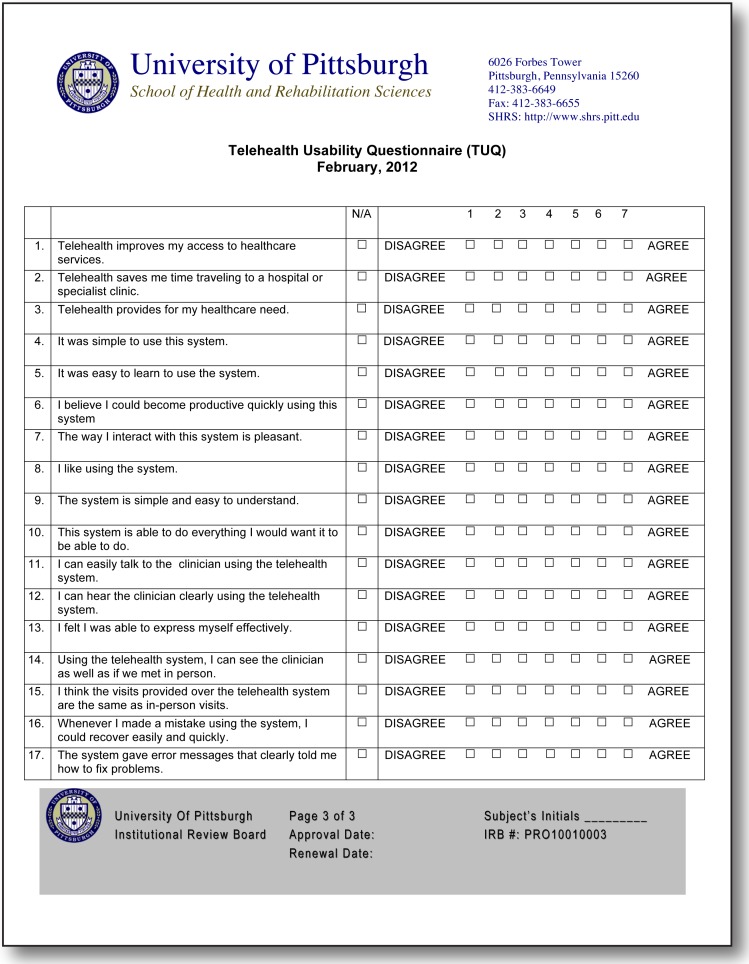
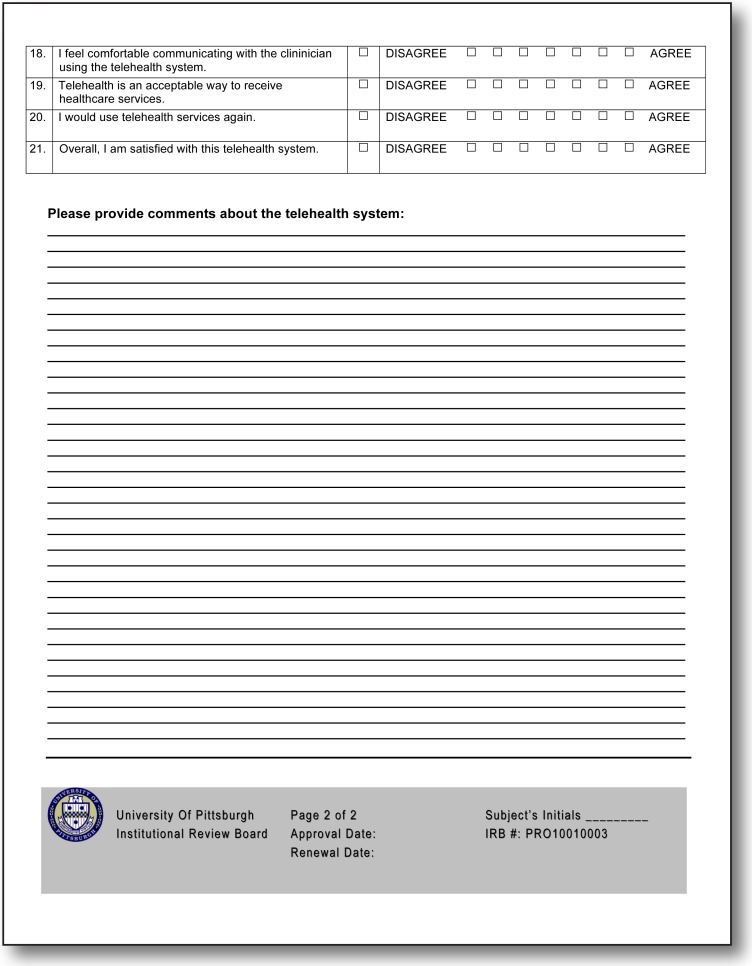
The Telehealth Usability Questionnaire (TUQ) (Parmanto, Pulantara, Schutte, Saptono, & McCue, 2013; Schein et al., 2011) was designed to evaluate usability of a variety of telehealth systems. The questionnaire addresses six factors: usefulness, ease of use and learnability, interface quality, interaction quality, reliability, and satisfaction. The tool uses a Likert scale (1=disagree to 7=agree). The total score is computed by determining a mean score for the 21 questions with a total possible score of 7.
Data Collection and Analysis
The IT Familiarity Questionnaire was completed by participants prior to the TR intervention. The TUQ was completed at the end of the six week TR intervention. Scores were analyzed using descriptive analysis; Spearman’s correlation coefficient was used to evaluate the relationship between the two variables. Data were analyzed using SPSS Statistical Analysis Software-Version 20.
Results
Sample characteristics
Thirteen participants were recruited for the study. One participant withdrew the second week of the intervention, stating that she was unable to don the advanced pneumatic compression device used in the study herself and did not have a caregiver available to assist her. A second participant withdrew prior to the beginning of the intervention stating it was due to personal issues and time constraint. Eleven participants completed the study. The participants mean age was 54.5 years (SD + 11.9, median 52 years, range 36–79 years). The majority (72.7%) were female. All subjects reported having at least a high school education and over half (63.6%) reported having pursued education beyond the high school level.
Of the 11 participants, five (45.5%) were diagnosed with multiple sclerosis and the remainder with various other health conditions. Although the mean duration of chronic swelling was 11.8 years, there was a large variability reflected in the median (3 years) and range (2–47 years) of time with this health condition. Only three of the participants had received previous treatment for their chronic swelling. Table 1 presents demographic and medical condition data for the 11 participants who completed the intervention.
Table 1.
Participants’ demographic characteristics (N = 11)
| Subject | Sex | Age | Years of Education | Diagnosis | Years of Swelling | Previous Treatment |
|---|---|---|---|---|---|---|
| 1 | F | 63 | 12+ | Spina Bifida | 47 | Y |
| 4 | F | 48 | 12+ | Lipo-lymphedema, lymphedmatardia | 6 | Y |
| 5 | M | 51 | 12 | SCI, C5–C7 | 2 | N |
| 6 | F | 62 | 12 | Head Injury, Age 3 | 20 | N |
| 7 | M | 43 | 12+ | Multiple Sclerosis | 3 | N |
| 8 | M | 79 | 12+ | Chronic Venous Insufficiency | 3 | Y |
| 9 | F | 52 | 12+ | Multiple Sclerosis | 2 | N |
| 10 | F | 36 | 12 | Life-long swelling, Familial | 36 | N |
| 11 | F | 64 | 12+ | Multiple Sclerosis | 2 | N |
| 12 | F | 54 | 12+ | Multiple Sclerosis | 2 | N |
| 13 | F | 50 | 12 | Multiple Sclerosis | 7 | N |
Telehealth Usability Questionnaire (TUQ)
Median scores for the six usability factors ranged from 5.09 (Reliability) to 6.95 (Satisfaction and Future Use). The median total score was 6.67 (range 4.90 – 7.00) (Table 2).
Table 2.
Telehealth Usability Questionnaire Scores TUQ [Likert Scale (1=Disagree; 7=Agree); N = 11]
| Variable | Median | Range |
|---|---|---|
| Usefulness | 6.34 | 6.36 – 6.90 |
| Ease of Use & Learnability | 6.45 | 6.27 – 6.64 |
| Interface Quality | 6.59 | 6.45 – 6.64 |
| Interaction Quality | 6.68 | 6.45 – 6.91 |
| Reliability | 5.09 | 4.50 – 5.27 |
| Satisfaction and Future Use | 6.95 | 6.82 – 7.00 |
| TUQ Total Score | 6.67 | 4.90 – 7.00 |
Information Technology (IT) Familiarity Questionnaire
The median score for IT Familiarity was 1.69. The range of the scores was 1.00 – 2.63, as per the Likert scale [1=Daily use for this activity, 2=Seldom use for this activity, 3=Never use for this activity].
Relationship between IT Familiarity and Telehealth Usability
Analysis was performed to determine if there was a relationship between the participants’ IT Familiarity and their perception of telehealth usability (TUQ). Results showed no significant correlation (rs =.−006, p = .987). See Table 2.
Discussion
This study was conducted to evaluate the usability of TR for the delivery of an in-home self-management education protocol for chronic swelling of the lower limbs, termed Telerehabilitation to Empower You to Manage and Prevent Swelling (TR-PUMPS). Participants’ responses indicated a high level of satisfaction with the approach and ease of use of the system. There was no correlation between the participants’ familiarity with information technology and their perception of TR usability.
When conducting the study, several steps were taken to promote user satisfaction and provide support for use of the system. Weekly TR interventions ranged from 1–4 times per week. Median duration of the TR sessions was 40 minutes. Scheduling of sessions was determined collaboratively by the participant and TR clinician. Frequency of sessions was determined by participant availability and educational needs. All but one of the participants needed a caregiver to assist with some self-management tasks, for example skin hygiene, donning/doffing of compression garments. This created the need for flexible scheduling and some sessions were conducted during evening and weekend hours. Others were rescheduled due to participant fatigue and pain level, unavailability of caregivers or a change in the participants’ daily schedule. These issues can be concerns due to availability of the TR clinician and could lead to missed sessions, a factor that needs to be considered when implementing TR.
Since many of the participants had multiple caregivers (professional and/or family members), a goal of this self-management program was to assist participants in obtaining the knowledge and skill set to instruct other caregivers who were an integral part of their care. The TR encounters allowed the remote clinician to observe participants’ interactions with multiple caregivers during their self-management activities and provide feedback and cueing when necessary. The speakerphone allowed the TR clinician to interact with the participant and caregiver who also had the ability to address any questions or concerns in regard to participant care. A secondary benefit related to the interaction and involvement this approach promoted was engagement of both participants and caregivers in the self-management process.
Some homes had inadequate lighting for skin assessments. Often the participants’ legs were dependent for skin inspection, necessitating the need for the participant or caregiver to manually maneuver the remote camera to assess behind the legs and under the feet. Lighting for proper assessment was successfully facilitated with the attachment of a gorilla light to the remote camera.
Several technical issues arose in regard to using VISYTER. Many participants had home computers with old software and hardware. This resulted in the inability to use VISYTER with their home computers. It was therefore necessary to provide a loaned laptop during the intervention phase of the study. In addition, internet access and adequate broadband speeds to use VISYTER posed difficulties. One participant did not have internet broadband access and another did not have adequate broadband speed. To address this issue, the study was modified to include the use of 4G wireless access. It was later determined that 4G wireless access was not available in the geographic area. One participant acquired broadband access on her own and the other had her access upgraded. Issues with connection and equipment occurred during some sessions, for example inability to connect to the VISYTER server, lack of audio feed and VISYTER software not recognizing camera and audio devices. The majority of these issues were handled either via teleconferencing or by telephone by either the TR clinician or a biomedical engineer who was a co-investigator in the study. The system was not as intuitive as was anticipated. A trouble shooting manual for VISYTER would have been beneficial for both the participant and the TR clinician in addressing technical issues. IT support for VISYTER would have also been of assistance. Three trips to participants’ homes were necessary during the study. One trip was to reinstall VISYTER software and the other two trips were due to the need to replace damaged remote cameras. Damage from the cameras occurred when they fell on the ground. A need for backup equipment was realized and addressed during the study. Despite these problems, scores from the TUQ indicated that delivery of TR with real-time face to face interactive education and evaluation sessions using the VISYTER software platform was viewed positively and all participants indicated satisfaction with the telehealth system and would use it again. This supported previous evidence that participants had high levels of satisfaction with TR provided by VISYTER (Schein, Schmeler, Saptono, & Brienza, 2010).
An advantage of using the VISYTER with a laptop was the flexibility it offered in regard to where teleconferencing can occur (e.g., multiple rooms within the home). VISYTER provided video conferencing with good resolution and minimal break-up into pixilation. The zoom capability of the remote camera enhanced ability to perform skin inspections. The ability to capture digital images by the TR clinician resulted in the ability of the clinician to obtain feedback from other clinicians in evaluation of skin assessments when indicated. These VISYTER capabilities supported evidence of the effectiveness of VISYTER in providing remote clinical evaluations (Schein, Schmeler, Holm, Saptono, & Brienza, 2010). Although TR prevented the remote clinician observer from using touch and smell to assess participant status, this disadvantage was resolved by instructing the participant or caregiver to inspect for pitting, tissue firmness and warmth, and assess odor from wound drainage. From this clinician’s prospective, TR using the VISYTER software platform is viewed as a viable method to provide this self-management protocol and could potentially be used to provide remote self-management programs for other chronic conditions.
Limitations of study
The study enrolled a small sample and there was no control group. Our goal was to recruit a larger sample but we were unable to accomplish this goal despite use of multiple sites for recruitment. The sample was a convenience sample and included participants with varied types of chronic swelling/lymphedema. While a limitation, this diversity also allowed evaluation of the system by individuals with varied health status and mobility limitation.
Conclusion
The TR program was well received by participants. It addresses barriers associated with traditional care such as transportation and access to specialists. Responses of participants indicated that delivery of TR with real-time face-to-face interactive education and evaluation sessions via the VISYTER software platform was an acceptable way to receive self-management education. The ability to observe participants in their home environment enabled the team to assess and address potential physical barriers that could negatively affect the participants’ care and more quickly respond to potential problems before they become major challenges. This study supports TR as a viable method of providing an educational component for a home based self-management program on lower limb chronic swelling/lymphedema in people with mobility limitations and a means to decrease the burden associated with lifelong management of this debilitating condition.
Directions for Future Research
The parent study which incorporated this protocol is designed to evaluate the effectiveness of this self-management program in this patient population. Suggestions for future research would include a randomized controlled trial to evaluate outcomes of a self-management program for patients with chronic swelling/ lymphedema and limited mobility delivered via TR versus traditional therapy.
Figure 1.
IT Familiarity Questionnaire (Geyer, M. J.)
Figure 2:
Telehealth Usability Questionnaire (Parmanto et al., 2013)
Table 3:
Spearman’s correlation coefficient analysis of IT Familiarity and TUQ Scores
[Likert Scale (1=Daily use for this activity, 2=Seldom use for this activity, 3=Never use for this activity); N = 11]
| Variable | Median | Range | rs | p |
|---|---|---|---|---|
| IT Familiarity | 1.69 | 1.00 – 2.63 | −.006 | .987 |
| TUQ | 6.67 | 4.90 – 7.00 |
Acknowledgments
Funding for this research was provided by the National Institute on Disability and Rehabilitation Research, United States Department of Education, Grant # H133E090002.
References
- 1.Baddour L. Recent considerations in recurrent cellulitis. Current Infections and Disease Reports. 2006;3:461–465. [PubMed] [Google Scholar]
- 2.Bogan L, Powell J, Dudgeon B. Experiences of living with non-cancer related lymphedema: Implications for clinical practice. Qualitative Health Research. 2007;17:213–224. doi: 10.1177/1049732306297660. [DOI] [PubMed] [Google Scholar]
- 3.Brennan M, Miller L. Overview of treatment options and review of the current role and use of compression garments, intermittent pumps, and exercise in management of lymphedema. Cancer Supplement. 1998;83:2822–2827. doi: 10.1002/(sici)1097-0142(19981215)83:12b+<2821::aid-cncr33>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 4.Bourbeau J, Julien M, Maltais F, Rouleau M, Beaupré A, Bégin R, Collet JP. Reduction of hospital utilization in patients with chronic obstructive pulmonary disease: A disease-specific self–management intervention. Archives of Internal Medicine. 2003;163:585–591. doi: 10.1001/archinte.163.5.585. [DOI] [PubMed] [Google Scholar]
- 5.Cavorsi J. Venous ulcers of the lower extremities: Current and newer management techniques. Topics in Geriatric Rehabilitation. 2000;16(2):24–34. [Google Scholar]
- 6.DeWalt D, Pignone M, Malone R, Rawls C, Kosnar M, Angel B. Development and pilot testing of a disease management program for low literacy patients with heart failure. Patient Education and Counseling. 2004;55:78–86. doi: 10.1016/j.pec.2003.06.002. [DOI] [PubMed] [Google Scholar]
- 7.Dupuy A, Benchikhi H, Roujeau JC, Bernard P, Vaillant L, Chosidow O, Bastuji-Garin S. Risks factors for erysipelas of the leg: A case control study. British Medical Journal. 1999;318:1591–1594. doi: 10.1136/bmj.318.7198.1591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Drainoni M, Lee-Hood, Tobias C, Bachman S, Andrew J, Maisels L. Cross-disability experiences of barriers to health-care access. Journal of Disability Policy Studies. 2006;17:101–115. [Google Scholar]
- 9.Faett B, Geyer MJ, Hoffman L, Brienza D. Design and development of a telerehabilitation self-management program for persons with chronic lower limb swelling and mobility limitations: Preliminary evidence. Nursing Research and Practice. 2012. 2012. pp. 1–10. Retrieved from: http://www.hindawi.com/journals/nrp/2012/608059/ [DOI] [PMC free article] [PubMed]
- 10.Finkelstein J, Lapshin O, Castro H, Cha E, Provance P. Home-based physical telerehabilitation in patients with multiple sclerosis: A pilot study. Journal of Rehabilitation Research and Development. 2008;45:1136–1137. doi: 10.1682/JRRD.2008.01.0001. [DOI] [PubMed] [Google Scholar]
- 11.Foldi E. The treatment of lymphedema. Cancer. 1998;83:2833–2844. doi: 10.1002/(sici)1097-0142(19981215)83:12b+<2833::aid-cncr35>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 12.Foldi E, Foldi M, Clodius L. The lymphedema chaos: A lancet. Annals of Plastic Surgery. 1989;22:505–515. doi: 10.1097/00000637-198906000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Geyer MJ. Chronic edema in wheelchair-dependent persons. Presented at the 2nd International Lymphoedema Framework Conference; Brighton, UK. 2010. [Google Scholar]
- 14.Holden MK, Dyar TA, Dayan-Cimardoro L. Telerehabilitation using a virtual environment improves upper extremity function in patients with strokes. IEEE Transactions on Neural Systems and Rehabilitation. 2007;15(1):36–42. doi: 10.1109/TNSRE.2007.891388. [DOI] [PubMed] [Google Scholar]
- 15.Iezzoni LI, Killeen MB, O’Day BL. Rural residents with disabilities confront substantial barriers to obtaining primary care. Health Services Research. 2006;41:1258–1275. doi: 10.1111/j.1475-6773.2006.00534.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iezzoni L, McCarthy E, Davis R, Siebens H. Mobility impairments and use of screening and preventive services. American Journal of Preventive Health. 2000;90:955–961. doi: 10.2105/ajph.90.6.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.International Society of Lymphology The diagnosis and treatment if peripheral lymphedema: 2009 consensus document of the International Society of Lymphology. Lymphology. 2009;42:51–60. Retrieved from http://www.solarismed.com/rr/journal.pdf. [PubMed] [Google Scholar]
- 18.Kaye S, Kang T, LaPlante M. Mobility device use in the United States Disability Statistics Report, (14) Washington, D.C: U.S. Department of Education, National Institute on Disability and Rehabilitation Research; 2000. Retrieved from http://dsc.ucsf.edu/pub_listing.php?pub_type=report. [Google Scholar]
- 19.Kerchner K, Fleischer A, Yosipovitch G. Lower extremity lymphedema update: Pathophysiology, diagnosis, and treatment guidelines. Journal of American Academy of Dermatology. 2008;59:324–331. doi: 10.1016/j.jaad.2008.04.013. [DOI] [PubMed] [Google Scholar]
- 20.Ko D, Learner R, Klose G, Cosimi A. Effective treatment of lymphedema of the extremities. Archives of Surgery. 1998;133:452–458. doi: 10.1001/archsurg.133.4.452. [DOI] [PubMed] [Google Scholar]
- 21.Kunimoto B, Cooling M, Gulliver W, Houghton P, Orsted H, Sibbald RG. Best practices for the prevention and treatment of venous leg ulcers. Ostomy/Wound Management. 2001;47(2):34–50. [PubMed] [Google Scholar]
- 22.Lorig K, Ritter P, Laurent D, Plant K. Internet-based chronic disease self- management a randomized trial. Medical Care. 2006;44:964–971. doi: 10.1097/01.mlr.0000233678.80203.c1. [DOI] [PubMed] [Google Scholar]
- 23.Lorig K, Sobel D, Ritter P, Laurent D, Hobbs M. Effect of a self-management program on patients with chronic disease. Effective Clinical Practice. 2001;4:256–262. [PubMed] [Google Scholar]
- 24.Lymphology Association of North America Certified LANA therapists. (n.d.) Retrieved from http://www.clt-lana.org/therapists/default.asp?list=all.
- 25.Mayrovitz H. The standard of care for lymphedema: Current concepts and physiological considerations. Lymphatic Research and Biology. 2009;7:101–109. doi: 10.1089/lrb.2009.0006. [DOI] [PubMed] [Google Scholar]
- 26.Morgan P, Franks P, Moffatt C. Health-related quality of life with lymphedema: A review of the literature. International Wound Journal. 2005;2(1):47–62. doi: 10.1111/j.1742-4801.2005.00066.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Lymphedema Network (NLN) Medical Advisory Committee Position statement of the National Lymphedema Network; Topic: The diagnosis and treatment of lymphedema. 2011. Retrieved from http://www.lymphnet.org/pdfDocs/nlntreatment.pdf.
- 28.Parmanto B, Pulantara IW, Schutte J, Saptono A, McCue M. An integrated telehealth system for remote administration of an adult autism assessment. Telemedine Journal and e-Health. 2013;19:88–94. doi: 10.1089/tmj.2012.0104.. [DOI] [PubMed] [Google Scholar]
- 29.Parmanto B, Saptono A, Pramana G, Pulantara W, Schein R, Schmeler M, Brienza D. VISYTER: Versatile and integrated system for telerehabilitation. Telemedicine and e-Health. 2010;16:939–944. doi: 10.1089/tmj.2010.0033. [DOI] [PubMed] [Google Scholar]
- 30.Ridner S, Fu M, Wanchai A, Stewart B, Armer J, Comier J. Self-management of lymphedema: A systematic review of the literature from 2004 to 2011. Nursing Research. 2012;61:291–299. doi: 10.1097/NNR.0b013e31824f82b2. [DOI] [PubMed] [Google Scholar]
- 31.Rockson S. Lymphedema. American Journal of Medicine. 2001;110:288–295. doi: 10.1016/s0002-9343(00)00727-0. [DOI] [PubMed] [Google Scholar]
- 32.Schein R, McCue M, Sponer M, Kumar S, Parmanto B, Hartman L. Exploring telerehabilitation uniform data system. Presented at RESNA 2011; Toronto, Canada. 2011. Retrieved from: http://www.rerctr.pitt.edu/DevHold/RERC_TR_RS_RESNA_6_2011.pdf. [Google Scholar]
- 33.Schein R, Schmeler M, Holm M, Saptono A, Brienza D. Telerehabilitation wheeled mobility and seating assessments compared with in person. Archives of Physical Medicine and Rehabilitation. 2010;91:874–878. doi: 10.1016/j.apmr.2010.01.017. [DOI] [PubMed] [Google Scholar]
- 34.Schein R, Schmeler M, Saptono A, Brienza D. Patient satisfaction with telerehabilitation assessments for wheeled mobility and seating. Assistive Technology. 2010;22:215–222. doi: 10.1080/10400435.2010.518579. [DOI] [PubMed] [Google Scholar]
- 35.Tiwara A, Cheng K, Button M, Myint F, Hamilton G. Differential diagnosis, investigation, and current treatment of lower limb lymphedema. Archives of Surgery. 2003;138:152–161. doi: 10.1001/archsurg.138.2.152. [DOI] [PubMed] [Google Scholar]
- 36.Tousignant M, Boissy P, Corriveau H, Moffett H, Cabana F. In-home telerehabilitation for post-knee arthroplasty: A pilot study. International Journal of Telerehabilitation. 2009;1(1):9–16. doi: 10.5195/ijt.2009.5997. Retrieved from http://telerehab.pitt.edu/ojs/index.php/Telerehab/article/view/5997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wallace R, Hughes-Cromwick P, Mull H, Khasnabis S. Access to health care and nonemergency medical transportation. Journal of the Transportation Research Board. 20051924:76–84. [Google Scholar]
- 38.Williams A, Moffatt C, Franks P. A phenomenological study of the lived experiences of people with lymphedema. International Journal of Palliative Nursing. 2004;10:279–286. doi: 10.12968/ijpn.2004.10.6.13270. [DOI] [PubMed] [Google Scholar]