The game of football, as it is called worldwide, is played by more than 300 million people globally. It is the most popular sport in the world, and participation in this dynamic sport is growing rapidly. We will from this point forward refer to the football athlete as a football (soccer) player for the importance of convention. The inherent nature of the game is played at the extremes of intense performance and at times is a high-impact contact sport associated with significant acute and chronic joint contact forces with potential detrimental effects to the joint surface. Articular cartilage injury is observed with increasing frequency in football players and is commensurate with the competitive level.1,2 Due to the limited spontaneous regeneration of articular cartilage, injuries often lead to significant symptoms under the continued high demands of football, ultimately resulting in a decrease in performance or the inability to play. The Fédération Internationale de Football Association (FIFA) Medical Assessment and Research Centre (F-MARC) and International Cartilage Repair Society (ICRS) recognize the enormous impact of articular cartilage injury for the football (soccer) player.3 This special issue presents a unique collaboration between FIFA and ICRS in an effort to help advance the science and the understanding of articular cartilage injury and degeneration in the football (soccer) player as well as the options for its treatment and prevention. The approach to the athlete always uses the “spectrum of care” paradigm (Figure 1): prevention, performance optimization, injury care, rehabilitation and restoration, return to sport, prevention of reinjury and osteoarthritis, and keeping the aging athlete healthy through exercise. These are the hallmark principles that illuminate the importance of these collaborative relationships. Using the successful FIFA Football for Health programme, including 11+ to prevent injuries and 11 for Health, this special issue provides 11 articles, like the 11 players on the field, that provide a comprehensive overview over the current knowledge of cartilage injury pathophysiology, epidemiology, and etiology and offers a contemporary view at existing management algorithms, developing treatment options, and prevention strategies for this at-risk population. We are so fortunate to have collaborative and consensus contributions from the world’s experts in their respective fields of cartilage repair! Because the majority of present knowledge is in the area of the knee joint, this is our focus.
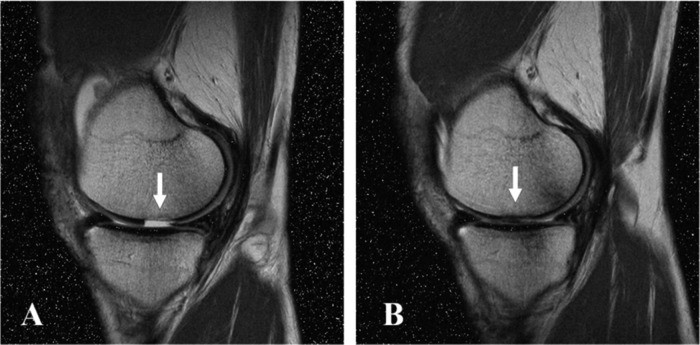
Figure 1.
The “spectrum of care” paradigm for the management of articular cartilage injury and degeneration in football (soccer) players.
In general, evidence-based medicine (EBM) and innovation drive clinical decision making and practice and vice versa. The scientific evidence base for cartilage injury and repair in the athlete is established by Drs. Steinwachs, Engebretsen, and Brophy. Football (soccer) players frequently injure the anterior cruciate ligament (ACL) and menisci.4 These injuries and the inherent risk of the game create an overall prevalence of knee articular cartilage lesions of 36% and up to 72%.5 The football (soccer) player with articular cartilage injury is often faced with a significant challenge because of the high demands placed on the normal, repaired, and regenerated tissue by the game over time.6 These cartilage defects in athletes can be treated with microfracture, osteochondral autogenic or allogenic tissues, and autologous chondrocyte implantation. There is increasing and robust scientific evidence for cartilage repair in athletes, with more extensive information available for microfracture and autologous chondrocyte implantation than for osteochondral grafting. The ultimate challenge is the quality of the repair tissue. Repaired and/or regenerated cartilage must closely resemble and function like normal hyaline cartilage, and this ability may be the most significant factor for the return to sport.
Drs. Mithoefer and Steadman present a case series of professional football (soccer) athletes and systematic review for microfracture.7 They conclude that the microfracture technique followed by appropriate rehabilitation provides restoration of knee joint function, allowing a high rate of return to football (soccer). The importance of the technical details of the surgical procedure and rehabilitation is critical to optimize the potential of a successful outcome of this frequently used repair technique. However, the issue of deterioration of clinical results in some after 2 years is a concern over time and requires further evaluation. Drs. Panics, Hangody, Baló, Vásárhelyi, and Gál establish that autologous osteochondral mosaicplasty in competitive elite and recreational football (soccer) players is a good alternative procedure to repair cartilage damage with best results in younger athletes with smaller lesions.8 In their article, Drs. Mithoefer, Minas, Peterson, and Mandelbaum demonstrate that articular cartilage repair with autologous chondrocyte implantation especially in elite football (soccer) players often allows for successful return to this high-impact sport with excellent durability at 5 years and beyond.9,10 The main disadvantage of this technique is the long time for tissue maturation and consequent return to sport. The critical importance of the functional unit of the joint includes the subchondral, chondral, and meniscal integrity. Recent trends in allograft procurement, safety, and access in some countries have allowed safe and effective means of replacement of osteochondral and meniscal deficits and restoration of function. Drs. Görtz, Williams, Gersoff, and Bugbee describe that osteochondral allograft reconstruction is an increasingly popular treatment option for osteoarticular lesions in athletes.11 These allografts provide mature and immune-privileged hyaline cartilage on an osseous scaffold that serves as an attachment vehicle. This is rapidly replaced via creeping substitution, leading to reliable graft integration that allows for simplified rehabilitation and accelerated return to sport.12 The importance of the meniscus to provide joint homeostasis and load distribution is essential to the joint. In the meniscectomized knee, meniscus allografts offer potential functional, analgesic, and chondroprotective benefits. In the player at the end of his or her professional/competitive career, meniscal allografts can play a role in averting progression of chondropenia and facilitating knee function and an active lifestyle.
So what do we do for the specific athlete with a spectrum of cartilage deficits? How do we select the best specific option and at what timing? Drs. Bekkers, de Windt, Brittberg, and Saris provide a critical review of the “state of cartilage repair” in football (soccer) athletes.13 In addition, the authors provide a critical review of the best available evidence for cartilage surgery and treatment selection, evaluate specific patient profiles for professional and recreational athletes, and propose a treatment algorithm for the treatment of focal cartilage lesions in football (soccer) players.
Once the intervention is completed, attention to detail of postoperative protocols, rehabilitation, restoration of function, return to sport participation and competition, as well as prevention of future injury or progression towards osteoarthritis is essential. Karen Hambly, Holly Silvers, and Matthias Steinwachs illuminate the fact that the evidence base for rehabilitative practice after articular cartilage repair is increasing but remains sparse in areas.14 In addition, articular cartilage repair has been shown to allow return to sport, but rehabilitation time scales can be lengthy. Successful rehabilitation for a return to football after articular cartilage repair of the knee requires the player to be able to accept the load of the sport and adapt on the local, regional, and systemic levels. This necessitates a multidisciplinary approach to rehabilitation, especially in the transition from therapy to performance, training, and playing in games. Return to football is always a “significant challenge”, as presented by Drs. Mithoefer and Della Villa.15 It should be recognized that not all players will return to football after articular cartilage repair. Factors that must be considered are return rate, time to return, and durability after return. The average return rate to sport after articular cartilage repair was 78% without a significant difference in return rate or postoperative level of play between cartilage repair techniques. The range of time to return varied between 7 to 17 months, with the longest time for autologous chondrocyte transplantation. These parameters and expectations by the patient, athlete, and coach must be considered in all clinical decisions. An advanced sport-specific and a multidisciplinary, phasic rehabilitation can effectively reduce recovery time.16 The durability of results was best after autologous chondrocyte implantation, with up to 96% continued sport participation after more than 3 years. There are several factors that determine favorable and successful return to football (soccer). These include player age (younger), time between injury symptoms and treatment (less time), competitive level of participation (higher), defect size (smaller), and repair tissue morphology (hyaline or hyaline-like) (Figure 2). Sports and exercise participation after cartilage repair can and will facilitate joint restoration, functional recovery, and fitness levels.17
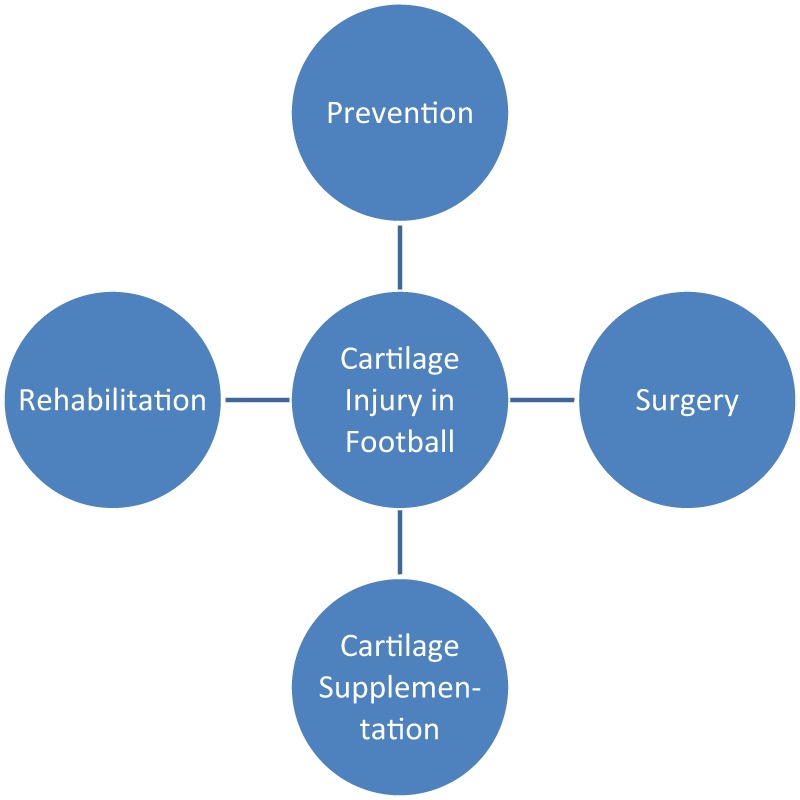
Figure 2.
Magnetic resonance image of a football (soccer) player before (A) and after (B) successful articular cartilage repair that allowed for full return to sport.
Although the spectrum of care approaches listed above are hopeful, Drs. Lee and Chu remind us that the probability of developing osteoarthritis in soccer players is 5 to 12 times more frequent than in the general population.18 It is also highest for the most elite athletes (Figure 3). It is also responsible for retirement in about a third of professional players and diagnosed 4 to 5 years earlier.19,20 This process is a spectrum of degeneration and loss of volume or chondropenia that ultimately leads to frank osteoarthritis. The etiology is multifactorial and involves the demands of the game and biochemical, biomechanical, inflammatory, nutritional, and aging factors. As a result, athletes, particularly those with a history of knee injury, have an earlier onset and higher prevalence of osteoarthritis that would be expected based on their age. In essence, these are “old knees in young people”. It remains a major cause of disability from the sport of football (soccer). This is our call for concern! For players with existing joint degeneration, Drs. Kirkendall and Garrett develop a strategy based on the available evidence and clinical practice guidelines that includes a regimen of patient education, self-management, weight control, and exercise supported by individualized pain management strategies.21 Other noninvasive and or less invasive strategies are available that have varying degrees of impact depending on the stratification of degenerative chondropenia or osteoarthritis (Figure 4). These suggestions can permit an active lifestyle and have, given the prevalence of the disease, a public health impact as a quality of life enhancement.
Figure 3.
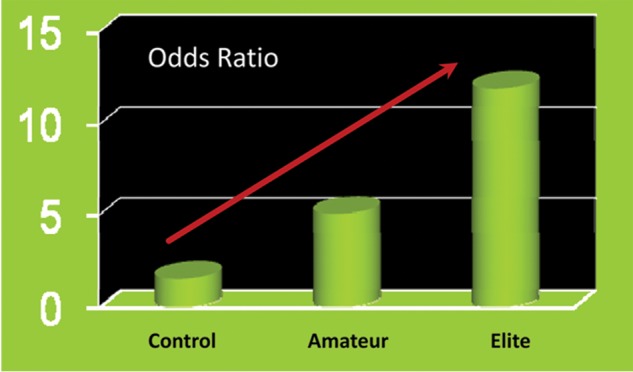
Probability of osteoarthritis in football (soccer) players is increased compared to control populations, particularly at the professional level.
Figure 4.
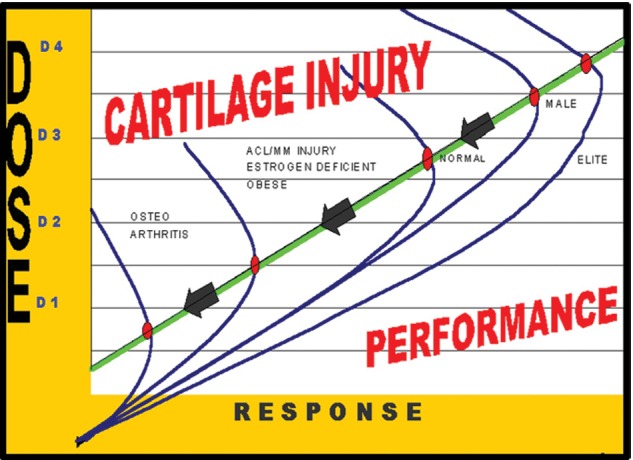
Chondropenia curve demonstrating the spectrum of changes in the articular cartilage status in athletes such as football (soccer) players.
Due to the significant impact of articular cartilage injury and degeneration for the player, the ultimate goal for FIFA and the ICRS is a prevention paradigm: prevention of the injury, whether acute or overuse, and prevention of chondropenia and osteoarthritis and the progression over time. Injury prevention has been a major focus of FIFA and F-MARC through development of the Prevent Injury and Enhance Performance (PEP) program and the evolution to the FIFA 11+ program. The PEP program was designed to reduce ACL injuries, and several studies including a level I randomized control trial have documented significant reductions when this program is successfully utilized as a warm up.22 The evolution to the FIFA 11+ program now includes focus on not only the knee but also muscle, groin, and ankle injury. Significant reductions in severe, overuse, and knee injuries have been demonstrated in large controlled trials.23 Therefore, injury reduction is not only possible, but it also can and should be a reality and part of any football program. These programs are time efficient, easy to do, and are free of expense!
The natural course progression is that articular cartilage defects are to become osteoarthritis over time. The next step in the FIFA/ICRS initiative is how to prevent this progression. Drs. Zaslav, McAdams, Scopp, Theosadakis, Mahajan, and Gobbi evaluate new frontiers for cartilage repair and protection.24 Although recent treatments for damage to articular cartilage have been successful in alleviating symptoms, more durable and complete, long-term articular surface restoration remains the unattained. This hopeful and futuristic approach looks at both new ways to prevent damage to articular surfaces as well as new techniques to re-create biomechanically sound and biochemically true articular surfaces once an athlete injures this surface. This “holy grail” objective should be to produce hyaline cartilage with a well-integrated and flexible subchondral base and the normal zonal variability. Newer surgical techniques, some already in clinical study, and others on the horizon offer opportunities to improve the surgical restoration of the hyaline matrix often disrupted in athletic injury. These include new scaffolds, single-stage cell techniques, engineered allogeneic tissues, the use of mesenchymal stem cells, and gene therapies.
The last step of the prevention paradigm is to prevent the progression of osteoarthritis severity over time. There are a number of nonoperative interventions that have shown early promise in mitigating cartilage symptoms and in preclinical studies have shown evidence for potential disease modification, chondrofacilitation, and chondroprotection. These include the use of glucosamine, chondroitin, and other neutraceuticals, viscosupplementation with hyaluronic acid, platelet-rich plasma, and pulsed electromagnetic fields.
In summary, this supplement provides a compact reference for players, coaches, medical staff, and researchers working with football (soccer) players. It intends to act as a catalyst for the advancement of science and education of cartilage injury in football and the development of innovative treatment concepts and prevention strategies that help to further reduce the incidence of cartilage injury and risk of osteoarthritis in football players of all ages and skill levels. The approach to the athlete always uses the “spectrum of care” systematic paradigm: prevention, performance, injury care, rehabilitation, restoration and return to sport, prevention of reinjury and osteoarthritis, and keeping the aging athlete healthy through exercise. The main objective of the FIFA and ICRS collaboration is to identify the scope of these problems and develop multidisciplinary solutions with the major goal of prevention for now and the future. Also FIFA / F-MARC took the initiative and sponcored a Professorship “Cartilage Engeneering” at the Swiss Federal Institute of Technology (ETH ZH) to stimulate the basic research which again could contribute to prevention and and maybe as a vision to regenerate cartilage damadge in vivo to shorten the time of rehabilitation and “return to play”. It was Einstein who said, “It is the intelligent that can solve problems but the genius will prevent them.” It is with this spirit that we thank FIFA and its president, Mr. Joseph S. Blatter, the ICRS and its president, Professor Daniel Saris, and all the authors for their timely and impactful contributions, all of which make the game of football a better game! Play on!
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the authorship and/or publication of this article.
Funding: The authors received no financial support for the research and/or authorship of this article.
References
- 1. Peterson L, Junge A, Chomiak J, Graf-Baumann T, Dvorak J. Incidence of football injuries and complaints in different age groups and skill-level groups. Am J Sports Med. 2000;28(5 Suppl):S51-7. [DOI] [PubMed] [Google Scholar]
- 2. Levy AS, Lohnes J, Sculley S, LeCroy M, Garrett W. Chondral delamination of the knee in soccer players. Am J Sports Med. 1996;24:634-9. [DOI] [PubMed] [Google Scholar]
- 3. Dvorak J. Osteoarthritis in football: FIFA/F-MARC approach. Br J Sports Med. 2011;45:673-6. [DOI] [PubMed] [Google Scholar]
- 4. Steinwachs MR, Engebretsen L, Brophy RH. Scientific Evidence Base for Cartilage Injury and Repair in the Athlete. Cartilage. 2012;3(Suppl 1):11S-17S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. McAdams T, Mithoefer K, Scopp J, Mandelbaum B. Articular cartilage injury in athletes. Cartilage. 2010;1(3):165-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Roos H, Dahlberg L, Hoerrner LA, Lark MW, Thonar EJ, Shinmei M, et al. Markers of cartilage matrix metabolism in human joint fluid and serum: the effect of exercise. Osteoarthritis Cartilage. 1995;3(1):7-14. [DOI] [PubMed] [Google Scholar]
- 7. Mithoefer K, Steadman RJ. Microfracture in Football (Soccer) Players: A Case Series of Professional Athletes and Systematic Review. Cartilage. 2012;3(Suppl 1):18S-24S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pánics G, Hangody LR, Baló E, Vásárhelyi G, Gál T, Hangody L. Osteochondral Autograft and Mosaicplasty in the Football Athlete. Cartilage. 2012;3(Suppl 1):25S-30S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mithoefer K, Peterson L, Saris DBF, Mandelbaum BR. Evolution and Current Role of Autologous Chondrocyte Implantation for Treatment of Articular Cartilage Defects in the Football (Soccer) Player. Cartilage. 2012;3(Suppl 1):31S-36S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mithöfer K, Peterson L, Mandelbaum B, Minas T. Articular cartilage repair in soccer players with autologous chondrocyte transplantation: functional outcome and return to competition. Am J Sports Med. 2005;33:1639-46. [DOI] [PubMed] [Google Scholar]
- 11. Görtz S, Williams RJ, Gersoff WK, Bugbee WD. Osteochondral and Meniscal Allograft Transplantation in the Football (Soccer) Player. Cartilage. 2012;3(Suppl 1):37S-42S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Robertson CM, Williams R. Return to sport after fresh osteochondral allograft transplantation. Annual Meeting of the American Orthopedic Society for Sports Medicine (AOSSM); 2010 July 17; Providence, RI. [Google Scholar]
- 13. Bekkers JEJ, de Windt TS, Brittberg M, Saris DBF. Cartilage repair in football (soccer) athletes: what evidence leads to which treatment? A critical review of the literature. Cartilage. 2012;3(Suppl 1):43S-49S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hambly K, Silvers HJ, Steinwachs M. Rehabilitation after articular cartilage repair of the knee in the football player. Cartilage. 2012;3(Suppl 1):50S-56S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mithoefer K, Della Villa S. Return to Sports after Articular Cartilage Repair in the Football Player. Cartilage. 2012;3(Suppl 1):57S-62S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Della Villa S, Kon E, Filardo G, Ricci M, Vincentelli F, Delcogliano M, Marcacci M. Does intensive rehabilitation permit early return to sport without compromising the clinical outcome after arthroscopic autologous chondrocyte implantation in highly competitive athletes. Am J Sports Med. 2010; 38(1):68-77. [DOI] [PubMed] [Google Scholar]
- 17. Kreuz PC, Steinwachs M, Erggelet C, Lahm A, Krause S, Ossendorf C, et al. Importance of sports in cartilage regeneration after autologous chondrocyte implantation. Am J Sports Med. 2007;35:1261-8. [DOI] [PubMed] [Google Scholar]
- 18. Lee HH, Constance CR. Clinical and Basic Science of Cartilage Injury and Arthritis in the Soccer Athlete. Cartilage. 2012;3(Suppl 1):63S-68S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Drawer S, Fuller CW. Propensity for osteoarthritis and lower limb joint pain in retired professional soccer players. Br J Sports Med. 2001;35:402-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kujala UM, Kettunen J, Paananen H, Aalto T, Battie MC, Impivaara O, et al. Knee osteoarthritis in former runners, soccer players, weight lifters, and shooters. Arth Rheum. 1995;38:539-46. [DOI] [PubMed] [Google Scholar]
- 21. Kirkendall DT, Garrett WE. Management of the Retired Athlete with Osteoarthritis of the Knee. Cartilage. 2012;3(Suppl 1):69S-76S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mandelbaum BR, Silvers HJ, Watanabe DS, Knarr JF, Thomas SD, Griffin LY, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med. 2005;33(7):1003-10. [DOI] [PubMed] [Google Scholar]
- 23. Soligard T, Nilstad A, Steffen K, Myklebust G, Holme I, Dvorak J, et al. Comprehensive warm-up programme to prevent injuries in young female footballers: cluster randomised controlled trial. Br J Sports Med. 2010;44(11):787-93. [DOI] [PubMed] [Google Scholar]
- 24. Zaslav K, McAdams T, Scopp JM, Theodosakis J, Mahajan V, Gobbi A. New frontiers for cartilage repair and protection. Cartilage. 2012;3(Suppl 1):77S-86S. [DOI] [PMC free article] [PubMed] [Google Scholar]