Commentary on: Kir S, White JP, Kleiner S, Kazak L, Cohen P, Baracos VE, Spiegelman BM. Tumour-derived PTH-related protein triggers adipose tissue browning and cancer cachexia. Nature 2014;513:100–104.
This month's headlines in Nature feature a return engagement for PTHrp in cancer biology, albeit this time as an inducer of cancer cachexia.1 This reminds us of the re-emergence of Cicadas from their underground nymph stage every seventeen years. That event, always much heralded in the press, re-awakens our awareness of life's diversity and rhythms but also reminds us that many original concepts in science re-emerge in novel forms; PTHrp is a prime example. Fuller Albright in the 1940s postulated the existence of a factor secreted by tumor cells that caused hypercalcemia.2 In 1987, several groups independently identified a parathyroid hormone (PTH)-like peptide secreted from various tumors that was responsible for the hypercalcemia of malignancy.3,4,5,6 Later studies found that high levels of PTHrp were a bad prognostic sign in malignancies and were associated with cancer cachexia, although most related the wasting syndrome to severe hypercalcemia.7 At the same time, work from other investigative groups delineated the critical role of PTHrp in fetal development and postnatal epithelial growth and differentiation.8,9 In particular, as many readers of BoneKey appreciate, PTHrp is recognized as an important modulator of mammary, placenta, skin, cartilage and bone homeostasis. More recently, an analog of PTHrp is nearing completion in a phase III clinical trial as an anabolic agent for the treatment of osteoporosis. And now, in the Journal Nature, Kir et al.1 suggest that PTHrp is a mediator of adipose tissue browning and tumor-induced cachexia.
Malignancies as well as chronic diseases such as congestive heart failure cause profound muscle wasting, loss of fat mass and dramatic weight loss, ultimately contributing to infections and death. The appearance of cachexia almost invariably means an inability to respond to further therapies and is a bad prognostic sign. Although anorexia contributes to weight loss, the syndrome of cachexia is also associated with negative energy balance and is more complex than simply a loss of appetite. Animal models can recapitulate tumor-induced cachexia although the mechanisms responsible for the syndrome have remained unclear, particularly because anti-cytokine therapy for high levels of tumor necrosis factor and interleukin-6 are ineffective in ameliorating the wasting syndrome.
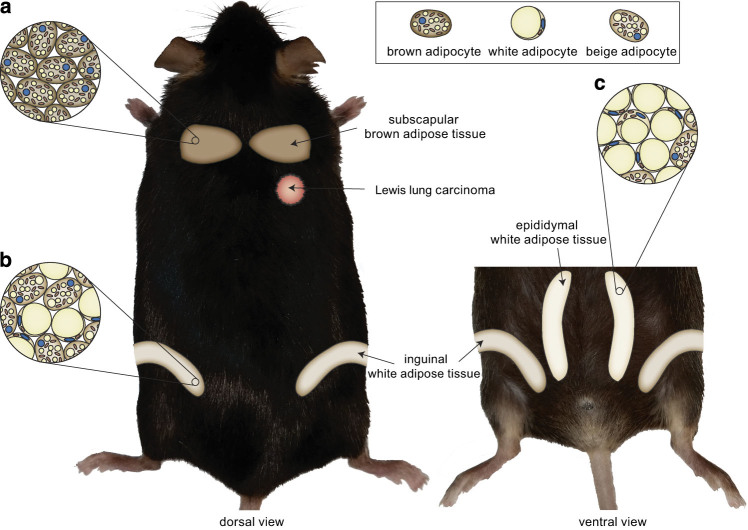
Kir et al.1 used the Lewis lung carcinoma (LLC) model to address the issue of tumor-induced cachexia. Transplantation of LLC cells into B6 mice resulted in weight loss, associated with greater overall heat production and increased oxygen consumption despite normal food intake and no change in physical activity. Not surprisingly, fat mass declined dramatically, but, in a key finding, was more accelerated in inguinal depots that normally contain genes responsible for ‘browning' and in interscapular brown adipose tissue (BAT; Figure 1). BAT maintains thermogenesis in neonates through fatty acid β-oxidation and mitochondrial biogenesis, in contrast to white adipose tissue (WAT) in which fatty acids are incorporated into triglycerides for storage. With advancing age, BAT function declines although recent work from several groups have shown the presence of functional BAT by PET/CT imaging in young, thin adults.10 Interestingly, the volume of BAT is directly related to bone mass in such individuals, possibly through its relationship to muscle as both share a common progenitor induced by the differentiation factor, Myf5.11 Additionally, several groups, spearheaded by the Spiegelman laboratory, have shown that WAT can be induced during β-adrenergic stimulation to exhibit ‘brown like' characteristics including fatty acid oxidation, mitochondrial biogenesis, expression of browning genes such as Ucp1 and Dio2, as well as Prdm16, an essential browning transcription factor.12 Uncoupling protein 1 (UCP1) is essential for thermogenesis, as it uncouples the electron transport chain from ATP production for heat generation and is the hallmark of a ‘browning' phenotype. However, unlike BAT, browning of WAT through enhanced sympathetic tone has been associated with bone loss.13 Nevertheless, peptides that induce brown-like adipogenesis as a means to dissipate energy rather than store it, have become a major therapeutic goal for the treatment of obesity.
Figure 1.
Tumor-induced cachexia results in browning of inguinal fat. After transplantation of Lewis lung carcinoma cells, B6 mice had reductions in fat pad mass and ‘browning' of white adipose tissue depots. Classical brown adipose tissue (BAT) depots, such as interscapular BAT, contain brown adipocytes (a) while inguinal white adipose tissue (WAT) depots normally contain white adipocytes, but demonstrate the presence of brown-like adipocytes (b) after tumor transplantation. Epididymal WAT also contains white adipocytes, although some ‘browning' (c) was seen in this model by histology.
The key finding by the Spiegelman group that inguinal fat (the most brown-like of the depots) and interscapular BAT expressed higher levels of genes associated with thermogenesis in the LLC-transplanted mice led those investigators to address whether ‘browning' was a major factor in cachexia. For this they turned to their most recently created model of impaired browning, a mouse with deletion of Prdm16 in fat tissue.14 This animal model exhibits virtually no browning with exposure to thermogenic stimuli and has adipocytic characteristics of visceral fat (i.e., macrophage infiltration in the stroma between cells and large expansive cells that are unilocular with few mitochondria). When LLC tumors were implanted in the fat-specific Prdm16-deficient mice, adipose wasting was prevented and Ucp1 and Dio2 expression were not changed whereas tumor size and muscle mass remained constant. Then, through several discovery steps using LLC cell-conditioned media, this group found that members of the EGF family and PTHrp induced Ucp1 expression in primary adipocytes. However, when EGF receptor inhibitors were used, ‘browning' persisted, suggesting that PTHrp was the inducing factor. To test that tenet, the investigators demonstrated PTHrp's ability to induce browning in primary adipocytes isolated from the inguinal depot of B6 mice. Moreover, PTHR1 was noted to be highly expressed in adipose tissue and injection of antibodies to PTHrp prevented LLC tumor induction of ‘browning', reduced in vivo oxygen consumption and prevented muscle wasting. Finally, the authors studied 47 patients with metastatic non-small cell lung cancer or colorectal cancer but no hypercalcemia and found higher energy expenditure, lower lean body mass and significantly detectable levels of PTHrp compared with another group of patients with no detectable PTHrp and normal energy expenditure. In sum, the investigators concluded that PTHrp from malignant cells drives the thermogenic/browning program in adipose tissue, although other factors may coordinate with PTHrp to induce muscle wasting.
How does this finding inform bone biologists and clinicians? First and foremost, there is a concern that sustained PTH (or in this case PTHrp) secretion working through the PTHR1 could have deleterious effects on whole-body homeostasis in normal individuals. This has clearly not been demonstrated in patients with primary hyperparathyroidism.15 However there have been studies that have used humanized anti-PTHrp antibodies to treat animal models bearing human lung carcinomas. These animals were hypercalcemic and had cachexia, which could be treated with the humanized antibody.16,17 Moreover, another example in nature is a gain of function mutation in the PTHR1 gene that leads to constitutive activation causing Jansen metaphyseal chondrodysplasia with skeletal features similar to hypophosphatasia and rickets.18 Although rare, some adults have been reported to have the disorder, yet there is no phenotypic evidence of metabolic disturbances. Hence it is conceivable that only in the setting of a malignancy in which other tumor-mediated factors are present will PTHrp induce browning and cachexia. Nevertheless, although no previous adverse metabolic signals have been detected, it seems reasonable to re-examine data from the few individuals who have ectopic production of PTH from tumors, as well as from subjects treated long term with PTH1-84 for hypoparathyroidism to test their hypothesis. Second, it becomes imperative that, as drug development proceeds in a direction focused on enhancing ‘browning' and reducing fat mass, off-target skeletal effects be examined. It is likely that the effects of brown adipogenesis on skeletal mass depend on the mechanism; for example, sympathetic excess or administration of FGF-21 cause bone loss,19 whereas in an animal model of FoxC2 overexpression in fat cells, browning is associated with increased bone mineral density.20 Third, we need to more clearly delineate the interaction between β2AR and PTHR1 signaling. Both are G protein-coupled receptors, and work from Hanyu et al.21 demonstrated an important synergism such that deletion of β2AR leads to impairment in the anabolic actions of PTH. Hence, there is likely to be cross talk between the two receptors through activation of PKA that may mediate the catabolic effects demonstrated by Kir et al.1 Finally, understanding the metabolic demands pressed upon the osteoblast (and adipocyte) by PTH needs better clarification. Bill Neumann and Bob Brommage22 in the late 1970s demonstrated clearly that PTH induces glycolysis to fuel the energy needs of the differentiating osteoblast. On the other hand, Kir et al.,1 using primary adipocytes (Seahorse XF Analyzer) and ex vivo adipose tissue (Clark electrode), show that PTHrp induces oxidative phosphorylation. Is the PTH (PTHrp) effect cell specific (osteoblast vs adipocyte) and if so, how does that translate at the remodeling level to individual cellular components of the niche?
In sum, the work of Kir et al.1 once again reinforces the intimate relationship between skeletal factors and energy metabolism. It is remarkably coincidental that chronically elevated PTHrp could have catabolic effects on whole-body energy (even if this is limited only to browning and not to the cachexia syndrome), whereas intermittent PTHrp and PTH is persistently anabolic for the skeleton. Until we clarify the long-standing PTH paradox (i.e. the effects of chronic vs intermittent administration) as it relates to bone metabolism, it is going to be difficult to fully understand the skeletal implications of the current study, but we can certainly say that the paper by Kir et al.1 has led PTHrp to come ‘full circle' from its origins in the cancer field.
Footnotes
The authors declare no conflict of interest.
References
- Kir S, White JP, Kleiner S, Kazak L, Cohen P, Baracos VE et al. Tumour-derived PTH-related protein triggers adipose tissue browning and cancer cachexia. Nature 2014;513:100–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case 27461. New Engl J Med 1941;225:789–791. [Google Scholar]
- Moseley JM, Kubota M, Diefenbach-Jagger H, Wettenhall RE, Kemp BE, Suva LJ et al. Parathyroid hormone-related protein purified from a human lung cancer cell line. Proc Natl Acad Sci USA 1987;84:5048–5052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juppner H, Abou-Samra AB, Uneno S, Gu WX, Potts JT Jr, Segre GV. The parathyroid hormone-like peptide associated with humoral hypercalcemia of malignancy and parathyroid hormone bind to the same receptor on the plasma membrane of ROS 17/2.8 cells. J Biol Chem 1988;263:8557–8560. [PubMed] [Google Scholar]
- Strewler GJ, Stern PH, Jacobs JW, Eveloff J, Klein RF, Leung SC et al. Parathyroid hormonelike protein from human renal carcinoma cells. Structural and functional homology with parathyroid hormone. J Clin Invest 1987;80:1803–1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orland SM, Stewart AF, Livolsi VA, Wein AJ. Detection of the hypercalcemic hormone of malignancy in an adrenal cortical carcinoma. J Urol 1986;136:1000–1002. [DOI] [PubMed] [Google Scholar]
- Iguchi H, Onuma E, Sato K, Sato K, Ogata E. Involvement of parathyroid hormone-related protein in experimental cachexia induced by a human lung cancer-derived cell line established from a bone metastasis specimen. Int J Cancer 2001;94:24–27. [DOI] [PubMed] [Google Scholar]
- Vortkamp A, Lee K, Lanske B, Segre GV, Kronenberg HM. Regulation of rate of cartilage differentiation by Indian hedgehog and PTH-related protein. Science 1996;273:613–622. [DOI] [PubMed] [Google Scholar]
- Simmonds CS, Kovacs CS. Role of parathyroid hormone (PTH) and PTH-related protein (PTHrP) in regulating mineral homeostasis during fetal development. Crit Rev Eukaryot Gene Expr 2010;20:235–273. [DOI] [PubMed] [Google Scholar]
- Cypess AM, Lehman S, Williams G, Tal I, Rodman D, Goldfine AB et al. Identification and Importance of Brown Adipose Tissue in Adult Humans. New Engl J Med 2009;360: p1509–1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bredella MA, Fazeli PK, Freedman LM, Calder G, Lee H, Rosen CJ et al. Young women with cold-activated brown adipose tissue have higher bone mineral density and lower Pref-1 than women without brown adipose tissue: a study in women with anorexia nervosa, women recovered from anorexia nervosa, and normal-weight women. J Clin Endocrinol Metab 2012;97:E584–E590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seale P, Conroe HM, Estall J, Kajimura S, Frontini A, Ishibashi J et al. Prdm16 determines the thermogenic program of subcutaneous white adipose tissue in mice. J Clin Invest 2011;121:96–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motyl KJ, Bishop KA, DeMambro VE, Bornstein SA, Le P, Kawai M et al. Altered thermogenesis and impaired bone remodeling in Misty mice. J Bone Miner Res 2013;28:1885–1897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen P, Levy JD, Zhang Y, Frontini A, Kolodin DP, Svensson KJ et al. Ablation of PRDM16 and beige adipose causes metabolic dysfunction and a subcutaneous to visceral fat switch. Cell 2014;156:304–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ybarra J, Donate T, Jurado J, Pou JM. Primary hyperparathyroidism, insulin resistance, and cardiovascular disease: a review. Nurs Clin North Am 2007;42:79–85 vii. [DOI] [PubMed] [Google Scholar]
- Ogata E. Parathyroid hormone-related protein as a potential target of therapy for cancer-associated morbidity. Cancer 2000;88:(12 Suppl): 2909–2911. [DOI] [PubMed] [Google Scholar]
- Sato K, Onuma E, Yocum RC, Ogata E. Treatment of malignancy-associated hypercalcemia and cachexia with humanized anti-parathyroid hormone-related protein antibody. Seminars in oncology 2003;30:(5 Suppl 16): 167–173. [DOI] [PubMed] [Google Scholar]
- Savoldi G, Izzi C, Signorelli M, Bondioni MP, Romani C, Lanzi G et al. Prenatal presentation and postnatal evolution of a patient with Jansen metaphyseal dysplasia with a novel missense mutation in PTH1R. Am J Med Genet A 2013;161A(10): 2614–2619. [DOI] [PubMed] [Google Scholar]
- Wei W, Dutchak PA, Wang X, Ding X, Wang X, Bookout AL et al. Fibroblast growth factor 21 promotes bone loss by potentiating the effects of peroxisome proliferator-activated receptor gamma. Proc Natl Acad Sci USA 2012;109:3143–3148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman S, Lu Y, Czernik PJ, Rosen CJ, Enerback S, Lecka-Czernik B. Inducible brown adipose tissue, or beige fat, is anabolic for the skeleton. Endocrinology 2013;154:2687–2701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanyu R, Wehbi VL, Hayata T, Moriya S, Feinstein TN, Ezura Y et al. Anabolic action of parathyroid hormone regulated by the beta2-adrenergic receptor. Proc Natl Acad Sci USA 2012;109:7433–7438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neuman WF, Neuman MW, Brommage R. Aerobic glycolysis in bone: lactate production and gradients in calvaria. Am J Physiol 1978;234:C41–C50. [DOI] [PubMed] [Google Scholar]