Abstract
Objective. To evaluate the accuracy of arthroscopic measurement of full-thickness (International Cartilage Repair Society grades 3-4) cartilage lesions of the knee. Design. In 33 consecutive arthroscopically evaluated cartilage lesion knees the lesion size was routinely estimated. At the final treatment, a knee arthrotomy was performed, and the lesion was reestimated. The 2 estimates were then compared by paired t test and the area estimated by knee arthrotomy was used as the gold standard. Results. The mean area of the cartilage lesion estimated by arthroscopic surgery was 3.5 cm2 (standard deviation [SD] = 1.7) whereas in the open surgery the mean area was 3.2 cm2 (SD = 1.5). The mean difference was 0.3 cm2, indicating a tendency toward overestimation by the arthroscopic evaluation, but the difference was not significant (P = 0.09). Additional MRI assessment of the area demonstrated a mean area of 2.3 cm2 (SD = 1.6). This underestimated the size of the lesion by 1.2 cm2 (SD = 0.8; P = 0.015). Conclusion. Knee arthroscopic examination estimated a cartilage full-thickness lesion with an error of less than 25 % in the majority of the patients.
Keywords: cartilage lesion, knee, size
Introduction
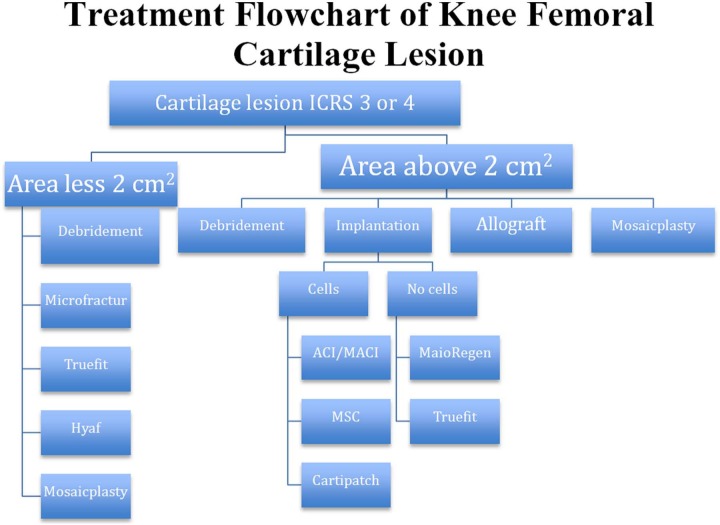
The choice of method for repairing cartilage lesions is based on several factors concerning the patient. Both the depth and the size of the cartilage lesion are important. Several grading systems of the cartilage lesion exist and full-thickness (International Cartilage Repair Society grades 3-4) cartilage lesions are common.1,2 The measured area of the cartilage lesion is an important guideline for the treatment option offered to the patient as illustrated in Figure 1.3 Authors have claimed the arthroscopic mapping to be unreliable due to overestimation as a result of the magnification in the arthroscope.4 However, the clinical verification of this statement is barely focused in the literature. The arthroscopic evaluation of the area of the cartilage injury is frequently used in clinical studies as basis for inclusion and treatment.5-7 Even though some kind of error can be accepted, problem arises when the error of measurement affect a commonly used treatment algorithm as adapted from prior publications and outlined in Figure 1.1,3,8 There is evidence that a large lesion would benefit from cartilage repair surgery as cell transplantation,9 though more debated are those lesions approximating 2 cm2. The current study tests the hypothesis that in clinical practice, the size of a cartilage lesion in the knee could be estimated accurately by arthroscopic evaluation compared to open assessment. This agreement is crucial, as the size of the cartilage lesion in many instances defines the treatment option available.
Figure 1.
Proposed treatment algorithm for handling a cartilage lesion. Before treatment is initiated, the presence of correctable knee pathology as malalignment, ligament injury, or patellafemoral instability needs to be corrected.
Method and Material
The estimation of the area of the cartilage lesions in the current study was performed arthroscopically with the patient in a supine position and with thigh tourniquet and total intravenous anaesthesia. This study only included patients with focal full-thickness femoral or patella cartilage lesions. This corresponds to those patients who most commonly are candidates for cartilage repair surgery. Prior to surgery all knees were evaluated by a standard MRI protocol for evaluating knee problems in a clinical practice, and the area of the cartilage lesions estimated by MRI is shown in Table 1. The patients were referred to the clinic as part of the inclusion in ongoing clinical trials on cartilage repair. Thirty-three consecutive patients were included. All were arthroscopically evaluated and subsequently treated with open surgery. The treatment was either implantation of cultured cells under coverage or implantation of bioengineering scaffolds to heal the cartilage lesion or refixation of a chondral fracture. Treatment preferred as the final treatment by arthrotomy is documented in Figure 2. The measurement made by the open surgery was considered as the golden standard in assessing the area of the cartilage lesion (Fig. 3). The mean age was 36 years (range = 11-59 years) and mean Lysholm score was 45 (standard deviation [SD] = 18) as illustrated in Table 2. A standard 4-mm arthroscopic probe was used to measure the area of the cartilage lesion as the longest anteroposterior distance and the width of the cartilage lesion. The area was reestimated by knee arthrotomy, which was carried out 2 to 4 weeks later when implantations of chondrocytes or mesenchymal stem cells were used. This was performed after stabilization of the edges of the cartilage lesion to represent the area that would need surgical treatment. Three experienced knee surgeons in cartilage repair surgery evaluated the patients in the current study and the arthroscopic measurements were documented before the arthrotomy was performed for the final measurement. A difference between the arthroscopic and arthrotomy measurement of more than 0.6 cm2 is considered clinically relevant, since this can affect the decision about which treatment to prefer and this would be of particular importance for the lesion in the area of 2 cm2. This difference of interest is based on a previous study,10 which demonstrated that a cartilage lesion has to be larger than 8 mm in diameter before stress can be observed at the rim of the lesion. Cartilage lesions do have irregular forms in the clinic and to estimate the size of the lesion as the product of the anteroposterior length and the width of the lesion could therefore introduce some overestimation. However, this error could be judged as a fixed error and would not affect the measured values neither in arthroscopic assessment nor by arthrotomy.
Table 1.
Area of Cartilage Lesion Assessed by the Different Modalities.
| Area in cm2 (SD) | P (Paired Student’s t Test)a | Mean Area Estimation Errora | |
|---|---|---|---|
| Arthrotomy | 3.5 (1.7) | ||
| Arthroscopy | 3.2 (1.5) | 0.091 | 24% |
| MRI | 2.3 (1.7) | 0.015 | 41% |
Area measured by arthrotomy used as reference.
Figure 2.
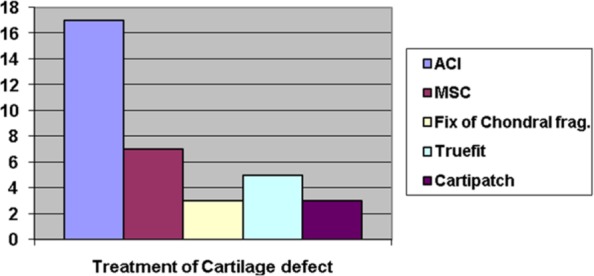
Treatment used in the current study groups.
Note: ACI = autologous chondrocyte implantation, MSC = mesenchymal stem cell implantation.
Figure 3.
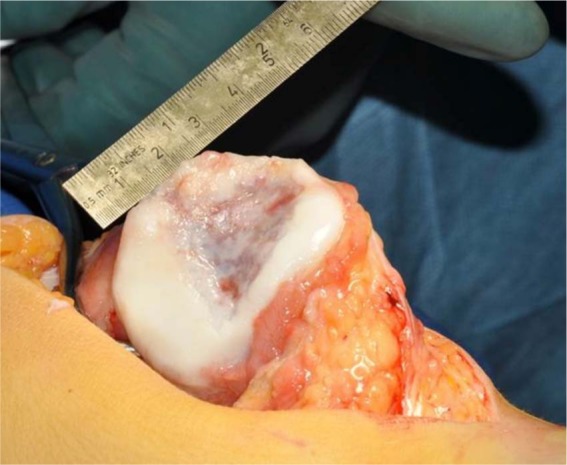
Assessment of the area at open surgery for a chondral fracture of the articular cartilage of patella.
Table 2.
Patients Demographics of the 33 Consecutive Patients Reported.
| Age in years; mean (SD) | 36 (12) |
| Area of lesion in cm2 at arthrotomy; mean (SD) | 3.2 (1.5) |
| Lysholm score; mean (SD) | 45 (18) |
| Microfracture before cartilage repair surgery, n | 5 |
| Female:male ratio | 11:22 |
The preoperative MRIs were used as additional information to the operative procedure. The regional ethical committee approved the study protocols and the study was performed according to the Helsinki Declaration.
Statistics
A power analysis with the current sample size using 0.05 as the significance revealed a power of 0.88 for testing the current hypothesis in the study. A paired Student’s t test was used to test the hypothesis of less than 0.6 cm2 systematic biases between the 2 assessments. To evaluate how well the arthroscopic assessment was likely to agree with the assessment performed during open surgery for an individual, we also calculated the 95% limits of agreement for the difference between the measurements.11 The differences between the 2 assessments were plotted against the average, as recommended by Bland and Altman.11
Results
The mean area of the cartilage lesion in arthroscopic surgery was 3.5 cm2 (SD = 1.7) and in the open surgery the mean area was 3.2 cm2 (SD = 1.5) with a P value of 0.09 between these 2 assessments of the area. All the mean area measurements are listed in Table 1 and the correlation coefficient between the measurements was 0.8. MRI measurements are presented in Table 1 as additional information to the surgical findings. The MRI assessment of the area in this study demonstrated a mean area of 2.3 cm2 (SD = 1.6) using a standard knee protocol. The mean difference between arthrotomy area and MRI area was 1.2 cm2 (SD = 0.8) with P = 0.015.
The mean absolute difference between the arthroscopy and the arthrotomy measurement of area was 0.8 cm2, which corresponds to a mean error in estimation of the area of the lesion of 24%. An error of less than 25% was found in 20 of 33 patients and the 95% limits of agreement for the arthroscopic assessment were from −47% to 70% of the arthrotomy assessment. Figure 4 illustrates the agreement of the measurements for all 33 patients.
Figure 4.
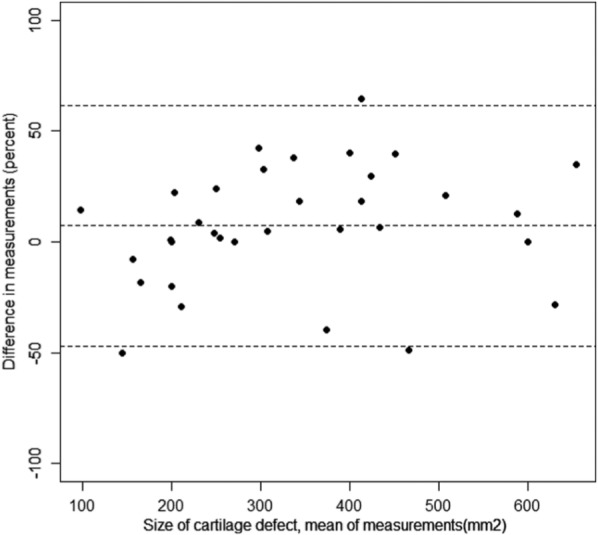
Bland–Altman plot of the differences.
Furthermore, the 95% limits of agreement for the MRI assessment of the area were −149% to 71% of the arthrotomy assessment. Additionally, it was noted that 2 of the cartilage lesions were missed at the preoperative MRI examination.
Discussion
The main finding in the current study is that assessment of the size of a full-thickness cartilage lesion located on the femoral condyle or patella by knee arthroscopy had a mean error of 24% compared with the assessment of the lesion performed during arthrotomy. Additionally, the findings demonstrated that the error was less than 25% in 63% of the cases, which seems to be an acceptable range if a difference of measurements of 0.6 cm2 is accepted. Clinically, the estimation of the lesion is considered to be reasonable to make preference for the treatment according to the methodological practice in the majority of the clinical trials reported. However, there is still a need for more precise quantification of the lesion with specific cartilage protocols for those patients subjected to cartilage surgery preoperatively. Standard MRI knee protocols as demonstrated in the current study clearly underestimated the size of the cartilage lesion and exact preoperative planning in cartilage repair surgery require a cartilage specific cartilage MRI protocol. Consequently, new clinical trials should report how the size of the lesion was assessed and this is especially important when an arthroscopic technique are is used in comparison with a technique using an arthrotomy, as this might cause differences in the area estimated of up to 24%.6,12
Another strength of this study is the clinical setting although this make it more difficult to make have blinded setup as reported in more experimental study on this issue. However, this is the decision-making process regarding treatment choice. A similar approach has only been used in one previous study13 whereas other studies use cadaver knees or video of arthroscopic surgery to investigate this issue.4,14,15 In the cases where the cartilage lesions were assessed by 2 different orthopedic surgeons, only a minor difference between the assessments was noted. This indicates that the results are applicable not only to a specific surgeon but also to most orthopedic surgeons practicing knee arthroscopy probably can reproduce them. It has been reported previously by other authors that the interrater reliability for arthroscopic grading of cartilage lesions is acceptable.14,15 This study focused on the clinical setting where blinding of the measurements would be very difficult to arrange or not very practical in use. Expensive equipment and imaging protocols, as suggested by some authors, would not be beneficial to the process of decision-making, as an arthroscopic evaluation in most cases would be needed anyway. Errors in mapping less than 0.6 cm2 would not affect our clinical decision regarding treatment of these challenging injuries. However, new imaging techniques might help to better assesses the surrounding cartilage and the quality of the repair cartilage. MRI in clinical practice is currently a guide for the clinician for grading the cartilage lesion. As demonstrated in this study, standard knee MRI is clearly inferior to an arthroscopic procedure with regard to assessment of the size of the lesion; however, this might be different with cartilage-devoted MRI protocol. Computer-assisted measurements of cartilage lesion might be more accurate but these depend on arthroscopic training in the evaluation of knee cartilage to discriminate between normal and abnormal cartilage.
It would be preferable that measurements of different surgeons had been available for all cases; however, the correlation between the assessments in those cases where 2 were available was quite high. This indicates that an interrater difference would not affect the findings in the current study.
Another related issue is the diagnosis of co-injuries in anterior cruciate ligament registries. These are often registered as an area description both in the International Cartilage Repair Society classification used in the registries. In the older Outerbrigde classification, which is still used by some authors, area is also an important parameter to distinguish between grades 3 and 4. Both these classification system depend on the ability of surgeon to accurately estimate the size of the lesion in the clinical setting when a knee arthroscopy is performed.
The major weakness of the study is that it is not blinded according to estimation of the lesion at open surgery evaluated as the golden standard. However, as the interrater variability in the current study is not large with regard to the arthroscopic measurements, this bias is probably of limited importance. This has also been reported in other studies.14,15 Furthermore, the arthroscopic area measurement is performed after removal of the injured cartilage in the lesion and this measurement is very unlikely to be subjected to large measurements errors. A small enlargement of the area might be found as the debridement of the cartilage lesion includes removal of healthy cartilage. A minor selection bias probably also exists as only patients with lesions large enough to be candidates for cartilage surgery by arthrotomy was included in the study. As a consequence, cartilage lesions less than 1 cm2 were not examined in the study; however, these would not generally be evaluated for extensive cartilage repair surgery and as such should not been included in the current study.
Several studies on cartilage repair compare an arthroscopic method as debridement or microfracture to more invasive method that includes open arthrotomy and cell implantation. The assessment of the size of the lesions might be associated with 24% difference in area of the cartilage lesion even though considered as equal. This is rarely described or focused in these studies but should be discussed in clinical trials on cartilage repair methods when microfracture is used as the standard treatment. Although it may not interfere with the results presented, it should probably be noted as a possible uneven distribution of lesion area treated in such trials. Knee arthroscopic examination estimated a cartilage full-thickness lesion with an error of less than 25% in the majority of the patients, and no significant difference of the mean estimations was found between arthroscopic and arthrotomy measurements of cartilage lesions in the knee. Hence, arthroscopic mapping of the cartilage lesion provided the accuracy needed in the clinic to assess the area of the cartilage lesion to decide the treatment based on the recommendations published in the literature; however, further research is needed to improve the results found in the study.
Footnotes
Acknowledgments and Funding: Grant research support from the Foundation of Sophies Minde is appreciated for the current study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval: The regional ethical committee approved the study protocols.
References
- 1. Arøen A, Jones D, Fu F. Arthroscopic diagnosis and treatment of cartilage injuries. Sports Med Arthrosc Rev. 1998;6(1): 31-40. [Google Scholar]
- 2. Arøen A, Løken S, Heir S, Alvik E, Ekeland A, Granlund OG, et al. Articular cartilage lesions in 993 consecutive knee arthroscopies. Am J Sports Med. 2004;32(1):211-5. [DOI] [PubMed] [Google Scholar]
- 3. Cole BJ, Pascual-Garrido C, Grumet RC. Surgical management of articular cartilage defects in the knee. J Bone Joint Surg Am. 2009;91(7):1778-90. [PubMed] [Google Scholar]
- 4. Diaz R, Kidwell M, Albright J, Dolan L. Knee cartilage defect documentation: computer assistance in quantification of cartilage defects. Orthopedics. 2005;28(10 Suppl):s1275-6. [DOI] [PubMed] [Google Scholar]
- 5. Knutsen G, Engebretsen L, Ludvigsen TC, Drogset JO, Grøntvedt T, Solheim E, et al. Autologous chondrocyte implantation compared with microfracture in the knee. A randomized trial. J Bone Joint Surg Am. 2004;86(3):455-64. [DOI] [PubMed] [Google Scholar]
- 6. Saris DB, Vanlauwe J, Victor J, Almqvist KF, Verdonk R, Bellemans J, et al. Treatment of symptomatic cartilage defects of the knee: characterized chondrocyte implantation results in better clinical outcome at 36 months in a randomized trial compared to microfracture. Am J Sports Med. 2009;37(Suppl 1):10S-19S. [DOI] [PubMed] [Google Scholar]
- 7. Hjelle K, Solheim E, Strand T, Muri R, Brittberg M. Articular cartilage defects in 1,000 knee arthroscopies. Arthroscopy. 2002;18(7):730-4. [DOI] [PubMed] [Google Scholar]
- 8. Steinwachs MR, Guggi T, Kreuz PC. Marrow stimulation techniques. Injury. 2008;39(Suppl 1):S26-31. [DOI] [PubMed] [Google Scholar]
- 9. Basad E, Ishaque B, Bachmann G, Sturz H, Steinmeyer J. Matrix-induced autologous chondrocyte implantation versus microfracture in the treatment of cartilage defects of the knee: a 2-year randomised study. Knee Surg Sports Traumatol Arthrosc. 2010;18(4):519-27. [DOI] [PubMed] [Google Scholar]
- 10. Guettler JH, Demetropoulos CK, Yang KH, Jurist KA. Osteochondral defects in the human knee: influence of defect size on cartilage rim stress and load redistribution to surrounding cartilage. Am J Sports Med. 2004;32(6):1451-8. [DOI] [PubMed] [Google Scholar]
- 11. Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307-10. [PubMed] [Google Scholar]
- 12. Nehrer S, Dorotka R, Domayer S, Stelzeneder D, Kotz R. Treatment of full-thickness chondral defects with hyalograft C in the knee: a prospective clinical case series with 2 to 7 years’ follow-up. Am J Sports Med. 2009;37(Suppl 1):81S-87S. [DOI] [PubMed] [Google Scholar]
- 13. Niemeyer P, Pestka JM, Erggelet C, Steinwachs M, Salzmann GM, Sudkamp NP. Comparison of arthroscopic and open assessment of size and grade of cartilage defects of the knee. Arthroscopy. 2011;27(1):46-51. [DOI] [PubMed] [Google Scholar]
- 14. Cameron ML, Briggs KK, Steadman JR. Reproducibility and reliability of the outerbridge classification for grading chondral lesions of the knee arthroscopically. Am J Sports Med. 2003;31(1):83-6. [DOI] [PubMed] [Google Scholar]
- 15. Marx RG, Connor J, Lyman S, Amendola A, Andrish JT, Kaeding C, et al. Multirater agreement of arthroscopic grading of knee articular cartilage. Am J Sports Med. 2005;33(11):1654-7. [DOI] [PubMed] [Google Scholar]