Abstract
Microfracture is frequently used for articular cartilage repair in athletes. This study aimed to define the strength and weaknesses of this minimally invasive cartilage repair technique in the athletic population in an effort to optimize indications, functional outcome, and athletic participation after microfracture in the athlete’s knee. A systematic analysis of original studies using microfracture in athletes was performed. Functional outcome was assessed by activity outcome scores, ability to return to sports participation, timing of the return to sport, level of postoperative sports activity, and continuation of athletic competition over time. Thirteen studies describing 821 athletes were included in the analysis with an average follow-up of 42 months. Good or excellent results were reported in 67% of athletes with normal International Knee Documentation Committee (IKDC) scores in 80% and significant increase of Lysholm scores, Tegner activity scores, and Knee injury and Osteoarthritis Outcome Score (KOOS) sports subscales. Return to sports was achieved in 66% at an average of 8 months after surgery, with return to competition at the preinjury level in 67%. Forty-nine percent of athletes continued to compete without change in level of play, while decreasing function was observed in 42% after 2 to 5 years. Athlete’s age, preoperative duration of symptoms, level of play, lesion size, and repair tissue morphology affected sports activity after microfracture. Microfracture improves knee function and frequently allows for return to sports at the preinjury level, but deterioration of athletic function occurs in some patients. Several independent factors were identified that can help to optimize the return to athletic competition after microfracture in the athlete’s knee.
Keywords: sport, athletics, cartilage, microfracture, injury, repair
Introduction
Sports-related articular cartilage injuries of the knee have been reported with increasing frequency.1-4 Injuries to the articular cartilage surface of the knee in the athlete frequently result in association with other acute injuries such as ligament or meniscal injuries, traumatic patellar dislocations, and osteochondral injuries. Articular cartilage defects of the femoral condyles have been observed in up to 50% of athletes undergoing anterior cruciate ligament reconstruction with an increased propensity in female athletes.4,5 Besides acute injury, articular cartilage defects can develop in the high-impact athletic population from chronic pathological joint-loading patterns such as joint instability or axis deviation.5 Irrespective of their origin, articular cartilage injuries in athletes will frequently limit athletic abilities, prevent athletes’ continued participation in their sport, and predispose them to progressive joint degeneration with up to a 12-fold increased risk for knee osteoarthritis documented in high-impact athletes.6-8 In a long-term study of 28 Swedish athletes with isolated severe chondral damage in the weightbearing condyles, 75% of athletes returned to their sport initially, but a significant decline of athletic activity was observed 14 years after the initial injury.3 In addition, high-impact joint loading, as is characteristic of high intensity exercise, has been shown to decrease cartilage protoglycan content, increase levels of degradative enzymes, and cause chondrocyte apoptosis.9,10 These facts demonstrate the need for an effective and durable joint-surface restoration in high-impact athletes that can withstand the significant joint stresses generated during athletic participation and facilitate a physically active lifestyle, thus reducing the risk for serious medical conditions such as heart disease, diabetes, and hypertension.
Microfracture has been shown to be the preferred method for articular cartilage defect repair in professional and recreational athletes including high-impact sports such as basketball, American football, soccer, and rugby.11-14 By systematic penetration of the subchondral bone plate, microfracture leads to formation of a blood clot that contains pluripotent, marrow-derived mesenchymal stem cells, which develops into a fibrocartilage repair tissue with varying amounts of type II collagen content.15-17 Previous reports have pointed out the detrimental effect of excessive loading on articular cartilage repair following marrow stimulating techniques.18 Despite its frequent use in the high-impact athletic population, limited information is still available on the results of microfracture chondroplasty under the significant mechanical demands associated with high-impact sports. We therefore systematically investigated the efficacy of microfracture for articular cartilage repair in the athlete’s knee by combining knee function and activity scores, postoperative return to sport at the preoperative level, and ability for continued sports participation and analyzed the factors that affect the athlete’s ability to return to sports participation after microfracture chondroplasty.
Methods
A comprehensive search of the English literature was performed to identify any published and unpublished clinical studies on microfracture in athletes using MEDLINE, MEDLINE preprints, EMBASE, CINAHL, Life Science Citations, and the British National Library of Health including the Cochrane Central Register of Controlled Trials (CENTRAL) medical electronic databases. The search period was from January 1, 1966 to October 31, 2009. The medical databases were searched using the terms “sport,” “athlete,” “return to sport,” “athletic activity,” “chondral defect,” “condylar lesion,” “condyle lesion,” “patellofemoral lesion,” “trochlear defect,” “knee lesion,” “joint surface defect,” “articular resurfacing,” “articular cartilage repair,” “chondroplasty,” “microfracture,” and “marrow stimulating technique.” In addition, searches were also performed in the bibliographies of identified studies, review articles on articular cartilage repair in athletes, and abstract books of relevant scientific meetings. Any study reporting clinical information on microfracture in the athletic polulation was selected for primary review. Specific attention was placed on identifying studies that described sports activity–related functional outcome scores, the postoperative ability to return to sport after microfracture, and the continued participation in athletic activity over time.
We identified 38 clinical studies reporting on microfracture and athletics. The abstracts of these studies were evaluated in a primary screening process, and only studies reporting on International Cartilage Repair Society (ICRS) grade III or IV chondral or osteochondral defects of the knee (femoral condyle, tibia, and patellofemoral) were included. Studies including individual cartilage repair procedures or comparing surgical techniques were accepted. Because cartilage injuries in athletes frequently occur in association with other injuries, studies with or without concomitant injuries and/or procedures were included in this review. All prospective randomized controlled studies (level I and II) on microfracture of the knee in athletes were included. Level III and IV studies were accepted into the study only if they provided postoperative follow-up data of 2 years or more. Studies providing macroscopic or histological data obtained at second-look arthroscopy more than 12 months after surgery were also included.
Fourteen studies met these primary inclusion criteria and were carefully analyzed in a secondary screening process. After secondary review, one study was excluded because it contained fewer than 20 study subjects. The modified Coleman Methodology Scores (CMSs) and subscales were determined to assess the methodological quality of each of the included studies.19,20 Furthermore, data on study characteristics and design, level of evidence, demographics, cartilage defect characteristics, surgical technique, concomitant procedures, and clinical follow-up were systematically analyzed. Information describing measures of sports participation such as activity scores, rate of return to sport, time and level of return, and continuation of sports participation at the preinjury level was collected. The Lysholm-Gillquist score, Tegner activity scale, Knee injury and Osteoarthritis Outcome Score (KOOS), and International Knee Documentation Committee (IKDC) scores were included as outcome measures because they have been specifically evaluated for articular cartilage repair in the knee or include specific sport activity information.21,22 In addition, macroscopic and histological data of the repair cartilage in athletes were collected when available from the reviewed studies.
The collected data were analyzed using established statistical software (SPSS version 17.0, SPSS, Chicago, IL). Differences between independent parameters were evaluated using the Kruskal-Wallis test. Relationships between variables were tested using the Pearson coefficient of correlation (r). Differences between variable proportions were measured by χ2 analysis. Differences were considered significant with a P value < 0.05. Data are presented as mean ± standard error of the mean (SEM).
Results
Thirteen studies describing 821 (range, 24-236) patients were included in the review with an average follow-up of 40 ± 5 months (range, 18-72 months). Mean number of study subjects was 63 ± 16 (range, 24-236). Defect size averaged 3.1 ± 0.4 cm2 (range, 2.2-4.9 cm2). Mean duration of symptoms before surgery was 26 ± 8 months (range, 1-48 months). Single articular cartilage lesions were treated in 70% of studies, and multiple lesions were present in 30%. Only 6 studies included isolated defects of the femoral condyle, and 7 studies included athletes treated for articular cartilage defects in the patellofemoral and/or tibiofemoral compartments. One third of the studies included patients with concomitant ligament or meniscal procedures. Seven studies reported on microfracture alone, while 6 studies compared microfracture to other cartilage repair techniques12-16,23-30 (Table 1). Five studies were randomized controlled studies, 7 were prospective cohort studies or case series, and 1 study was a retrospective case series. Level-of-evidence rating showed 4 level I, 2 level II, 1 level III, and 6 level IV studies. The average CMS was 67 ± 6 (range, 29-100 points) (Fig. 1).
Table 1.
Study Demographics
| n | |
|---|---|
| Patients | 821 |
| Age, y | 31 ± 2 |
| Follow-up, mo | 40 ± 5 |
| Lesion type, % | |
| Single only | 70 |
| Single and multiple | 30 |
| Traumatic only | 75 |
| Traumatic and degenerative | 25 |
| Lesion location, % | |
| Femorotibial only | 46 |
| Femorotibial and patellofemoral | 54 |
| Lesion size, cm2 | 3.1 ± 0.3 |
| Duration of symptoms, mo | 26 ± 6 |
| Concomitant procedures, % | 46 |
Figure 1.
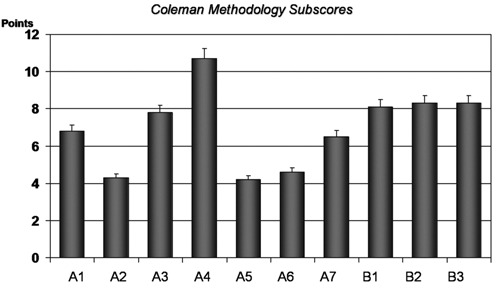
Total Coleman Methodology Scores and Subscores for studies on microfracture in athletes: A1 (study size), A2 (follow-up), A3 (concomitant surgical procedures), A4 (study design), A5 (diagnostic certainty), A6 (surgical technique), A7 (rehabilitation), B1 (outcome criteria), B2 (procedure of outcome assessment), B3 (patient selection process).
Good and excellent results were reported in 67% ± 7% after microfracture. Postoperative Lysholm scores after microfracture in athletes averaged 89 ± 3 points. An increase in Tegner activity scores of observed in 76% ± 4% of all patients after microfracture, with an average postoperative Tegner score of 5.4 ± 0.3 points. KOOS subscales for sports and recreation significantly increased between 19 to 21 points following microfracture chondroplasty.27,29,30 IKDC scores were normal or nearly normal in 80% ± 10% after microfracture in athletes. Following the initial significant improvement after microfracture, decreasing activity scores were observed in 5 studies (42%) and occurred in 47% to 80% of athletes. The score decrease was observed between 24 to 60 months postoperatively; however, the decreased activity scores were still higher than the preoperative scores.
Return to sports participation was achieved successfully in 66% ± 6% (range, 44%-100%) after microfracture. No statistical correlation was observed between the rate of return to sport and level of evidence or CMS. Time to return to sports averaged 8 ± 1 months (range, 2-16 months) after microfracture. Return to sport at the preinjury level was possible in 67% ± 5% of athletes (range, 50%-100%), with continued sports participation at the preinjury level in 49% ± 9% (range, 18%-71%) at 2 to 5 years after microfracture. Several factors were found to influence the ability to return to sports after articular cartilage repair in the knee (Table 2). Sixty-five percent of athletes younger than 40 years of age returned to sports after microfracture compared to 20% of older patients (P < 0.05).14 The preoperative interval also significantly affected the ability to return to sport. Athletes who were symptomatic less than 1 year before microfracture returned to sports in 67% compared to 14% (P < 0.01) if preoperative intervals exceeded 12 months.14 Lesion size of <2 cm2 was associated with a significantly higher rate of return to sports than larger lesions after microfracture (P < 0.05).14,25 Significantly better results were demonstrated in chondral compared to osteochondral defects after microfracture (P < 0.01).24,25 Worse clinical outcome and less consistent return to sports were observed with defects of the central aspect medial femoral condyle after microfracture (P < 0.05).24 The average number of prior surgeries was lower in athletes who returned to sports participation after microfracture.14 Eighty-six percent of athletes undergoing microfracture as a first-line procedure were able to return to sport compared to 33% with prior surgeries (P < 0.01).14 Return to sports was significantly better in high-level, competitive athletes (71%) than recreational athletes (29%) after microfracture (P < 0.01). While high return rates to preinjury level of competition were reported in professional athletes, performance levels were found to be below preinjury levels during the initial seasons after returning to professional-level athletics.12,23,28 Simultaneous adjuvant procedures such as reconstruction of the anterior cruciate ligament were associated with better results when performed with microfracture.15
Table 2.
Factors Affecting Return to Sport after Microfracture
| Factor | Associated with Better Return to Sport |
|---|---|
| Age | Age <40 years |
| Preoperative interval | Duration <12 months |
| Athletic skill level | Competitive athletes |
| Defect size | Size <2 cm2 |
| Defect location | Lateral femoral condyle |
| Defect type | Chondral defects |
| Number of prior surgeries | Primary microfracture |
| Adjuvant procedures | Simultaneous surgery |
| Repair tissue morphology | Better cartilage morphology |
Information on macroscopic and microscopic appearance of the cartilage repair tissue in athletes was available in only 5 studies after microfracture.13,15,16,24,25 Macroscopic evaluation showed normal or nearly normal repair tissue morphology in 45% after microfracture. While all athletes with normal or nearly normal morphology were able to return to preinjury activity levels, only 36% of athletes with abnormal repair tissue morphology were able to return (P < 0.001). Limited fill grade with exposed subchondral bone was observed more frequently in recreational athletes (35%) compared to competitive athletes (8%; P < 0.05) after microfracture.15 Histological evaluation showed predominantly hybrid tissue (fibrous and hyaline) after microfracture without association between histological tissue quality and return to sport in the reviewed studies.13,15,16,24,25 Postoperative magnetic resonance imaging (MRI) demonstrated 49% to 87% good/excellent repair, 18% complete fill, surface congruency in 52%, and subchondral cysts in 33% (Fig. 2).13 No significant technique-specific complications were reported for microfracture in athletes.
Figure 2.
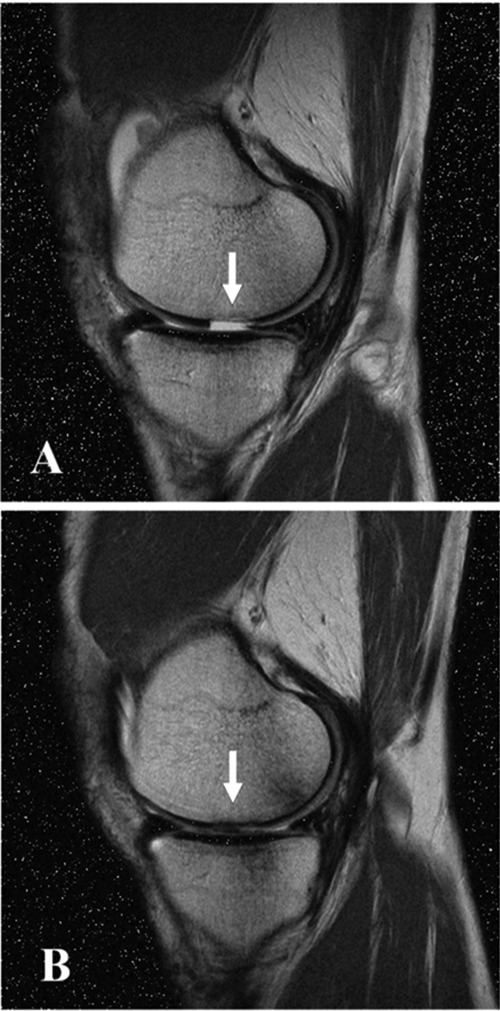
Preoperative (A) and postoperative (B) magnetic resonance images demonstrating successful articular cartilage repair in an athlete who returned to high-impact sports 8 months after microfracture.
Discussion
While the ability to return to sports participation often presents a critical aspect of functional outcome for an injured athlete, little systematic information is available on the return to athletic activities after microfracture. However, the ability to return to sports is routinely discussed during the therapeutic counseling of the athlete with articular cartilage injury. Detailed analysis of return to sport after microfracture therefore provides important information for the perioperative management of the athlete and his postoperative expectations. To address the lack of specific information of this important aspect of functional outcome in the athletic population, we systematically reviewed 12 predominantly prospective studies with more than 750 patients and compiled comprehensive information on sports participation after microfracture in the athlete. Average CMSs in this review were significantly higher than CMS scores for cartilage repair studies reported previously, attesting to the quality of the included studies.20 High CMS subscores for study type, outcome criteria, and outcome assessment further underscore the methodological quality of the results of our study, which provides comprehensive, valuable information on the efficacy of articular cartilage repair with microfracture in the athlete’s knee.
Our review revealed a high percentage of good and excellent ratings, increased KOOS subscores for sports and recreation, good postoperative Lysholm scores, and improved Tegner activity scores, confirming that microfracture improves activity levels even under high mechanical demands in the athletic population. Following the initial improvement, a decrease in activity scores was noted in several studies 2 to 3 years after microfracture.14,16,24-26 Despite the observed average score decrease, activity and functional outcome remained improved compared to preoperative function scores in most athletes. The reasons for the observed functional decline after microfracture are not completely understood. Deterioration of knee function occurred primarily in athletes with poor repair cartilage morphology and fill after microfracture.15 This is consistent with the critical role previously observed for repair cartilage volume on durability of postoperative improvement after microfracture.31 However, decreasing knee function was also observed in some patients with good repair tissue volume, and other factors must be considered. Limited peripheral integration of the repair cartilage tissue may contribute to the decreasing activity scores observed after microfracture because it increases vertical shear stresses between repair and native cartilage and promotes cartilage degeneration.31
Relative thinning of the overlying repair cartilage tissue by subchondral bone overgrowth after microfracture chondroplasty may be another potential factor involved in the observed functional deterioration in high-impact athletes.31 The functional decrease observed after microfracture in some athletes certainly requires further systematic study to improve the understanding of which athletes will benefit most from microfracture and which athletes may be better candidates for other primary cartilage repair techniques. Defining the optimal indications for primary cartilage repair with microfracture is important because recent data suggest that prior marrow stimulation may negatively affect the outcome of subsequent secondary cartilage repair procedures.32 Evidence-based selection of cartilage repair techniques that take into consideration the individual athlete’s demands and circumstances provides a promising approach to optimizing the ability to return to unrestricted and durable sports participation after cartilage repair.
Our study confirms that microfracture can successfully return athletes with knee articular cartilage defects to demanding, high-impact sports participation. The average return rate of 66% (range, 50%-100%) after microfracture is similar to the return rate of 71% (range, 53%-81%) after anterior cruciate ligament reconstruction and 74% (range, 56%-85%) after meniscal repair.33,34 The observed variability of the reported return rates within the individual studies has also been observed for the other sports medicine procedures and can be attributed to mixed patient populations and demographics and variable cartilage defect characteristics. Considering the high mechanical demands placed on the repaired cartilage defects in high-level, competitive athletes, the better than average return rate in competitive athletes is encouraging. However, recent data in professional basketball players suggest that some performance parameters may still be decreased at the time of the initial return to competition.12,23 Similar performance limitations have been observed after anterior cruciate ligament reconstruction in professional athletes and may result from incomplete recovery of sport-specific fitness, quadriceps inhibition, pain, joint effusion, and altered joint proprioception that is still present at the initial return to high-impact sports.35,36 The reasons why athletes return to sports and continue participation are certainly complex, and further study is needed to systematically evaluate the influence of clinical and nonclinical factors on sports participation after articular cartilage repair with microfracture.
Time to return to sport was short after microfracture and similar to recovery times seen after anterior cruciate ligament reconstruction. Second-generation microfracture techniques using growth factor or matrix augmentation may be able to accelerate postoperative rehabilitation and shorten the time to return to sports participation after microfracture.37
The observed decrease of sports activity scores after initial functional improvement following microfracture in some patients has been attributed to the limited repair tissue quality and variable fill volume following marrow stimulation.15,28 Socioeconomic and psychological factors, such as the fear for reinjury, have been shown to affect return to sport after anterior cruciate ligament reconstruction and may also contribute to the observed reduction of activity in athletes after microfracture.38 Our systematic review was able to identify several factors that affect the return to sports participation after articular cartilage repair in the athlete’s knee with microfracture. The athlete’s age significantly affected sports participation after microfracture, with better results with patients younger than 40 years. Age-dependent qualitative and quantitative differences in metabolic activity and repair cartilage synthesis offer a biologic explanation for this effect, but other factors such as a slower overall recovery and increasing socioeconomic demands in older patients have also been suggested.39,40 Prolonged preoperative intervals also had a significant influence on the return to sports after microfracture, with a 5-fold increased return rate if surgery was performed within 12 months after cartilage injury.14 Our data suggest that untreated cartilage injury may create an unfavorable environment for later cartilage repair from microfracture, resulting in inferior macroscopic repair cartilage quality.15 This factor and prolonged absence from athletic activity may explain the decreased rate of sports participation after delayed articular cartilage repair in the knee with microfracture. This is also consistent with the better results found in athletes who received no prior surgical intervention before microfracture.14 Our results emphasize the critical importance of early surgical intervention for articular cartilage injury in the athlete’s knee for the successful return to sports participation. Better return to sport was observed for high-level athletes after microfracture. Earlier diagnosis, shorter preoperative intervals, younger age, higher motivation to return to sport, better repair cartilage fill, and improved access to rehabilitation may explain the increased return rates in high-level competitive athletes, while changing social demands and avoidance of additional injuries may have contributed to the lower return rate observed in recreational athletes.14,15
Lesion characteristics also influenced the return to sports activity. Defect size <2 cm2 was associated with a significantly higher rate of return to high-impact athletics after microfracture,14,24,25 and better outcomes were observed for chondral defects compared to osteochondral defects. This is not surprising because microfracture is indicated primarily for small cartilage defects. It appears that filling of smaller, well-shouldered cartilage defects even with nonhyaline repair tissue still improves function, while the histological repair tissue quality becomes more important for larger defects.27,31 The size threshold in athletes at 2 cm2 is smaller than the threshold of 4 cm2 reported for the general population treated with microfracture, reflecting the increased demands on the cartilage repair in the demanding athletic population.31,41
Knee articular cartilage defects in the athlete are frequently associated with other pathological knee conditions. While addressing the combined pathology is critical for the success of the cartilage repair procedure, little information exists on whether the adjuvant procedures affect the ability to return to sport after microfracture. Our review showed that concomitant procedures improved the outcome after microfracture in athletes and suggests that treatment of the concomitant pathology should be performed simultaneously with articular cartilage repair to optimize the athlete’s return to sport.15 A limitation of this conclusion is that concomitant pathology may have been more closely associated with patient impairment than the defect itself that was treated with microfracture. However, addressing associated pathologies in a single stage may minimize the negative effects of prolonged rehabilitation and extended absence from competition. Besides the advantage for the athlete, the 1-stage approach provides a significant cost benefit by avoiding a second surgical intervention and associated rehabilitation.
In conclusion, articular cartilage repair in the athlete’s knee with microfracture provides a high rate of return to sport comparable to that of other common sports medicine procedures. Athletes are often able to return to sports participation at the preinjury level, even at the highest competitive level. Younger, competitive players with small defect size, short duration of symptoms, fewer prior surgical interventions, and better repair cartilage morphology have a higher rate of return to sports after microfracture. Further investigation is warranted to improve our understanding of why a subgroup of athletes fail to return to sport or show decreasing knee function and activity levels after initial improvement. Preoperative identification of these athletes will help to optimize the indications, functional outcome, and ability for continued participation in demanding athletics after microfracture.
Footnotes
The authors declared no potential conflicts of interest with respect to the authorship and/or publication of this article.
The authors received no financial support for the research and/or authorship of this article.
References
- 1. Curl WW, Krome J, Gordon ES, Rushing J, Smith BP, Poehling GG. Cartilage injuries: a review of 31,516 knee arthroscopies. Arthroscopy. 1997;13:456-60. [DOI] [PubMed] [Google Scholar]
- 2. Levy AS, Lohnes J, Sculley S, LeCroy M, Garrett W. Chondral delamination of the knee in soccer players. Am J Sports Med. 1996;24:634-9. [DOI] [PubMed] [Google Scholar]
- 3. Maletius W, Messner K. The long-term prognosis for severe damage to the weightbearing cartilage in the knee: a 14-year clinical and radiographic follow-up in 28 young athletes. Acta Orthop Scand. 1996;67:165-8. [DOI] [PubMed] [Google Scholar]
- 4. Piasecki DD, Spindler KP, Warren TA, Andrish JT, Parker RD. Intraarticular injuries associated with anterior cruciate ligament tear: findings at ligament reconstruction in high school and recreational athletes. Am J Sports Med. 2003;31:601-5. [DOI] [PubMed] [Google Scholar]
- 5. Mandelbaum RB, Browne JE, Fu F, Micheli L, Mosely BJ, Erggelet C, et al. Articular cartilage lesions in the knee. Am J Sports Med. 1998;26:853-61. [DOI] [PubMed] [Google Scholar]
- 6. Drawer S, Fuller CW. Propensity for osteoarthritis and lower limb joint pain in retired professional soccer players. Br J Sports Med. 2001;35:402-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Felson DT. Osteoarthritis: new insights. Part 1: the disease and its risk factors. Ann Intern Med. 2000;133:635-46. [DOI] [PubMed] [Google Scholar]
- 8. Kujala UM, Kettunen J, Paananen H, Aalto T, Battie MC, Impivaara O, et al. Knee osteoarthritis in former runners, soccer players, weight lifters, and shooters. Arth Rheum. 1995;38:539-46. [DOI] [PubMed] [Google Scholar]
- 9. Lohmander LS, Roos H, Dahlberg L, Hoerrner LA, Lark MW. Temporal patterns of stromelysin, tissue inhibitor and proteoglycan fragments in synovial fluid after injury to the knee criciate ligament or meniscus. J Orthop Res. 1994;12:21-8. [DOI] [PubMed] [Google Scholar]
- 10. Vrahas MS, Mithoefer K, Joseph D. Long-term effects of articular impaction. Clin Orthop Rel Res. 2004;423:40-3. [DOI] [PubMed] [Google Scholar]
- 11. Brophy RH, Rodeo SA, Barnes RP, Powell JW, Warren RF. Knee articular cartilage injuries in the National Football League: epidemiology and treatment approach by team physicians. J Knee Surg. 2009;22(4):331-8. [DOI] [PubMed] [Google Scholar]
- 12. Namdari S, Baldwin K, Anakwenze O, Park MJ, Huffman GR, Sennett BJ. Results and performance after microfracture in national association basketball. Am J Sports Med. 2009;37:943-8. [DOI] [PubMed] [Google Scholar]
- 13. Riyami M, Rolf C. Evaluation of microfracture of traumatic chondral injuries to the knee in professional football and rugby players. J Orthop Surg Res. 2009;4:13-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mithoefer K, Williams RJ, Warren RF, Wickiewicz TL, Marx RG. High-impact athletics after knee articular cartilage repair: a prospective evaluation of the microfracture technique. Am J Sports Med. 2006;34:1413-8. [DOI] [PubMed] [Google Scholar]
- 15. Blevins FT, Steadman JR, Rodrigo JJ, Silliman J. Treatment of articular cartilage defects in athletes: an analysis of functional outcome and lesion appearance. Orthopedics. 1998;21:761-7. [DOI] [PubMed] [Google Scholar]
- 16. Gobbi A, Nunag P, Malinowski K. Treatment of chondral lesions of the knee with microfracture in a group of athletes. Knee Surg Sports Traumatol Arthrosc. 2004;13:213-21. [DOI] [PubMed] [Google Scholar]
- 17. Mithoefer K, Steadman JR. The microfracture technique. Tech Knee Surg. 2006;5(3):140-8. [Google Scholar]
- 18. Buckwalter JA. Evaluating methods for restoring cartilaginous articular surfaces. Clin Orthop. 1999;367S:S224-38. [DOI] [PubMed] [Google Scholar]
- 19. Coleman BD, Khan KM, Mafulli N, Cook JL, Wark JD. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Scand J Med Sci Sports. 2000;10:2-11. [DOI] [PubMed] [Google Scholar]
- 20. Jakobsen RB, Engebretsen L, Slauterbeck JR. An analysis of the quality of cartilage repair studies. J Bone Joint Surg Am. 2005;87(10):2232-9. [DOI] [PubMed] [Google Scholar]
- 21. Hambly K, Griva K. IKDC or KOOS? Which measures symptoms and disabilities most important to postoperative articular cartilage repair patients? Am J Sports Med. 2008;36:1695-704. [DOI] [PubMed] [Google Scholar]
- 22. Kocher MS, Steadman JR, Briggs KK, Sterret WI, Hawkins RJ. Reliability, validity, and responsiveness of the Lysholm knee rating scale for various chondral disorders of the knee. J Bone Joint Surg. 2004;86:1139-45. [DOI] [PubMed] [Google Scholar]
- 23. Cerynik DL, Lewullis GE, Joves BC, Palmer MP, Tom JA. Outcomes of microfracture in professional basketball players. Knee Surg Sports Traumatol Arthroscop. 2009;17:232-9. [DOI] [PubMed] [Google Scholar]
- 24. Gudas R, Kalesinskas RJ, Kimtys V, Stankevivius E, Toliusis V, Bernotavicius G, et al. A prospective randomized clinical study of mosaic osteochondral autologous transplantation versus microfracture for the treatment of osteochondral defects in the knee joint in young athletes. Arthroscopy. 2005;2:1066-75. [DOI] [PubMed] [Google Scholar]
- 25. Gudas R, Stankevicius E, Monastyreckiene E, Pranys D, Kalesinkas RJ. Osteochondral autologous transplantation versus microfracture for the treatment of articular cartilage defects in the knee joint in athletes. Knee Surg Traumatol Arthrosc. 2006;14:834-42. [DOI] [PubMed] [Google Scholar]
- 26. Kon E, Gobbi A, Filardo G, Delcogliano M, Zaffagini S, Marcacci M. Arthroscopic second-generation autologous chondrocyte implantation compared with microfracture for chondral lesions of the knee: prospective nonrandomized study at 5 years. Am J Sports Med. 2009;37:33-41. [DOI] [PubMed] [Google Scholar]
- 27. Saris DBF, Vanlauwe J, Victor J, Almquist KF, Verdonk R, Bellemans J, et al. Treatment of symptomatic cartilage defects of the knee: characterized chondrocyte implantation results in better clinical outcome at 36 months in a randomized trial compared to microfracture. Am J Sports Med. 2009;37(Suppl 1):10S-9S. [DOI] [PubMed] [Google Scholar]
- 28. Steadman JR, Miller BS, Karas SG. The microfracture technique in the treatment of full-thickness chondral lesions of the knee in National Football League players. J Knee Surg. 2003;16:83-6. [PubMed] [Google Scholar]
- 29. Van Assche D, Inklaar M, Saris DB, Vanlauwe J, Staes F, Luyten FP. Sports participation and patient perspective after cartilage repair of the knee: a comparison between characterized chondrocyte implantation and microfracture. Results after three years. Proceedings of the 8th World Congress of the International Cartilage Repair Society; 2009 May 23-26; Miami, FL. [Google Scholar]
- 30. Van Asche D, Van Caspel D, Vanlauwe J, Bellemans J, Saris DB, Luyten FP, et al. Physical activity levels after characterized chondrocyte implantation versus microfracture in the knee and the relationship to objective functional outcome with 2-year follow-up. Am J Sports Med. 2009;37(Suppl 1):42S-9S. [DOI] [PubMed] [Google Scholar]
- 31. Mithoefer K, Williams RJ, Warren RF, Potter HG, Spock CR, Jones EC, et al. The microfracture technique for the treatment of articular cartilage lesions in the knee: a prospective cohort study. J Bone Joint Surg Am. 2005;87:1911-20. [DOI] [PubMed] [Google Scholar]
- 32. Minas T, Gomoll AH, Rosenberger R, Royce RO, Bryant T. Increased failure rate of autologous chondrocyte implantation after previous treatment with marrow stimulation techniques. Am J Sports Med. 2009;37:902-8. [DOI] [PubMed] [Google Scholar]
- 33. Cascio BM, Culp L, Cosragea AJ. Return to play after anterior cruciate ligament reconstruction. Clin Sports Med. 2004;23:395-408. [DOI] [PubMed] [Google Scholar]
- 34. McCarty EC, Marx RG, Wickiewicz TL. Meniscal tears in the athlete: operative and nonoperative management. Phys Ther Rehabil Clin North Am. 2000;11:867-80. [PubMed] [Google Scholar]
- 35. Carey JL, Huffman GR, Parakh SG, Sennett BJ. Outcomes of anterior cruciate ligament injuries to running backs and wide receivers in the National Football League. Am J Sports Med. 2006;34:1911-7. [DOI] [PubMed] [Google Scholar]
- 36. Palmeri-Smith RM, Kreinbrink J, Ashton Miller JA, Wojtys EM. Quadriceps inhibition induced by an experimental knee joint effusion affects knee joint mechanics during single drop landing. Am J Sports Med. 2007;35:1269-75. [DOI] [PubMed] [Google Scholar]
- 37. Mithoefer K, McAdams TR, Scopp J, Mandelbaum BR. Emerging options for treatment of articular cartilage injury in the athlete. Clin Sports Med. 2009;28:25-40. [DOI] [PubMed] [Google Scholar]
- 38. Gobbi A, Frabcisco R. Factors affecting return to sports after anterior cruciate ligament reconstruction with patellar tendon and hamstring graft: a prospective clinical investigation. Knee Surg Sports Traumatol Arthroscop. 2006;14:1021-8. [DOI] [PubMed] [Google Scholar]
- 39. Tew S, Redman S, Kwan A, Walker E, Khan I, Dowthwaite G, et al. Differences in repair responses between immature and mature cartilage. Clin Orthop Relat Res. 2001;391(Suppl):S142-52. [DOI] [PubMed] [Google Scholar]
- 40. Wei X, Messner K. Age- and injury-dependent concentrations of transforming growth factor-beta 1 and proteoglycan fragments in rabbit knee joint fluid. Osteoarthritis Cartilage. 1998;6:10-8. [DOI] [PubMed] [Google Scholar]
- 41. Knutsen G, Engebretsen L, Ludvigsen TC, Drogset JO, Grontvedt T, Solheim E. Autologous chondrocyte implantation compared with microfracture in the knee. J Bone Joint Surg Am. 2004;86:455-64. [DOI] [PubMed] [Google Scholar]


