Abstract
Objective:
To evaluate the clinical outcomes of mosaicplasty in the treatment of focal chondral and osteochondral defects of joints among elite football players.
Methods:
Case series; Level of evidence, 4. The results of mosaicplasty were prospectively evaluated with 1-year intervals with patient-reported outcome measures, radiographs, and sports participation.
Results:
Sixty-one patients who received mosaicplasty in the knee joint were followed from 2 to 17 years (average, 9.6 years). The International Cartilage Repair Society (ICRS) score showed 89% good and excellent results. Sixty-seven percent of all players returned to the same level of sport, with 89% of the elite players and 62% of the competitive players. The average time to return to competitions was 4.5 months (range, 3.5-6.1 months). Players who had better clinical outcomes were significantly younger and had smaller lesions. The results of the medial and lateral condyles were significantly better than those in the patella or trochlea. Concomitant adjuvant procedures improved clinical outcomes. Despite a higher rate of preoperative osteoarthritic changes, clinical outcomes demonstrated a success rate similar to that of less athletic patients.
Conclusion:
Autologous osteochondral mosaicplasty in competitive football players is a good alternative procedure to repair cartilage damage.
Keywords: full-thickness chondral defect, osteochondral transfer, mosaicplasty, autogenous osteochondral graft, football
Introduction
Chondral or osteochondral defects caused by degenerative or traumatic disorders often cause complaints in football and may be career ending without adequate treatment. These changes often present in the younger population participating in football with different levels of activity. In a review study of 25,124 knee arthroscopies, Widuchowski et al.1 reported the incidence of localized focal osteochondral or chondral lesions in 67% of patients, of which 30% were isolated lesions.
According to recent studies, it is obvious that significant mechanical stress on the articular surfaces of the knee is generated during participation in soccer. Drawer and Fuller2 found that 32% of English professional football players had osteoarthrosis when they retired. Levy et al. found a higher risk of chondral injuries in highly skilled football players.3 According to Noyes et al.,4 acute and chronic anterior cruciate ligament (ACL) injuries were 40% to 70% associated with articular cartilage injuries. There are also reports that 40% to 50% of cases with meniscus injury also have cartilage damage. Roos et al.5 showed a relative risk of 14 (an increased prevalence of 1,400%) in knee osteoarthritis 21 years after meniscectomy.
Nonsurgical treatments with chondroprotective medications, nonsteroidal anti-inflammatory drugs, physiotherapy, and hydrotherapy are suitable in the initial stages and are mainly applied as a symptomatic treatment. If healing response was observed in traditional resurfacing procedures (debridement, Pridie drilling, abrasion arthroplasty, microfracture), defect areas were covered with reparative fibrocartilage.6,7 As a consequence of poor biomechanical characteristics of fibrocartilage, these methods are not capable of providing long-lasting relief of symptoms. Permanent or recurrent complaints may indicate repeated surgery. Repair of full-thickness chondral or osteochondral defects with hyaline or hyaline-like tissue through a newly developed technique may have great importance to achieve a durable functional articular surface for the long term.
However, whether these new techniques provide reliable and lasting repair of full-thickness articular cartilage lesions in the knee in top-level football players has only been evaluated with autologous chondrocyte transplantation8 and microfracture.9 Although our previous study10 demonstrated the long-term efficacy of autologous mosaicplasty in elite athletes, no investigation has focused on long-term functional outcome in footballers in terms of lesion healing and their ability to return to play.
Methods
Between 1992 and 2008, 61 professional football players were treated with mosaicplasty. Only those patients were included whose follow-up period was at least 2 years or longer. Based on these data, the average follow-up was 9.6 years (range, 2-17 years).
Players were evaluated at baseline and prospectively re-evaluated at defined postoperative follow-up intervals. Baseline evaluation included thorough history, physical, and radiological examinations. Demographic data, surgical history, modified Hospital for Special Surgery (HSS) score,11 Lysholm score, modified Cincinnati score,12 International Cartilage Repair Society (ICRS)13 score, and skill level were recorded.
Skill level was divided into elite (division I) and competitive (division II and III) for players who participated in the first 3 divisions of their national league. Femoropatellar complaints, as possible donor site disturbances, were evaluated by the Bandi scoring system.14
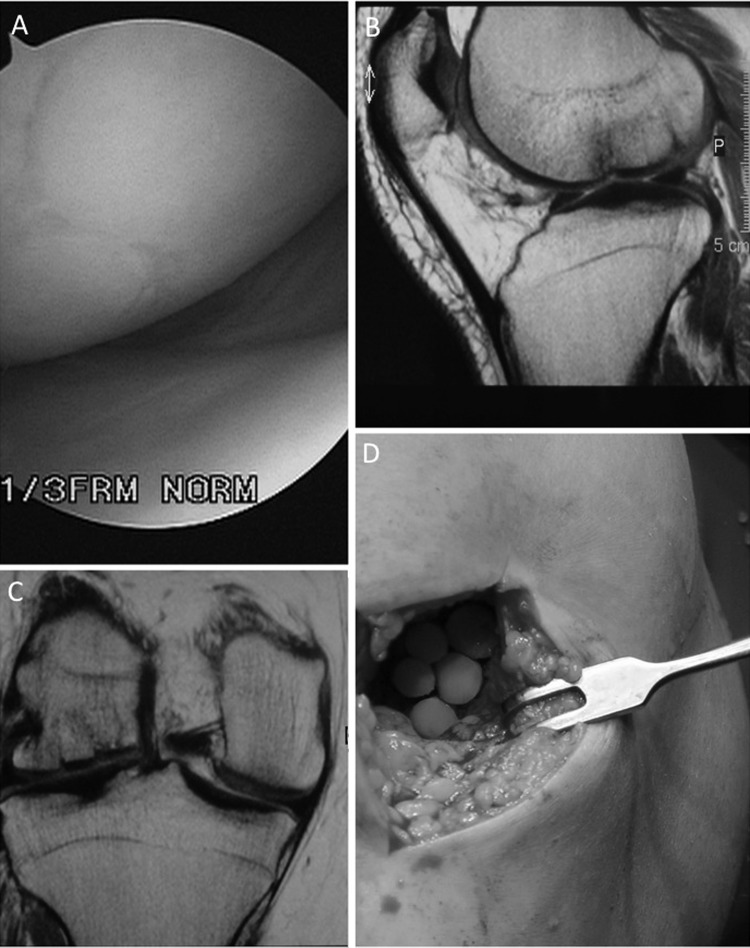
Magnetic resonance imaging (MRI) was done preoperatively, at 6 months, and at 1 year in most of the cases, whereas standard radiographs were conducted preoperatively, at 6 weeks, at 6 months, and afterward yearly in all cases. (Figure 1 B, C)
Figure 1.
(A) Second-look arthroscopy 6 years postoperatively (B) Postoperative MRI at 1-year follow up (C) Postoperative MRI of the chondral damage on the lateral condyle (salvage procedure). (D) Intraoperative picture of the mosaicplasty procedure.
In 69% of the knee patients, other additional surgical interventions were performed, including high tibial osteotomy, ACL reconstruction, meniscal resection, and femoropatellar realignment procedure. Articular cartilage lesions were graded using the depth classification system described by Outerbridge.15 Two thirds of the patients had focal grade III or IV chondral defects, and one third had shallow osteochondral lesions.
The average age of the patients was 25.2 ± 1.6 years (range, 16-41 years), and there were 55 males and 6 females. Nineteen players participated in the first and 42 in the second or third division of their national league.
In 28% of our professional football population, mild or moderate degenerative changes were observed on the preoperative radiographs. Function and radiological scores were analyzed and compared by the Mann-Whitney U nonparametric test. For comparison, we used Statistica 6.0 program (Statsoft Inc., Tulsa, OK).
Results
According to clinical scores, a good to excellent outcome occurred in 90% of femoral condylar, 84% of tibial condylar, and 73% of patellotrochlear resurfacing procedures. Postoperative outcome measures demonstrated an increase of the average modified HSS score (68-90 points, P < 0.05), Lysholm score (66-93 points, P < 0.05), modified Cincinnati score (59-89 points, P < 0.05), and ICRS score (65%-89%, P < 0.05).
There were 87% of the players (elite and combined) who returned to play soccer, 67% of them to the same level. However, while 89% of the elite players returned to the same level, only 62% of the competitive athletes did so (P < 0.05). The average time to return to football was 4.5 months (range, 3.5-6.1 months). Patients who failed to return to football were significantly older.
Lesion size and defect location significantly affected the ability to return to the same level. There were 79% of the players with lesions of the femoral condyles who maintained their preinjury level, while none of the patients with lesions on the tibial condyles, patella, or trochlea were able to return to play (Table 1).
Table 1.
Player Demographics and Lesion Characteristics
| All players | Return | No returna | |
|---|---|---|---|
| Gender (male:female), % | 90:10 | 95:5 | 80:20 |
| Age (range),b y | 25.3 ± 1.2 (16-41) | 24.1 ± 1.3c | 30.6 ± 1.4 |
| Skill, n | |||
| Division I | 25 | 89c | 11 |
| Division II and III | 75 | 62 | 38 |
| Lesion size, cm2 | 2.4 | 2.2c | 3 |
| Lesion location, n | |||
| Medial femoral condyle | 38 | 30 | 8 |
| Lateral femoral condyle | 15 | 11 | 4 |
| Lateral tibial condyle | 3 | 0 | 3 |
| Medial tibial condyle | 0 | 0 | 0 |
| Patella | 4 | 0 | 4 |
| Trochlea | 1 | 0 | 2 |
| ICRS score (excellent/good), % | 89 | 91 | 81 |
Note: ICRS = International Cartilage Repair Society.
No return to same level.
Values are reported as means ± standard deviations; ranges are in parentheses, as indicated.
P < 0.05.
Among 61 knee cases, the following implantations were performed: 53 femoral condylar (38 medial, 15 lateral), 3 tibial condylar (3 lateral), and 5 femoropatellar (4 patellar and 1 trochlear). Table 2 presents detailed results of knee cases. The mean size of the defects was 2.4 cm2 (range, 1.0-5.0 cm2), and the mean number of implanted grafts was 2.6 (range, 1-7). In more than two thirds of the knee patients, other additional surgical interventions were performed: 28 patients underwent ACL reconstruction, 6 high tibial osteotomy, 6 meniscus resection, 2 lateral retinacular release, and 1 femoropatellar realignment procedure. Long-lasting donor site disturbances were found in 5% of all players, as determined by the Bandi score.14 The average number of harvested grafts in this group was 4.1 (range, 3-7). Mosaicplasties on the medial femoral condyle were evaluated according to the alignment; treatment involving high tibial osteotomy was evaluated separately. Table 3 presents clinical outcomes according to preoperative femorotibial alignment.
Table 2.
Clinical Results of 61 Knee Mosaicplasties
| Concomitant procedures | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Defect site | Patients, n | Defect size, mean (range), cm2 | Implanted grafts,a mean (range), n | HTO | ACL | Meniscus resection | Lateral release | Tibial tubercle | Modified HSS score, preoperative/postoperative | Donor site morbidity | |
| Medial femoral condyle | 38 | 2.8 (1.0-5.0) | 3.1 (1-7) | 6 | 18 | 4 | 0 | 0 | 69/91, P = 0.032 | 2 | |
| Lateral femoral condyle | 15 | 1.8 (1.0-4.0) | 2.1 (1-6) | 0 | 10 | 2 | 0 | 0 | 66/90, P = 0.024 | 0 | |
| Lateral tibial condyle | 3 | 1.2 (1.0-2.0) | 1.7 (1-3) | 0 | 0 | 0 | 0 | 0 | 52/86 | 0 | |
| Patella | 4 | 2.4 (1.0-3.0) | 3.5 (2-6) | 0 | 0 | 0 | 2 | 1 | 57/71 | 0 | |
| Trochlea | 1 | 2.1 (1.0-3.5) | 3.1 (1-4) | 0 | 0 | 0 | 0 | 0 | 66/79 | 0 | |
Note: HTO = high tibial osteotomy; ACL = anterior cruciate ligament; HSS = Hospital for Special Surgery.
4.5-, 6.5-, and 8.5-mm-diameter grafts.
Table 3.
Mosaicplasty Outcome on the Medial Femoral Condyle
| Femorotibial alignment | Patients, n | Defect size, mean (range), cm2 | Follow-up period, mean (range), y | Modified HSS score, mean (range) |
|---|---|---|---|---|
| Varus malalignment without correction by HTO | 4 | 2.8 (1.0-4.0) | 7.8 (2-14) | 82 (46-95) |
| Varus malalignment corrected by HTO | 6 | 3.2 (1.0-5.0) | 8.6 (2-16) | 89 (52-100) |
| Valgus alignment, 0°-8° | 25 | 2.7 (1.0-4.5) | 8.8 (2-16) | 91 (61-100) |
| Valgus malalignment, >8° | 3 | 2.2 (1.0-3.4) | 7.5 (3-12) | 94 (88-100) |
Note: HSS = Hospital for Special Surgery; HTO = high tibial osteotomy.
In 28% of our professional players, mild or moderate degenerative changes were observed on the preoperative radiographs. All these signs were classified as Fairbank grade I or II disorders. According to the regular indications of the mosaicplasty procedure, osteoarthritis is a contraindication, but in this professional footballer group, mosaicplasties were still performed as salvage interventions (Figure 1 C). During the last radiographic evaluation, we found Fairbank grades I, II, or III among 35% of our patients. However, MRI scans were not performed routinely; most of the patients arrived to our institute with this type of radiographic findings. These scans were performed in different MRI labors, with different parameters, so they were not suitable for statistical comparison with specific radiographic scores such as the MOCART score. Table 4 presents detailed radiographic evaluation of 61 knee cases.
Table 4.
Radiological Evaluation of 61 Knee Mosaicplasties
| Preoperative Fairbank grade | Patients, n | Postoperative Fairbank grade | Patients, n | Follow-up period, mean (range), y | Defect size, mean (range), cm2 | Age, mean (range), y | HSS value, mean (range) |
|---|---|---|---|---|---|---|---|
| Grade 0 | 44 | Unchanged (grade 0) | 39 | 7.4 (2-17) | 2.2 (1.0-4.5) | 23.7 (16-31) | 92 (52-100) |
| Worsened (grade I-III) | 5 | 7.8 (2-16) | 2.8 (1.5-5.0) | 27.3 (17-36) | 87 (47-100) | ||
| Grade I and II | 17 | Unchanged (grade I and II) | 11 | 6.6 (2-15) | 2.4 (1.0-3.5) | 25.6 (25-39) | 88 (48-100) |
| Worsened (grade II and III) | 5 | 8.1 (4-12) | 3.2 (2.0-5.0) | 33.2 (29-41) | 75 (46-88) |
Note: HSS = Hospital for Special Surgery.
Discussion
Autologous osteochondral mosaicplasty is a promising technique for the treatment of limited-size chondral and osteochondral defects. Several groups have reported good clinical results in different-sized series of patients with few complications.6,16-22 Besides mosaicplasty,10 other techniques have been used successfully to treat focal chondral damages of athletes such as microfracture19,23,24 and autologous chondrocyte transplantation.25-27 Although microfracture9 and autologous chondrocyte transplantation8 have been already evaluated among football players, an assessment of mosaicplasty has not yet been published. It is well documented2,28 that the high demand of this sport provides increased risk in developing cartilage damage. Therefore, evaluation of this method among this particular population will provide essential data about the long-term ability of this technique to withstand increased mechanical load.
In 89% of the cases, good or excellent clinical results were found in football players treated with mosaicplasty. These findings were almost similar to our previous study10 and the study of Gudas et al. (86%)29 on elite athletes but were higher than the results of Marcacci et al. on a mixed population21 (78.9%).
According to location of the lesion, our findings were similar to Gudas et al.29 There were no significant differences in the objective and subjective scores and functional levels between patients with medial or lateral femoral condyle lesions, but the outcomes of the tibial plateau and the patellofemoral lesion were significantly inferior.
Our values concerning return to sports activity on the preinjury level were lower (67%) than the findings of Marcacci et al.21 (73%) and Gudas et al.29 (93%), but the average time to return to sport was significantly less (4.5 months v. 6.5 months). The reason for this difference could be that 28% of our patients had mild to moderate osteoarthritis at the time of the procedure.
In contrast to Gudas et al.29 who used 5.5-mm grafts, we found that 6.5- and 8.5-mm-diameter grafts are suitable to create good congruency, and they do not result in extensive damages of possible donor sites. However, extended graft harvest for bigger lesions yielded increased donor site complaints. It seems that besides graft size, the age of the patient is important. In our group, patients older than 30 years had lower success rates than did younger athletes.
Smaller condylar lesions in ACL-deficient knees treated by mosaicplasty and ACL reconstruction in the same step had good and excellent outcomes in nearly 90% of the group. The Marcacci et al.21 study group found similar outcomes with concomitant procedures.
Bigger condylar lesions, usually occurring in the presence of varus malalignment, had a less successful outcome in spite of the fact that realignment osteotomies were often used to correct the biomechanical background. If the varus malalignment was not corrected, the outcome was significantly worse than in the case of concomitant high tibial osteotomy. Normal alignment or slightly increased valgus seems to be beneficial in the case of medial femoral condylar lesions treated by mosaicplasty of the symptoms.
Careful analysis of failed cases demonstrated that larger lesions requiring extended graft harvest and longer duration of the symptoms, especially in cases of radiological-detectable degenerative changes, may have less chance for long-lasting good results than that of smaller lesions without radiological changes operated closer to the onset of symptoms.
An important element of this study was the high percentage of salvage-category indications. Osteoarthritic degenerative changes of Fairbank grade I or II were observed in 28% of the affected joints. The average size of the chondral defects in these knees was 2.7 cm2. All scoring systems indicated significant improvement. Of 17 patients, 64% resumed the same level of athletic activity, 19% returned to a lower level, and 17% failed to return to sports activities. Only 8% of the athletes rated the postoperative knee function and symptom scores as being worse than before the procedure. The authors concluded that because of the high motivation of this patient group, autologous chondral mosaicplasty provided favorable functional results in high-level footballers, even in those with radiographic evidence of osteoarthritic changes. Radiographic evaluation of salvage-category patients represented better outcomes of younger patients having smaller defects.
A small number of complications was observed, such as postoperative hemarthrosis and in 5%, patellofemoral complaints, according to the Bandi score,14 which is due to long-term donor site morbidity related to the graft harvest. Because we found that athletes reported nearly double the incidence of mild or moderate donor site pain as compared with less active patients, it is likely that vigorous exercise increases donor site pain.
According to these long-term evaluations supported by similar findings from different centers, it seems that autologous osteochondral mosaicplasty may be a useful alternative in the treatment of focal full-thickness cartilage on the femoral condyles of the knee in elite football players.
Footnotes
Acknowledgments and Funding: The authors received no financial support for the research and/or authorship of this article.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the authorship and/or publication of this article.
References
- 1. Widuchowski W, Widuchowski J, Trzaska T. Articular cartilage defects: study of 25,124 knee arthroscopies. Knee. 2007;14(3): 177-82. [DOI] [PubMed] [Google Scholar]
- 2. Drawer S, Fuller CW. Propensity for osteoarthritis and lower limb joint pain in retired professional soccer players. Br J Sports Med. 2001;35(6):402-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Levy AS, Lohnes J, Sculley S, LeCroy M, Garrett W. Chondral delamination of the knee in soccer players. Am J Sports Med. 1996;24(5):634-9. [DOI] [PubMed] [Google Scholar]
- 4. Noyes FR, Bassett RW, Grood ES, Butler DL. Arthroscopy in acute traumatic hemarthrosis of the knee: incidence of anterior cruciate tears and other injuries. J Bone Joint Surg Am. 1980;62(5):687-95, 757. [PubMed] [Google Scholar]
- 5. Roos H, Lauren M, Adalberth T, Roos EM, Jonsson K, Lohmander LS. Knee osteoarthritis after meniscectomy: prevalence of radiographic changes after twenty-one years, compared with matched controls. Arthritis Rheum. 1998;41(4): 687-93. [DOI] [PubMed] [Google Scholar]
- 6. Buckwalter JA, Mankin HJ. Articular cartilage repair and transplantation. Arthritis Rheum. 1998;41(8):1331-42. [DOI] [PubMed] [Google Scholar]
- 7. Newman AP. Articular cartilage repair. Am J Sports Med. 1998;26(2):309-24. [DOI] [PubMed] [Google Scholar]
- 8. Mithofer K, Peterson L, Mandelbaum BR, Minas T. Articular cartilage repair in soccer players with autologous chondrocyte transplantation: functional outcome and return to competition. Am J Sports Med. 2005;33(11):1639-46. [DOI] [PubMed] [Google Scholar]
- 9. Riyami M, Rolf C. Evaluation of microfracture of traumatic chondral injuries to the knee in professional football and rugby players. J Orthop Surg Res. 2009;4:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hangody L, Dobos J, Balo E, Panics G, Hangody LR, Berkes I. Clinical experiences with autologous osteochondral mosaicplasty in an athletic population: a 17-year prospective multicenter study. Am J Sports Med. 2010;38(6):1125-33. [DOI] [PubMed] [Google Scholar]
- 11. Kladny B, Albrecht C, Haase I, Swoboda B. [Outcome of inpatient rehabilitation following total knee replacement using the HSS score]. Z Orthop Ihre Grenzgeb. 2002;140(1):37-41. [DOI] [PubMed] [Google Scholar]
- 12. Risberg MA, Holm I, Steen H, Beynnon BD. Sensitivity to changes over time for the IKDC form, the Lysholm score, and the Cincinnati knee score: a prospective study of 120 ACL reconstructed patients with a 2-year follow-up. Knee Surg Sports Traumatol Arthrosc. 1999;7(3):152-9. [DOI] [PubMed] [Google Scholar]
- 13. Smith GD, Taylor J, Almqvist KF, Erggelet C, Knutsen G, Garcia Portabella M, et al. Arthroscopic assessment of cartilage repair: a validation study of 2 scoring systems. Arthroscopy. 2005;21(12):1462-7. [DOI] [PubMed] [Google Scholar]
- 14. Bandi W. Vorverlagerung der tuberositas tibiae bei chondromalacia patellae und femoropatellarer arthrose. Hefte Unfallheilkd. 1975;127:175-86. [PubMed] [Google Scholar]
- 15. Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43-B:752-7. [DOI] [PubMed] [Google Scholar]
- 16. Bartha L, Vajda A, Duska Z, Rahmeh H, Hangody L. Autologous osteochondral mosaicplasty grafting. J Orthop Sports Phys Ther. 2006;36(10):739-50. [DOI] [PubMed] [Google Scholar]
- 17. Bobic V. Arthroscopic osteochondral autograft transplantation in anterior cruciate ligament reconstruction: a preliminary clinical study. Knee Surg Sports Traumatol Arthrosc. 1996;3(4):262-4. [DOI] [PubMed] [Google Scholar]
- 18. Chow JC, Hantes ME, Houle JB, Zalavras CG. Arthroscopic autogenous osteochondral transplantation for treating knee cartilage defects: a 2- to 5-year follow-up study. Arthroscopy. 2004;20(7):681-90. [DOI] [PubMed] [Google Scholar]
- 19. Gudas R, Kalesinskas RJ, Kimtys V, Stankevicius E, Toliusis V, Bernotavicius G, et al. A prospective randomized clinical study of mosaic osteochondral autologous transplantation versus microfracture for the treatment of osteochondral defects in the knee joint in young athletes. Arthroscopy. 2005;21(9):1066-75. [DOI] [PubMed] [Google Scholar]
- 20. Horas U, Pelinkovic D, Herr G, Aigner T, Schnettler R. Autologous chondrocyte implantation and osteochondral cylinder transplantation in cartilage repair of the knee joint: a prospective, comparative trial. J Bone Joint Surg Am. 2003; 85-A(2):185-92. [DOI] [PubMed] [Google Scholar]
- 21. Marcacci M, Kon E, Zaffagnini S, Iacono F, Neri MP, Vascellari A, et al. Multiple osteochondral arthroscopic grafting (mosaicplasty) for cartilage defects of the knee: prospective study results at 2-year follow-up. Arthroscopy. 2005;21(4):462-70. [DOI] [PubMed] [Google Scholar]
- 22. Hangody L, Kish G, Karpati Z, Eberhart R. Osteochondral plugs: autogenous osteochondral mosaicplasty for the treatment of focal chondral and osteochondral articular defects. Oper Tech Orthop. 1997;7(4):312-22. [Google Scholar]
- 23. Gobbi A, Nunag P, Malinowski K. Treatment of full thickness chondral lesions of the knee with microfracture in a group of athletes. Knee Surg Sports Traumatol Arthrosc. 2005;13(3):213-21. [DOI] [PubMed] [Google Scholar]
- 24. Mithoefer K, Williams RJ, Warren RF, Wickiewicz TL, Marx RG. High-impact athletics after knee articular cartilage repair: a prospective evaluation of the microfracture technique. Am J Sports Med. 2006;34(9):1413-8. [DOI] [PubMed] [Google Scholar]
- 25. Mithofer K, Minas T, Peterson L, Yeon H, Micheli LJ. Functional outcome of knee articular cartilage repair in adolescent athletes. Am J Sports Med. 2005;33(8):1147-53. [DOI] [PubMed] [Google Scholar]
- 26. Mithoefer K, Hambly K, Della Villa S, Silvers H, Mandelbaum BR. Return to sports participation after articular cartilage repair in the knee: scientific evidence. Am J Sports Med. 2009;37 Suppl 1:167S-76S. [DOI] [PubMed] [Google Scholar]
- 27. Della Villa S, Kon E, Filardo G, Ricci M, Vincentelli F, Delcogliano M, et al. Does intensive rehabilitation permit early return to sport without compromising the clinical outcome after arthroscopic autologous chondrocyte implantation in highly competitive athletes? Am J Sports Med. 2010;38(1):68-77. [DOI] [PubMed] [Google Scholar]
- 28. Roos H. Are there long-term sequelae from soccer? Clin Sports Med. 1998;17(4):819-31, viii. [DOI] [PubMed] [Google Scholar]
- 29. Gudas R, Stankevicius E, Monastyreckiene E, Pranys D, Kalesinskas RJ. Osteochondral autologous transplantation versus microfracture for the treatment of articular cartilage defects in the knee joint in athletes. Knee Surg Sports Traumatol Arthrosc. 2006;14(9):834-42. [DOI] [PubMed] [Google Scholar]