Abstract
The purpose of this study was to evaluate long-term outcome, following microfracture of the knee in a large patient group, using a random-effect model for longitudinal data analysis. There were 350 subjects (males, 55%; females, 65%) who underwent knee microfracture by a single surgeon between 1992 and 2002. Mean age was 48 years (range, 12-76 years). Subjective questionnaires were collected from patients at 1 year postsurgery and each consecutive year thereafter. Of treated chondral lesions, 53% were traumatic lesions, and 47% were degenerative. Average initial follow-up was 4 years (range, 1-12 years). Outcome variables included Lysholm score and Tegner activity scale. Analysis showed that Lysholm score improved during the first 2 years following microfracture. After 2 years, the score remained steady with a slight decline but remained above preoperative level through the study period. There was no significant difference in the improvement of outcome over time between men and women (P > 0.05). There was no significant difference in improvement of outcome over time between degenerative and traumatic chondral lesions (P > 0.05). Subjects with traumatic lesions demonstrated a significant difference in trajectory of Lysholm scores over time by age (≤45 years, >45 years) (P = 0.04). This study showed that there was no difference in improvement in outcome following microfracture between men and women or between degenerative and traumatic chondral lesions. However, there were age-dependent differences in the improvement in outcome over time.
Keywords: microfracture, cartilage repair, knee, articular cartilage, outcome measures
Introduction
Injury to the articular cartilage of the knee is a common component of sports-related knee injuries. Chondral lesions of the knee are particularly difficult to manage due to the fact that cartilage has an inherently poor capacity to heal itself.1,2 Most mammalian tissues demonstrate a predictable response to injury, which involves an inflammatory response followed by a complex reparative process.3 However, because articular cartilage has no direct blood supply, the cellular mediators necessary to carry out the healing process are absent.1-3 As a result, these cartilage lesions demonstrate little to no inherent healing over time.1-3 If left untreated, these cartilage injuries progress over time and may result in chronic knee pain, stiffness, and swelling.1
Several surgical treatment options exist to address these cartilage injuries.1,4 The microfracture technique is an arthroscopic surgical intervention that harnesses the body’s inherent healing capacity.5,6 There is a paucity of literature regarding long-term clinical outcomes following the microfracture procedure.5-11 Studies have shown that age, lesion size, time from injury to surgery, and body mass index are associated with outcomes following microfracture.5-11 Few studies have documented how these factors affect how a patient’s improvement changes over time.
The purpose of this study was to evaluate long-term outcomes following the microfracture procedure in treating full-thickness cartilage lesions of the knee in a large sample using random-effect models for longitudinal data analysis.
Methods
There were 350 patients (229 males, 121 females) who underwent the microfracture procedure by a single surgeon between 1992 and 2002. Mean age was 47.6 years (range, 12.1-76.3 years). Subjective questionnaires were collected from patients at 1 year postsurgery and each consecutive year thereafter. Questionnaires included the Lysholm score and Tegner activity scale. All data were collected prospectively and stored in a database. Exclusion criteria were patients who underwent concomitant ligament surgery or meniscus surgery.
Data Analysis
Data were analyzed with a random-effect model for longitudinal analysis (SAS 9.1 software; SAS Institute Inc., Cary, NC). Outcomes variables included the Lysholm score12,13 and the Tegner activity scale.12,14 Independent variables included gender, age at time of index surgery, etiology of the chondral defect (degenerative v. traumatic), and number of years since index surgery. A traumatic lesion was defined as time from onset to surgery less than 6 months and no sclerotic bone at arthroscopy. A lesion with sclerotic observed at arthroscopy was degenerative.
Exploratory Data Analysis
The distributions of each of the study’s variables were assessed. As the distribution for Lysholm scores in this study population was left skewed, a squared transformation was carried out on this variable prior to analysis. A 2-tailed t-test was carried out to evaluate for any baseline differences in Lysholm or Tegner scores between males and females and between subjects with traumatic and degenerative lesions.
Profile plots of the outcomes variables over time were created for each independent variable. Due to apparent nonlinearity of the profile plots, it was determined that a “summary measure” analysis would not be appropriate for these data. Instead, a random-effect model was selected for analysis of the primary research questions. The study’s sample size (n = 350) allows for the application of this model, the strength of which includes the ability to evaluate both continuous and categorical variables as well as the ability to decompose the variance if desired. The random-effect model also provides the ability to assess variation between subjects at baseline as well as over time.
Fitting the Model/Checking the Fit of the Model
The appearance of the profile plots suggests a quadratic component to the distribution of the outcomes variables over time. Thus, for each analysis, a “reduced” model containing a time-factor interaction was compared with a “full” model that contained an additional time2-factor element. When appropriate, analyses were controlled for age. The fit of the model was then determined by comparing the −2 log-likelihood values of the models with a χ2 test. The model that was determined to demonstrate the best fit was then applied to hypothesis testing.
Results
There were 185 (53%) knees with traumatic chondral lesions and 165 (47%) knees with degenerative chondral lesions in this population. There were 220 lesions in the medial compartment, 122 lesions in the lateral compartment, and 101 lesions in the patellofemoral compartment. The average size of the lesion was 362 mm2 (range, 6-2800 mm2). Mean initial follow-up was 4 years (range, 1-12 years). Minimum 10-year follow-up was available in 195 patients, and minimum 5-year follow-up was available in 315 patients.
At the time of surgery, patients with degenerative lesions were significantly older than those with traumatic lesions (mean age, 53.2 v. 40.9 years; 95% confidence interval [CI], −14.83 to −9.575; P < 0.0001). At baseline, there was a significant difference in Lysholm score for gender but not in the Tegner score. There was no difference in baseline outcomes scores between subjects with degenerative versus traumatic lesions (Table 1).
Table 1.
Baseline Values
No significant difference in Lysholm score was seen between males and females over the time period (P = 0.88) (Table 2). Although the graph (Fig. 1) shows an apparent trend favoring the outcomes of males over females after 1 year, there is no significant difference in the trajectory of the plots. The graph also shows continued improvement 2 years following surgical intervention.
Table 2.
Time Trajectory for Outcome Variables
| Outcome Variable | Interaction Term | t Value | df | P Value |
|---|---|---|---|---|
| Lysholm | Years-squared*gender | 0.14 | 1,547 | 0.88 |
| Tegner | Years-squared*gender | 0.01 | 835 | 0.99 |
| Lysholm | Years-squared*degenerative | 0.98 | 1,520 | 0.328 |
| Tegner | Years-squared*degenerative | 1.1 | 834 | 0.271 |
Figure 1.
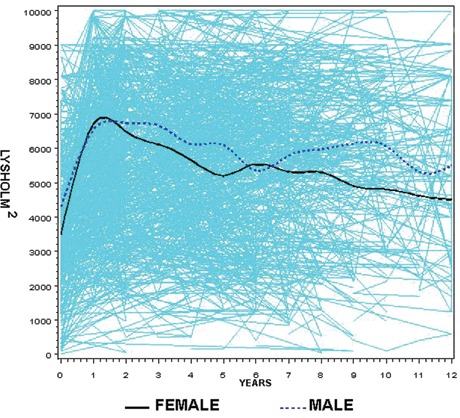
Profile plots of Lysholm scores2 over time by gender. The model for the time trajectory for the Lysholm score between males and females (gender: male = 1, female = 0) was as follows: Lysholm-squared = 4954 + 435 (years since surgery) − 45 (years-squared) + 408 (gender) − 10.6 (years*gender) + 1.3 (years-squared*gender).
There was also no significant difference in Lysholm score between degenerative and traumatic lesions over the time period (P = 0.33) (Table 2). The graph shows an apparent trend favoring the outcomes of traumatic over degenerative lesions between years 1 and 7; however, there is no significant difference in the trajectory of the plots (P > 0.05) (Fig. 2).
Figure 2.
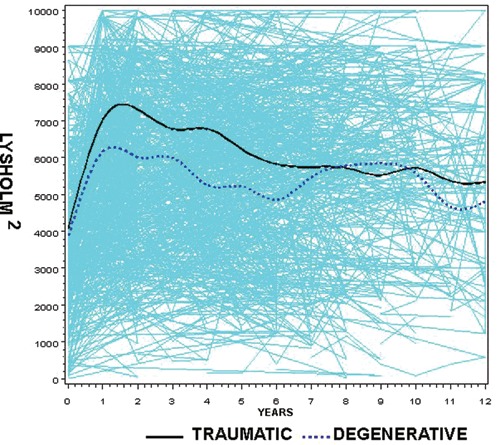
Profile plots of Lysholm scores over time by lesion type. A repeated measures analysis using a random-effect model adjusted for age revealed the following model (degenerative: djd = 1; traumatic: djd = 0): Lysholm-squared = 5539 − 3.4 (age at surgery) + 456 (years since surgery) − 47 (years-squared) − 333 (djd) − 85.6 (years*djd) + 8.8 (years-squared*djd).
No significant difference in Tegner activity scale was seen between males and females over the time period (P = 0.99) (Table 2). The graph (Fig. 3) shows Tegner scores improving for males over females; however, this was not significant (P > 0.05). These results do not significantly change when the model is adjusted for age.
Figure 3.
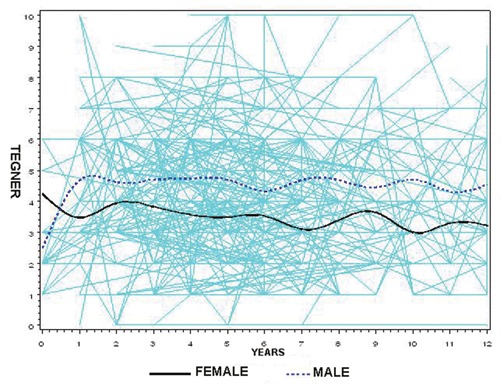
Profile plots of Tegner scores over time by age. The model for the time trajectory for the Tegner activity scale between males and females (gender: male = 1, female = 0) was as follows: Tegner = 3.73 − 0.001 (years since surgery) − 0.002 (years-squared) + 0.7 (gender) + 0.035 (years*gender) + 0.0006 (years-squared*gender).
There was also no significant difference in Tegner activity scale between degenerative and traumatic lesions over the time period (P = 0.27) (Table 2). The graph (Fig. 4) shows higher Tegner scores in traumatic lesions; however, there is no significant difference in the trajectory of the plots (P > 0.05).
Figure 4.
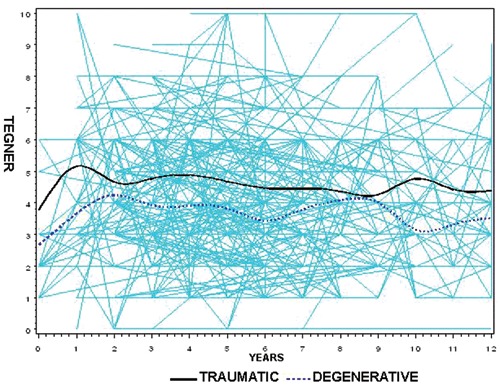
Profile plots of Tegner scores over time by lesion type. A repeated measures analysis using a random-effect model adjusted for age revealed the following model (degenerative: djd = 1; traumatic: djd = 0): Tegner = 6.0 − 0.03 (age at surgery) − 0.04 (years since surgery) + 0.002 (years-squared) − 0.539 (djd) + 0.123 (years*djd) − 0.011 (years-squared*djd).
For the purpose of this analysis, subjects were divided into 2 age groups, “young” (≤45 years of age) and “old” (>45 years of age). When subjects with degenerative lesions and subjects with traumatic lesions were analyzed together, there was no significant difference in the trajectory of either the Lysholm or Tegner scores over time by age group. Subjects with traumatic lesions demonstrated a significant difference in Lysholm scores when divided into the 2 age groups, with the younger group showing more improvement over time (P = 0.04). The following model supports this finding: (for age at surgery ≤45, age at surgery = 0; for age at surgery >45, age at surgery = 1) Lysholm2 = 5194 + 607 (years since surgery) − 58.2 (years since surgery squared) + 598 (age at surgery) − 336 (years since surgery* age at surgery) + 24.5 (years since surgery squared*age at surgery).
Discussion
In this longitudinal data analysis of the microfracture procedure in a large sample size, we have demonstrated that the improvement in Lysholm score over time is not different between males and females. There was also no significant difference in Lysholm score between patients with degenerative and traumatic chondral lesions after microfracture. Patients with traumatic lesions and patients with degenerative lesions showed a significant improvement in Lysholm scores when compared preoperatively to postoperatively in this study. The Tegner activity scale did not discriminate any significant differences in any of the analyses carried out in this study. The only difference noted was that younger patients with traumatic defects do better over time.
Previously published data by Miller et al. support our findings, showing no significant difference in Lysholm improvement by gender for degenerative chondral lesions of the knee.5 In 2003, Steadman et al. reported on independent predictors of outcomes after microfracture of traumatic chondral defects.6 Results showed that gender was not an independent predictor of Lysholm score.6 Our study showed that there was no difference in outcome over time between degenerative and traumatic; however, previous studies suggest that patients with traumatic lesions have a higher baseline Lysholm score than patients with degenerative lesions.5,6 These findings may be helpful to the surgeon in counseling patients who might be candidates for the microfracture procedure. Patients can be shown how outcome improves over the first 2 years, as has been seen in other studies, and the improvement levels off over the next several years. This was seen in traumatic and degenerative lesions, so the patient with the degenerative lesion can see several years of improved outcome over their preoperative function.
We identified age-dependent differences in the surgical outcomes over time. Specifically, subjects with traumatic lesions demonstrated a significant difference in the trajectory of Lysholm scores over time by age group. These data support the findings of Steadman et al., where age was found as an independent predictor of Lysholm scores in patients with traumatic chondral defects.6 Patients <35 years old showed a mean Lysholm improvement of 32 points, while patients aged 35 to 45 years old only showed a mean Lysholm improvement of 26 points.6 Also, patients greater than 45 years old showed decreased outcomes when compared to younger patients. Kreuz et al. demonstrated similar results, showing that patients under 40 years old had significantly better results according to the International Cartilage Repair Society (ICRS) score and the Cincinnati score.9 Although Mithoefer et al. did not show a significant difference in function between older and younger patients, which may have been due to a low patient population, there was a trend toward better scores on the activities of daily living scale for patients who were less than 30 years old at the time of microfracture.11
As expected, subjects with degenerative lesions were on average older at baseline than those with traumatic lesions. This finding likely reflects the natural history of degenerative disease of the knee as well as different physical activity patterns in these age groups. In addition, at the time of treatment, males reported significantly higher Lysholm scores than females. This finding was also supported by Miller et al., showing a mean difference in Lysholm score of 10 points between males and females.5
One of the values of applying random-effect models is the ability to assess variation between subjects at baseline as well as intersubject and intrasubject variation over time. Although we have not addressed the issue of variation in this study, further analyses could be carried out to investigate this area.
The Tegner activity scale is widely reported in the orthopedic literature as an outcomes measure for various conditions of the knee.7,12,14 In studies validating the score for meniscus injuries and anterior cruciate ligament (ACL) injuries, the score shows adequate responsiveness; however, the level of change is not of the same magnitude as seen in scores of 0 to 100. On a 0- to 10-point scale, this scale may not show enough change to evaluate a large group of mixed patients over long periods. Furthermore, although model fitting suggested a quadratic element to the Tegner curves, the curves look grossly “flat,” and the relationships, given the plots, change very little over time.
While the Tegner score profiles remain relatively flat over time, the profiles of the Lysholm score demonstrate a consistent pattern. There is an apparent steep increase in the Lysholm score over the first 1 to 2 years followed by a slow decline over time. This decrease in Lysholm scores over time was previously published. Mithoefer et al. showed a decrease in knee function after 2 years; however, overall postoperative function remained improved.10 Steadman et al. suggest that deterioration in knee function may be due to inadequate cartilage fill at second-look arthroscopy.12 Our data showed that at the latest follow-up points, Lysholm scores appear to remain above the preoperative baseline scores.
Overall, this study showed that the improvement in Lysholm score is not different by gender or type of lesion. However, if patients are grouped by age over 45 years and under, then the Lysholm score was better for younger patients with traumatic lesions.
Footnotes
One or more of the authors has received research funding from Smith & Nephew, Arthrex, Ossur, and/or Siemens.
The authors received no financial support for the research and/or authorship of this article.
References
- 1. Alford JW, Cole BJ. Basic science update: cartilage restoration, part 1. Am J Sports Med. 2005;33:295-306. [DOI] [PubMed] [Google Scholar]
- 2. Mankin HJ. The response of articular cartilage to mechanical injury. J Bone Joint Surg Am. 1982;64:460-5. [PubMed] [Google Scholar]
- 3. Suh J, Scherping S, Mardi T, Steadman JR, Woo SL. Basic science of articular cartilage injury and repair. Operat Tech Sports Med. 1995;3:78-86. [Google Scholar]
- 4. Knutsen G, Drogset JO, Engebretsen L, Grøntvedt T, Isaksen V, Ludvigsen TC, et al. A randomized trial comparing autologous chondrocyte implantation with microfracture: findings at five years. J Bone Joint Surg Am. 2007;89:2105-12. [DOI] [PubMed] [Google Scholar]
- 5. Miller BS, Steadman JR, Briggs KK, Rodrigo JJ, Rodkey WG. Patient satisfaction and outcome after microfracture of the degenerative knee. J Knee Surg. 2004;17:13-7. [DOI] [PubMed] [Google Scholar]
- 6. Steadman JR, Briggs KK, Rodrigo JJ, Kocher MS, Gill TJ, Rodkey WG. Outcomes of microfracture for traumatic chondral defects of the knee: average 11-year follow-up. Arthroscopy. 2003;19:477-84. [DOI] [PubMed] [Google Scholar]
- 7. Gobbi A, Nunag P, Malinowski K. Treatment of full thickness chondral lesions of the knee with microfracture in a group of athletes. Knee Surg Sports Traumatol Arthrosc. 2005; 13:213-21. [DOI] [PubMed] [Google Scholar]
- 8. Knutsen G, Engebretsen L, Ludvigsen TC, Drogset JO, Grøntvedt T, Solheim E, et al. Autologous chondrocyte implantation compared with microfracture in the knee: a randomized trial. J Bone Joint Surg Am. 2004;86:455-64. [DOI] [PubMed] [Google Scholar]
- 9. Kreuz PC, Erggelet C, Steinwachs MR, Krause SJ, Lahm A, Niemeyer P, et al. Is microfracture of chondral defects in the knee associated with different results in patients aged 40 years or younger? Arthroscopy. 2006;22:1180-6. [DOI] [PubMed] [Google Scholar]
- 10. Mithoefer K, McAdams T, Williams RJ, Kreuz PC, Mandelbaum BR. Clinical efficacy of the microfracture technique for articular cartilage repair in the knee: an evidence-based systematic analysis. Am J Sports Med. 2009;37:2053-63. [DOI] [PubMed] [Google Scholar]
- 11. Mithoefer K, Williams RJ, Warren RF, Potter HG, Spock CR, Jones EC, et al. The microfracture technique for the treatment of articular cartilage lesions in the knee: a prospective cohort study. J Bone Joint Surg Am. 2005;87:1911-20. [DOI] [PubMed] [Google Scholar]
- 12. Kocher MS, Steadman JR, Briggs KK, Sterett WI, Hawkins RJ. Reliability, validity, and responsiveness of the Lysholm knee scale for various chondral disorders of the knee. J Bone Joint Surg Am. 2004;86:1139-45. [DOI] [PubMed] [Google Scholar]
- 13. Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10:150-4. [DOI] [PubMed] [Google Scholar]
- 14. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43-9. [PubMed] [Google Scholar]


