Abstract
Objectives
To examine racial/ethnic differences in the effects of body mass index (BMI) on the onset of functional impairment over 10 years of follow-up.
Design
Longitudinal analyses of a cohort from a nationally representative survey of community-dwelling American adults.
Setting
Six waves (1996-2006) of US Health and Retirement Study (HRS).
Participants
Two groups of HRS participants aged ≥50 without functional impairment at baseline (1996): 5,884 with no mobility difficulty, and 8,484 with no Activities of Daily Living (ADLs) difficulty.
Measurements
Mobility difficulty was a composite measure of difficulty in walking several blocks, walking one block, climbing several flights of stairs, and climbing one floor of stairs. ADL difficulty was measured by difficulty in dressing, bathing or showing, eating, and getting in or out of bed without help. The association between the baseline BMI categories and risk to develop functional impairment was estimated using generalized estimating equations (GEE) models.
Results
Overweight and obesity were significant predictors for functional impairment. Compared to the Whites in the same overweight and obese categories, Hispanics were 41% and 91% more likely to develop ADL disability. Blacks in the overweight and severely obese categories were also more likely than their White counterparts to develop ADL disability. Risk of developing ADL difficulty was higher for Hispanics than for Blacks in the obese category. For onset of mobility difficulty, no significant differences were found across racial/ethnic groups within any BMI Category.
Conclusion
Blacks and Hispanics were at higher risk than Whites for ADL but not mobility impairment. In addition to weight control, prevention efforts should promote exercise to reduce functional impairment, especially for Blacks and Hispanics, who are at higher risk.
Keywords: obesity, overweight, mobility difficulty, ADL difficulty, racial/ethnic difference
INTRODUCTION
Prevalence of obesity in all age groups has increased during the past three decades in the United States.1-3Age-adjusted prevalence of obesity among US adults over age 20 rose from 23% between 1988 and1994 to approximately 34% in 2008.4 An estimated47.5 million US adults (21.8%) had at least one disability in 2005, an increase of 3.4 million from 1999; the prevalence of disability increased with age.5, 6 As average life expectancy and the number of older adults continue to rise in the US, increasing numbers of Americans are expected to experience some level of functional impairment.
Living free of functional impairment (e.g., mobility difficulty and difficulty with activities of daily living (ADLs) has long been a targeted outcome of United States aging policy.7Given that functional impairment is common in older Americans and the prevalence of obesity is increasing, it is important to examine the relationship between the two. Strong evidence suggests that obesity has an impact on onset of self-reported functional impairment.8-14,30-32However, relatively few longitudinal studies have focused on the role of obesity and overweight in the development of functional impairment across racial/ethnic groups.12,13Wee et al.,12 using Medicare Beneficiary Survey data, found that adults aged ≥65 with higher body mass index (BMI) were more likely than those of normal weight to develop new disability, particularly ADL disability. In their sample, the association between obesity and onset of ADL disability was weaker for Black than for White elders. This sample included only persons aged ≥65 who were Medicare beneficiaries, Blacks were only minority group represented, and the follow-up period (2 years) was short, which may limit the generalizability of these findings. Dunlop et al.13reported baseline obesity data from a 6-year study of disability onset in a sample of Americans aged ≥65 that included Hispanics, Blacks, and Whites, but obesity was not included as a predictor in their models. .Because individuals can develop functional impairments (particularly mobility difficulty) before age 65,there is a need for longitudinal research on onset of functional impairment in middle-aged populations.11, 32
The purpose of our study was to examine the long-term impact of overweight and obesity on onset of functional impairment in older Americans of three racial/ethnic groups (Black, Hispanic, White), controlling for confounders such as socio-demographic characteristics, health behaviors, and chronic clinical conditions. This study is unique in that it combines: 1) longitudinal research on a nationally representative U.S. sample with biennial data collection over a 10-year period; 2) sample members at baseline were predominantly middle-aged (50- 64 years), allowing evaluation of the onset of functional impairment in this age group; and 3) a focus on the effects of obesity and overweight on functional impairment across the three racial/ethnic groups. We propose two research questions: 1) Are there racial/ethnic differences in overweight and obesity as predictors of onset of functional impairment? 2) If such differences exist, are they consistent across different domains of functional impairment – specifically mobility difficulty and ADL difficulty?
Given the increasing size and diversity of the elderly population and the increasing prevalence of obesity and overweight among older adults, a better understanding of effects of obesity on functional impairment in this population is relevant to US health care planning. Information generated from this study could also help inform the discussion about the appropriateness of weight control in diverse elderly populations.
METHODS
Data and Study Population
We analyzed the effect of baseline BMI on the onset of functional impairment using six successive waves (1996 to 2006) from the US Health Retirement Study (HRS). The HRS is a biennial panel study designed to permit analyses of impacts and interrelationships of various changes and transitions for community-residing older Americans in the domains of health, finances, and family.15 The 1996 wave was used as baseline for this study because response options for functional limitation items in this and subsequent waves were different from those in the previous (1992 and 1994) waves. The 1996 wave included 12,622 persons; of these, 10,964 respondents (86.9%) completed the interview. Exclusion criteria for this study were: 1) respondents with race/ethnicity, gender, or BMI data missing (n=132); 2) respondents aged <50 at baseline (n=479); 3) respondents of any race/ethnicity other than White, Black, or Hispanic (n=229); 4) respondents in the “under normal weight” (BMI<18.5) category at baseline (n=131); 5) respondents missing functional impairment data in all follow-up waves (n=574).
The remaining 9,419 respondents were eligible for the study. From this group, we selected two samples:
Respondents who reported no mobility difficulties at baseline one group (n=5,884),
Respondents who reported no ADL difficulties at baseline (n=8,484).
Measurement of Dependent Variables
Functional Impairment
Dependent variables assessed functional impairment in two domains: mobility difficulty and difficulty in performing activities of daily living (ADL). Mobility difficulty was a composite measure based on respondents’ answers to items asking if they had difficulty walking several blocks, walking one block, climbing several flights of stairs without resting, and climbing one flight of stairs without resting. ADL difficulty was a composite measure based on respondents’ answers to items asking if they had difficulty dressing, bathing or showering, eating, and getting in or out of bed without help. For each item, respondents who reported “Yes” or “Can't do” were coded as “1”; those who responded “no” were coded as “0”; and those who answered “don't do”, “don't know”, or “refused” were set as missing. The outcome variable for each functional impairment domain (mobility or ADL) was coded as “1” (impairment) if respondents reported having difficulty with any activity in the domain; otherwise it was coded as “0” (no impairment).Self-reported mobility difficulty and ADL difficulty have been shown to be valid in comparisons with objective measures of physical function.16Standardized Cronbach's alphas for the four mobility difficulty items and the four ADL difficulty items were 0.84 and 0.77 respectively.
Baseline Body Mass Index (BMI) Category
Baseline BMI for all eligible respondents was calculated from self-reported body weight and height using the formula BMI = [weight in pounds / (height in inches* Height in inches)] * 703. Body weight data (collected at all waves)were available in 1996 for all but 112 respondents. For those individuals, weight at the 1994 or 1992 waves was used as the baseline value. Body height had been recorded for all HRS participants in 1992 and 1994, but from 1996 on, it was recorded only for individuals who had not previously reported their height at an earlier wave. The most recent available body height value was therefore used for baseline BMI calculation. Following the NHLBI guidelines and previous research,17-18 we grouped respondents into five groups according to their baseline BMI: BMI<18.5(underweight), 18.5≤BMI<25(normal weight), 25≤BMI<30(overweight), 30≤BMI<35 (obese) and BMI≥35 (severely obese).17
Socio-demographic Characteristics
Socio-demographic characteristics including age, gender, marital status, race/ethnicity, and education, which are well-known potential confounders of functional impairment,19were coded as follows: Baseline age: age ≥65=1, age 50-64=0; gender: female=1, male=0; marital status: married=1, otherwise=0; education=actual years of schooling completed). Race/ethnicity was categorized as White, Black, or Hispanic.
Health Behaviors
Lack of physical activity and smoking are known risk factors for functional impairment,20-23while moderate alcohol intake is a protective factor. 24Drinking was assessed using a trichotomous variable derived from responses to items asking 1) whether participants ever drink alcoholic beverages (if no, code as nondrinkers); 2) average number of days/week that they drink; 3) average number of drinks/day on days when they drink. Respondents reporting drinking <5 days/week (<4 days/week for women) and average consumption of ≤14 drinks per week were coded as light/moderate drinkers; those reporting more frequent drinking or consumption of 15+ drinks/week were coded as heavy drinkers.25Smoking was assessed by classifying participants as never smoked, former smokers, or current smokers. Vigorous physical activity was coded as 1 if respondents reported participating in activities such as, sports, heavy housework, or a job involving physical labor at least 3 times per week during the past year, 0 otherwise.26
Disease Severity
Self-reported diseases as risk factors for functional impairment have been explored in many studies.10, 27-29 HRS includes several questions which can be used to measure severity of seven major chronic diseases: hypertension, diabetes, lung disease, heart disease, stroke, arthritis, and cancer. Disease severity was assessed by assigning one point to participants reporting ever having been diagnosed with the disease, and adding additional points for a) any report of current treatment of the disease, any report of having current symptoms of the disease.10, 18
Data Analysis
Descriptive and multivariate analyses were performed using SAS 9.3 (SAS Institute Inc., Cary, NC). ANOVAs were used to compare means between Blacks and Whites and between Hispanics and Whites. Chi-square tests were used for proportional comparisons. We created 12 dummy variables based on combinations of BMI categories with racial/ethnic groups. Normal-weight Whites were chosen as a reference group in the analysis. Repeated measurements of health behaviors and disease severity were used in fitting GEE models to estimate the impact of BMI on the onset of functional impairment in both the mobility and ADL domains. For the onset of ADL disability outcome, baseline mobility difficulty was also added as an independent variable. Final models did not include terms for interactions between BMI categories and racial/ethnic groups because preliminary analyses revealed no significant interactions. Family income was excluded from this the study, because so many respondents (24%) did not report family income at the 1996 baseline wave. Model fit was assessed using quasi-likelihood under the independence model criterion (QIC). Significance of racial/ethnic differences within the each BMI category were tested using the GEE models adjustedfor socio-demographic and health behavior variables (Model 1), and socio-demographic, health behavior, and disease severity scores (Model 2).
RESULTS
Descriptive Analysis
At study baseline (1996), the mobility difficulty sample included 5,884 participants (78.5% White, 13.4% Black, and 8.1% Hispanic) without mobility impairment. During the 10-year follow-up, 3,051 participants developed mobility difficulty (51.9% onset rate). Onset rates for mobility difficulty were significantly higher for Hispanics and Blacks than for Whites (Table 1). At the 2006 wave, 4,901 (83.3% of the original participants) remained in the sample; 522 (8.9%) had died. Descriptive statistics for each race/ethnicity group and the total sample are presented in Table 1.
Table 1.
BMI Categories, Socio-demographic Characteristics, Health Behaviors, Disease Severity Scores, and Onset of Mobility Difficulty during Follow-up, by Race/Ethnicity, in U.S. OlderAdults Who Were Free of Mobility Difficulty at Baseline.
| Variables | Whiteb (N=4618) | Black (N=791) | Hispanic (N=475) | Total (N=5884) | |
|---|---|---|---|---|---|
| BMI Categories (%) | |||||
| Normal (18.5 ≤ BMI < 25) | 39.8 | 26.7*** | 28.8*** | 37.1 | |
| Overweight (25 ≤ BMI < 30) | 43.6 | 44.9 | 48.0 | 44.1 | |
| Obese (30 ≤ BMI < 35) | 13.7 | 21.3*** | 19.4*** | 15.2 | |
| Severely obese (BMI ≥ 35) | 2.9 | 7.1*** | 3.8 | 3.6 | |
| Socio-demographic Characteristics | |||||
| Age group 50-64 years (%) | 86.9 | 89.4 | 86.9 | 87.2 | |
| Age group 65+ years (%) | 13.1 | 10.6 | 13.1 | 12.8 | |
| Education, years: mean (SD) | 13.1(2.6) | 11.6(3.1)*** | 9.0(4.4)*** | 12.6(3.1) | |
| Female (%) | 47.0 | 50.6 | 45.1 | 47.3 | |
| Married (%) | 84.9 | 63.3*** | 81.3* | 81.7 | |
| Health Behaviors (%) | |||||
| Light/moderate drinker | 46.7 | 40.9** | 40.0** | 45.4 | |
| Heavy drinker | 14.7 | 5.6*** | 6.1*** | 12.8 | |
| Former smoker | 48.3 | 41.2*** | 42.7* | 46.9 | |
| Current smoker | 17.8 | 21.5* | 17.7 | 18.3 | |
| Vigorous physical activity | 63.2 | 56.0*** | 52.6*** | 61.4 | |
| Disease Severity Scores (%) | Score | ||||
| Hypertension | 0 | 67.4 | 47.4*** | 65.3 | 64.6 |
| Ever told had hypertension (1 pt.) | 1 | 8.9 | 11.8* | 11.4 | 11.4 |
| Taking medication (1 pt.) | 2 | 23.7 | 40.8*** | 23.3 | 23.4 |
| Diabetes | 0 | 93.2 | 84.6*** | 87.6*** | 91.6 |
| Ever told had diabetes (1 pt.) | 1 | 2.5 | 3.4 | 3.6 | 2.7 |
| Taking oral medication (1 pt.) | 2 | 4.1 | 11.4*** | 8.4*** | 5.4 |
| Using insulin (1 pt.) | 3 | 0.2 | 0.6* | 0.4 | 0.3 |
| Lung disease | 0 | 91.8 | 92.2 | 94.1 | 92.0 |
| Ever told had COPD (1 pt.) | 1 | 6.3 | 6.8 | 4.8 | 6.3 |
| Taking medication (1 pt.) | 2 | 1.3 | 0.6 | 0.8 | 1.2 |
| Report respiratory symptoms (1 pt.) | 3 | 0.5 | 0.4 | 0.0 | 0.5 |
| Report limitation in activities (1 pt.) | 4 | 0.1 | 0.0 | 0.2 | 0.1 |
| Heart disease | 0 | 88.6 | 92.2** | 93.5** | 89.5 |
| Ever told had heart attack, coronary heart disease, angina, congestive heart failure, or other heart problem (1 pt.) | 1 | 4.5 | 3.7 | 3.0 | 4.3 |
| Taking or carrying medications (1 pt.) | 2 | 4.9 | 3.0* | 2.7* | 4.5 |
| Had any angina or chest pain (1 pt.) | 3 | 1.8 | 1.0 | 0.4* | 1.6 |
| Ever had cardiac surgery (1 pt.) | 4 | 0.2 | 0.1 | 0.4 | 0.2 |
| Stroke | 0 | 98.2 | 97.4 | 98.1 | 98.1 |
| Ever had a stroke (1 pt.) | 1 | 1.0 | 1.4 | 1.3 | 1.1 |
| Taking medications (1 pt.) | 2 | 0.5 | 1.1* | 0.6 | 0.6 |
| Still have remaining problem (1 pt.) | 3 | 0.3 | 0.1 | 0.0 | 0.2 |
| Arthritis | 0 | 61.6 | 61.4 | 68.0** | 62.1 |
| Ever had arthritis or rheumatism (1 pt.) | 1 | 7.1 | 7.0 | 9.3 | 7.3 |
| Taking medication or other treatment (1 pt.) | 2 | 22.6 | 22.4 | 16.0*** | 22.1 |
| Had pain, stiffness or swelling in joints (1 pt.) | 3 | 8.6 | 9.2 | 6.7 | 8.5 |
| Cancer | 0 | 93.2 | 96.7*** | 95.8* | 93.9 |
| Ever told had cancer (1 pt.) | 1 | 5.9 | 2.8*** | 3.6* | 5.3 |
| Receiving treatment for cancer (1 pt.) | 2 | 0.8 | 0.5 | 0.6 | 0.8 |
| Onset of mobility difficulty during follow-upb (N) | 2321 | 445 | 285 | 3051 | |
| Onset ratec for mobility difficulty (%) | |||||
| Total sample | 50.3 | 56.3* | 60.0*** | 51.9 | |
| Participants with normal weight at baseline | 41.4 | 49.8* | 54.0** | 43.0 | |
| Participants overweight at baseline | 51.3 | 53.0 | 55.7 | 51.9 | |
| Participants obese or severely obese at baseline | 68.7 | 67.6 | 76.4 | 69.2 | |
| Participants in each weight category at baseline | |||||
| Normal weight at baseline(N) | 1837 | 211 | 137 | 2185 | |
| Overweight at baseline(N) | 2012 | 355 | 228 | 2595 | |
| Obeseor severely obese at baseline(N) | 769 | 225 | 110 | 1104 |
Notes: Mobility difficulty was a composite measure of difficulty in walking several blocks, walking one block, climbing several flights of stairs, and climbing one floor of stairs.
aThe reference category for racial/ethnic group is White.
Total number of participants in sample with onset of mobility difficulty between 1996 and 2006.
10-year onset rate = (number of participants with onset of mobility difficulty during follow-up)/(number of participants at baseline).
BMI = Body Mass Index; SD = Standard Deviation; COPD = Chronic Obstructive Pulmonary Disease.
p<0.05
p<0.01
p<0.001.
At study baseline, the ADL difficulty sample included 8,484 participants (77.3% White, 14.6% Black, and 8.1% Hispanic) without ADL impairment. During the 10-year follow-up, 1,711 participants developed ADL difficulty (20.2% onset rate). Onset rates for ADL difficulty were significantly higher for Hispanics and Blacks than for Whites (Table 2). At the 2006 wave, 6,993 (82.4% of the original participants) remained in the sample, and 974 (11.5%) had died. Descriptive statistics for each race/ethnicity group and the total sample are presented in Table 2.
Table 2.
BMI Categories, Socio-demographic Characteristics, Health Behaviors, Disease Severity Scores, and Onset of ADL Difficulty during Follow-up,by Race/Ethnicity, in U.S. Older Adults Who Were Free of ADL Difficulty at Baseline
| Variables | Whitea (N=6559) | Black (N=1237) | Hispanic (N=688) | Total (N=8484) | |
|---|---|---|---|---|---|
| BMI Categories (%) | |||||
| Normal (18.5 ≤ BMI < 25) | 36.3 | 23.9*** | 25.7*** | 33.7 | |
| Overweight (25 ≤ BMI < 30) | 41.9 | 42.0 | 47.3** | 42.3 | |
| Obese (30 ≤ BMI < 35) | 16.3 | 23.5*** | 21.2*** | 17.7 | |
| Severely obese (BMI ≥ 35) | 5.5 | 10.6*** | 5.8 | 6.3 | |
| Socio-demographic Characteristics | |||||
| Age group 50-64 years(%) | 87.0 | 89.0 | 87.2 | 87.3 | |
| Age group 65+ years(%) | 13.0 | 11.0 | 12.8 | 12.7 | |
| Education, years: mean (SD) | 12.8(2.6) | 11.5(3.1)*** | 8.8(4.4)*** | 12.3(3.1) | |
| Female (%) | 51.9 | 58.5*** | 52.0 | 52.9 | |
| Married (%) | 83.1 | 61.0*** | 78.3** | 79.5 | |
| Health Behaviors (%) | |||||
| Light/moderate drinker | 44.4 | 36.8*** | 36.4*** | 42.6 | |
| Heavy drinker | 13.5 | 5.4b | 5.5*** | 11.7 | |
| Former smoker | 46.8 | 41.2*** | 39.7*** | 45.4 | |
| Current smoker | 19.9 | 23.0* | 17.9 | 20.1 | |
| Vigorous physical activity | 55.9 | 47.5*** | 44.6*** | 53.7 | |
| Disease Severity Scores (%) | Score | ||||
| Hypertension | 0 | 62.4 | 40.8*** | 58.6 | 58.9 |
| Ever told had hypertension (1 pt.) | 1 | 9.3 | 11.7** | 12.3* | 9.9 |
| Taking medication (1 pt.) | 2 | 28.3 | 47.5*** | 29.1 | 31.2 |
| Diabetes | 0 | 90.8 | 80.3*** | 83.1*** | 88.6 |
| Ever told had diabetes (1 pt.) | 1 | 2.9 | 3.8 | 4.4* | 3.2 |
| Taking oral medication (1 pt.) | 2 | 5.9 | 14.4*** | 11.2*** | 7.6 |
| Using insulin (1 pt.) | 3 | 0.4 | 1.5*** | 1.3** | 0.6 |
| Lung disease | 0 | 87.0 | 87.5 | 92.3*** | 87.5 |
| Ever told had COPD (1 pt.) | 1 | 8.4 | 8.7 | 4.9** | 8.1 |
| Taking medication (1 pt.) | 2 | 2.3 | 1.5 | 1.9 | 2.1 |
| Report respiratory symptoms (1 pt.) | 3 | 1.5 | 1.8 | 0.4* | 1.5 |
| Report limitation in activities (1 pt.) | 4 | 0.8 | 0.5 | 0.4 | 0.7 |
| Heart disease | 0 | 84.5 | 86.7 | 91.1*** | 85.4 |
| Ever told had heart attack, coronary heart disease, angina, congestive heart failure, or other heart problem (1 pt.) | 1 | 5.3 | 4.8 | 3.8 | 5.1 |
| Taking or carrying medications (1 pt.) | 2 | 6.2 | 5.5 | 3.6** | 5.9 |
| Had any angina or chest pain (1 pt.) | 3 | 3.4 | 2.9 | 1.2** | 3.2 |
| Ever had cardiac surgery (1 pt.) | 4 | 0.5 | 0.1 | 0.3 | 0.4 |
| Stroke | 0 | 97.4 | 95.9** | 97.7 | 97.2 |
| Ever had a stroke (1 pt.) | 1 | 1.2 | 2.3** | 1.3 | 1.4 |
| Taking medications (1 pt.) | 2 | 0.8 | 1.1 | 0.7 | 0.8 |
| Still have remaining problem (1 pt.) | 3 | 0.6 | 0.7 | 0.3 | 0.6 |
| Arthritis | 0 | 54.1 | 51.2 | 60.8*** | 54.2 |
| Ever had arthritis or rheumatism (1 pt.) | 1 | 7.0 | 6.5 | 10.3** | 7.2 |
| Taking medication or other treatment (1 pt.) | 2 | 25.5 | 26.7 | 16.8*** | 25.0 |
| Had pain, stiffness or swelling in joints (1 pt.) | 3 | 13.4 | 15.6* | 12.1 | 13.6 |
| Cancer | 0 | 92.6 | 95.3*** | 95.4** | 93.2 |
| Ever told had cancer (1 pt.) | 1 | 6.4 | 3.6*** | 3.6** | 5.8 |
| Receiving treatment for cancer (1 pt.) | 2 | 1.0 | 1.1 | 1.0 | 1.0 |
| Mobility Difficulty at Baseline (%) | 30.8 | 37.2*** | 33.4 | 31.9 | |
| Onset of ADL difficulty during follow-upb (N) | 1183 | 338 | 190 | 1711 | |
| Onset ratec for ADL difficulty (%) | 18.0 | 27.3*** | 27.6*** | 20.2 | |
| Total sample | 18.0 | 27.3*** | 27.6*** | 20.2 | |
| Participants with normal weight at baseline | 13.9 | 23.7*** | 18.6 | 15.2 | |
| Participants overweight at baseline | 17.5 | 23.3** | 25.5*** | 19.0 | |
| Participants obese or severely obese at baseline | 26.1 | 34.8*** | 39.8*** | 29.1 | |
| Participants in each weight category at baseline | |||||
| Normal weight at baseline (N) | 2384 | 295 | 177 | 2856 | |
| Overweight at baseline (N) | 2748 | 520 | 325 | 3593 | |
| Obese or severely obese at baseline (N) | 1427 | 422 | 186 | 2035 |
Notes: ADL difficulty was measured by difficulty in dressing, bathing or showing, eating, and getting in or out of bed without help.
The reference category for Racial/ethnic group is White.
Total number of participants in sample with onset of mobility difficulty between 1996 and 2006.
10-year onset rate = (number of participants with onset of mobility difficulty during follow-up) / (number of participants at baseline).
BMI = Body Mass Index; ADL = Activities of Daily Living; SD = Standard Deviation; COPD = Chronic Obstructive Pulmonary Disease.
p<0.05
p<0.01
p<0.001.
In both samples, the percentage of respondents in the normal weight range was significantly lower for Blacks (26.7%, 23.9%) and Hispanics (28.8%, 25.7%)than for Whites (39.8%, 36.4%). Correspondingly, Blacks (21.3%, 23.5%) and Hispanics(19.4%, 21.2%) had significantly higher prevalence of obesity than Whites (13.7%, 16.3%). Prevalence of severe obesity was higher in Blacks (7.1%, 10.6%), than in Whites (2.9%, 5.5%) and Hispanics (3.8%, 5.8%). Furthermore, Blacks (46.3%, 16.2%) and Hispanics (43.5%, 18.1%) were significantly more likely than Whites (34.9%, 7.6%) to report a mobility difficulty and ADL difficulty at baseline (data were not presented in tables). Among those respondents who reported having mobility difficulty or ADL difficulty at baseline, Blacks and Hispanics had higher prevalence of mobility difficulty, ADL difficulty, and obesity than Whites.
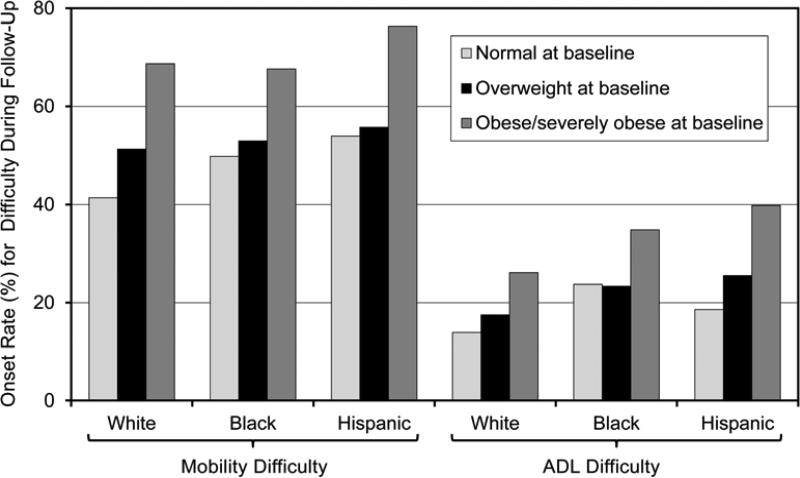
Figure 1 shows differences among racial/ethnic groups in onset of mobility and ADL difficulty over the 10-year study period for participants in three baseline BMI groups: normal weight, overweight, and obese/severely obese. Within all racial/ethnic groups, onset rates for mobility difficulty were somewhat higher for overweight participants, and much higher for obese/severely obese participants, than for those of normal weight. A similar pattern was seenfor the onset of ADL difficulty for White and Hispanic respondents. For Blacks, the onset rate was higher for obese/very obese participants, but not for overweight participants.
Figure 1.
Racial-Ethnic Differences in Effects of Baseline BMI on10-year Onset RatesforMobility Difficulty and ADL Difficulty.
Multivariate Analysis
Mobility Difficulty
Among White respondents, those who were overweight, obese, or severely obese at baseline were at increased risk of having mobility difficulty when compared to those of normal weight (Table 3).After controlling for covariates, Whites who were overweight, obese, and severely obese were, respectively 1.51, 2.18, and 2.77 times more likely to experience onset of mobility difficulty than those of normal weight.
Table 3.
Results of GEE Models for Onset of Mobility Difficulty and ADL Difficulty During 10 Years of Follow-up.
| Mobility Difficultya (N=5884) | ADL Difficultyb (N=8484) | |||
|---|---|---|---|---|
| Variable | Model 1c OR (95% CI) | Model 2d OR (95% CI) | Model 1c OR (95% CI) | Model 2d OR (95% CI) |
| Combined Groups of BMI Categories and Race/Ethnicity: | ||||
| Normal Weight (18.5 ≤ BMI < 25) | ||||
| Whitee | (Ref) | (Ref) | (Ref) | (Ref) |
| Black | 1.30(1.02-1.66)* | 1.35(1.06-1.72)* | 1.55(1.15-2.09)* | 1.46(1.08-1.98)** |
| Hispanic | 1.15(0.85-1.56) | 1.47(1.09-1.97)* | 1.16(0.76-1.76) | 1.67(1.11-2.51)** |
| Overweight (25 ≤ BMI < 30) | ||||
| White | 1.56(1.39-1.75)*** | 1.51(1.34-1.70)*** | 1.27(1.08-1.50)** | 1.10(0.93-1.30) |
| Black | 1.38(1.14-1.68)** | 1.39(1.14-1.69)** | 1.63(1.27-2.10)*** | 1.44(1.12-1.86)** |
| Hispanic | 1.27(1.01-1.60)* | 1.48(1.19-1.84)** | 1.33(0.99-1.77) | 1.55(1.17-2.05)** |
| Obese (30 ≤ BMI < 35) | ||||
| White | 2.37(2.05-2.74)*** | 2.18(1.88-2.53)*** | 1.66(1.37-2.01)*** | 1.14(0.93-1.39) |
| Black | 2.02(1.56-2.62)*** | 1.87(1.45-2.42)*** | 1.57(1.17-2.10)** | 1.27(0.93-.172) |
| Hispanic | 2.01(1.48-2.73)*** | 2.06(1.51-2.80)*** | 2.23(1.59-3.11)*** | 2.15(1.55-2.98)*** |
| Severely Obese (BMI ≥ 35) | ||||
| White | 3.29(2.60-4.18)*** | 2.77(2.14-3.56)*** | 3.03(2.40-3.84)*** | 1.75(1.36-2.25)*** |
| Black | 4.07(2.74-6.04)*** | 3.14(2.10-4.71)*** | 4.75(3.48-6.53)*** | 2.76(1.99-3.84)*** |
| Hispanic | 2.98(1.51-5.90)** | 2.96(1.57-5.60)*** | 3.40(1.83-6.32)*** | 2.79(1.54-5.06)*** |
| Socio-demographic Characteristics | ||||
| Age ≥ 65 years | 1.53(1.35-1.74)*** | 1.32(1.16-1.49)*** | 1.60(1.37-1.87)*** | 1.27(1.09-1.50)** |
| Female | 1.47(1.35-1.62)*** | 1.66(1.51-1.82)*** | 0.92(0.82-1.04) | 0.81(0.72-0.92)** |
| Education (years) | 0.93(0.92-0.95)*** | 0.94(0.93-0.96)*** | 0.92(0.91-0.94)*** | 0.95(0.93-0.97)*** |
| Married | NAf | NAf | 0.76(0.66-0.87)*** | 0.83(0.72-0.95)** |
| Health Behaviors | ||||
| Former Smoker | 1.15(1.05-1.27)** | 1.10(0.99-1.21) | 1.15(1.02-1.31) | 1.04(0.92-1.18) |
| Current Smoker | 1.12(0.99-1.27) | 1.19(1.05-1.35)* | 0.99(0.85-1.88) | 0.92(0.78-1.09) |
| Vigorous Physical Activity | 0.53(0.50-0.56)*** | 0.54(0.51-0.57)*** | 0.48(0.44-0.52)*** | 0.53(0.48-0.58)*** |
| Light/Moderate Drinking | 0.86(0.80-0.93)*** | 0.89(0.82-0.95)** | 0.68(0.61-0.75)*** | 0.75(0.68-0.84)*** |
| Heavy Drinking | 0.76(0.68-0.86)*** | 0.80(0.71-0.90)*** | 0.60(0.50-0.71)*** | 0.73(0.60-0.87)*** |
| Disease Severity Scores | ||||
| Hypertension | 1.10(1.05-1.14)*** | 1.05(0.99-1.11) | ||
| Diabetes | 1.23(1.17-1.30)*** | 1.23(1.16-1.30)*** | ||
| Lung Disease | 1.71(1.59-1.84)*** | 1.32(1.24-1.40)*** | ||
| Heart Disease | 1.31(1.25-1.38)*** | 1.14(1.09-1.20)*** | ||
| Stroke | 1.67(1.52-1.83)*** | 1.74(1.60-1.88)*** | ||
| Arthritis | 1.31(1.25-1.38)*** | 1.39(1.33-1.45)*** | ||
| Cancer | 1.45(1.33-1.57)*** | 1.32(1.20-1.46)*** | ||
| Mobility Difficulty at Baselineg | 2.12(1.87-2.39)*** | |||
| QICu | 27893 | 26135 | 19009 | 17176 |
Notes. Mobility difficulty was a composite measure of difficulty in walking several blocks, walking one block, climbing several flights of stairs, and climbing one floor of stairs. ADL difficulty was measured by difficulty in dressing, bathing or showing, eating, and getting in or out of bed without help.
Onset of mobility difficulty between 1996 and 2006.
Onset of ADL difficulty between 1996 and 2006.
Model 1: controlling for socio-demographic characteristics and health behaviors.
Model 2: controlling for socio-demographic characteristics, health behaviors, and disease severity.
White with normal weight is the reference group.
NA: Removed from Mobility Difficulty models because p value > 0.15.
Mobility Difficulty at Baseline was included only in ADL Difficulty Model 2.
GEE = Generalized Estimating Equations; ADL = Activities of Daily Living; BMI = Body Mass Index; OR = Odds Ratio; CI = Confidence Interval; QICu= Approximation of Quasilikelihood under the Independencemodel Criterion (QIC).
p<0.05
p<0.01
p<0.001.
Among Blacks, normal weight, overweight, obese and severely obese respondents were, respectively, 1.35, 1.39, 1.87, and 3.14 times more likely to experience onset of mobility difficulty than normal weight Whites.
Hispanics who were normal weight, overweight, obese, and severely obese were 1.47, 1.48, 2.06, and 2.96 times more likely to experience onset of mobility difficulty thannormal weight Whites.
ADL Difficulty
Whites who were severely obese were 1.75 times more likely to experience onset of ADL difficulty than Whites of normal weight. For Blacks, normal weight, overweight and severely obese respondents were 1.46, 1.44, and 2.76 times more likely to experience onset of ADL difficulty than normal weight Whites. Hispanics who were normal weight, overweight, obese or severely obesewere 1.67, 1.55, 2.15, and 2.79 times more likely to experience onset of ADL difficulty than normal weight Whites.
Racial/Ethnic Differences
Racial/ethnic differences in the impact of BMI on functional impairment within the same BMI category were tested in both Model 1and Model 2 (Table 4).Results summarized below are based on Model 2.
Table 4.
Racial/Ethnic Differences Within Each BMI Category in Risk of Onset of Mobility Difficulty and ADL Difficulty during 10 Years of Follow-up: Results from GEE Models.
| Combined Groups of BMI Categories and Race/Ethnicity | Mobility Difficultya (N=5884) | ADL Difficultyb (N=8484) | ||
|---|---|---|---|---|
| Model 1c OR (95% CI) | Model 2d OR (95% CI) | Model 1c OR (95% CI) | Model 2d OR (95% CI) | |
| Normal Weight (18.5 ≤ BMI < 25) at Baseline | ||||
| Black vs. White | 1.33(1.05-1.70)* | 1.35(1.06-1.73)* | 1.55(1.15-2.09)** | 1.46(1.08-1.98)* |
| Hispanic vs. White | 1.15(0.85-1.57) | 1.47(1.09-1.97)* | 1.16(0.76-1.76) | 1.66(1.11-2.51)* |
| Hispanic vs. Black | 0.87(0.60-1.25) | 1.08(0.76-1.55) | 0.75(0.46-1.20) | 1.14(0.71-1.84) |
| Overweight (25 ≤ BMI < 30) at Baseline | ||||
| Black vs. White | 0.90(0.75-1.09) | 0.93(0.77-1.12) | 1.28(1.01-1.63)* | 1.31(1.03-1.67)* |
| Hispanic vs. White | 0.82(0.66-1.02) | 0.98(0.80-1.21) | 1.04(0.78-1.38) | 1.41(1.07-1.85)* |
| Hispanic vs. Black | 0.91(0.70-1.18) | 1.06(0.82-1.37) | 0.81(0.58-1.13) | 1.07(0.78-1.48) |
| Obese (30 ≤ BMI < 35) at Baseline | ||||
| Black vs. White | 0.87(0.67-1.14) | 0.86(0.66-1.12) | 0.95(0.70-1.28) | 1.14(0.84-1.55) |
| Hispanic vs. White | 0.85(0.62-1.16) | 0.94(0.69-1.29) | 1.34(0.96-1.89) | 1.91(1.37-2.68)** |
| Hispanic vs. Black | 0.98(0.67-1.42) | 1.10(0.76-1.59) | 1.42(0.95-2.11) | 1.70(1.39-2.53)* |
| Severely Obese (BMI ≥ 35) at Baseline | ||||
| Black vs. White | 1.27(0.82-1.97) | 1.13(0.72-1.79) | 1.56(1.10-2.23)* | 1.58(1.09-2.28)* |
| Hispanic vs. White | 0.91(0.45-0.84) | 1.07(0.55-2.08) | 1.12(0.59-2.12) | 1.60(0.86-2.95) |
| Hispanic vs. Black | 0.72(0.33-1.55) | 0.94(0.45-1.97) | 0.72(0.37-1.40) | 1.01(0.53-1.94) |
Notes.
Onset of mobility difficulty between 1996 and 2006.
Onset of ADL difficulty between 1996 and 2006.
Model 1: controlling for socio-demograpbic characteristics and health behaviors.
Model 2: controlling for socio-demographic characteristics, health behaviors, and disease severity.
BMI = Body Mass Index; ADL = Activities of Daily Living.
p<0.05
p<0.01.
Among participants in the normal weight category at baseline,odds of developing mobility difficulty were significantly higher for both Blacks and Hispanics than for whites. . No significant racial/ethnic differences were found within any other BMI categories.
Among participants in the normal weight and overweight baseline BMI categories, risks of developing ADL difficulty were significantly higher for both Hispanics and Blacks than for Whites... Among those who were obese at baseline, Hispanics were significantly more likely to develop ADL difficulty than either Whites or Blacks. .Within the severely obese group, the odds for onset of ADL disability were higher for Blacks than for Whites.
DISCUSSION
Using the HRS, a nationally representative data, our study provides further evidence on the impact of both obesity and overweight on the onset of functional impairment in the mobility and ADL domains.11-13, 30-32 Compared with previous studies, our study used a longer follow-up time, and the findings suggest that high BMI may have a long-term effect on the development of functional impairment. More importantly, our study contributes to this body of literature by demonstrating that the long-term impact of obesity and overweight on the onset of functional impairment varies across racial/ethnic groups in the U.S. The racial/ethnic differences were more significant in domain of ADL difficulty than in mobility difficulty. Blacks and Hispanics, being more overweight and obese in middle age or early old age, were more likely to develop ADL difficulty over a 10-year follow-up than their White counterparts. Furthermore, obesity had more impact on the onset of ADL difficulty in Hispanics than in Blacks. However, with regard to onset of mobility difficulty, no significant differences were found across racial/ethnic groups. The findings that overweight and obesity had a more significant impact on the onset of functional impairment for Blacks than Whites were different from those of Wee et al12 which shows weaker impact for Blacks Differences between our findings and those of Wee et al. may partially be attributed to differences in length of follow-up (10 years in this study vs. two years in that of Wee et al.). In addition, different study populations are likely to be an important factor: most of the study population (87%) in our study was between the age of 50 and 64 years old. Blacks may be more likely to develop earlier onset of ADL difficulty than their White counterparts. Among Blacks, chronic diseases, rather than obesity, may have more significant impacts on the onset of function impairment in later life. Future research is warranted to further examine the racial/ethnic differences in impact of obesity on functional impairment among middle-aged and older adults. Our study found that Blacks and Hispanics are more likely to develop physical impairment than Whites for the same BMI. This result may partially be attributed to the different body fat composition across racial/ethnic groups. Previous studies have shown that in comparison to Whites, Blacks and Hispanics have a greater body fat and waist circumference for the same BMI. 33-34Presumably, abdominal fat may be more important than total obesity for disability in older adults.35-36 Our results showed that adjustment for disease severity attenuated the association between obesity and the onsets of functional limitations in both the mobility and ADL domains. The attenuation was stronger in ADL difficulty domain than in the mobility difficulty domain. After controlling for disease severity, the impact of obesity on development of functional impairment was reduced in severely obese participants for all racial/ethnic groups, although the association was still significant. The reason for this significant risk reduction can be partially explained by the higher prevalence of chronic diseases in severely obese American old adults. 37-38Our study also shows that all the chronic diseases included in the study had significant impact on onset of functional impairment. Given these chronic diseases are common among older adults (and particularly in those of minority race/ethnicity), in order to decrease the onset of functional impairment, a significant effort needs to be invested to reduce the development of chronic diseases.
Some recent research suggests obesity in older adults is not necessarily significantly associated with increased risk of mortality controlling for chronic diseases. Being slightly overweight might be associated with lower mortality risk, 39-40 particularly among White older adults. 41 The results from our competing risk analysis (data not shown) further demonstrated that both obesity and overweight were protective factors of mortality. Nonetheless, evidence suggests that obesity raises the risk of chronic diseases, and these diseases lead to an increased risk of mortality.42-44 Although overweight and obesity may be protective factors for mortality, each remains a risk factor for the onset of functional impairment. Studies suggest that weight control interventions, particularly when exercise is a component of the intervention, can improve muscle strength, pain symptoms, and overall physical functioning. 45 Thus, weight control is still a critical issue in relation to quality of life for middle-aged and older Americans.
This study is one of the few that have used longitudinal data to examine racial/ethnic differences paired with obesity and overweight as predictors of specific types of functional impairment. When interpreting these findings, certain limitations may merit further discussion. One limitation of this study is that the measurements of height and weight relied on self-reported data. However, previous studies have demonstrated the validity of self-reported weight and height, suggesting that self-reported and actual weight are correlated by more than 90%, even though respondents tend to overestimate their height and underestimate their weight.46-48 In addition, BMI does not indicate how weight is distributed over the body.31 Further, our GEE models relied on baseline BMI categories, thus, the models did not capture the effects of weight change over time on the development of functional impairment. Participant's BMI may change across different waves. However, our exploratory analysis suggests that changes in BMI in this community-dwelling sample of middle-aged and older Americans are more likely to involve transitions from lower to higher BMI categories. Meanwhile, dynamic measurements of disease scores and health behaviors over follow-up waves may also contribute to underestimation of obesity's impact. Therefore, use of baseline BMI categories in analysis may have underestimated the impact of obesity and overweight on the development of functional impairment. We found that baseline obesity increased risk of functional impairment, but weight change over the follow-up period may also have influenced the onset of functional impairment in this population. We are also aware that there are certain proxy biases. Interviews for 5.9% of 9,419 participants were obtained through their proxies. The percentage of proxy respondents varied from 4.0% to 7.7% in follow-up waves in both the ADL difficulty and mobility difficulty groups. Rates of onset for mobility and ADL difficulty were slightly higher (by about 1%) for proxy respondents than for respondents who were interviewed directly. Proxy respondents in all racial/ethnic groups were also more likely to be overweight and less likely to be obese than interviewed respondents. Data for proxy respondents may be somewhat less accurate, and could have introduced additional error into the models.
CONCLUSIONS
In conclusion, this study demonstrates that both overweight and obesity are risk factors for onset of functional impairment. We found racial/ethnic differences exist in the long-term impact of obesity on onset of functional impairment; we alsofound that compared to Whites, Blacks and Hispanics are more likely to develop functional impairment at the same BMI. This study provides empirical evidence that policy and prevention strategies should target not only people who are obese but also those who are overweight. Prevention efforts should promote weight control intervention in both groups. However, interventions that incorporate exercise as a component with a focus on improving muscle strength, balance, and flexibility could reduce functional impairment in all BMI categories, especially for Blacks and Hispanics who are at higher risk.
ACKNOWLEDGMENTS
The authors gratefully acknowledge the editorial assistance of Dr. Elizabeth Flint.
Funding source: National Institutes of Health/National Institute of Dental and Craniofacial Research (NIH/NIDCR: R01DE019110)
Sponsor's Role: None.
Footnotes
Author Contributions: Liang Wei contributed to the study design, data analysis and interpretation, and preparation of the manuscript. Dr. Wu contributed to the study concept, design, data interpretation and preparation of this manuscript.
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper. Both authors have an affiliation with Trend and Trajectories of Oral Health among Older Americans: The Role of Cognition.
REFERENCES
- 1.Flegal KM, Carroll MD, Kuczmarski RJ, et al. Overweight and obesity in the United States: prevalence and trends, 1960-1994. Int J Obes Relat Metab Disord. 1998;22:39–47. doi: 10.1038/sj.ijo.0800541. [DOI] [PubMed] [Google Scholar]
- 2.Hedley AA, Ogden CL, Johnson CL, et al. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999-2002. JAMA. 2004;291:2847–2850. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- 3.Kuczmarski RJ, Flegal KM, Campbell SM, et al. Increasing prevalence of overweight among US adults. The National Health and Nutrition Examination Surveys, 1960 to 1991. JAMA. 1994;272:205–211. doi: 10.1001/jama.272.3.205. [DOI] [PubMed] [Google Scholar]
- 4.Ogden CL, Carroll MD. [May 3 2012];Prevalence of Overweight, Obesity, and Extreme Obesity Among Adults: United States, Trends 1960-1962 Through 2007-2008(On-line) Available at www.cdc.gov/nchs/data/hestat/obesity_adult_07_08/obesity_adult_07_08.pdf.
- 5.Brault M. Americans with disabilities:2005, Current Population Reports. US Census Bureau; Washington, DC: 2008. [Google Scholar]
- 6.Foot DK, Lewis RP, Pearson TA, et al. Demographics and cardiology, 1950-2050. J Am Coll Cardiol. 2000;35:1067–1081. doi: 10.1016/s0735-1097(00)00561-1. [DOI] [PubMed] [Google Scholar]
- 7.A Fogel BS, Brock D, Goldscheider F, et al. Cognitive dysfunction and the need for long-term care: Implications for public policy (Public Policy Institute Report #9309) American Association for Retired Persons; Washington, DC: 1994. [Google Scholar]
- 8.Sternfeld B, Ngo L, Satariano WA, et al. Associations of body composition with physical performance and self-reported functional limitation in elderly men and women. Am J Epidemiol. 2002;156:110–121. doi: 10.1093/aje/kwf023. [DOI] [PubMed] [Google Scholar]
- 9.Friedmann JM, Elasy T, Jensen GL. The relationship between body mass index and self-reported functional limitation among older adults: A gender difference. J Am Geriatr Soc. 2001;49:398–403. doi: 10.1046/j.1532-5415.2001.49082.x. [DOI] [PubMed] [Google Scholar]
- 10.Clark DO, Mungai SM, Stump TE, et al. Prevalence and impact of risk factors for lower body difficulty among Mexican Americans, African Americans, and whites. J Gerontol A Biol Sci Med Sci. 1997;52:M97–M105. doi: 10.1093/gerona/52a.2.m97. [DOI] [PubMed] [Google Scholar]
- 11.Ferraro KF, Su YP, Gretebeck RJ, et al. Body mass index and disability in adulthood: A 20-year panel study. Am J Public Health. 2002;92:834–840. doi: 10.2105/ajph.92.5.834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wee CC, Huskey KW, Ngo LH, et al. Obesity, race, and risk for death or functional decline among Medicare beneficiaries: A cohort study. Ann Intern Med. 2011;154:645–655. doi: 10.7326/0003-4819-154-10-201105170-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dunlop DD, Song J, Manheim LM, et al. Racial/ethnic differences in the development of disability among older adults. Am J Public Health. 2007;97:2209–2215. doi: 10.2105/AJPH.2006.106047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mwachofi AK, Broyles R. Is minority status a more consistent predictor of disability than socioeconomic status? J Disabil Policy Stud. 2008;19:34–43. [Google Scholar]
- 15.Soldo BJ, Hurd MD, Rodgers WL, et al. Asset and Health Dynamics Among the Oldest Old: an overview of the AHEAD Study. J Gerontol B Psychol Sci Soc Sci. 1997:52. doi: 10.1093/geronb/52b.special_issue.1. Spec No:1-20. [DOI] [PubMed] [Google Scholar]
- 16.Guralnik JM, Ferrucci L, Simonsick EM, et al. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332:556–561. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Institutes of Health. Clinical Guidelines on the Identification Evaluation, and Treatment of Overweight and Obesity in Adults--The Evidence Report. Obes Res. 1998;6(Suppl 2):51S–209S. [PubMed] [Google Scholar]
- 18.Damush TM, Stump TE, Clark DO. Body-mass index and 4-year change in health-related quality of life. J Aging Health. 2002;14:195–210. doi: 10.1177/089826430201400202. [DOI] [PubMed] [Google Scholar]
- 19.Stuck AE, Walthert JM, Nikolaus T, et al. Risk factors for functional status decline in community-living elderly people: A systematic literature review. Soc Sci Med. 1999;48:445–469. doi: 10.1016/s0277-9536(98)00370-0. [DOI] [PubMed] [Google Scholar]
- 20.Clark DO. The effect of walking on lower body disability among older blacks and whites. Am J Public Health 1996. 1996;86:57–61. doi: 10.2105/ajph.86.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Seeman TE, Berkman LF, Charpentier PA, et al. Behavioral and psychosocial predictors of physical performance: MacArthur studies of successful aging. J Gerontol A Biol Sci Med Sci. 1995;1995;50:M177–M183. doi: 10.1093/gerona/50a.4.m177. [DOI] [PubMed] [Google Scholar]
- 22.House JS, Lepkowski JM, Kinney AM, et al. The social stratification of aging and health. J Health Soc Behav. 1994;35:213–234. [PubMed] [Google Scholar]
- 23.Liu X, Liang J, Muramatsu N, et al. Transitions in functional status and active life expectancy among older people in Japan. J Gerontol B Psychol Sci Soc Sci. 1995;50:S383–S394. doi: 10.1093/geronb/50b.6.s383. [DOI] [PubMed] [Google Scholar]
- 24.Maraldi C, Harris TB, Newman AB, et al. Health ABC study. Moderate alcohol intake and risk of functional decline: the Health, Aging, and Body Composition study. J Am Geriatr Soc. 2009;57:1767–1775. doi: 10.1111/j.1532-5415.2009.02479.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Williams GD, Debakey SF. Changes in levels of alcohol consumption: United States, 1983-1988. Br J Addict. 1992;87:643–648. doi: 10.1111/j.1360-0443.1992.tb01966.x. [DOI] [PubMed] [Google Scholar]
- 26.US Department of Health and Human Services (UDDHHS) 2008 Phyical Actitivity Guidelines for Americans. USDHSS; Washingston, DC: 2008. [Google Scholar]
- 27.Whitson HE, Hastings SN, Landerman LR, et al. Black-white disparity in disability: The role of medical conditions. J Am Geriatr Soc. 2011;59:844–850. doi: 10.1111/j.1532-5415.2011.03401.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ettinger WH, Davis MA, Neuhaus JM, et al. Long-term physical functioning in persons with knee osteoarthritis from NHANES. I: Effects of comorbid medical conditions. J Clin Epidemiol. Jul. 1994;47:809–815. doi: 10.1016/0895-4356(94)90178-3. [DOI] [PubMed] [Google Scholar]
- 29.Ferrucci L, Alley D. Obesity, disability, and mortality: A puzzling link. Arch Intern Med. 2007;167:750–751. doi: 10.1001/archinte.167.8.750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Launer LJ, Harris T, Rumpel C, et al. Body mass index, weight change, and risk of mobility disability in middle-aged and older women. The epidemiologic follow-up study of NHANES I. JAMA. 1994;271:1093–1098. [PubMed] [Google Scholar]
- 31.Jenkins KR. Obesity's effects on the onset of functional impairment among older adults. Gerontologist. 2004;44:206–216. doi: 10.1093/geront/44.2.206. [DOI] [PubMed] [Google Scholar]
- 32.He XZ, Baker DW. Body mass index, physical activity, and the risk of decline in overall health and physical functioning in late middle age. Am J Public Health. 2004;94:1567–1573. doi: 10.2105/ajph.94.9.1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Aleman Mateo H, Lee SY, Javed F, et al. Elderly Mexicans have less muscle and greater total and truncal fat compared to African-Americans and Caucasians with the same BMI. J Nutr Health Aging. 2009;13:919–923. doi: 10.1007/s12603-009-0252-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen H, Bermúdez OI, Tucker KL. Waist circumference and weight change are associated with disability among elderly Hispanics. J Gerontol A Biol Sci Med Sci. 2002;57:M19–25. doi: 10.1093/gerona/57.1.m19. [DOI] [PubMed] [Google Scholar]
- 35.Aloia JF, Vaswani A, Ma R, et al. Comparison of body composition in black and white premenopausal women. J Lab Clin Med. 1997;129:294–299. doi: 10.1016/s0022-2143(97)90177-3. [DOI] [PubMed] [Google Scholar]
- 36.Reid IR. Racial effects on body composition: it's not all black and white. J Lab Clin Med. 1997;129:281–282. doi: 10.1016/s0022-2143(97)90173-6. [DOI] [PubMed] [Google Scholar]
- 37.Vinciguerra F, Baratta R, Farina MG, et al. Very severely obese patients have a high prevalence of type 2 diabetes mellitus and cardiovascular disease. Acta Diabetol. 2013;50:443–449. doi: 10.1007/s00592-013-0460-3. [DOI] [PubMed] [Google Scholar]
- 38.Clark DO, Mungai SM. Distribution and association of chronic disease and mobility difficulty across four body mass index categories of African-American women. Am J Epidemiol. May 15. 1997;145:865–875. doi: 10.1093/oxfordjournals.aje.a009046. [DOI] [PubMed] [Google Scholar]
- 39.Thorpe RJ, Ferraro KF. Aging, obesity, and mortality: Misplaced concern about obese older people? Res Aging. 2004;26:108–129. doi: 10.1177/0164027503258738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dahl AK, Fauth EB, Ernsth-Bravell M, et al. Body mass index, change in body mass index, and survival in old and very old persons. J Am Geriatr Soc. 2013;61:512–518. doi: 10.1111/jgs.12158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Adams KF, Schatzkin A, Harris TB, et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med. 2006;355:763–778. doi: 10.1056/NEJMoa055643. [DOI] [PubMed] [Google Scholar]
- 42.Calle EE, Thun MJ, Petrelli JM, et al. Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med. 1999;341:1097–1105. doi: 10.1056/NEJM199910073411501. [DOI] [PubMed] [Google Scholar]
- 43.Must A, Spadano J, Coakley EH, et al. The disease burden associated with overweight and obesity. JAMA. 1999;282:1523–1529. doi: 10.1001/jama.282.16.1523. [DOI] [PubMed] [Google Scholar]
- 44.Prospective Studies Collaboration. Whitlock G, Lewington S, Sherliker P, et al. Body-mass index and cause-specific mortality in 900 000 adults: Collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083–1096. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shea MK, Houston DK, Nicklas BJ, et al. The effect of randomization to weight loss on total mortality in older overweight and obese adults: The ADAPT Study. J Gerontol A Biol Sci Med Sci. 2010;65:519–525. doi: 10.1093/gerona/glp217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jeffrey R. Bias in reported body weight as a function of education, occupation, health and weight concern. Addict Behav. 1996;21:217–222. doi: 10.1016/0306-4603(95)00050-x. [DOI] [PubMed] [Google Scholar]
- 47.Stunkard AJ, Albaum JM. The accuracy of self-reported weights. Am J Clin Nutr. 1981;34:1593–1599. doi: 10.1093/ajcn/34.8.1593. [DOI] [PubMed] [Google Scholar]
- 48.Boutier V, Payette H. Validity of weight and height given from memory in an elderly population. Age Nutr. 1994;5:17–21. [Google Scholar]