Abstract
This study examines the effects of different cigarette package warnings in Australia, Canada and the United Kingdom up to 5 years post-implementation. The data came from the International Tobacco Control Surveys. Measures included salience of warnings, cognitive responses, forgoing cigarettes and avoiding warnings. Although salience of the UK warnings was higher than the Australian and Canadian pictorial warnings, this did not lead to greater levels of cognitive reactions, forgoing or avoiding. There was no difference in ratings between the Australian and UK warnings for cognitive responses and forgoing, but the Canadian warnings were responded to more strongly. Avoidance of the Australian warnings was greater than to UK ones, but less than to the Canadian warnings. The impact of warnings declined over time in all three countries. Declines were comparable between Australia and the United Kingdom on all measures except avoiding, where Australia had a greater rate of decline; and for salience where the decline was slower in Canada. Having two rotating sets of warnings does not appear to reduce wear-out over a single set of warnings. Warning size may be more important than warning type in preventing wear-out, although both probably contribute interactively.
Introduction
Health warnings on tobacco packages are a simple and cost-effective means to increase awareness of the health effects of smoking and to reduce tobacco use, as recognized in the World Health Organization (WHO) Article 11 Guidelines (packaging and labelling of tobacco products) of the Framework Convention on Tobacco Control (FCTC) [1]. WHO has urged governments to require that all tobacco packages include effective pictorial warnings to warn people about the health effects of tobacco use. However, only about 40% of the world’s population is covered by the 63 countries/jurisdictions that have implemented pictorial warning regulations [2].
Strong health warnings on tobacco packaging is only one of a number of interventions designed to discourage smoking and encourage cessation. Of itself, effects on major outcomes like smoking cessation are likely to be small and difficult to identify independent of other interacting effects. The approach that is now recommended to establish evidence of a contributory role is to use meditational models where proximal responses to warnings are prospectively linked to increases in outcomes of interest [3]. It is now well established that the introduction of larger and stronger pack warnings leads to greater levels of awareness/noticing and immediate impact (e.g. increased motivational/cognitive responses and microbehavioural responses such as forgoing cigarettes and avoiding the warnings) [4–11]. Furthermore, these reactions to warnings, all are prospectively associated with increased levels of quit attempts, with this effect seemingly mediated through both levels of cognitive reactions and forgoing of cigarettes [12–14].
There are many factors that can contribute to the effectiveness of tobacco pack warnings. Such factors include, but are not limited to, warning size, positioning, format, message contents, novelty, background colour and design [4, 5, 11, 14–17]. Integrating pack warnings with other tobacco control measures, such as mass media campaigns and cessation services, may help increase the effectiveness of pack warnings [9, 18, 19].
The impact of warnings starts to decline around 1 year post-implementation, but some effects are sustained long-term. Using the first four waves of the ITC Four Country Survey (ITC-4) data (2002–2005), Hammond et al. [4] showed that, adjusting for time since implementation, the pictorial Canadian warnings elicited greater avoidance, cognitive responses and forgoing than the UK text-based ones. Borland et al. [12] extended the work by adding one more wave of data (i.e. Wave 5), and found that controlling for date of introduction, new pictorial Australian warnings also stimulated more cognitive responses and avoidant behaviours than the UK text-only ones in the year following implementation. Borland et al. [5] also found partial wear-out of both Canadian and UK warnings, but the Canadian pictorial warnings appeared to have more sustained effects than the UK text-only warnings, especially for cognitive reaction and forgoing cigarettes. More recently, Hitchman et al. [20] investigated the effectiveness of pack warnings over 9 years in Canada and the United States and found that, although the Canadian pictorial warnings showed greater declines in cognitive and microbehavioural responses, they were significantly more effective than the US warnings (i.e. text-only warnings located on the side of the pack) throughout the study years (2002–2011).
The three countries included in this study (Australia, Canada and the United Kingdom) vary considerably in the pack warnings they mandate (for details see Table I and Borland et al. [12]) [5]. About 2 years prior to our first wave of data was collected, Canada introduced world-first pictorial warnings (December 2000, covering 50% of the top of both main faces of a cigarette pack) [6, 21]; since then, the International Tobacco Control (ITC) surveys have collected eight waves of data in these three countries. During our data collection period (late 2002–early 2012), the United Kingdom introduced new, larger, text-based pack warnings in January 2003, increasing the size from 6% on both main faces of the pack to around 40% on the front (at least 30% of the external area plus a black boundary, placed at the bottom of the front pack face; 40% plus black boundary on the back); the United Kingdom subsequently implemented pictorial warnings from October 2008 [22, 23]. In March 2006, Australia introduced pictorial warnings, covering 30% of the front and 90% of the back, rotating two sets of seven warnings (Series A and B), which were rotated every 12 months [24]. Series A warnings were mandated to appear on all tobacco products for retail sale in Australia from 1 March 2006, meaning that in 2007 there was a completely new set of warnings (Series B) on tobacco products. Part of the rationale for this was to reduce warning wear out [24].
Table I.
Pack warning descriptions, comparable survey waves/years and sample size in studied countries
| Canada | UK | Australia | |
|---|---|---|---|
| Warnings studied | 2000 pictorial warnings | 2003 text warnings | 2006 pictorial warnings |
| Implementation date | Dec 2000 | Jan 2003 | Mar 2006 |
| Pack coverage | 50% front/50% back | At least 30% front/ 40% back surrounded by a border of 3–4 mm (40%+ in total) | 30% front/90% back |
| Other details | 16 pictorial/text warnings | Used one of two general warnings on the front, and one of 14 more specific warnings on the reverse, with all of the warnings being used regularly | Rotated two sets of seven warnings every 12 months |
| ITC-4 Survey Wave 1 data collection: Sep–Dec 2002 | Year 2 of implementationa | — | — |
| (22–24 months) | |||
| (number of current smokers n = 2189) | |||
| Wave 2: May–Sep 2003 | Year 3 | Year 1of implementation | — |
| (27–33 months) | (4–8 months) | ||
| (n = 2003) | (n = 1929) | ||
| Wave 3: Jun–Dec 2004 | Year 4 | Year 2 | — |
| (40–48 months) | (18–23 months) | ||
| (n = 1889) | (n = 1839) | ||
| Wave 4: Sept–Dec 2005 | Year 5 | Year 3 | — |
| (58–61 months) | (33–36 months) | ||
| (n = 1774) | (n = 1738) | ||
| Wave 5: Oct 2006–Feb 2007 | — | Year 4 | Year 1 of implementation |
| (46–48 months) | (7–11 months) | ||
| (n = 1706) | (n = 1801) | ||
| Wave 6: Sep 2007–Feb 2008 | — | Year 5 | Year 2 |
| (56–61 months) | (18–23 months) | ||
| (n = 1643) | (n = 1791) | ||
| Wave 7: Oct 2008–Jul 2009 | — | — | Year 3 |
| (31–36 months) | |||
| (n = 1372) | |||
| Wave 8: Jul 2010–May 2011 | — | — | Year 4 |
| (52–62 months) | |||
| (n = 1111) | |||
| Wave 8.5 (Australia only): Sep 2011–Feb 2012 | — | — | Year 5 |
| (66–70 months) | |||
| (n = 1104) |
aApproximate number of years from the time warnings were first introduced in a specific country to the time when an ITC-4 survey wave was conducted. More detailed information (number of months since warning introduction, and number of current smokers at each selected wave) is provided for each country in the brackets. For the purpose of this article, up to 5 years (or a bit longer in Australia) of implementation is indicated in the table (and based on this, indepth cross-country comparisons were conducted; See Tables II and III.).
To date no study has systematically explored differential decay of effects of warnings over the early years post-implementation and how this might vary by warning regimen. In particular, we were interested to see if the Australian strategy of rotating two sets of warnings every 12 months reduced wear out. This study explored wear-out effects of the 2006 Australian pictorial pack warnings in comparison to the 2003 United Kingdom slightly larger front of pack text warnings (replaced in 2008), and the even larger Canadian warnings.
Methods
Data source and participants
The data for this study came from the ITC-4 Survey, which has been running nearly annually since 2002 in Australia, Canada, the United Kingdom, and the United States (Note: this study did not include the United States which has had the same small text-based warnings since 1984). A detailed description of the conceptual framework and methods of the ITC-4 Survey has been reported by Fong et al. [25] and Thompson et al. [26], and more detail is available at http://www.itcproject.org. Briefly, the ITC-4 Survey employs a prospective multicountry cohort design and involves telephone surveys of representative cohorts of adult smokers in each country using random-digit dialling. The sample size per country was initially around 2000 at each survey wave, with replenishment sampling from the same sampling frame used to maintain sample size across waves (with a slightly reduced sample from Wave 7, mainly due to budget constraint). At the time of initial recruitment, participants were aged 18+ years, had smoked at least 100 cigarettes lifetime, and had smoked at least once in the past 30 days.
The analyses reported in this article are restricted to current smokers, as exsmokers have less opportunity to see cigarette packs. The number of smokers at each ITC-4 survey wave (up to Wave 8) and their characteristics were reported elsewhere [5, 27]. For this paper, the number of current smokers at each selected wave in each country was indicated in Table I [in the brackets, e.g. ‘(n = 2189)’ at Wave 1 for Canada]. Data collection dates for each ITC-4 survey wave together with warning implementation time in each studied country are also presented in Table I. For Australia, an additional Wave (Australia only wave—Wave 8.5, collected between September 2011 and February 2012) was also used. (Note: This article did not evaluate the effect of Australia’s standardized plain packaging which was only introduced on 1 December 2012). For the purpose of this article, indepth cross-country comparisons were conducted for data collected up to 5–6 years after the implementation of studied warning labels in each respective country.
Measures
Salience of warning
At each survey wave, salience of the health warnings was assessed by asking how often, over the preceding month, respondents had (1) noticed the warnings, and (2) read/looked closely at them (both on five-point scales: ‘never’ to ‘very often’); and based on respondents’ answers to these two questions, a combined salience measure was computed (range = 1–5, Cronbach’s α = 0.79–0.83, across waves).
Cognitive response
From Wave 2, the respondents were asked about cognitive responses in terms of the extent to which the warnings (i) made them think about the health risks of smoking and (ii) made them more likely to quit smoking (on four-point scales: ‘not at all’ to ‘a lot’); and respondents were also asked if ‘warning labels on cigarette packages’ motivated them to think about quitting in the past 6 months (with three response options: ‘not at all’, ‘somewhat’, and ‘very much’), combined into a cognitive response scale based on respondents’ answers to these three questions (range = 1.00–3.67, Cronbach’s α = 0.76–0.81, across waves).
Microbehavioural responses
Respondents were also asked about two mircobehavioural reactions: frequency (if ever) of forgoing cigarettes as a result of the warnings (with four response options: ‘never’, ‘once’, ‘a few times’ and ‘many times’) and about four ways of avoiding the warnings (cover-up, keep out of sight, use cigarette case or avoid particular labels) from which a binary variable, ‘no avoidance’–‘any avoidance’, was computed across all the selected waves (note: from Wave 6 to Wave 8 there was only one single question for this (avoiding labels in any way—yes/no), instead of having four separate questions).
Covariates (control variables)
Self-efficacy to quit was assessed at each wave by asking: ‘If you decided to give up smoking completely in the next 6 months, how sure are you that you would succeed?’ (‘not at all sure’, ‘slightly sure’, ‘moderately sure’, ‘very sure’ and ‘extremely sure’). Because of small numbers in some categories, both the first two options and last two were combined, resulting in a three-category variable.) Cigarettes per day (CPD) was asked at each wave and recoded as ‘1–10 CPD’, ‘11–20 CPD’, ‘21–30 CPD’ and ‘30 + CPD’. We also included one measure of expressed intention to quit at each wave (‘not planning to quit’, ‘sometime in the future beyond 6 months’, ‘within the next 6 months’ and ‘within the next month’). Socio-demographics included sex (male, female), age (18–24, 25–39, 40–54, 55 and older), identified ethnic minority status (nonminority versus minority group), highest level of education attained (low, moderate or high), and annual household income (low, moderate, high or not disclosed). Education and income were adjusted according to the norms within each country [28]. A time-in-sample variable was computed based on the number of survey waves a participant completed.
Data analysis
For the purpose of cross-country comparison, the data was re-aligned around the target warning implementation dates, so that the analyses only included the first and subsequent survey assessments (up to 5 years) after the target warnings were implemented. The target warning implementation dates are presented in Table I along with the range for the number of months from these dates in which surveying took place in each country. We used data from Waves 1–4 for Canada (22–61 months post-implementation), Waves 2–6 for the United Kingdom (4–61 months) and Waves 5 to 8.5 for Australia (7–70 months); with UK data from Wave 2 re-aligned with Australian data from Wave 5 (within 1 year after new warning introduction); UK data from Wave 3 were re-aligned with Australian data at Wave 6 and Canadian data from Wave 1 (about 2 years since implementation), and so forth. Thus, we effectively covered the period from shortly after implementation to around 5–6 years post-implementation for cross-country comparisons except for Canada which began from around 2 years post-implementation. Weighted data were used when the percentages/means of the key warning response measures were calculated to better reflect the underlying population by controlling for age and gender prevalence estimates within geographic strata, as well as to account for nonresponse and the survey design.
To account for the correlated nature of the data from participants present in multiple survey waves, Generalized Estimating Equations (GEE) models were employed to compute parameter estimates and compare country/group differences. For the binary dependent variable (i.e. avoidance), logit link function and binomial family distribution were specified for the GEE models while for continuous dependent variables (i.e. warning salience, cognitive response and forgoing cigarettes), identity link function and Gaussian family distribution were specified. An unstructured correlation matrix was employed to account for the within subjects clustering for all GEE models. On the basis of the date that the target warning labels were introduced in a country and the date when a participant was interviewed at a particular post-warning-introduction survey wave, we computed a warning implementation length variable for all studied countries (i.e. ‘time after warning introduction’ variable, with years as the time unit). We then used GEE modelling to examine its relationship with the key response measures, controlling for sociodemographics (treated as time-invariant), time-in-sample and CPD, intention to quit and self-efficacy to quit (these smoking characteristics were treated as time varying).
Indepth cross-country comparisons (using GEE modelling) were first conducted between the United Kingdom and Australia, where up to 5 waves/years of postimplementation data were available for both countries. This step included up to 3863 unique individuals providing up to 8490 observations. We then used data for those post-implementation waves/years when all three countries had available data (from the second through fifth year after the target warnings were introduced, except for the cognitive response measure where only years 3–5 data were available for Canada) for our GEE analyses. This second step included up to 5558 unique individuals providing up to 11 262 observations. Tests of differential wear-out effects for key warning measures in our GEE analyses were examined using country by time interactions. If there was no significant country by time interaction, a combined model was used for all countries. Otherwise separate models were used for each country. All analyses were conducted using Stata Version 12.1.
Ethics approval
The study protocol was approved by the institutional review boards or research ethics boards of the University of Waterloo (Canada), Roswell Park Cancer Institute (the US), University of Strathclyde (the UK), University of Stirling (UK), The Open University (UK) and Cancer Council Victoria (Australia).
Results
Salience of warnings
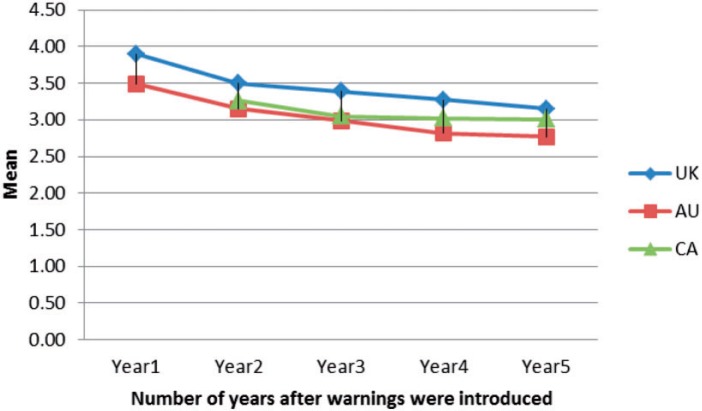
As seen in Fig. 1, reported salience of pack warnings in Australia and the United Kingdom was the highest at year 1 of implementation, and after that (from year 2 of implementing the target warnings) salience declined gradually over time. In GEE models pooling data for both the United Kingdom and Australia (Table II), there was a significant negative effect for time since implementation (i.e. years from warning introduction to survey date) when estimating the salience of warnings (P < 0.001). As time went by, smokers were generally less likely to report having noticed/read the warnings. Salience of the UK text-only warnings was consistently higher than the Australian pictorial warnings, with both declining at similar rates over time (there was no significant country and time interaction). When we restricted the analyses only to the post-implementation period when all three countries had available data (years 2–5, Table III), results indicate that there were significant country and time interactions for salience. The Canadian pictorial warnings, although also rated less salient than the UK warnings, had these ratings declined more slowly over the latter period (Table III; Fig. 1).
Fig. 1.
Salience of warning labels, aligned.
Notes: Weighted data were used. ‘Year1’ means the first survey wave/year after the new warnings were implemented. This applies to other years, all three countries and other response measures. ‘Mean’: ranges from 1 to 5, by averaging the responses to ‘having noticed the warnings’ and ‘having read/looked closed at them’.
Table II.
Association between warning implementation length and smokers’ responses to warnings—GEE modelling results for UK and Australia, Years 1–5, with 8490 observations from 3863 individualsa
| UK | Australia | Two countries combined | Notes on interactions | |
|---|---|---|---|---|
| Salience of warnings | ||||
| Time (years) after warning introductionc Beta coef. (β) (95% CI)b | — | — | −0.16 (−0.18 to −0.15)*** | No country*time interactiond |
| Country (Au versus UK) β (95% CI) | — | — | −0.39 (−0.47 to −0.30)!*** | |
| Cognitive response | ||||
| Time after warning introduction β (95% CI) | — | — | −0.05 (−.06 to 0.04)*** | No country*time interaction |
| Country (Au versus UK) β (95% CI) | — | — | 0.03 (−0.02 to 0.09) | |
| Forgoing cigarettes | ||||
| Time after warning introduction β (95% CI) | — | — | −0.02 (−0.03 to −0.01)*** | No country*time interaction |
| Country (Au versus UK) β (95% CI) | — | — | 0.01 (−0.04 to 0.06) | |
| Avoiding warnings (UK: 6026 observations from 2815 individuals; Australia: 2435 observations from 1041 individuals) | ||||
| Time after warning introduction OR (95% CI)b | 0.83 (0.79 to 0.87)*** | 0.75 (0.71 to 0.79)*** | — | With country*time interaction (P < 0.05) |
| Country (Au versus UK) OR (95% CI) | Reference | 2.05 (1.60–2.63)*** | — | |
aFor some analyses, the numbers of cases are fewer than the total, especially when separate models are generated for each country.
bOR: odds ratio. OR value is reported for avoiding outcome (dichotomous); β value is reported for other outcomes (as continuous variables). All ORs/β were adjusted for socio-demographics (sex, age, ethnicity, education, income), time-in-sample, self-efficacy and intention to quit, and cigarettes per day. Significant at *P < 0.05; **P < 0.01; ***P < 0.001.
cWe used year (i.e. 365 days) of implementation as a time unit.
dIf there is no significant country*time interaction, a combined model is used for both countries. Otherwise separate models are used for each country. This applies to other responses in the table.!Country main effect; UK’s value as the reference.
Table III.
Association between warning implementation length and smokers’ responses to warnings—GEE modelling results for all three countries (restricted to implementation years when all countries had available data: from 2 to 5 years of warning implementationa) (11 262 observations from 5558 individualsb)
| Canada | UK | Australia | Three countries combined | Notes on interactions | |
|---|---|---|---|---|---|
| Salience of warnings (Canada: 5014 observations from 2443 individuals; UK: 4406 observations from 2232 individuals; Australia: 1817 observations from 878 individuals) | |||||
| Time (years) after warning introductiond β (95% CI)c | −0.06 (−0.09 to −0.04)*** | −0.11 (−0.14 to −0.09)*** | −0.14 (−0.16 to −0.11)*** | — | With country*time interaction (P < 0.001)e |
| Country β (95% CI) | Reference | 0.43 (0.30 to 0.56)!*** | 0.10 (−0.06 to 0.26) | — | |
| Cognitive response (Canada: 3558 observations from 1490 individuals; UK: 3221 observations from 1855 individuals; Australia: 1311 observations from 735 individuals) | |||||
| Time after warning introduction β (95% CI) | 0.01 (−0.01 to −0.03) | −0.09 (−0.11 to −0.06)*** | −0.02 (−0.04 to 0.003) | — | With country*time interaction (P < 0.001) |
| Country β (95% CI) | Reference | −0.10 (−0.14 to −0.06)*** | −0.13 (−0.19 to −0.07)*** | — | |
| Forgoing cigarettes | |||||
| Time after warning introduction β (95% CI) | — | — | — | −0.02 (−0.03 to −0.01)*** | No country*time interaction |
| Country β (95% CI) (UK versus Canada) (Australia versus Canada) | — | — | — | −0.06 (−0.09 to 0.02)** | |
| −0.004 (−0.05 to −0.04) | |||||
| Avoiding warnings | |||||
| Time after warning introduction OR (95% CI)c | — | — | — | 0.84 (0.81–0.87)*** | No country*time interaction |
| Country OR (95% CI) (UK versus Canada) (Australia versus Canada) | — | — | — | 0.45 (0.39–0.51)*** | |
| 0.60 (0.50–0.73)*** | |||||
aExcept for cognitive responses where only implementation years 3–5 data was available for all three countries.
bFor some analyses the numbers of cases are fewer than the total, especially when separate models are generated for each country.
cOR: odds ratio. OR value is reported for avoiding outcome (dichotomous); β value is reported for other outcomes (as continuous variables). All ORs/β were adjusted for socio-demographics, time-in-sample, and the smoking related variables. Significant at *P < 0.05; **P < 0.01; ***P < 0.001.
dWe used year (i.e. 365 days) of implementation as a time unit.
eIf there is no significant country*time interaction, a combined model is used for all countries. Otherwise separate models are used for each country. This applies to other outcomes in the table.!Country main effect; Canada’s value as the reference.
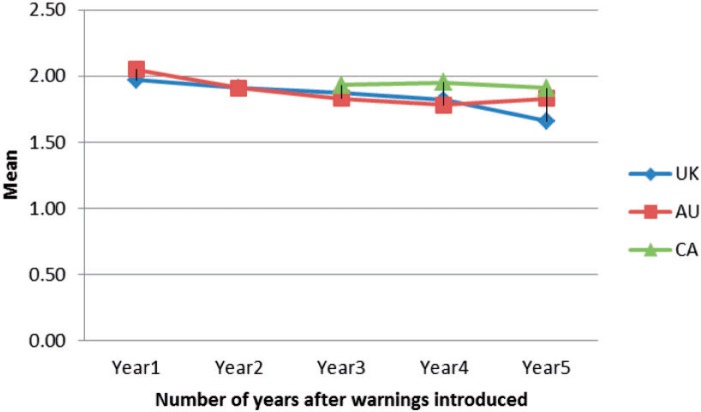
Cognitive responses
For cognitive responses, there were no significant differences in ratings between the Australian and UK warnings, or in the rates of decline (both with significant declines, Table II; Fig. 2). In the latter period (between years 3–5 post-warming implementation), the Canadian warnings were responded to more strongly and there was only evidence of a significant decline in reactions for the UK text warnings (Table III).
Fig. 2.
Cognitive response, aligned.
Notes: This question was only asked from Wave 2 of the ITC-4 Survey (in 2003), and it was the third year of pictorial warning implementation in Canada. ‘Mean’: ranges from 1.00 to 3.67, by averaging the responses to ‘the warnings made the respondent think about the risks of smoking’, ‘be more likely to quit’ and ‘be motivated to think about quitting’.
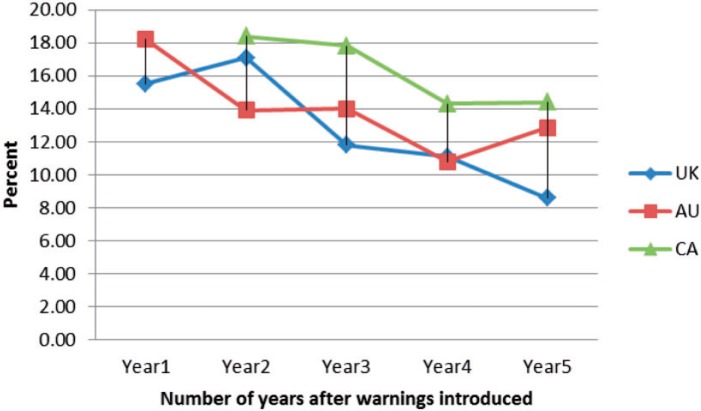
Forgoing cigarettes
For forgoing, there was no overall difference between the United Kingdom and Australian warnings, with similar rates of decline (Table II; Fig. 3). However, in the period 2–5 years post-implementation, the Canadian warnings were responded to with greater forgoing than the UK ones (P < 0.01), with response levels in all three countries declining at similar rates (Table III).
Fig. 3.
Forgoing cigarettes, aligned.
Notes: Percentages are the proportion reporting positive responses, i.e. ‘% that had forgone cigarettes at least once over the preceding month’.
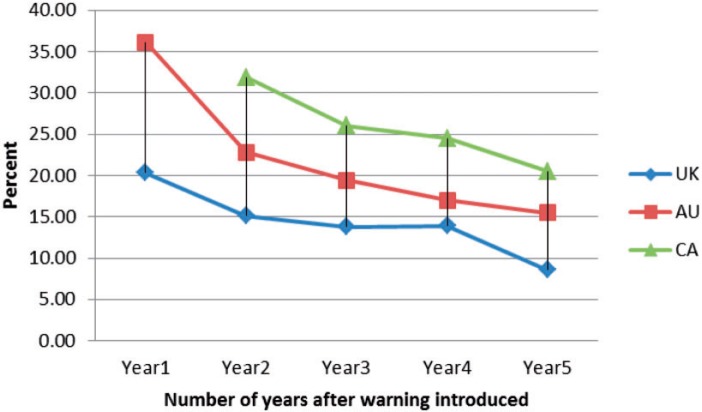
Avoidance of warnings
There was a statistically significant interaction between country and time in the GEE model pooling data for the United Kingdom and Australia (Table II). Compared with smokers in the United Kingdom, Australian smokers had a significantly larger decline in avoidance over time (from a much higher level at Year 1 of implementation) (OR = 0.75 in Australia versus OR = 0.83 in the United Kingdom), although they consistently reported higher levels of avoiding behaviours than their United Kingdom counterparts (OR = 2.05, Table II; also see Fig. 4). In the later period, the Canadian warnings were avoided even more, but avoidance declined similarly by country (Table III).
Fig. 4.
Avoiding warnings, aligned.
Notes: Percentages are the proportion reporting positive responses, i.e. ‘% that used at least one strategy to avoid warning labels’.
Discussion
This study confirms that the impact of pack warning labels declines over time after implementation [4, 5, 20]. When considering the period up to 5 years post-implementation, declines were comparable across the three countries for most measures; with no evidence of an expected slower decline in Australia. Specifically, the declines were comparable between Australia and the United Kingdom on all measures except avoiding warnings, where Australia had a greater decline but from a much higher initial level, and a similar pattern emerged for the follow-up period of 2–5 years for Canada, except for salience where it declined at a lower rate between 2 and 5 years post-implementation. It should be remembered that the overall reactions to the Australian warnings were greater than the United Kingdom ones on avoiding, but were inferior to the Canadian warnings on avoiding and cognitive reactions. The text-only UK warnings were superior to the other two countries on reported salience.
In interpreting the results, we need to consider the differences across countries in the size, design, nature of the health warning messages and how the measures we assessed relate to making quit attempts. As we have shown elsewhere [5, 13], salience has its impact on quitting mediated primarily through cognitive reactions and to a lesser extent forgoing cigarettes and avoidance. In the United Kingdom, it is plausible that the old pack warnings (prior to 2003) were almost invisible (only 6% of the pack on the front with the previous warnings); therefore the change in warnings from pre- to post-implementation was much greater in the United Kingdom than in Canada and Australia (which changed from large, high contrast text only to large pictorial warnings). The higher salience of the UK text-only warnings, compared with the Australian or Canadian warnings, also suggests that the stark contrast of the black and white warnings with the cigarette package may be more eye-catching. Text warnings need to be read to be processed. However, this has not led to greater levels of cognitive reactions or to other responses more proximally related to quitting in the UK compared with Canada or Australia. This suggests that the text-only warnings work in slightly different ways to the pictorial ones by relying more on being noticed and then read to be considered salient, while pictorial warnings can have effects without being consciously processed via the emotion-generating capacity of pictures.
The most surprising result was the failure to find any evidence that rotating two sets of warnings annually (as was done in Australia) reduces the speed of wear-out. Two main purposes of warnings are to inform the public about health risks from tobacco use and encourage quitting. Rotating warnings allows for more health effects to be communicated, but it would appear that this does not result in any overall increase in warning effectiveness, or in a reduction in wear-out. Possible explanations for the failure to find a positive effect on wear-out include it being the overall impression of the warning format that leads to a re-engagement with the warning label such as marked changes in size, position on the pack or background colours. These might be more important for gaining attention than changes in content within the same basic frame. Second, it could be that the smokers had not become familiar enough with the first set of warnings to really notice that they were being replaced. If this second explanation was the case, then rotating on a longer schedule might lead to some recovery. A final possibility is that the measures we used have missed some important aspect of warning impact, but apart from warning-specific knowledge, we can think of nothing. In thinking about how warnings impact on smokers, it is important to realise that most of the time, smokers do not look at or think about the warnings; therefore, marked changes in elements of the warnings may be required to reactivate their orienting reactions to the novelty in the warnings.
The study also has implications for assessing the relative contributions of size and pictorial aspects of packs. Consider the implications for cognitive reactions and forgoing, the two main influences on quitting [12, 13]. In this study, cognitive reactions and forgoing were equivalent for the approximately 40% sized (of the front of the pack) text-only warnings in the United Kingdom and the 30% pictorial warnings in Australia, but both were inferior to the 50% pictorial warnings in Canada. This suggests pictorial and size both contributed to the more important impacts of warnings.
The Australian pictorial warnings were responded to more strongly than the UK ones only on avoidance. This is plausible as there is less reason to actively avoid text to avoid the message it conveys. However, as the likely positive effects of avoidance are mediated though other reactions, it is not evidence of a superiority of the pictorial Australian warnings to the UK text-only ones. It is notable that in addition to the size requirement, the United Kingdom specifically requires a border of 3–4 mm to help set the health warnings apart from the rest of the package (and Canada also does this to some extent). This may have contributed to the better than expected performance of the UK text-only warnings. Research on the impact of a strong border on the extent to which warnings are attended to and processed is needed. A further possible reason for the failure to find increased superiority of the Australian warnings is that there was a strong campaign of anti-smoking television ads, most of which have pictorial elements, running concurrent to the time of data collection in Australia. These ads may play a significant role in the perceptions of the messages in the warnings, with the pack warnings considered as extended images of TV ads, leading to their effects being attributed to TV rather than to the tobacco pack warning labels. However, this explanation does not explain the lack of difference between the United Kingdom and Australian warnings in forgoing cigarettes.
One of the main strengths of this study is its prospective multi-country cohort design, which allowed for changes in levels of warning salience, cognitive responses and microbehavioural responses to be assessed over time and across countries. However, because country and warning are confounded means that caution must be taken in interpreting the results. Given that, the findings of similar levels of some reactions and differential reactions to others, precludes explanations such that smokers in one country are more sensitive or more prone to use extreme categories. It requires an explanation that accounts for the pattern found, and features of the warning regimen provide the only plausible explanation we can think of. Given that no country has transitioned from pictorial to text-only warnings we are unable to test the differential effects fully.
Ideally, other possible factors such as public education, price, advocacy levels and media coverage also need to be considered. In our analysis these measures (which are not proximal reactions to health warnings) have not been included. This is a limitation. We have considered the possibility that the pattern of differences is due to such factors, the most plausible being other public education efforts, e.g., anti-smoking advertisements and information on television which work in a similar way to health warnings [29, 30] and can complement warnings [19], but can think of no way these could account for all the main results, except perhaps for the lack of avoidance effect mentioned earlier. In all three countries levels of reporting seeing material were high (unpublished ITC data), and there were no marked differences between or within countries that corresponded to the changes we report here, but as we have no information on the content or precise timing of material, cannot absolutely rule out any effects.
In summary, the findings of this study indicate that while the impact of pack warning labels does decline in the years after implementation, and we found no evidence of any benefits of an annual rotation system like that used in Australia on reducing decay in quit-related reactions to warnings. The data is suggestive that warning size may be more important than warning type (pictorial versus text only) in reducing wear-out, but it remains likely that both play an interactive role. From a policy viewpoint, the results clearly show superiority of the Canadian warnings, and we can think of no by-country effect that could have contributed to this other than the differences in the specific warnings used. It is also important to remember that other studies have shown residual positive effects of the weak US warning decades after their implementation [12, 20], so what we are talking about here is a reduction in effects, not their elimination. It will be of considerable interest to evaluate the impact of the even stronger warnings that have been introduced in Australia and Canada (as well as other places) to see if there are limits to the value of increasing warning size.
Acknowledgements
The authors thank other members of the ITC Four Country Survey team for their support. Supported by a Public Policy Network Travel Award from the Society for Research on Nicotine and Tobacco (SRNT), the lead author (Dr. Lin Li) presented some of the results and received valuable feedback at the 2014 SRNT Annual Conference in Seattle in February 2014. We are grateful to the anonymous reviewers and editors who provided useful suggestions on earlier drafts of this article.
Funding
National Cancer Institute at the National Institutes of Health of the United States (grant numbers P50 CA111326, P01 CA138389, and R01 CA100362); Robert Wood Johnson Foundation (045734); Canadian Institutes of Health Research (57897, 79551 and 115016); National Health and Medical Research Council of Australia (265903 and 450110); Cancer Research UK (C312/A3726); Canadian Tobacco Control Research Initiative (014578); and the Ontario Institute for Cancer Research, with additional support from the Propel Centre for Population Health Impact, Canadian Cancer Society, and a Prevention Scientist Award from the Canadian Cancer Society Research Institute.
Conflict of interest statement
None declared.
References
- 1.World Health Organization. Guidelines for implementation of Article 11 of the WHO Framework Convention on Tobacco Control (Packaging and labelling of tobacco products). 2008. Available at: http://www.who.int/fctc/guidelines/article_11.pdf. Accessed: 26 June 2013. [Google Scholar]
- 2.Canadian Cancer Society. Cigarette Package Health Warnings: International Status Report. 3rd. ed., October 2012. Available at: http://www.ensp.org/node/817. Accessed: 17 June 2013. [Google Scholar]
- 3.International Agency for Research on Cancer. IARC Handbooks of Cancer Prevention: Tobacco Control. vol. 12. Lyon: Methods for Evaluating Tobacco Control Policies, 2008. [Google Scholar]
- 4.Hammond D, Fong GT, Borland R, et al. Text and graphic warnings on cigarette packages: Findings from the International Tobacco Control Four Country Study. Am J Prev Med. 2007;32:202–9. doi: 10.1016/j.amepre.2006.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Borland R, Wilson N, Fong GT, et al. Impact of graphic and text warnings on cigarette packs: findings from four countries over five years. Tob Control. 2009;18:358–64. doi: 10.1136/tc.2008.028043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Canadian Cancer Society. Media Backgrounder - Evaluation of new warnings on cigarette packages. 2002. Available at: http://www.ash.org.uk/files/documents/ASH_602.pdf. Accessed: 27 June 2013. [Google Scholar]
- 7.O'Hegarty M, Pederson L, Nelson D, et al. Reactions of young adult smokers to warning labels on cigarette packages. Am J Prev Med. 2006;30:467–73. doi: 10.1016/j.amepre.2006.01.018. [DOI] [PubMed] [Google Scholar]
- 8.Hammond D, Fong GT, McNeill A, et al. Effectiveness of cigarette warning labels in informing smokers about the risks of smoking: findings from the International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006;15(Suppl. 3):iii19–25. doi: 10.1136/tc.2005.012294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hammond D. Health warning messages on tobacco products: a review. Tob Control. 2011;20:327–37. doi: 10.1136/tc.2010.037630. [DOI] [PubMed] [Google Scholar]
- 10.Yong H-H, Fong GT, Driezen P, et al. Adult Smokers’ Reactions to Pictorial Health Warning Labels on Cigarette Packs in Thailand and Moderating Effects of Type of Cigarette Smoked: Findings From the International Tobacco Control Southeast Asia Survey. Nic Tob Res. 2013;15:1339–47. doi: 10.1093/ntr/nts241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fong GT, Hammond D, Hitchman SC. The impact of pictures on the effectiveness of tobacco warnings. Bull World Health Organ. 2009;87:640e3. doi: 10.2471/BLT.09.069575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Borland R, Yong H, Wilson N, et al. How reactions to cigarette pack health warnings influence quitting: findings from the ITC Four Country survey. Addiction. 2009;104:669–75. doi: 10.1111/j.1360-0443.2009.02508.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yong HH, Borland R, Thrasher J, et al. Mediational pathways of the impact of cigarette warning labels on quit attempts in four countries. An application of the International Tobacco Control (ITC) Conceptual Model. Health Psychol. in press doi: 10.1037/hea0000056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fathelrahman A, Li L, Borland R, et al. Stronger pack warnings predict quitting more than weaker ones: findings from the ITC Malaysia and Thailand surveys. Tob Induc Dis. 2013;11:20. doi: 10.1186/1617-9625-11-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Strahan EJ, Fabrigar LR, Fong GT, et al. Enhancing the effectiveness of message labels on tobacco packaging: a social psychological perspective. Tob Control. 2002;11:183–90. doi: 10.1136/tc.11.3.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Corporate Research Associates. Creative Concept Testing for Health Warning Messages. Prepared for Health Canada. 2005. http://www.tobaccolabels.ca/healt/canada2005. Accessed: 14 October 2013. [Google Scholar]
- 17.De Wit JB, Das E, Vet R. What works best: objective statistics or a personal testimonial? An assessment of the persuasive effects of different types of message evidence on risk perception. Health Psychol. 2008;27:110e15. doi: 10.1037/0278-6133.27.1.110. [DOI] [PubMed] [Google Scholar]
- 18.Willemsen MC, Simons C, Zeeman G. Impact of the new EU health warnings on the Dutch quit line. Tob Control. 2002;11:382. doi: 10.1136/tc.11.4.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brennan E, Durkin S, Cotter T, et al. A Mass media campaigns designed to support new pictorial health warnings on cigarette packets: evidence of a complementary relationship. Tob Control. 2011;20:412–18. doi: 10.1136/tc.2010.039321. [DOI] [PubMed] [Google Scholar]
- 20.Hitchman S, Driezen P, Logel C, et al. Changes in effectiveness of cigarette health warnings over time in Canada and the United States, 2002-2011. Nic Tob Res. 2014;16:536–43. doi: 10.1093/ntr/ntt196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hammond D, Fong G, McDonald P, et al. Graphic Canadian cigarette warning labels and adverse outcomes: evidence from Canadian smokers. Am J Public Health. 2004;94:1442–5. doi: 10.2105/ajph.94.8.1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. The National Archives (UK). The Tobacco Products (Manufacture, Presentation and Sale) (Safety) Regulations 2002, SI 3041/2002. Available at: http://www.legislation.gov.uk/uksi/2002/3041/contents/made. Accessed 14 June 2013.
- 23. The National Archives (UK). The Tobacco Products (Manufacture, Presentation and Sale) (Safety) (Amendment) Regulations 2007, SI 2473/2007. Available at: http://www.legislation.gov.uk/uksi/2007/2473/contents/made. Accessed: 7 June 2013.
- 24. Australian Government. Trade Practices (Consumer Product Information Standards) (Tobacco) Regulations 2004. Commonwealth of Australia Statutory Rules 2004 No. 264. http://www.comlaw.gov.au/ComLaw/Legislation/LegislativeInstrumentCompilation1.nsf/all/search/0AE4DEC91A2D84E3CA2572870013926E. Accessed: 2 July 2013.
- 25.Fong GT, Cummings KM, Borland R, et al. The conceptual framework of the International Tobacco Control (ITC) Policy Evaluation Project. Tob Control. 2006;15(Suppl. 3):iii3–11. doi: 10.1136/tc.2005.015438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thompson ME, Fong GT, Hammond D, et al. Methods of the International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006;15(Suppl 3):iii12–8. doi: 10.1136/tc.2005.013870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li L, Borland R, Fong GT, et al. Impact of point-of-sale tobacco display bans: findings from the International Tobacco Control Four Country Survey. Health Educ Res. 2013;28:898–910. doi: 10.1093/her/cyt058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li L, Borland R, Hua Yong, et al. The association between exposure to point-of-sale anti-smoking warnings and smokers’ interest in quitting and quit attempts: findings from the International Tobacco Control Four Country Survey. Addiction. 2012;107:425–33. doi: 10.1111/j.1360-0443.2011.03668.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Borland R, Balmford J. Understanding how mass media campaigns impact on smokers. Tob Control. 2003;12(Suppl. II):ii45–ii52. doi: 10.1136/tc.12.suppl_2.ii45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wakefield M, Spittal M, Durkin S, et al. Effects of mass media campaign exposure intensity and durability on quit attempts in a population-based cohort study. Health Educ Res. 2011;26:988–97. doi: 10.1093/her/cyr054. [DOI] [PMC free article] [PubMed] [Google Scholar]