Abstract
The purpose of this study was to gather information regarding the receptivity of clinicians, caregivers and family members, and adults with spina bifida (SB) to the use of a mHealth application, iMobile Health and Rehabilitation (iMHere) system. Surveys were administered to end user groups in conjunction with a conference presentation at the Spina Bifida Association’s 38th Annual Conference. The survey results were obtained from a total of 107 respondents. Likert scale and qualitative results are provided in consideration of future application of the iMHere system in clinical practice. The results of this survey indicate respondents were receptive and supportive with regard to adopting such a system for personal and professional use. Challenges likely to be encountered in the introduction of the iMHere system are also revealed and discussed.
Keywords: mHealth, wellness, self-management, telerehabilitation, telehealth, spina bifida, myelomeningocele, smartphone
Background and Introduction
By 2030, it is projected that 171 million persons, over half the United States population, will be living with one or more chronic conditions (Menehan, 2011). The iMHere system addresses the needs of persons with chronic conditions by providing a means to manage and support persons while residing in the community through a proactive approach to care. This innovative system allows for dynamic two-way communication in order to provide seamless coordinated healthcare services and encourage self-management of one’s condition. The iMHere system has the potential to address the needs associated with many chronic conditions and disabilities due to the versatility in the design of the system and ubiquity of mobile devices. Furthermore, the iMHere system allows for customization that can occur through design of unique apps for specific populations and can be even further adapted and utilized to meet individuals’ needs.
The Spina Bifida population was selected to pilot the iMHere system due to the complexity of needs and opportunity to create a significant impact on a variety of outcomes. Spina bifida (SB) has been described as the most severe congenital condition that is compatible with life (Bowman, McLone, Grant, Tomita, & Ito, 2001). Very early in the growth of the embryo, when only about the length of a grain of rice, abnormal development of the spinal cord and surrounding structures occurs in the open forms of SB (Sandler, 1997). There are several types of open SB which have varying degrees of impact upon the person’s development and functional abilities. The most severe form of SB is myelomeningocele (MM), which is often associated with hydrocephalus, neurogenic bowel and bladder, depression, sensory loss and varying degrees of paralysis. Secondary medical issues such as urinary tract infections (UTIs) and pressure ulcers are among the most challenging and expensive complications for these individuals (Dicianno & Wilson, 2010).
Studies have shown that hydrocephalus has a negative effect on cognitive status (Barf et al., 2003; Iddon, Morgan, Loveday, Sahakian, & Pickard, 2004). Approximately 80% of children born with SB either have or will develop hydrocephalus which will require treatment (SBA, 2012b). Hydrocephalus is typically treated by shunting, a surgical procedure used to control pressure in the brain. Individuals with MM, who have undergone shunt revisions after the age of two years, tend to have poor long term achievement as adults (Hunt, Oakeshott, & Kerry, 1999) and deficits in movement, timing, attention and orienting (Dennis et al., 2006). Specifically, research has shown executive functioning deficits in persons with SB in areas including: planning, shifting attention, initiation, working memory, problem-solving and self-monitoring (Calvery, 2008; Mahone et al., 2002; Dise & Lohr, 1998).
Executive function is considered to be central to the completion of activities of daily living (ADLs), particularly when expected to be initiated and completed at fixed time intervals throughout the day. In persons with hydrocephalus, direct correlations have been found between executive dysfunction and inability to complete many of their necessary self-care tasks independently (Hunt et al., 1999). The individual tasks of ADLs are fairly simple. However, self-care routines can be quite complex from a cognitive perspective, involving the need to plan, initiate and execute numerous tasks at different times throughout the day. Medication routines, self-catheterization and daily skin checks are examples of common self-care tasks required of persons with SB. In combination, these self-care routines demand more complex cognitive processes to effectively maintain.
Over the past 20–30 years, advances in medical interventions have greatly increased the life expectancy of persons with SB (Brown, 2001; Dillon, Davis, Duguay, Seidel, & Shurtleff, 2000). The result is that a growing number of persons with SB are outliving their caregivers without adequate support systems in place. Without the necessary care and support, chronic health conditions commonly develop and often lead to secondary disability and death (Dicianno & Wilson, 2010; Exner, Burgdöffer, Bohatyrewicz, Bomnüter, & Wenck 1993). Research has also shown that preventable conditions (e.g., wounds, UTIs and sepsis) account for over one-third of the U.S. hospitalizations of young adults with SB incurring a total cost of $360 million annually for this group (Dicianno & Wilson, 2010). Using preventative approaches to providing health care services could potentially reduce mortality, morbidity, the cost of healthcare, and improve the experience of utilizing health related services (Dicianno et al., in press). Developing a network of care to support adults with SB is a pressing challenge for medicine and social service systems (Bowman et al., 2001).
Hayden, Davenport, and Campbell (1979) were some of the first researchers to document the need for increased self-management skills in youths with SB. Despite the identification of this need, over 30 years later, a limited understanding of the experience of self-management and strategies to develop these skills in persons with SB still remains. In a recent multi-center study we showed that higher self-management skills are negatively correlated with number of UTIs, pressure ulcers and hospitalizations in young adults with SB (Mahmood, Dicianno, & Bellin, 2011). Sawin and colleagues (2009) note that it is critical for persons with SB to enhance self-management skills in order to improve overall quality of life.
Implementing a mHealth System to Extend and Enhance Wellness Services
In order to respond to this problem, a proactive approach to promote health and well-being in young adults with SB was originally developed as an in-person Wellness Program at the Spina Bifida Association of Western Pennsylvania (SBAWP). The SBAWP Wellness program produced remarkably improved outcomes including fewer instances of UTIs and pressure ulcers as well as decreased incidence and duration of hospitalizations in comparison with national data gathered in a study by Ouyang and colleagues (2007) (Dicianno et al., in press). While the SBAWP grant-funded Wellness program was very successful in reducing secondary conditions and decreasing healthcare costs, it also had significant limitations in the number of persons which could be served over a small geographic region due to limited funding. With an existing shortage of nursing staff in the United States (AACN, 2012) it did not seem feasible to consider expansion of the program to more persons in a wider geographic area by hiring more nursing staff to serve as Wellness Coordinators (WCs). Furthermore, persons with SB residing in outlying rural areas often have even fewer resources and could benefit even further from the program.
Telerehabilitation (TR) or telehealth is one means to efficiently and cost-effectively provide support to persons in rural areas. A remote system can employ the wireless technology of a smartphone and specially designed applications (“apps”) for the most common needs of the SB population in order to help support and maintain self-management skills. Increased support through a TR delivery method could potentially also decrease the burden of seeking assistance and healthcare services upon the consumer (i.e., person with MM) and improve overall quality of life (McCue, Fairman, & Pramuka, 2010). The smartphone was selected as the best method of delivery of remote support for multiple reasons. Smartphones are quickly growing in popularity in the United States due to their versatility. According to Neilson (2012), 56% of mobile phone users are now smartphone owners, and this growth is expected to continue. Software and support can be easily transported in the user’s hand, whether at home, work, or at a ball game. Portability is very important to achieve success in the clinical application of a system where self-care activities need to occur regardless of the location of the user. When emerging mobile communication and network technologies are integrated for use within healthcare systems, this is known as mobile health or mHealth (Istepanian et al., 2005). The American Telemedicine Association (2012) advises that mHealth is to be thought of as a tool through which telehealth or telemedicine can be provided.
The purpose of this paper is to evaluate the overall impressions and receptivity of potential users of a mHealth system to encourage self-management of secondary conditions often associated with SB. Individuals likely to utilize such a mHealth system include: persons with SB, clinicians (physicians, nurses, social workers, therapists), and family members and caregivers of persons with SB. Therefore, it was vital to seek out input and information regarding the receptivity of these end user groups as the system was further developed and prepared for clinical testing.
Methods
A novel mHealth technology called iMHere (iMobile Health and Rehabilitation) was developed through the Rehabilitation Engineering and Research Center on Telerehabilitation (RERC-TR). During the 38th Annual Spina Bifida Conference held in Anaheim, California (June 26 – 29, 2011) two informative and interactive sessions were delivered by the lead authors of this article. Development of iMHere and usability testing of the individual smartphone apps was underway at the time the survey data in this study was collected. Researchers wanted to gather additional information from a larger audience (beyond usability testing subjects) regarding overall impressions of the iMHere system and its use in supporting self-management skills in persons with SB. This annual conference attracts a national audience and even some international participants. An educational format was utilized to explain the need for the iMHere system and how it can improve self-management skills in persons with SB. The first session was held specifically for healthcare professionals who work with persons diagnosed with SB. The second session was tailored for an audience of persons with SB, their family members and caregivers. Both sessions focused on identification and interventions for executive dysfunction outside of the school setting through adulthood including: independent living, vocation, self-care tasks, and social interaction skills. The presenters described mobile applications commonly referred to as “apps” to support ADLs. Presenters then highlighted their own work in developing a suite of apps designed for the SB population to help manage self-care routines and maintain wellness. Each of the specialized iMHere apps was demonstrated for the audience to view with screen shots similar to those shown in the figures of this article and live demonstration of the iMHere system’s two-way communication features. Screen shots of the clinician portal were also shown. Various examples of how an individual with SB may benefit from using a system such as this were provided as part of the presentation.
After researchers shared their own work in developing the iMHere system and demonstrated how each of the apps functioned, a consent script was read aloud to the audience and willing participants completed a survey. This study was approved by the University of Pittsburgh’s Institutional Review Board as part of the RERC-TR. The researcher-presenters specified that any member of the audience, who did not wish to participate in the study, simply did not need to complete and submit a survey. The surveys did not gather any identifiable data, but did request that subjects: indicate various categories of demographic information, respond to Likert scale questions and provide narrative comments. The surveys included six questions with both a seven-point Likert scale and open-ended narrative responses. The specific questions asked are listed in Tables 2 and 4. The following section provides a description of the iMHere system as was shared with the audiences of the two conference sessions.
Table 2:
Clinicians’ Responses to Likert Scale Questions
| Likert Scale Questions | N | Median | # and % of Responses | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |||
| Q1: I feel comfortable using technology in my everyday life. | 35 | 1.0 | 20 56% |
5 14% |
5 14% |
3 8% |
2 6% |
0 - |
0 - |
| Q2: I feel comfortable using technology in my clinical practice. | 36 | 2.0 | 14 39% |
7 19% |
9 25% |
9 5.6% |
2 5.6% |
2 5.6 % |
0 - |
| Q3: I would use this system in my clinical practice. | 36 | 1.0 | 17 47% |
9 25% |
2 5.6% |
1 2.8% |
0 - |
2 5.6% |
2 5.6% |
| Q4: The system seems simple to use for a person with SB. | 33 | 2.5 | 9 25% |
7 19% |
8 22% |
6 17% |
2 5.6% |
0 - |
0 - |
| Q5: The system seems simple for a clinician to use. | 32 | 2.0 | 12 33% |
11 31% |
2 5.6% |
6 17% |
1 2.8% |
1 2.8% |
0 - |
| Q6: I believe using a system such as this would make a strong positive impact to improve the health of persons with SB. | 33 | 1.5 | 16 44% |
9 25% |
4 11% |
0 - |
2 5.6% |
0 - |
1 2.8% |
Table 4:
Responses of Persons with SB, Family Members & Caregivers to Likert Scale Questions
| Likert Scale Questions | N | Median | # and % of Responses | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |||
| Q1: I feel comfortable using technology in my everyday life. | 71 | 1.0 | 40 56% |
17 24% |
8 11% |
0 - |
3 4.2% |
1 1.4% |
2 2.8% |
| Q2: I feel comfortable using technology in my clinical practice. | 70 | 1.0 | 46 66% |
5 7% |
8 11% |
2 2.9% |
2 2.9% |
4 5.7% |
1 1.4% |
| Q3: I would use this system in my clinical practice. | 70 | 1.0 | 39 56% |
14 20% |
8 11% |
6 8.6% |
0 - |
2 2.9% |
1 1.4% |
| Q4: The system seems simple to use for a person with SB. | 66 | 1.0 | 34 52% |
18 27% |
5 7.6% |
6 9.1% |
1 1.5% |
0 - |
2 3% |
| Q5: The system seems simple for a clinician to use. | 59 | 1.0 | 40 68% |
8 14% |
3 5.1% |
5 8.5% |
0 - |
0 - |
3 5.1% |
| Q6: I believe using a system such as this would make a strong positive impact to improve the health of persons with SB. | 66 | 1.0 | 48 73% |
6 9.1% |
6 9.1% |
3 4.5% |
0 - |
1 1.5% |
2 3.0% |
iMHere - mHealth Technology System
The iMHere system consists of software including a suite of smartphone apps specifically designed for persons with SB, a clinician portal, and a communication system connecting the two. It is important to note the use of the iMHere system is not intended to replace traditional, in-person medical care. Nor is it to be used as an emergency response system. Instead, users are prompted to perform routine self-care tasks in a timely manner through the automated system. By performing these tasks as scheduled, the user is proactively reducing the possibility of developing secondary conditions. However, since it is not feasible to prevent every problem an individual may encounter, the system also provides non-emergency support and monitoring to help educate individuals regarding self-management of chronic conditions and accessing health care services as needed.
Figure 1 shows the home screen of the iMHere suite of apps. Each individual app is accessed by an icon to represent the purpose of the corresponding self-care activity. The MyMeds app is highlighted in Figure 1. All of the apps include a scheduling component to program reminders for performance of self-care activities. Five apps were demonstrated as part of this survey study:
Figure 1:

iMHere home screen with icons for all current apps
MyMeds is an app that provides cues to remind the user to take his or her medication at recommended times, tracks the number of doses and reminds the user to contact the pharmacy for refills. Generic and brand names are integrated into the app to make entry of one’s medication regimen easy. The user then also has a portable list of medications to share with clinicians which can be easily revised as prescriptions change.
Figure 2 shows what the user sees on the home screen of the smartphone when the MyMeds alarm is activated to alert the user to take his or her medication.
Figure 2:
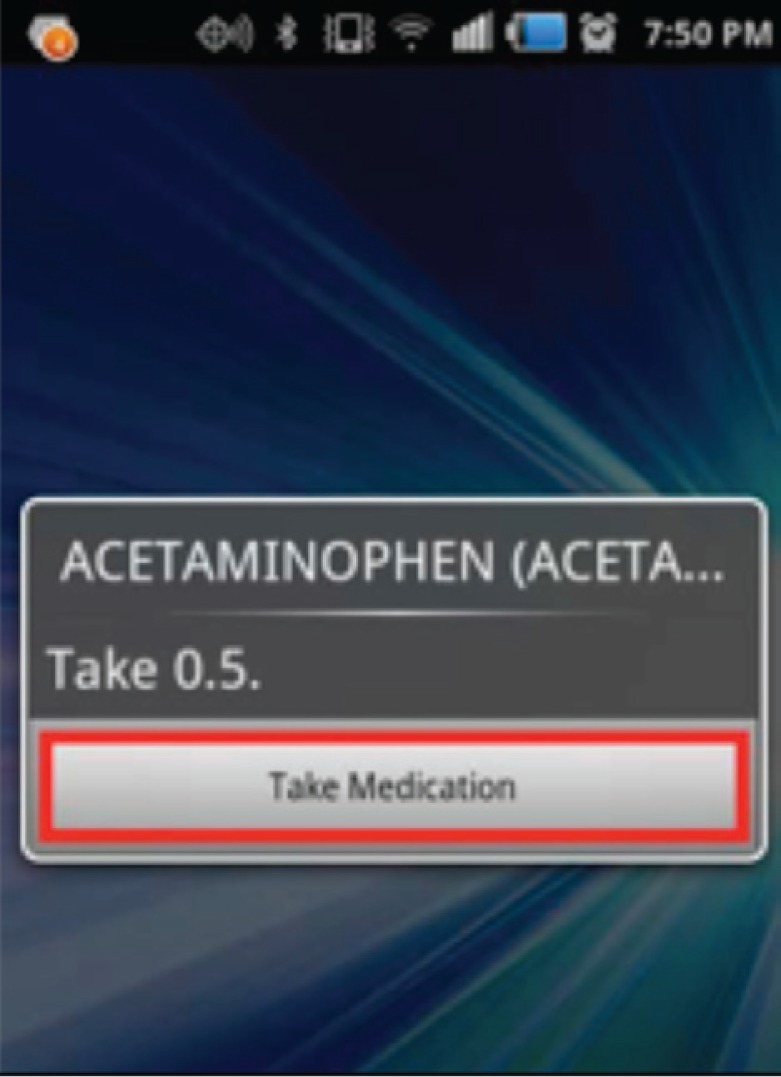
MyMeds alarm/reminder to take medication
TeleCath allows the user to program the app to receive reminders to catheterize the bladder. Once the reminder is provided, the user can then easily indicate whether or not he or she encountered any problems when catheterizing (e.g., low volume output, bleeding, etc.). The information is automatically updated in real time to quickly alert the clinician of the difficulty the person is encountering when performing this self-care task as depicted in Figure 3. This app can also be set to ask users once per day about frequency of incontinence (Figure 4). Incontinence is a sign of an ineffective bladder management program. Tracking this information on a daily basis may help revise the plan of care including frequency of catheterization, fluid intake or prescription of medications frequently utilized in the urologic care of persons with SB.
Figure 3:
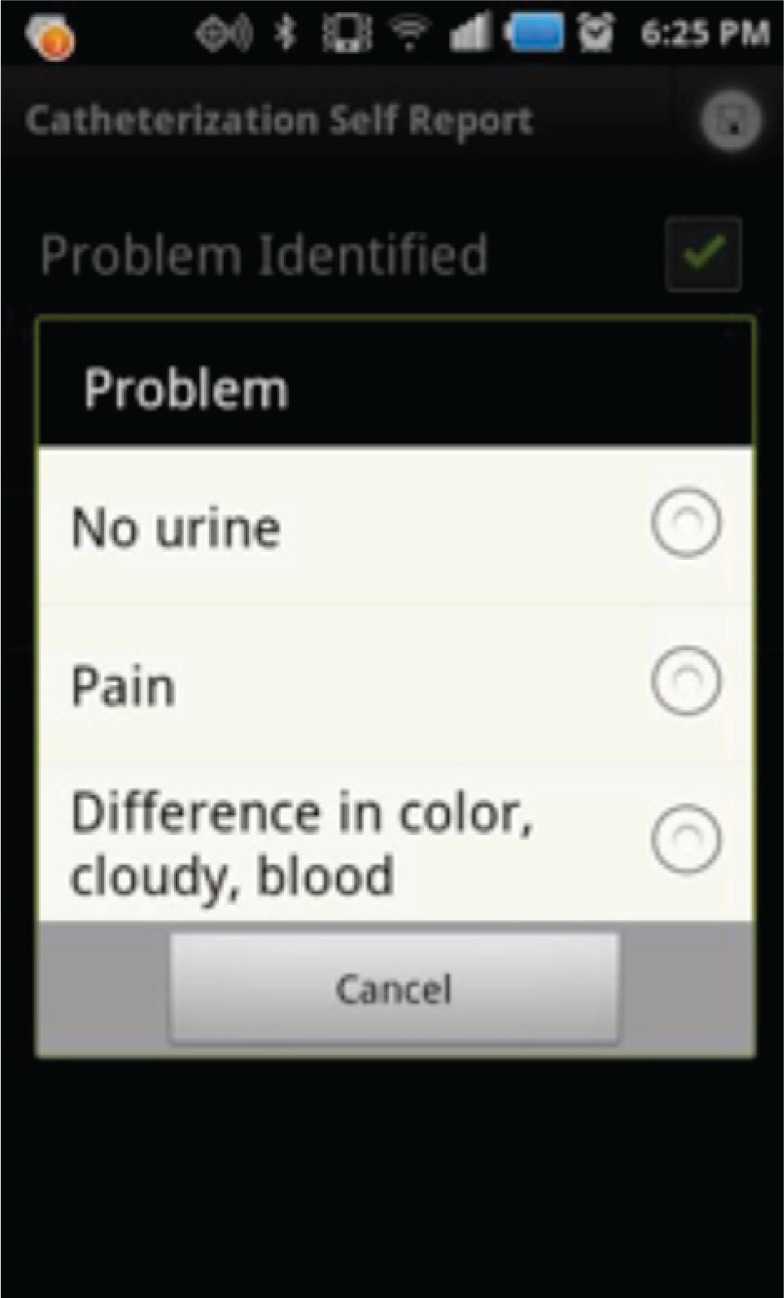
TeleCath screen to report problems encountered
Figure 4:
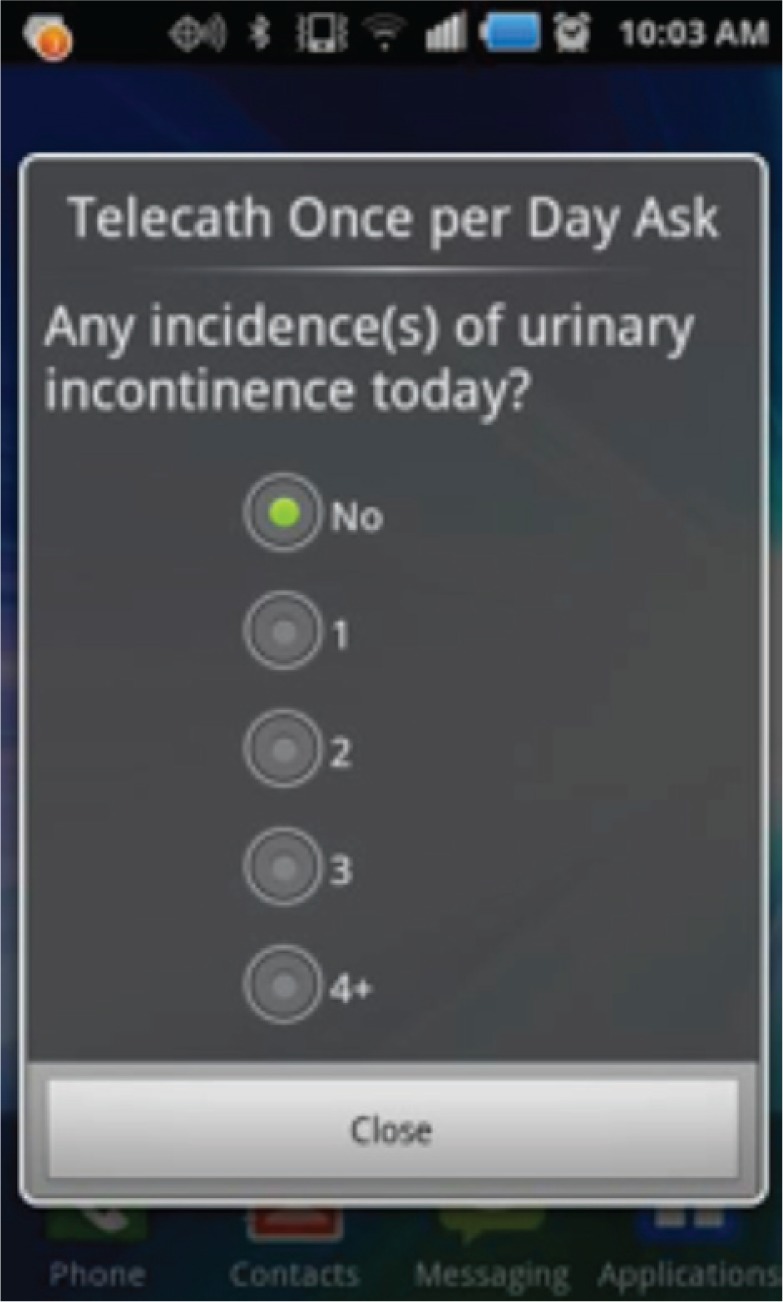
TeleCath requests information regarding incontinence on a daily basis
BMQ, the bowel movement cue (BMQ) app, provides reminders, much like TeleCath. However, these reminders can be set less frequently, such as every other day, or every third day, to reflect common bowel program schedules using enemas or medications. Figure 5 shows the screen utilized in setting alarms within the app, which can then serve as a reminder to perform one’s bowel management program. The save button is highlighted in this screenshot and is a common feature consistent within the design of all of the apps. This design consistency increases ease of use. Also, like TeleCath, BMQ allows the user to easily and quickly alert clinicians if problems are encountered while performing one’s bowel management program.
Figure 5:
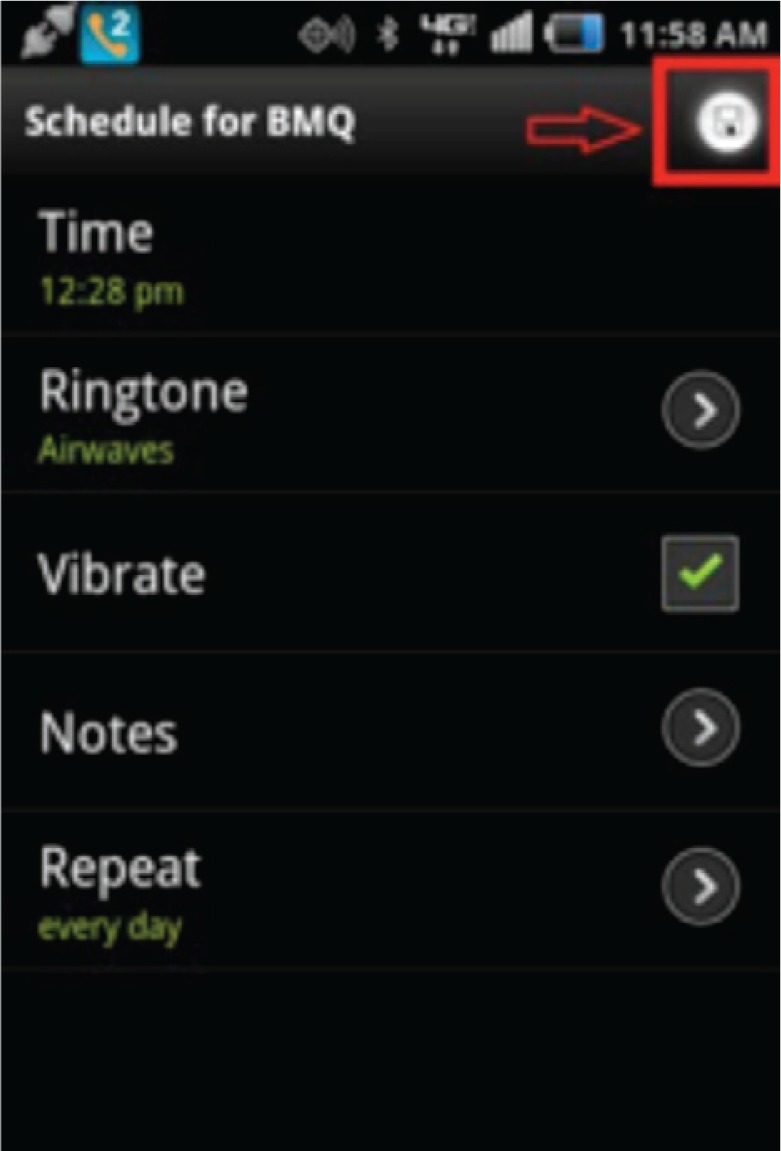
Screenshot of BMQ showing screen to program reminders
Mood Tracker, (shown in Figure 6) is an app that asks a series of ten yes/no questions to help detect a person’s level of depression. Questions included in this app are based on those developed as a depression screening by Mental Health America, formerly known as the National Mental Health Association (MHA, 2008). A newer version of the screening tool is now available through MHA; however, the questions for the app are based on the original version which was available during the development of this app in 2010. Mood Tracker can be set as frequently as daily, but is recommended for weekly or bi-weekly use similar to MHA’s Depression Screening Quiz. Clinicians are then able to remotely monitor mood over time to determine changes and intervene if a user shows an increase in depressive symptoms as indicated through their responses to the questions. If a user indicates a high level of depressive symptoms 5/10 or greater (answers yes to five or more questions) or indicates the presence of suicidal thoughts, the app is programmed to provide the user with the option to call 9-1-1 emergency response number or the mental health crisis line designated for his or her geographic region. Both phone numbers are programmed into the Mood Tracker app to provide this information automatically to the user upon completion of the questions.
Figure 6:
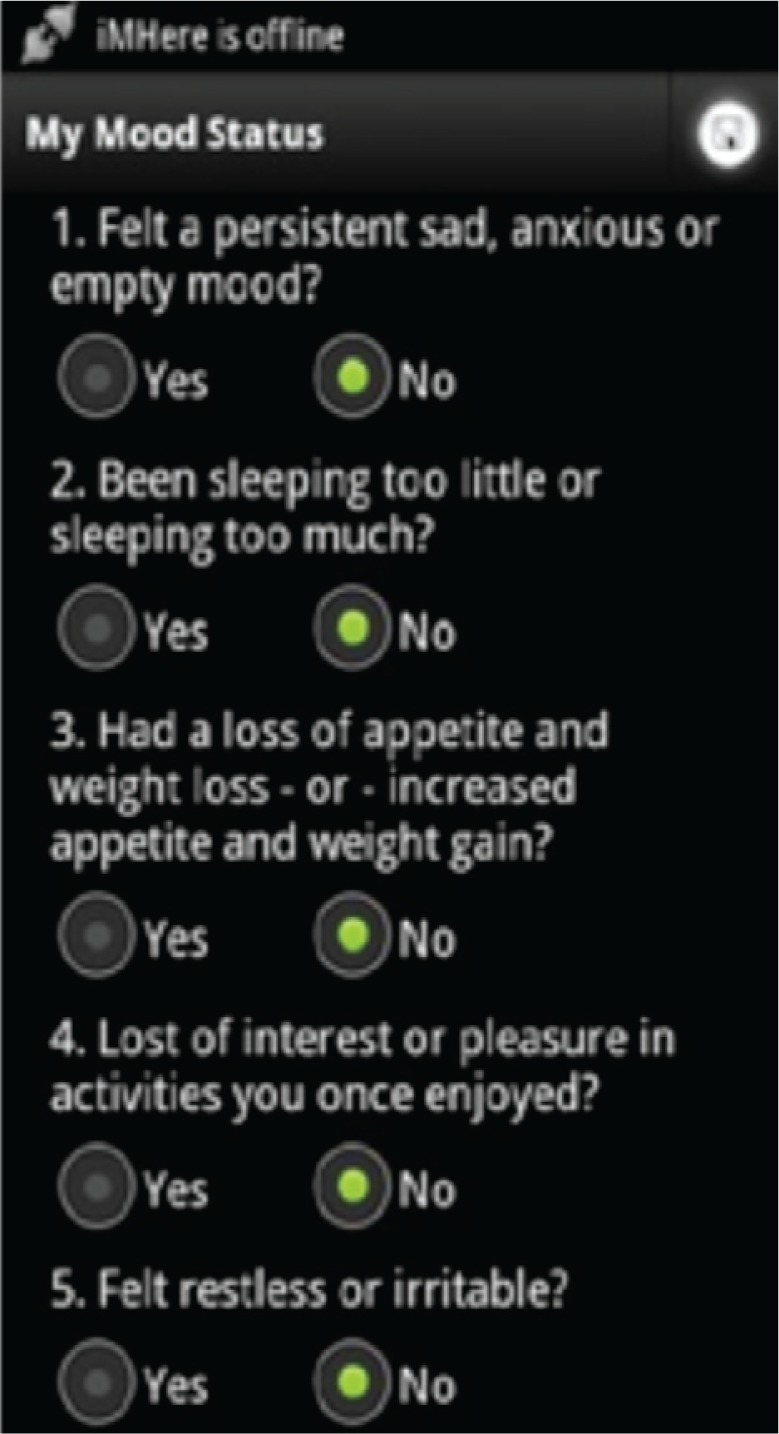
Mood Tracker provides a series of 10 yes/no questions to determine the user’s level of depression
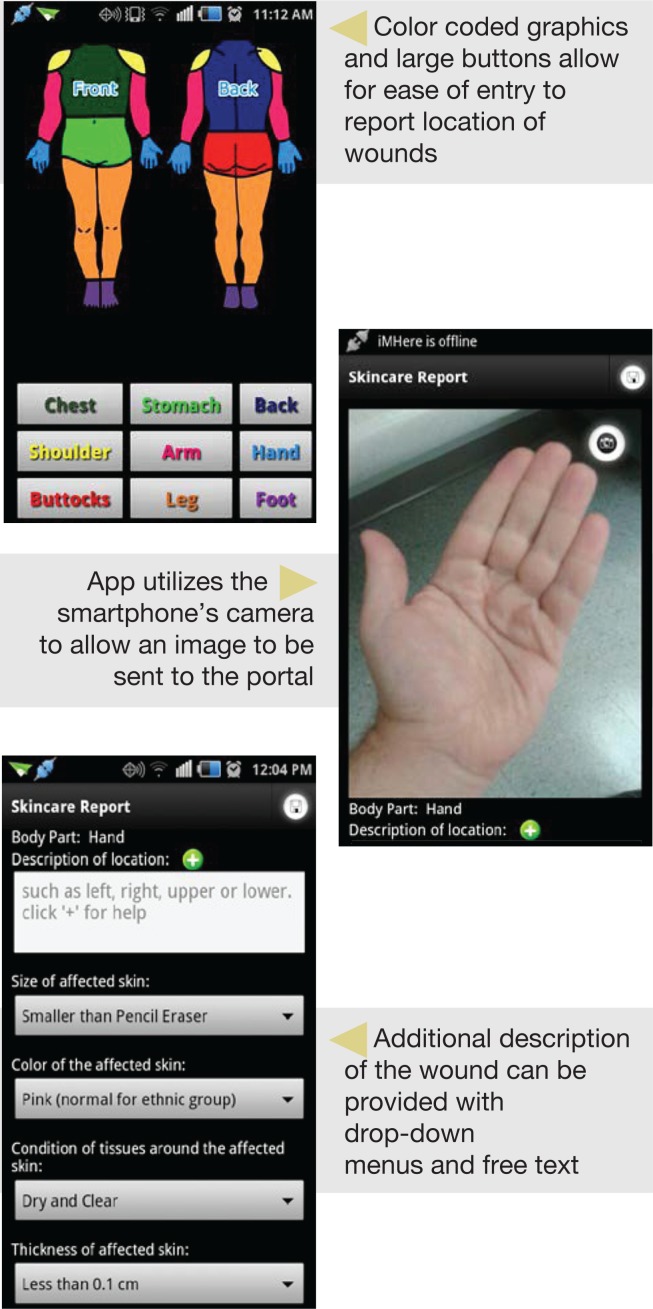
SkinCare is the most complex of the iMHere apps developed to date. SkinCare has several screens (Figure 7) and features: reminders that can be set to cue users to perform daily skin checks as a preventative measure. If skin breakdown or injury occurs, users can report it to the monitoring clinician using a combination of text feedback and also send a picture of the wound. The wound is tracked over time to monitor progress in healing and/or provide instructions for how to best care for the wound. See an example of wound tracking in Figure 9 of the clinician portal.
Figure 7:
The Skin Care App has several screens to allow user to report wounds
Figure 9:

Symbol indicates the patient does not require attention.
Persons are able to customize use of the system by using only the apps that are relevant to their individual needs. For instance, not all persons with SB complete a bowel program; therefore the BMQ app may not be utilized. Depression is a common problem for many persons with SB, but not every person will deem it necessary to monitor mood if he or she has not encountered mental health problems. A person can use only one, a few, or all of the apps for a customized remote wellness program.
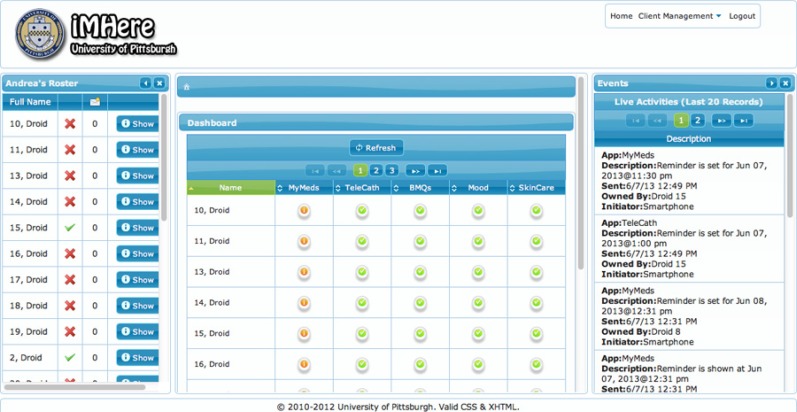
Web-Based Clinician Portal
The clinician portal is a web-based tool to monitor the activity of a caseload of patients currently using the iMHere app. The apps send monitoring data to, and receive self-care plans from, the web-based clinician portal. This portal includes a graphical dashboard for clinicians to monitor aggregate real-time data from all patients, and to identify patients in need of assistance. The clinician uses the portal to tailor treatment plans for each patient and can push the plan to the smartphone apps. It can be used to schedule drug regimens and maintenance plans, and to view any schedule a patient sets. Any problems the patient reports are communicated to the portal and are flagged for clinicians’ attention on the portal dashboard. A patient may also create or modify self-care plans from his or her smartphone, and these changes will be synchronized with the portal for the clinician’s review. The portal dashboard has been designed to allow the clinician to quickly review numerous patients at once, and to provide quick access to the areas of the portal that need attention. By clicking on Attention Flags on the Dashboard iMHere will direct the monitoring clinician or WC to the area that needs attention (Figure 8).
Figure 8:
iMHere Clinician Dashboard provides a graphical overview of incoming information from the patients’ apps. Clinicians can quickly scan the dashboard and determine how to prioritize contact with patients based on this information.
The portal maintains a persistent connection with all registered patients’ devices currently running iMHere. The patients whose devices are powered on and currently connected will be indicated on the Patient Roster with a green checkmark. The Patient Roster can be used to bring up the Client Details Box which has the advantage of allowing the clinician to navigate one patient at a time. The clinician portal provides a dashboard using symbols to make it easy to visually review a caseload of patients’ incoming information. The symbols help the clinician to discern which patients do not require attention (see Figures 9, 10 & 11).
Figure 10:

Symbol indicates the patient may need attention.
Figure 11:

Symbol indicates the patient needs immediate attention.
Additional description regarding the technical aspects of the development of the iMHere system will be available in future publications. Information is also included in this paper to describe the security of the iMHere system, which meets all HIPAA regulations.
Results
Session 1: Clinicians Providing Services to Persons with SB Thirty-six audience members of the first session, held specifically for clinicians who work with persons with SB, elected to complete the survey and act as respondents. Twenty of the respondents (55.6%) were nurses. A variety of other professionals, as described in Table 1, also participated in the survey.
Table 1:
Demographic Descriptive Statistics of Clinician Respondents
| Professional Background | # of Respondents | Percentage |
|---|---|---|
| Physician (MD) | 6 | 16.7% |
| PhD - Clinical / Research | 2 | 5.6% |
| Nurse | 20 | 55.6% |
| Social Worker | 3 | 8.3% |
| Occupational Therapist | 2 | 5.6% |
| Physical Therapist | 2 | 5.6% |
| Education (Teacher) | 1 | 2.8% |
| Total N = | 36 | 100% |
| Variable / Question | Mean | SD |
| # of Years in Clinical Practice | 20.6 | 13.7 |
| # of Years with SB Population | 10.7 | 11.0 |
Overall, these respondents were experienced, with an average of 20 years in practice. In addition, the respondents also had an average of over 10 years of experience with the SB population. The respondents’ answers to the survey questions on a seven-point Likert scale are summarized in Table 2. The Likert scale represents a respondent’s level of agreement according to the following qualitative descriptions: 1 = Very Strongly Agree, 2 = Strongly Agree, 3 = Agree, 4 = Neutral, 5 = Disagree, 6 = Strongly Disagree, 7 = Very Strongly Disagree. Therefore, the lower the score, the higher the respondents were in agreement with the statement.
The written narrative responses were transcribed verbatim from the survey forms for analysis. For both sets of surveys, the narrative responses were coded, sorted and categorized into themes independently by three researchers all familiar with utilizing the iMHere system. Themes were then compared across these three sets of data and agreement was achieved to increase the rigor of the qualitative analysis. By repeatedly reviewing the data, researchers collaborated to develop inductive ideas and interpretations about converging, recurring, and contradictory patterns -- along with illustrative examples (Hammersley & Atkinson, 2007).
Narrative Themes – Clinicians
Theme: Comfort in using technology
A mean Likert score of 1.29 for the group overall shows the majority of clinicians who participated in this survey are active users of smartphones or similar devices (e.g., tablets, computers) and applications (e.g., Facebook, texting, express scripts, to-do list apps). Narrative comments that support these scores include the following quotes:
“It [technology] has become a part of routine daily life.”
“Less labor intensive. Keeps connections.”
“Use technology to manage life tasks -alarm clock, to-do list, calendar.”
“Technology is daily developing new ways to save not only time, but money.”
However, other clinician-respondents provided some feedback to indicate they are not as comfortable with, or are resistant to use of technology. The following comments exemplify these clinicians’ hesitancy to incorporate use of technology:
“Technology has progressed so much in the last 10 years. [It’s] hard to keep up with what’s available and what’s relevant and useful in everyday practice. [I] need time and assistance to investigate technology.”
“I’m often a little resistant to new technology at first (for myself). I often question: “I’m getting by OK now, why spend more money on something new?”
“Tech info and content overload. [The electronic health record] is more complicated and slower than paper. Never seems to work as advertised.”
Theme: Efficient or burdensome?
A noteworthy theme presented by clinicians was whether or not introducing the iMHere technology into clinical practice would ease the workload of clinicians or unintentionally create a burden. The respondents relayed numerous possible positive aspects of implementation of a system such iMHere in their clinical practice. These two comments exemplify these thoughts:
“To save time checking up on people - you will know right away! So awesome.”
“I like the user-friendly aspect. Also, many of our patients have smartphones and could benefit.”
A follow-up question specifically inquired about potential barriers of implementing this system at their current institution and integration into clinical practice.
“I believe this has great potential; However, I am concerned it may be very time consuming, especially with complicated patients.”
“May increase practitioner workload to the point of becoming overwhelming.”
“We do not have the support we need for doing anything extra at this point.”
“Seems manageable with small number of patients, but could it rapidly take over all of your clinic time? RN coverage - currently have two nurses for > 300 patients.”
“Patients may send pictures of vacation, etc., [an] overuse...boundary issue.”
The following quote exemplifies concerns related to costs:
“Low income families cannot afford smartphones. If the clinic purchased a smartphone for a low income patient, I would be concerned about cost of the plan (service usage charges) and other family members ‘using’ or ‘borrowing the phone.’”
Many clinicians communicated great excitement, which shows their confidence in the potential for this program to improve the workflow within their practice setting(s):
“Like the idea of being able to track patterns of problems.”
“Solving problems in real time better than relying on memory - more accurate reactions of problems (real or perceived).”
Theme: Generalizable or exclusive?
The impact of SB upon individuals is incredibly varied in relationship to medical needs and cognitive and functional abilities. Is it possible to create a system that will meet the needs of the SB population as a whole? This concern was suggested by several clinicians in the following quotes:
“Such a wide level of cognitive issues - it would have to be a select group.”
“[Would] not support at the current time. Our clients would have to be chosen very carefully.”
“Varies person to person - may be easier for younger kids who grew up with technology.”
“Too many variables to assess. For some of my patients, yes. [For] some it would be too complicated.”
“Patients with SB think very concretely, so it would have to be very clear that they won’t get an immediate call back.”
“Anything available in Spanish?”
“Might be a challenge with SB [and] OCD [Obsessive Compulsive Disorder] dual diagnosis getting stuck on an issue.”
“Like an alarm, it can be ignored”
With this positive response to this idea of applicability, it becomes apparent that a target population is present. This idea is illustrated in the following responses:
“I think technology is a great motivator for my clients (age 0–21).
“This would be great for adolescents in helping them transition to adulthood.”
“I would like [to be able to use it] for cerebral palsy / other developmental disabilities.”
Theme: Immediate reports of health status
Several clinicians reflected this positive aspect of clinical application of the iMHere system:
“Like the idea of being able to track patterns of problems.”
“Solving problems in real time better than relying on memory - more accurate reactions of problems (real or perceived).”
Depending on the background of the clinician, past experiences may have positively or negatively affected their opinions of the iMHere system. However, it is clear that there is great excitement for iMHere and its ability to promote self-management skills for persons with SB. This can be seen in some concluding narrative comments from clinicians:
“Would help with focus, completion of activities, raise self-esteem when able to perform/complete activities.”
“Awesome! Could be life changing for both patients and providers!”
“Brilliant ideas - look forward to sharing this information with my patients and team.”
Session 2: Persons with SB, Family Members & Caregivers
The survey questions posed to persons with SB, family members, and caregivers were similar to those included in the clinicians’ survey with a few changes related to current use of technology (specific devices: cell phone, smartphone, iPod™, PDA, Electronic Tablet) as listed in Table 3.
Table 3:
Demographic Descriptive Statistics of Persons with SB, Family Members & Caregivers (N = 71)
| Role/Profession* | # of Respondents | Percentage |
|---|---|---|
| Person with SB | 19 | 26.8% |
| Family Member / Caregiver | 52 | 73.2% |
| Researcher (PhD) | 1 | 1.4% |
| Physical Therapist | 1 | 1.4% |
| Other Role / Relationship | 4 | 5.6% |
| Present Use of Popular Wireless Electronic Devices | ||
| Cell Phone | 44 | 62% |
| Smartphone | 34 | 47.9% |
| iPod™ | 26 | 36.6% |
| PDA | 4 | 5.6% |
| Electronic Tablet | 56 | 78.9% |
Please note - these categories are not mutually exclusive. Two individuals indicated they worked as clinicians in addition to being family members of persons with SB.
Narrative Themes - Adults with SB Family Members & Caregivers
Many of the parents/caregivers in this audience had younger children. The Likert scores in Table 4 indicate an overall high level of comfort. Many individuals felt they have been able to be more productive in their daily lives with the use of technology:
“It will help me stay on track.”
“Using technology on my phone has helped me accomplish more during the day by making lists and setting alarms.”
“I think it will be great because I have memory issues.”
“Allows multi-tasking as well as immediate information.”
However, the positive response to use of technology was not universal for this group. A few respondents indicated they struggle with technology and have preferences for other means to manage daily life:
“Technology seems to change every day. I feel like I am playing catch up.”
“Too much trial and error - not understanding manual.”
“Parent of several children, farm animals, house, etc. to care for - no time to mess with it.”
“I want to talk to a person in person.” I can’t stand messages or push this button for this or that. I want to ask questions and have my questions answered. Not tech-savvy 69-1/2 years old.”
“When I get to read I want to lie in bed, relax, and read. My eyes are better at reading large print. Not good with electronics.”
“I personally prefer less technology, but I see the importance of it and I’m learning.”
Theme: Time consuming for clinicians
Similar to concerns expressed by clinicians themselves, some persons with SB and/or family members and caregivers felt it may be burdensome on the clinician side:
“Concerned for the practicality of clinicians’ ability to handle/process so much incoming data, especially with statistic of number of persons with SB without a PCP [Primary Care Physician] and due to complexity of SB (adults specifically).
“It may take additional time for a busy professional.”
“...it can be overwhelming if a lot of patients are being followed.”
Theme: Applications beyond self-management and clinical practice
Several parents and individuals with SB commented on how a system such as this could be helpful beyond activities related to self-care. This feedback can be exemplified in the following narrative responses indicating interest and in trying out the features in their daily lives:
“Consider making these available independent of clinics. These would be helpful for children (even very young) as they are electronically adapting.”
“This is great for helping them remember when to do all of their many needed activities”
“Thank you for researching this. My 13 yr old has trouble remembering assignments or turning them in... Other interventions have not yet worked and she loves her cell phone. Great idea!”
“A lot of these ideas are great for my non-spina bifida child as well. Thank you.”
“My daughter has had problems remembering homework or turning it in. Thank you for the idea of [using apps for] recording assignments.”
“Developing grant to get iPads/iPhones into the hands of young adults with SB with personal health record and scheduling app. Would love to include these new apps when available.”
A few respondents were more skeptical as to whether or not it would be effective:
“Even a reminder may not work if I’m lazy.”
“My son likes technology; however, he may just turn it off.”
In addition, if a person has many tasks for which he or she requires frequent reminders the number of alarms could be overwhelming. As one respondent notes:
“People may not want to set and hear all of these alarms.”
There are several other concerns that were raised from this group which again indicate a system such as this would not be effective for every person with SB. One respondent to this survey noted that he or she has had nine children with SB over the years (likely as a foster parent). Observations were included as feedback:
“1) They break electronic devices fast and often, 2) They lose a lot, 3) Some bring up inappropriate pictures or use cell phones to charge thousands of dollars in phone charges with women or anyone else….Can’t leave anything out where it is convenient to use.”
In general, this group also sees great potential for the use of the system. Some general comments include:
“Especially for days that are out of the routine. Weekend cathing reminders would be helpful.”
“Now-a-days this is the way to go. We all have our cell phone on us. The fact that it alerts you when you have to do something and not put it off.” “Consider making these available independent of clinics. These would be helpful for children (even very young) as they are electronically adapting”
“I love the idea of TeleCath. My son’s so bad at telling time, but he always has a phone or iPod in hand”
“I think these would help me even more in my already independent life.”
“This seems awesome and very efficient. With all medical professionals converting to EMR, this is a no brainer.”
“I think that it would be great not just for clinics but for patients too. Cause we all hate going to doctors for small things. Nice to be able to take a pic and send. Then if doctors think they need to come in they can.”
Discussion
The open-ended section of the survey revealed some general concerns about the adoption of new technologies and excitement surrounding the introduction of the iMHere system. Receptivity seems to be closely related to an individual’s past experiences with technology in the clinic and personal use. Many clinicians already use technology for work or personal needs in their daily life. Overall, there were also more positive than negative scores and comments noting the benefits of the use of technology in clinical practice. However, several respondents indicated apprehension toward the introduction of any new technology, not specifically the iMHere system. Many of the concerns raised by the respondents were predicted, and careful planning around these issues may help to ensure a smooth introduction of such a system as iMHere within clinical practice settings.
Several clinicians expressed concern about time availability to monitor, manage information received, and respond to patients using such a system, as well as the costs associated with this time. This frequently discussed concern is one of great importance and has been recognized by the clinicians and developers of the system. Throughout the development and introduction of iMHere and the portal, constant communication with the development team that includes software developers and clinicians has allowed for improvements in the system. These improvements have been to ensure ease of use for both the patient and clinician. A specific example of designing with the clinician in mind includes the visual layout of the portal’s dashboard. Because of the simplicity of the symbols that indicate who has the problem, and what type and degree of health concern is present, with a quick glance, a clinician would be able to determine who needs attention. The goal of the system is to promote efficiency with regard to identification of potential problems the patient is experiencing along with seamless communication to follow-up and provide coordinated care.
Regarding the cost that would occur in supplying the SB population with smartphones brings about several discussion points including the responsibility and requirements of an individual to participate in a wellness program. Supplying a smartphone and a phone contract to an individual can be a pricy investment; however, when each patient is considered on an individual level an appropriate device and contract can be provided. The fear of losing or breaking a device is a reasonable concern and instances of loss and breakage will occur. However, the cost of the device and service plan may be offset by the cost of treating these preventable conditions (i.e., wounds and UTIs) on the part of the insurer, or the time and effort of triaging and managing the conditions on the part of the clinicians involved.
A potential user of the system would need to demonstrate that he or she can responsibly use the device. In setting up the usability testing and clinical trial for this project, we were wary of potential problems with overage charges. Accounts were established with unlimited voice, data and text, rather than set up to enforce a limit to the number of minutes or messages. The devices cannot be used to call outside of the U.S. and charges cannot be applied to the account for any phone services with fees (i.e., psychic readings, chat lines). All subjects are required to sign an agreement that the device would not be utilized for any sort of illegal activity (i.e., computer hacking, harassing others, dealing drugs, etc.). This agreement was included as part of the informed consent document approved by the IRB and signed by each participant.
The system was not designed to address more severe cognitive deficits (i.e., Intellectual Disability) or persons with severe mental illness (i.e. Schizophrenia, Bipolar Disorder), suicidal ideation and/or other conditions requiring continuous supervision. From a self-care perspective, the system can be tailored so that only the apps that are relevant are utilized. For instance, if the person never had any concerns related to depression, the Mood app would not need to be used. The researchers also recognize the birth rate of SB is more common among the Hispanic population than among non-Hispanic women (SBA, 2012a). The text included in the apps could be easily translated to create a Spanish version or versions in other languages.
The strong response to whether or not this system would be generalizable to the general population was matched with the same number of responses suggesting that iMHere may be applicable to populations other than adults with SB. Some respondents felt iMHere could assist in helping with other developmental disabilities and in the younger SB population. While the many issues presented have clinicians divided and have raised discussion, one that was agreed upon to be a beneficial feature of this program is the ability to report problems in the moment they occur. If a problem is reported when it occurs, patterns and habits can be recognized that would otherwise not be detected. Real-time storage of that information in the portal system eliminates the need for the patient to recall events. This will hopefully lead to collection of more accurate data by eliminating some recall bias, better allowing a clinician to correctly identify an issue and its potential cause.
Another concern presented by family and caregivers was that excessive reminders could become a distraction to participants and those around them. However, the alarms can be set to silent or vibrate mode so as not to disturb others in the user’s environment or call attention to the user. The system can be set up so that the user has only those apps he or she needs, thereby decreasing the number of reminders. For instance, if the person has no difficulty remembering to take his or her medication(s) in the morning, there is no need to use the MyMeds app.
Aside from the concerns raised by families and caretakers, they perceived applications for organizational skills outside of self-care to other tasks (e.g., household chores; homework for school, etc.). They also considered opportunities to improve performance even without the connection to medical professionals by using it as a support on their own, with parents monitoring their children’s activities. Much like the clinician-respondents, this group’s previous or current experience in utilizing technology in their daily lives greatly impacted their receptivity to use of the iMHere system.
Some clinical practices already maintain outreach activities and programs focused on wellness. For those practices that are primarily implementing a reactive approach to problems encountered by their patient population, this system would entail additional time and effort with long-term benefits of a cohort with fewer and less severe needs in the future. If an accurate population is chosen to utilize this technology it could allow for a cost-effective, efficient method to diagnose and treat problems faced by the SB population in a more accurate, timely and well documented method.
Limitations and Future Directions
This technology is appropriate only for a subset of the overall SB population. The system would not be appropriate for every individual with SB to effectively utilize in his or her everyday life. The system has limitations of applicability, whether it is due to comfort with the technology, degree of cognitive impairment or many other various factors. However, this system along with a training protocol has been designed to meet the needs of tech-savvy persons as well as first time phone owners. The system was designed for persons with SB who are residing in the community setting who do not have paid personnel to assist with needs throughout the day.
While the respondents to these surveys provided feedback from persons with SB, family members, caregivers and clinicians who provide care to persons with SB from all across the United States, we recognize this group is not a representative national sample. Attending the Annual National Spina Bifida Conference is an expense that many individuals, families and health care institutions cannot afford. In general, this sample is likely to be of higher socioeconomic status and various resources than the larger population affected by SB. The conference was held in San Diego, CA, and therefore most likely attracted larger numbers of attendees from closer to this geographic region.
Furthermore, individuals who have interest in learning more about the technology were more likely to attend these sessions, indicating a level of receptivity prior to even being shown samples of how the technology functions. Lastly, presenters were able to demonstrate the system only in a large group format. Audience members did not actually get an opportunity to trial the system themselves, nor utilize it in their everyday lives. The information gathered through this survey research was used to help partially guide a more in-depth usability study in which persons were issued smartphones and tested each app for at least one week in their home and community settings. Intensive usability testing was completed by individuals with SB, and results will be shared in a future publication. Also, a year-long clinical intervention study is on-going at the time of this writing. This clinical study is projected to conclude in the fall of 2013. Future publications to share the results of the clinical study are also planned.
In general, the results of this survey research indicate persons with SB, family members and clinicians are receptive to using the iMHere system in their everyday lives and clinical practice settings. A variety of potential factors that could influence the success of the system in supporting persons with SB to maintain health and wellness through self-management activities were revealed through the respondents’ narrative comments. This information was highly informative in guiding the design of our usability testing and clinical application of the iMHere system. Current research is exploring clinical outcomes from using this system with persons who have SB. Further research is needed to explore integration of a system such as this into the workflow of clinical practice settings. Future research and development plans include clinician-usability testing of the iMHere portal and expanding application of the system to other populations with disabilities and chronic conditions.
Figure 12:
iMHere Clinician View of SkinCare Entry which can allow monitoring of progress in wound healing over time.
Acknowledgments
This research was supported in part by grants from the National Institute on Disability and Rehabilitation Research (NIDRR) grant # H133E090002 Rehabilitation Engineering Research Center on Telerehabilitation (RERC-TR), and the Verizon Foundation.
References
- 1.American Association of Colleges of Nursing 2012. Nursing shortage fact sheet. Retrieved from http://www.aacn.nche.edu/media-relations/NrsgShortageFS.pdf.
- 2.American Telemedicine Association Telemedicine frequently asked questions (FAQs) 2012. Retrieved from http://www.americantelemed.org/learn/what-is-telemedicine/faqs.
- 3.Barf HA, Verhoef M, Jennekens-Schinnkel A, Post WM, Gooskens RH, Prevo AH. Cognitive status of young adults with spina bifida. Developmental Medicine & Child Neurology. 2003;45:813–820. doi: 10.1017/s0012162203001518. [DOI] [PubMed] [Google Scholar]
- 4.Bowman RM, McLone DG, Grant JA, Tomita T, Ito JA. Spina bifida outcome: A 25-year prospective. Pediatric Neurosurgery. 2001;34:114–120. doi: 10.1159/000056005. [DOI] [PubMed] [Google Scholar]
- 5.Brown J. Orthopaedic care of children with spina bifida: You’ve come a long way, baby! Orthopaedic Nursing. 2001;20(4):51–58. doi: 10.1097/00006416-200107000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Calvery M. Building skills for independence. Insights. 2008. Winter. pp. 10–11. Retrieved from http://www.spinabifidaassociation.org/atf/cf/%7BEED435C8-F1A0-4A16-B4D8-A713BBCD9CE4%7D/EXCERPTS.PDF.
- 7.Dennis M, Landry SH, Barnes M, Fletcher JM. A model of neurocognitive function in spina bifida over the life span. Journal of the International Neuropsychological Society. 2006;12:285–296. doi: 10.1017/S1355617706060371. [DOI] [PubMed] [Google Scholar]
- 8.Dicianno BE, Peele P, Lovelace J, Fairman AD, Smyers D, Halgas M, Burkholder K, Boninger ML. Specialty medical homes and wellness services in congenital and acquired spinal cord injury. (in press). American Medical Group Association Compendium of Chronic Care Practices.
- 9.Dicianno BE, Wilson R. Hospitalizations of adults with spina bifida and congenital spinal cord anomalies. Archives of Physical Medicine and Rehabilitation. 2010;91:529–535. doi: 10.1016/j.apmr.2009.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dillon CM, Davis BE, Duguay S, Seidel KD, Shurtleff DB. Longevity of patients with myelomeningocele. European Journal of Pediatric Surgery. 2000;10:33–39. doi: 10.1055/s-2008-1072412. [DOI] [PubMed] [Google Scholar]
- 11.Dise JE, Lohr ME. Examination of deficits in conceptual reasoning abilities associated with Spina Bifida. American Journal of Physical Medicine & Rehabilitation. 1998;77:247–251. doi: 10.1097/00002060-199805000-00011. [DOI] [PubMed] [Google Scholar]
- 12.Exner G, Burgdöffer H, Bohatyrewicz A, Bomnüter G, Wenck B. The lack of comprehensive care causing complications in patients with myelodysplasia. Paraplegia. 1993;31:102–104. doi: 10.1038/sc.1993.17. [DOI] [PubMed] [Google Scholar]
- 13.Hammersley M, Atkinson P. Ethography: Principles in practice. 2nd ed. New York: Routledge; 2007. [Google Scholar]
- 14.Hayden PW, Davenport SL, Campbell MM. Adolescents with myelodysplasia: Impact of physical disability on emotional maturation. Pediatrics. 1979;64(1):53–59. [PubMed] [Google Scholar]
- 15.Hunt GM, Oakeshott P, Kerry S. Link between the CSF shunt and achievement in adults with Spina Bifida. Journal of Neurology, Neurosurgery & Psychiatry. 1999;67:591–595. doi: 10.1136/jnnp.67.5.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iddon JL, Morgan DJR, Loveday C, Sahakian BJ, Pickard JD. Neuropschological profile of young adults with spina bifida with or without hydrocephalus. Journal of Neurology, Neurosurgery & Psychiatry. 2004;75:1112–1118. doi: 10.1136/jnnp.2003.029058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Istepanian R, Laxminarayan S, Pattichis CS, editors. M-Health: Emerging mobile health systems. New York, NY: Springer; 2005. [Google Scholar]
- 18.King GA, Shultz IZ, Steel K, Gilpin M, Cathers T. Self-evaluation and self-concept of adolescents with physical disabilities. American Journal of Occupational Therapy. 1993;47:132–140. doi: 10.5014/ajot.47.2.132. [DOI] [PubMed] [Google Scholar]
- 19.Mahmood D, Dicianno B, Bellin M. Self-management, preventable conditions and assessment of care among young adults with myelomeningocele. Chid: Care, Health and Development. 2011;37:861–865. doi: 10.1111/j.1365-2214.2011.01299.x. [DOI] [PubMed] [Google Scholar]
- 20.Mahone EM, Zabel TA, Levey E, Verda M, Kinsman S. Parent and self-report ratings of function in adolescents with myelomeningocele and hydrocephalus. Child Neuropsychology. 2002;8:258–270. doi: 10.1076/chin.8.4.258.13510. [DOI] [PubMed] [Google Scholar]
- 21.Menehan K. Improving chronic illness care: A RWJF national program. Robert Wood Johnson Foundation; 2011. Retrieved from http://www.rwjf.org/content/dam/farm/reports/program_results_reports/2011/rwjf71050. [Google Scholar]
- 22.Mental Health America Depression screening. 2008. Retrieved from http://www.nmha.org/ Alternate depression screen available at: http://www.mentalhealthamerica.net/llw/depression_screen.cfm.
- 23.McCue M, Fairman A, Pramuka M. Enhancing quality of life through telerehabilitation. Physical Medicine and Rehabilitation Clinics of North America. 2010;21:195–205. doi: 10.1016/j.pmr.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 24.Neilsen Company Neilsen tops of 2012: Digital. 2012. Retrieved from http://www.nielsen.com/us/en/newswire/2012/nielsen-tops-of-2012-digital.html.
- 25.Ouyang L, Grosse SD, Armour BS, Waitzman NJ. Health care expenditures of children and adults with spina bifida in a privately insured U.S. population. Birth Defects Research. 2007;79:552–558. doi: 10.1002/bdra.20360. [DOI] [PubMed] [Google Scholar]
- 26.Sandler A. Living with spina bifida: A guide for families and professionals. The University of North Carolina Press; 1997. (ISBN 0-8078-4657-0) [Google Scholar]
- 27.Sawin KJ, Bellin MH, Roux G, Buran CF, Brei TJ. The experience of self-management in adolescent women with spina bifida. Rehabilitation Nursing. 2009;34(1):26–38. doi: 10.1002/j.2048-7940.2009.tb00245.x. [DOI] [PubMed] [Google Scholar]
- 28.Spina Bifida Association of America Genetics and spina bifida (Fact Sheet) 2012a. Retrieved from http://www.spinabifidaassociation.org/atf/cf/%7B85F88192-26E1-421E-9E30-4C0EA744A7F0%7D/Genetics%20and%20Spina%20Bifida.pdf.
- 29.Spina Bifida Association of America Hydrocephalus and shunts (Fact Sheet) 2012b. Retrieved from http://www.spinabifidaassociation.org/atf/cf/%7B85F88192-26E1-421E-9E30-4C0EA744A7F0%7D/Hydrocephalus%20and%20Shunts.pdf.