Abstract
This study aims to explore how media use for health information and interpersonal health communication interact in the context of healthy lifestyle behaviors. This study hypothesizes that media use for health information and interpersonal health communication will serve as substitutes for one another. To test this hypothesis, this study uses a nationally representative survey of 2,107 civilian, noninstitutionalized adults in the United States. The results show that the associations between television use and Internet use and healthy lifestyle behaviors are enhanced among those who talk about health issues with their family and friends less frequently, which supports the substitution model. The implications that these findings have for future research are discussed.
Mass media have increasingly focused on health-related lifestyle behaviors (e.g., exercise, diet, alcohol consumption, and smoking), partly because the focus of public health has undergone a rapid shift from disease treatment to disease prevention and to health promotion over the past decades (Labre & Walsh-Childers, 2003; Rimal, Flora, & Schooler, 1999; Viswanath, 2005). Recently, the Internet has emerged as a health-information provider (Pew Research Center, 2006). Scholars have documented that the increasing amount of information available through mass media and the Internet has the potential to promote individuals’ healthy behaviors (e.g., Stryker, 2003; Yanovitzky & Stryker, 2001).
Prior studies examining the beneficial effects of media use and interpersonal communication on health behaviors have focused on informational gains or normative pressures (Fishbein & Yzer, 2003; Yanovitzky & Stryker, 2001). Receiving health information from media channels and from significant others could lead one to engage in healthy lifestyle behaviors by boosting attitudes, social norms, and self-efficacy, on which these healthy behaviors are based. Also, as Berkman, Glass, Brissette, and Seeman (2000, p. 849) stated, “Shared norms around health behaviors might be powerful sources of social influence with direct consequences for the behaviors.” Given that social norms are established and disseminated mainly through communication activities (Rimal & Real, 2003), media coverage of health issues and interpersonal health communication with significant others may form and strengthen social norms related to healthy lifestyle behaviors.
However, previous studies in this area are limited in some respects. First, most studies have focused primarily on public health campaigns, while relatively ignoring the ordinary flow of health information in mass media and on the Internet (Brown & Walsh-Childers, 2002; Stryker, 2003; Yanovitzky & Stryker, 2001). The effects of media may be attributable to public health campaign messages, which are strategically produced and diffused within a specific period of time. At the same time, media effects on health behaviors can manifest themselves in a less strategic way, insofar as media’s coverage of health issues is a routine activity for journalists who describe or sometimes recommend behavioral practices. To fill in this gap, the current study focuses on media’s routine transmission of health information rather than on media health campaigns.
Second, many scholars in the communication area have contended that media use and interpersonal communication are in complementary or convergent relationships with one another (Chaffee, 1986; Hornik, 1989; Southwell & Torres, 2006). However, surprisingly little empirical research has been conducted on this topic. A handful of studies have addressed mainly the interactive effects of media exposure and interpersonal communication on cognitive outcomes, such as political candidate evaluation, issue salience, and memory (see Southwell & Yzer, 2007, and Valente & Saba, 1998, for excellent reviews). To our knowledge, only two studies (i.e., Hardy & Scheufele, 2005; Scheufele, 2002) went beyond cognition and tested the joint effects of media use and interpersonal communication on actual behavior. However, because theses studies focus only on political participation, their results cannot be generalized to other types of behavior, such as healthy lifestyle behaviors. More empirical evidence regarding other types of behavior is necessary.
Third, despite having established that interpersonal communication can mediate or moderate media effects, previous studies have not theorized about the conditions under which such relationships occur. Also, a variety of possible interaction patterns between interpersonal communication and media exposure have been suggested (Chaffee, 1986; Hornik, 1989). However, only a few studies (e.g., Southwell & Torres, 2006) have tried to reveal the underlying mechanisms through which media exposure about a particular topic is related to interpersonal talk about that topic. Without such theoretical efforts, one will be left with case studies that could report contrasting results. This clearly impedes the theoretical advancement in this area.
Directly addressing these issues, the current study first suggests some theoretical reasons to explain why we expect a specific pattern of interactive effects between media use and interpersonal communication on healthy lifestyle behaviors. Then, a U.S. nationally representative dataset provides an empirical test of this interaction.
Healthy Lifestyle Behaviors Index
Major causes of death in the United States, such as cardiovascular disease (CVD) and cancer, are associated with health-related lifestyle behaviors (e.g., exercise, diet, alcohol consumption, and smoking) (Barefoot et al., 2002; Blanchard et al., 2004). Thus, public health endeavors to reduce the prevalence of these major diseases have focused on modifying individuals’ unhealthy behaviors as well as on reinforcing their healthy lifestyle choices (Viswanath, 2005).
Most studies investigating the effects of media on health behaviors have “taken only a narrow focus, relying predominantly on a single health behavior in any analysis” (Rimal et al., 1999, p. 323). Certainly, this emphasis on specific health behaviors that is prevalent in the current health communication literature makes some sense, given that most public health campaigns deal with one or two specific health behaviors. Additionally, this narrow approach has been privileged because media use and interpersonal communication may have different effects on different health behaviors, effects which are more easily discernible with a focus on single behaviors.
In contrast to this granular focus on a few health behaviors, some researchers embrace an all-encompassing model and present a broader, less fine-grained overview of the media effects model for health behaviors (e.g., Berkman & Syme, 1979; Gottlieb & Green, 1984; Rimal et al., 1999). This group of scholars have argued that because major diseases are a function of multiple health behaviors and because health-threatening practices may offset healthy behaviors (i.e., even if an individual adopts one health-inducing behavior, he or she can eliminate this positive effect by continuing health-threatening behaviors), one should simultaneously examine diverse health behaviors—whether health-inducing or health-threatening—in assessing the effects of public health campaigns or mass media’s daily coverage of health issues.
Adopting the latter perspective, the current study constructs an index of healthy lifestyle behaviors that captures key health behaviors (i.e., smoking, binge drinking, exercise, fruit and vegetable consumption). Although this comprehensive index is sensitive to neither differential effects of media use nor interpersonal health communication across a variety of behaviors, the index can serve the practical need to evaluate the effects of health-information environments on individuals’ overall health behaviors.
The Relationship between Media Use and Interpersonal Communication
From the early days of communication research, scholars have suggested that interpersonal communication mediates the effects of media exposure on human behaviors, which produces the classic two-step flow model (Katz, 1987; Katz & Lazarsfeld, 1955) and its variants, such as the communication mediation model (Shah et al., 2007) and the inter/media processes (Rogers, 2003). These mediation models are based on the following roles of interpersonal communication: relaying media information to others (i.e., social diffusion; see Katz, 1987), providing opportunities for elaboration about media content before and during conversation (Eveland, 2004), and establishing and reinforcing social norms (Valente & Saba, 1998).
However, the present study views the relationship between media exposure and interpersonal communication according to an interaction model rather than to a mediation model and does so for the following reason. Health communication campaigns may come before the interpersonal communication concerning the topic addressed by the campaigns. Communication campaigns artificially and strategically increase public information flow about a certain topic, and this increased information may facilitate interpersonal interactions about the campaign itself or the topic of the campaign (Hornik et al., 2001; Southwell & Yzer, 2007). This is particularly true when the topic of the campaign is not something that is often thought about or frequently talked about in our daily lives (e.g., the HPV vaccine). In contrast, when it comes to the media’s routine relay of health issues, there are few compelling reasons to assume that media use should temporally precede interpersonal communication (Brosius & Weimann, 1996). This regular dissemination of health information by the media may occur at the same time as interpersonal communication about these health issues, or such interpersonal health communication could lead to related media use, rather than the reverse, because healthy lifestyle behaviors are a popular conversation topic. Therefore, the current study examines how media exposure and interpersonal communication interact and jointly influence healthy lifestyle behaviors.
How Media Use and Interpersonal Health Communication Interact
Before proposing the interaction hypothesis for the current study, it should be noted that two contrasting patterns have been proposed in past research with regard to the interaction between media exposure and interpersonal communication.
Many communication researchers have argued that interpersonal communication reinforces media effects: the influence of media information on individuals’ behaviors is expected to be larger if those individuals talk about the media content with others in their social networks. Two mechanisms for such reinforcement effects have been suggested. First, individuals may be better prepared to make sense of health information from media channels if they have a knowledge foundation as the result of having been exposed to relevant information from others (McDonald, 1990). Second, after individuals are exposed to health information from media, they can better understand and respond more fully to such media information by making use of their interpersonal communication networks (Eveland, 2001, 2004; Shah et al., 2007).
However, the opposite pattern has been also proposed: interpersonal communication and media exposure have substitution effects (Rogers, 2003; Valente & Saba, 1998). That is, health news from the media may reach individuals and persuade them to engage in healthy lifestyle behaviors to a greater degree when there is less exposure to similar information from interpersonal networks. This will be the case if media and interpersonal channels provide overlapping information.1 If similar information from both sources is provided, it is possible that the effect of each source becomes smaller than when exposed to complementary information (Kline, Miller, & Morrison, 1974). This can be explained by the concept of “information sufficiency” (Kahlor, Dunwoody, Griffin, Neuwirth, & Giese, 2003), which posits that “people will exert whatever effort is required to attain a ‘sufficient’ degree of confidence that they have accomplished their processing goals” (Eagly & Chaiken, 1993, p. 330). Because human beings are “cognitive misers” and because active information processing is partly determined by the gap between one’s desired level of information and current level of information, those who already receive enough health information from their interpersonal communication network may be less likely to actively process the overlapping media information. This argument suggests that the effect of each additional unit of exposure regardless of source is reduced at higher levels of exposure.
The current research hypothesizes a substitution effect rather than a reinforcement effect for the following reasons. A basic assumption is that the sorts of health information that people get from routine use of media may be fairly superficial, and thus is likely to overlap substantially with the pro-health information they get from high levels of interpersonal communication (see Davidson & Wallack, 2004; Pribble et al., 2006; Shuchman & Wilkes, 1997). Then, those who frequently talk about health with others may fulfill most of their need for information; that is, they will reach a ceiling and additional information from media sources will be essentially redundant. Therefore, the benefits from media exposure will be smaller for those who engage in high than in low levels of interpersonal communication.
Second, the incremental effect of information on individuals’ healthy lifestyle behaviors may decrease at higher levels of information exposure from the media. For healthy lifestyle behaviors, it may be that normative pressure becomes more critical than the acquisition of new knowledge – particularly given that information available from the media may be fairly superficial – once a certain level of health knowledge is accomplished (Fishbein & Yzer, 2003). Even if media channels can be utilized to convey normative information about healthy lifestyle behaviors, it has been argued that media channels are more suitable for the diffusion of new knowledge, whereas interpersonal channels are better in terms of the normative influences (for an overview, see Price & Oshagan, 1995).
Unfortunately, there have not been enough empirical studies to test the substitution effects in this area. However, several studies in related areas provide evidence to support the substitution effects model. Sociometric studies on campaign effects (e.g., Rogers, 2003; Valente & Saba, 1998) found that some individuals adopt new behaviors even when a low proportion of the individuals’ social networks engage in these behaviors. These so-called “low-threshold adopters,” who adopt innovations before others in their personal network, have been found to make greater use of media channels than others. Moreover, some scholars researching innovation diffusion in third World countries (e.g., Hornik, 1989) found that media campaign effects were maximized when no diffusion agents were available in that region. Even though none of the above studies directly tested the interaction between media exposure and interpersonal communication, and they did not address healthy lifestyle behaviors, these findings strengthen our expectation that media’s routine coverage of health issues and interpersonal health communication will have substitution effects.
Based on the above considerations, the current study put forth the following hypothesis:
-
Hypothesis 1
The effects of media use (television, print media, and the Internet) for obtaining health information on healthy lifestyle behaviors will be stronger for those with low levels of interpersonal health communication than for those with higher levels of interpersonal health communication, which supports the substitution model.
Methods2
The current study is a secondary analysis of the Annenberg National Health Communication Survey (ANHCS) data that uses a national probability sample of civilian, non-institutionalized adults (age 18 and above) in the United States. The Knowledge Networks (KN) conducted the ANHCS survey over the Internet from January 2005 through May 2006. The response rate for the study was 22.5%. Although there were 4,957 cases available, the sample size for the current study was 2,107 because the survey items comprising the Internet use for health information construct were only asked of a random half of all respondents.
Dependent Measures
An index of healthy lifestyle behaviors was formed with regard to smoking, binge drinking, eating fruits, eating vegetables, and exercising. Firstly, exercising was measured by asking respondents how often they exercise during an average week. Eating fruits and eating vegetables both were operationalized by a single indicator respectively. With regard to eating fruits, respondents were asked about how many servings of fruit they ate or drank per day on average during the past week. Also, respondents were asked about how many servings of vegetables they ate or drank per day on average during the past week, not counting potatoes. Smoking was measured by asking respondents how many cigarettes they smoked on a typical day during the past 7 days and then this item was reverse recoded, such that not smoking received the highest score. Finally, binge drinking was measured by asking respondents how many days they had 5 or more drinks of any alcoholic beverage and then this item was recoded so that respondents who had not had alcohol received the highest score.
Each of these five items was translated into a z-score and then summed to compose an index of healthy lifestyle behaviors (M = .00, SD = 2.88).3 The current study used self-rated health status (r = .23, p < .001) as a criterion to assess the validity of the index of healthy lifestyle behaviors.
Media Use for Health Information
Media use for health information consists of three variables: print media use for health information, television use for health information, and Internet use for health information. First, print media use for health information was computed by adding two four-point items (1 = “not at all,” 2 = “less than once per week,” 3 = “once per week,” 4 = “a few times a week”): “Some newspapers or general magazines have sections that report on health matters. About how often have you read such health sections in the past 30 days?” and “Some special health or medical magazines or newsletters focus on health issues. About how often have you read such magazines or newsletters in the past 30 days?” (r = .57, p < .001; M = 3.86, SD = 1.70).
Second, television use for health information was calculated by adding two four-point items (1 = “not at all” to 4 = “a few times a week”): “Some local or national television news programs include special segments of their newscasts which focus on health issues. About how often have you watched such health segments in the past 30 days?” and “Sometimes television shows (other than news programs) address issues about health or focus on doctors or hospitals. About how often have you watched such shows in the past 30 days?” (r = .53, p < .001; M = 4.32, SD = 1.82).
Third, Internet use for health information was constructed by adding two four-point items (1 = “not at all” to 4 = “a few times a week”): “How much have you actively looked for information about a specific health concern or medical problem that you or a family member had from the Internet in the past 30 days?” and “How often have you read health information in the Internet when you were not trying to find out about a specific health concern in the past 30 days?” (r = .58, p < .001; M = 3.64, SD = 1.81).
Interpersonal Health Communication
Interpersonal health communication was an additive index of two four-point items (1 = “not at all” to 4 = “a few times a week”): “Some people talk with family or friends about health issues. About how often have you talked with family or friends about health in the past 30 days?” and “How much have you actively looked for information about a specific health concern from family and friends in the past 30 days?” (r = .44, p < .001; M = 4.54, SD = 1.68).
Other Antecedent Variables
The control variables include self-rated health, family health status, and visits to health professionals that can be assumed to precede and to influence the relationship between media use and healthy lifestyle behaviors. People may seek health information from the media or interpersonal channels or engage in healthy lifestyle behaviors, especially when they or close family members have health problems (Jeong, 2007). Also, physician visits have been found to promote individuals’ healthy lifestyle practices in previous studies (e.g., Valente & Saba, 1998). Respondents were asked on a six-point scale (1 = “very poor” to 6 = “excellent”) how they would say their health is in general (M = 4.21, SD = .97). Family health status was measured by asking respondents whether anyone else now living in their household has a serious or chronic health condition or disease (24.7 percent responded “yes”). Physician visits was measured by asking respondents, on an eleven-point scale (1 = “never” to 11 = “more than twice a week”), how often they went to a doctor’s office or medical clinic (M = 3.03, SD = 1.69).
In addition, because individuals’ beliefs about the importance of healthy behaviors in determining their own health may influence both health information seeking behaviors and healthy lifestyle practices, the current study controlled for genetic determinism, which reflects health-related involvement and efficacy (Jeong, 2007). Genetic determinism was operationalized as an average score of respondents’ agreement with the following two statements on a five point scale (1 = “strongly disagree” to 5 = “strongly agree”): “Genes are more important than my own behavior in determining my health” and “The genes I was born with determine how healthy I will be throughout life” (r = .44, p < .001; M = 2.87, SD = 1.01).
Analysis Procedures
In order to test the substitution effects hypothesis in a multivariate model, the current study built a hierarchical ordinary least squares (OLS) regression that first enters demographic variables, i.e., age (M = 49.37, SD = 17.51), gender (52.9 percent females), formal education in years (M = 13.48, SD = 2.63), and income (median household income between $40,000 and $49,999), as well as the control variables outlined above, followed by the main effects of media use for health information and interpersonal health communication, and finally, by the interaction terms.
Therefore, in the final block of the regression predicting healthy lifestyle behaviors, three multiplicative terms were included, tapping (1) the interaction term between television use and interpersonal health communication, (2) the interaction term between newspaper use and interpersonal health communication, (3) and the interaction term between Internet use and interpersonal health communication. To avoid a multicollinearity problem between the product terms and their components, the current study standardized the main effect variables by translating them into z-scores before the interaction terms were formed (Cohen, Cohen, West, & Aiken, 2003). In addition, all of the regression analyses used unweighted samples.4
Results
The cross-sectional test of the hypothesis is presented in three models in Table 1. The first model presents the correlations between each independent variable and the healthy lifestyle behaviors index, the second presents the main effects of media use and interpersonal health communication after entering control variables, and the third presents the final model that adds the interaction terms as well as all the other variables.
Table 1.
Test for Interactions Predicting Healthy lifestyle Behaviors
| Zero-order Correlation | Main-Effect Model | Interaction-Effect Model | |
|---|---|---|---|
| Block 1: Controls | |||
| Age | .13*** | .15*** | .14*** |
| Gender (female=0, male=1) | −.15*** | −.10*** | −.09*** |
| Education | .17*** | .10*** | .10*** |
| Income | .10*** | −.00 | −.00 |
| Self-Rated Health | .24*** | .26*** | .26*** |
| Family Health Status | −.01 | .00 | .00 |
| Physician Visits | .04* | .06** | .06** |
| Genetic Determinism | −.04* | −.04 | −.04 |
| Incremental R2 (%) | 13.8*** | ||
| Block 2: Main Effects | |||
| Print Media Use | .28*** | .18*** | .18*** |
| TV Use | .10*** | −.04 | −.04 |
| Internet Use | .15*** | .05* | .06* |
| Interpersonal Health Communication | .17*** | .08*** | .09*** |
| Incremental R2 (%) | 4.8*** | ||
| Block 3: Interactions | |||
| Print Media Use × Interpersonal Health Communication | −.02 | ||
| Television Use × Interpersonal Health Communication | −.06** | ||
| Internet Use × Interpersonal Health Communication | −.05* | ||
| Incremental R2 (%) | .4* | ||
| Total R2 (%) | 18.6*** | 19.0*** | |
Notes: N = 2,107.
p < .05.
p < .01.
p < .001.
Cell entries are final standardized regression coefficients for Blocks 1 and 2 and before-entry standardized regression coefficients for Block 3.
As the main-effect model in Table 1 shows, demographics and other control variables accounted for a sizable amount of variance in healthy lifestyle behaviors (Incremental R2 = 13.8 percent, p < .001). Age and education were positively associated with healthy lifestyle behaviors. Also, females were found to engage in healthy lifestyle behaviors more than males. In addition, respondents’ self-rated health and their frequency of physician visits were positively linked with healthy lifestyle behaviors.
With regard to the main effects, print media use for health information (β = .18, p < .001) and Internet use for health information (β = .05, p < .05) were positively related to healthy lifestyle behaviors, even after controlling for demographics and other possible confounding variables (see the main-effect model in Table 1). Also, interpersonal health communication was positively related to healthy lifestyle behaviors (β = .08, p < .001), whereas the main effect of television use was not statistically significant (β = −.04, ns).
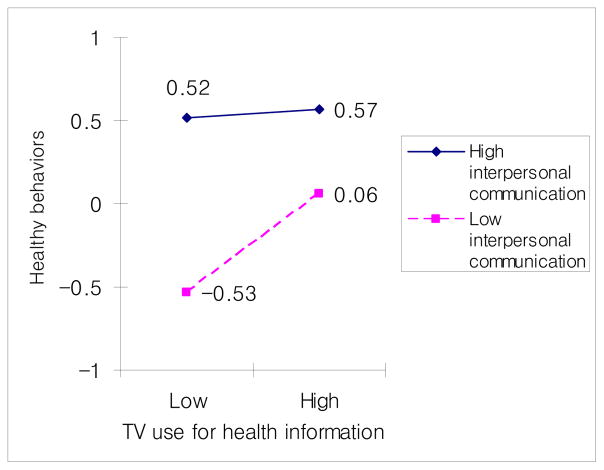
More importantly, Hypothesis 1 concerns the interactive effects between media use and interpersonal health communication on healthy lifestyle behaviors. As expected, TV use had a significantly stronger association with healthy lifestyle behaviors for respondents who had low levels of interpersonal health communication than for respondents who had high levels of interpersonal health communication (β = −.06, p < .01; see the interaction-effect model in Table 1 and Figure 1).
Figure 1.
Interplay between Interpersonal Health Communication and TV Use for Health Information
NOTE: Based on the distributions of both “TV use for health information” and “Interpersonal health communication,” these variables were divided into two groups. “Low TV use for health information” represents the bottom 57.6 percent (M = 3.00, SE = .02) and “High TV use for health information” represents the top 42.4 percent (M = 6.11, SE = .03). Moreover, “Low interpersonal communication” represents the bottom 51.3 percent (M = 3.14, SE = .02) and “High interpersonal communication” represents the top 48.7 percent (M = 6.01, SE = .03).
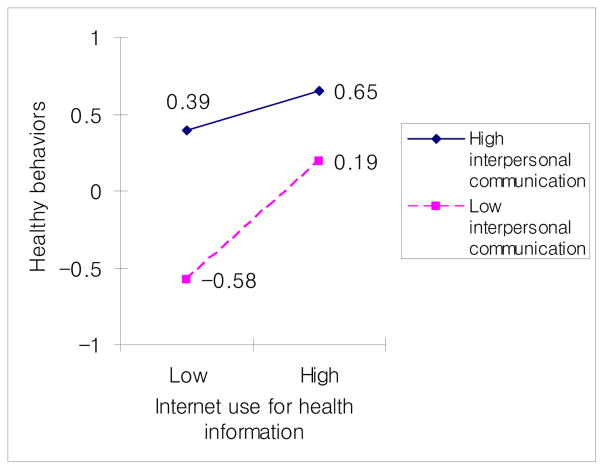
Likewise, Internet use for health information had significantly stronger effects on healthy lifestyle behaviors for those with low levels of interpersonal health communication (β = −.05, p < .05; see the interaction-model in Table 1 and Figure 2). In contrast, there was no interaction between print media use and interpersonal health communication. In sum, the results partially support Hypothesis 1.
Figure 2.
Interplay between Interpersonal Health Communication and Internet Use for Health Information
NOTE: Based on the distributions of both “Internet use for health information” and “Interpersonal health communication,” these variables were divided into two groups. “Low Internet use for health information” represents the bottom 56.1 percent (M = 2.27, SE = .01) and “High Internet use for health information” represents the top 43.9 percent (M = 5.40, SE = .04). Moreover, “Low interpersonal communication” represents the bottom 51.3 percent (M = 3.14, SE = .02) and “High interpersonal communication” represents the top 48.7 percent (M = 6.01, SE = .03).
Discussion
The most interesting findings in the current study are the interaction patterns between media use (television and the Internet) for health information and interpersonal health communication. To more accurately interpret the results, however, one methodological concern (i.e., a ceiling effect) should be considered. That is, one may argue that the substitution model was supported because respondents with high levels of interpersonal health communication had reached the upper limit of the measure of healthy lifestyle behaviors. However, this alternative explanation can be easily discounted because, among those who had high levels of interpersonal health communication, the variance in healthy lifestyle behaviors is not restricted, and the mean (M = .56, SD = 2.79) is not even close to the maximum (7.88) for the healthy-lifestyle-behaviors measure.
Findings should be interpreted with caution, however, due to limitations of the ANHCS data used in the current research. First, the current study is based on a cross-sectional survey and thus, cannot confirm the causality between communication variables and healthy lifestyle behaviors.
Second, the current study utilized only one or two items to measure each critical variable in this study, which makes the variables susceptible to measurement error. If we had been able to use multi-item measures, we could have detected a stronger relationship among our variables of interest and increased the validity of our research findings (Lee, Hornik, & Hennessy, 2008).
Relatedly, the measures of media exposure are limited in that they capture only the frequency of media use, while ignoring other important aspects of media use. As communication researchers have suggested, future studies should consider attention to media as well (Chaffee & Schleuder, 1986; McLeod & McDonald, 1985).
Moreover, it is possible that other confounding variables not included in the current study (e.g., interest in health) may have influenced media use, interpersonal health communication, and healthy lifestyle behaviors simultaneously. However, this possibility seems to be a less acute problem than at first glance because the same interaction patterns were not observed across all media channels.
In addition, the current study assumes that interpersonal interaction with family and friends should be conducive to health. However, recent studies (e.g., Hornik et al., 2001; Maxwell, 2002) have reported that some interpersonal communication networks, such as those of sensation-seeking adolescents, often encourage conversations about health-threatening behaviors (e.g. binge drinking, marijuana use). This type of interpersonal interaction has negative effects on healthy lifestyle behaviors.
Finally, the response rate for the ANHCS sample is somewhat low (22.5 percent), and consequently, the claim for national representativeness is rather limited. However, weighting the original sample to the U.S. population distribution on crucial variables (e.g., gender, education, race-ethnicity, region, etc.) did not materially affect the distribution of the current study’s critical variables or the coefficients in the regression results.
Despite these limitations, this study provided very important insights into the interaction between media use and interpersonal communication in the context of healthy lifestyle behaviors. Two findings should be highlighted in this context.
Above all, Figures 1 and 2 suggest that these interactive effects stemmed from two factors: first, obtaining health information from both television and from the Internet seemed to lead to healthy lifestyle behaviors among respondents with low levels of interpersonal health communication; second, both television and the Internet failed to provide additional information that could reinforce healthy lifestyle behaviors for those with high levels of interpersonal health communication. That is, television and Internet content had relatively little impact on healthy lifestyle behaviors among individuals who engaged in high levels of interpersonal health communication. In contrast, those who had fewer opportunities to engage in health communication chose to rely upon television and the Internet to make up for their lack of interpersonal sources (Kline et al., 1974). Put differently, those with high levels of interpersonal health communication had reached almost the maximum level of health information that is necessary for healthy lifestyle behaviors. On the other hand, information from television and the Internet could still improve the minimal knowledge held by those who exhibited low interpersonal communication, so the gap between the two groups appeared to be reduced.
Notably, print media use did not interact with interpersonal health communication. The size of the main effect of print media use on healthy lifestyle behaviors was substantially larger than those of TV use and Internet use, suggesting that print media use seems to predict healthy lifestyle behaviors regardless of the levels of interpersonal communication. This finding may reflect the possibility that, in comparison with health information on television or on the Internet, print media convey information that complements the health information provided by interpersonal communication with family and friends.
Implications
The findings of the current study suggest that the transmission of health information by television and by the Internet have empowering effects for individuals who do not frequently engage in interpersonal health communication with family and friends. That is, individuals who have low levels of interpersonal health communication and are consequently less likely to engage in healthy lifestyle behaviors can engage in higher levels of healthy lifestyle behaviors by using the health information that they acquire from television and the Internet. Given that those with low SES are less likely to engage in interpersonal health communication (Brashers, Goldsmith, & Hsieh, 2002) and that they are also subject to serious disparities in health care (Shaw et al., 2006), health practitioners and educators can utilize television and the Internet to increase health knowledge levels for those with low SES. Considering that the Digital Divide is still a significant problem in the U.S. (Shaw et al., 2006), television seems to be a more accessible medium to underserved populations as a health information channel.
In a theoretical sense, the findings of the current study are quite interesting, given that in the case of political participation, the reinforcement model continues to be supported (Hardy & Scheufele, 2005; Scheufele, 2002). For example, scholars have contended that political participation inherently needs much knowledge or deep understanding of political issues, which requires much “internal reflective integration” and “external reflective integration” of media content (i.e., interpersonal health talk) (Eveland, 2001; Sotirovic & McLeod, 2001). Therefore, even those who frequently talk about politics with others still have more room to increase their political participation behaviors by gaining more political information from media channels. These different patterns suggest that the interaction patterns between media exposure and interpersonal communication depend on what types of behaviors and information researchers focus on. Although speculative, the current study certainly provides a starting point for further theorizing the interplay between media exposure and interpersonal communication.
However, it should be noted that the theoretical model proposed in the current research is restricted in the sense that some critical factors in the health consumer informatics and the health literacy literature are missing.5 For example, in the era of “a consumer-driven health care system” (Niederdeppe, Frosch, & Hornik, 2005, p. 4), the increasing number of studies have found that patients’ health orientation and their attitude toward active participation in the medical decision making processes play a major role in determining their media use for health information gathering and health outcomes (Blumenthal, 1996; Dutta-Bergman, 2004, 2005; Hardey, 2001; Johnson, 1997). Moreover, it has been found that health literacy – “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions” (Parker & Gazmararian, 2003, p. 116) – predicts individuals’ healthy lifestyle behaviors and other health outcomes (Davis, Gazmararian, & Kennen, 2006; Schnittker, 2005). In addition, individuals’ “information sufficiency” levels could be measured and included as a control in the research model (Kahlor et al., 2003). It is possible that the interaction patterns observed in the current research could be changed if these variables were incorporated. Therefore, future studies may want to build on this study to construct a more elaborate model to examine how media exposure and interpersonal health communication interact and jointly influence health outcomes.
Footnotes
A previous version of this paper was presented at the annual meeting of the Association for Education in Journalism and Mass Communication, Washington DC, 2007. The author would like to thank Robert C. Hornik, Elihu Katz, Joseph N. Cappella, Minkyung Koo, Bridget J. Kelly, Jean Brechman, Xiaoxia Cao, and Hyunseo Hwang for their valuable feedback on the manuscript. I also acknowledge the very insightful comments of the editor and two anonymous reviews from Mass Communication & Society. This study was supported under a grant from the NCI Center of Excellence in Cancer Communication (CECCR) at the University of Pennsylvania (P50 CA101404). The data for this paper was provided by the Annenberg National Health Communication Survey supported, in part, by the Annenberg Trust at Sunnylands.
The current research focuses only on health-inducing interpersonal interaction, as is clearly delineated in the wording of the interpersonal health communication construct (see the measurement section). Admittedly, some interpersonal communication networks provide health-threatening information that contradicts media information; this type of information can diminish the beneficial effects of media exposure on healthy lifestyle behaviors (Bearman, Moody, & Stovel, 2004; Christakis & Fowler, 2007; Maxwell, 2002). Therefore, even when media and interpersonal sources provide contradictory information, the substitution effects rather than the reinforcement effects will be supported. However, it is beyond the scope of the present research to discuss this issue in greater detail.
Additional detailed information for the data collection procedure is described elsewhere (i.e., Lee, 2009).
This study does not report Cronbach’s alpha for the index of healthy lifestyle behaviors. Cronbach’s alpha assumes that all items comprising a scale commonly capture one latent variable, whereas an index consists of mutually exclusive items of healthy lifestyle behaviors (for an overview, see Bollen & Lennox, 1991; Streiner, 2003). Content validity and face validity are crucial in constructing indexes, whereas statistics tapping internal consistency are not relevant. As Streiner (2003) argued, validity for indexes heavily depends on prior research. One evidence for the validity of the index of healthy lifestyle behaviors comes from the fact that this same index has been used in the fields of public health (e.g., Gottlieb & Green, 1984), health communication (e.g., Rimal et al., 1999), and epidemiology (e.g., Berkman & Syme, 1979) during the past couple of decades.
Weights for the U.S. population are available and are used to verify some results. However use of weights produces inflated standard errors and thus reduces statistical power. This paper is meant to test theory; we were willing to sacrifice surer claims of national representativeness to increase the power for, and thus maximize sensitivity to, tests of theory.
I am indebted to an anonymous reviewer for this point.
References
- Barefoot JC, Gronbaek M, Feaganes JR, McPherson RS, Williams RB, Sieger IC. Alcoholic beverage preference, diet, and health habits in the UNC Alumni Health Study. American Journal of Clinical Nutrition. 2002;76 (2):466–472. doi: 10.1093/ajcn/76.2.466. [DOI] [PubMed] [Google Scholar]
- Bearman PS, Moody J, Stovel K. Chains of affection: The structure of adolescent romantic and sexual networks. American Journal of Sociology. 2004;110 (1):44–91. [Google Scholar]
- Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Social Science & Medicine. 2000;51:843–857. doi: 10.1016/s0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Syme L. Social networks, host resistance, and mortality: A nine-year follow-up study of Alameda County residents. American Journal of Epidemiology. 1979;109 (2):186–204. doi: 10.1093/oxfordjournals.aje.a112674. [DOI] [PubMed] [Google Scholar]
- Blanchard CM, Stein KD, Baker F, Dent MF, Denniston MM, Courneya KS, et al. Association between current lifestyle behaviors and health-related quality of life in breast, colorectal, and prostate cancer survivors. Psychology & Health. 2004;19 (1):1–13. [Google Scholar]
- Blumenthal D. Effects of market reforms on doctors and their patients. Health Affairs. 1996;15:170–184. doi: 10.1377/hlthaff.15.2.170. [DOI] [PubMed] [Google Scholar]
- Bollen K, Lennox R. Conventional wisdom on measurement: A structural equation perspective. Psychological Bulletin. 1991;110 (2):305–314. [Google Scholar]
- Brashers DE, Goldsmith DJ, Hsieh E. Information seeking and avoiding in health contexts. Human Communication Research. 2002;28 (2):258–271. [Google Scholar]
- Brosius H, Weimann G. Who sets the agenda? Agenda-setting as a two-step flow. Communication Research. 1996;23 (5):561–580. [Google Scholar]
- Brown J, Walsh-Childers K. Effects of media on personal and public health. In: Bryant J, Zillman D, editors. Media effects: Advances in theory and research. Hilldale, NJ: Lawrence Erlbaum; 2002. pp. 453–488. [Google Scholar]
- Chaffee SH. Mass media and interpersonal channels: Competitive, convergent, or complementary? In: Gumpert G, Cathart R, editors. Inter/media: Interpersonal communication in a media world. New York: Oxford University Press; 1986. pp. 57–77. [Google Scholar]
- Chaffee SH, Schleuder J. Measurement and effects of attention to media news. Human Communication Research. 1986;13:76–107. [Google Scholar]
- Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. New England Journal of Medicine. 2007;357:370–379. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3. Hillsdale, NJ: Lawrence Erlbaum Associates; 2003. [Google Scholar]
- Davidson AE, Wallack L. A content analysis of sexually transmitted diseases in the print news media. Journal of Health Communication. 2004;9:111–117. doi: 10.1080/10810730490425268. [DOI] [PubMed] [Google Scholar]
- Davis TC, Gazmararian JA, Kennen EM. Approaches to improving health literacy: Lessons from the field. Journal of Health Communication. 2006;11:551–554. doi: 10.1080/10810730600835517. [DOI] [PubMed] [Google Scholar]
- Dutta-Bergman MJ. Primary sources of health information: Comparisons in the domain of health attitudes, health cognitions, and health behaviors. Health Communication. 2004;16 (3):273–288. doi: 10.1207/S15327027HC1603_1. [DOI] [PubMed] [Google Scholar]
- Dutta-Bergman MJ. Developing a profile of consumer intention to seek out additional information beyond a doctor: The role of communicative and motivation variables. Health Communication. 2005;17 (1):1–16. doi: 10.1207/s15327027hc1701_1. [DOI] [PubMed] [Google Scholar]
- Eagly AH, Chaiken S. The psychology of attitude. Belmont, CA: Wadsworth; 1993. [Google Scholar]
- Eveland WP., Jr The cognitive mediation model of learning from the news: Evidence from nonelection, off-year election, and presidential election contexts. Communication Research. 2001;28 (5):571–601. [Google Scholar]
- Eveland WP., Jr The effect of political discussion in producing informed citizens: The roles of information, motivation, and elaboration. Political Communication. 2004;21:177–193. [Google Scholar]
- Fishbein M, Yzer MC. Using theory to design effective health behavior interventions. Communication Theory. 2003;13:164–183. [Google Scholar]
- Freidson E. The changing nature of professional control. Annual Review of Sociology. 1984;10:1–20. [Google Scholar]
- Gottlieb NH, Green LW. Life events, social network, life-style, and health: An analysis of the 1979 national survey of personal health practices and consequences. Health Education Quarterly. 1984;11 (1):91–105. doi: 10.1177/109019818401100105. [DOI] [PubMed] [Google Scholar]
- Hardey M. “E-Health”: The Internet and the transformation of patients into consumers and producers of health knowledge. Information, Communication, & Society. 2001;4 (3):388–405. [Google Scholar]
- Hardy BW, Scheufele DA. Examining differential gains from Internet use: Comparing the moderating role of talk and online interactions. Journal of Communication. 2005;55 (1):71–84. [Google Scholar]
- Hornik RC. Channel effectiveness in development communication programs. In: Rice RE, Atkin CK, editors. Public communication campaigns. Newbury Park, CA: Sage; 1989. pp. 309–330. [Google Scholar]
- Hornik RC, Maklan D, Judkins D, Cadell D, Yanovitzky I, Zador P, et al. Evaluation of the national youth anti-drug media campaigns: Second semi-annual report of findings. Rockville, MD: Westat; 2001. [Google Scholar]
- Jeong S. Effects of news about genetics and obesity on controllablity attribution and helping behavior. Health Communication. 2007;22 (3):221–228. doi: 10.1080/10410230701626877. [DOI] [PubMed] [Google Scholar]
- Johnson JD. Cancer-related information seeking. Cresskill, NJ: Hampton Press; 1997. [Google Scholar]
- Kahlor L, Dunwoody S, Griffin RJ, Neuwirth K, Giese J. Studying heuristic-systematic processing of risk communication. Risky Analysis. 2003;23 (2):355–368. doi: 10.1111/1539-6924.00314. [DOI] [PubMed] [Google Scholar]
- Katz E. Communication research since Lazarsfeld. Public Opinon Quarterly. 1987;51:S25–S45. [Google Scholar]
- Katz E, Lazarsfeld PF. Personal influence: The part played by people in the flow of mass communication. Glencoe, IL: The Free Press; 1955. [Google Scholar]
- Kline FG, Miller PV, Morrison AJ. Adolescents and family planning information: An exploration of audience needs and media effects. In: Blumler J, Katz E, editors. The uses of mass communication: Current perspectives on gratification research. Newbury Park, CA: Sage; 1974. pp. 112–136. [Google Scholar]
- Labre MP, Walsh-Childers K. Friendly advice? Beauty messages in web sites of teen magazines. Mass Communication & Society. 2003;6 (4):379–378. [Google Scholar]
- Lee CJ. The role of Internet engagement in the health-knowledge gap. Journal of Broadcasting and Electronic Media. 2009;53(3):365–382. doi: 10.1080/08838150903102758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee CJ, Hornik RC, Hennessy M. The reliability and stability of general media exposure measures. Communication Methods and Measures. 2008;2 (1–2):6–22. [Google Scholar]
- Maxwell K. Friends: The role of peer influence across adolescent risk behaviors. Journal of Youth and Adolescence. 2002;31 (4):267–278. [Google Scholar]
- McDonald DG. Media orientation and television news viewing. Journalism Quarterly. 1990;67:11–20. [Google Scholar]
- McLeod JM, McDonald DG. Beyond mere exposure: Media orientations and their impact on political processes. Communication Research. 1985;12 (1):3–33. [Google Scholar]
- Niederdeppe J, Frosch DL, Hornik RC. Cancer-related news coverage and information seeking: Results from a national survey; Paper presented at the annual meeting of the American Society for Preventive Oncology; San Francisco, CA. 2005. Mar, [Google Scholar]
- Nilson LB. An application of the occupational “uncertainty principle” to the professions. Social Problems. 1979;26 (5):570–581. [Google Scholar]
- Parker RM, Gazmararian JA. Health literacy: Essential for health communication. Journal of Health Communication. 2003;11:116–118. doi: 10.1080/713851963. [DOI] [PubMed] [Google Scholar]
- Pew Research Center. Online Health Search 2006: Most internet users start at a search engine when looking for health information online. Released on October. 2006;29:2006. [Google Scholar]
- Pribble JM, Goldstein KM, Fowler EF, Greenberg MJ, Noel SK, Howell JD. Medical news for the public to use? What’s on local TV news. American Journal of Managed Care. 2006;12 (3):170–176. [PubMed] [Google Scholar]
- Price V, Oshagan H. Social-psychological perspectives on public opinion. In: Glasser TL, Salmon CT, editors. Public opinion and the communication of consent. New York: Guilford; 1995. pp. 177–216. [Google Scholar]
- Rimal RN, Flora JA, Schooler C. Achieving improvements in overall health orientation: Effects of campaign exposure, information seeking, and health media use. Communication Research. 1999;26 (3):322–348. [Google Scholar]
- Rimal RN, Real K. Understanding the influence of perceived norms on behaviors. Communication Theory. 2003;13:184–203. [Google Scholar]
- Rogers EM. Diffusion of innovations. 5. New York: Free Press; 2003. [Google Scholar]
- Scheufele DA. Examining differential gains from mass media and their implications for participatory behavior. Communication Research. 2002;29 (1):46–65. [Google Scholar]
- Schnittker J. Cognitive abilities and self-rated health: Is there a relationship? Is it growing? Does it explain disparities? Social Science Research. 2005;34:821–842. [Google Scholar]
- Shah DV, Cho J, Nah S, Gotlieb MR, Hwang H, Lee N, Scholl RM, et al. Campaign ads, online messaging, and participation: Extending the communication mediation model. Journal of Communication. 2007;57 (4):676–703. [Google Scholar]
- Shaw B, Gustafson DH, Hawkins R, McTavish F, McDowell H, Pingree S, Ballard D. How underserved breast cancer patients use and benefit from ehealth programs: Implications for closing the digital divide. American Behavioral Scientist. 2006;49 (6):823–834. [Google Scholar]
- Shuchman M, Wilkes MS. Medical scientists and health news reporting: A case of miscommunication. Annals of Internal Medicine. 1997;12 (1):976–982. doi: 10.7326/0003-4819-126-12-199706150-00008. [DOI] [PubMed] [Google Scholar]
- Sotirovic M, McLeod JM. Values, communication behavior, and political participation. Political Communication. 2001;18 (3):273–300. [Google Scholar]
- Southwell BG, Torres A. Connecting interpersonal and mass communication: Science news exposure, perceived ability to understand science, and conversation. Communication Monographs. 2006;73 (3):334–350. [Google Scholar]
- Southwell BG, Yzer MC. The roles of interpersonal communication in mass media campaigns. Communication Yearbook. 2007;31:419–462. [Google Scholar]
- Streiner DL. Being inconsistent about consistency: When coefficient alpha does and doesn’t matter. Journal of Personality Assessment. 2003;80 (3):217–222. doi: 10.1207/S15327752JPA8003_01. [DOI] [PubMed] [Google Scholar]
- Stryker JE. Media and marijuana: A longitudinal analysis of news media effects on adolescents’ marijuana use and related outcomes, 1977–1999. Journal of Health Communication. 2003;8 (4):305–328. doi: 10.1080/10810730305724. [DOI] [PubMed] [Google Scholar]
- Valente TW, Saba WP. Mass media and interpersonal influence in a reproductive health communication campaign in Bolivia. Communication Research. 1998;25(1):96–124. [Google Scholar]
- Viswanath K. The communications revolution and cancer control. Nature Reviews. 2005;5:828–835. doi: 10.1038/nrc1718. [DOI] [PubMed] [Google Scholar]
- Yanovitzky I, Stryker J. Mass media, social norms, and health promotion effects. Communication Research. 2001;28 (2):208–239. [Google Scholar]