Abstract
Objective:
Patellofemoral instability is common and affects a predominantly young age group. Chondral injury occurs in up to 95%, and includes osteochondral fractures and loose bodies acutely and secondary degenerative changes in recurrent cases. Biomechanical abnormalities, such as trochlear dysplasia, patella alta, and increased tibial tuberosity-trochlear groove distance, predispose to both recurrent dislocations and patellofemoral arthrosis.
Design:
In this article, we review the mechanisms of chondral injury in patellofemoral instability, diagnostic modalities, the distribution of lesions seen in acute and episodic dislocation, and treatments for articular cartilage lesions of the patellofemoral joint.
Results:
Little specific evidence exists for cartilage treatments in patellofemoral instability. In general, the results of reparative and restorative procedures in the patellofemoral joint are inferior to those observed in other compartments of the knee.
Conclusion:
Given the increased severity of chondral lesions and progression to osteoarthritis seen with recurrent dislocations, careful consideration should be given to early stabilisation in patients with predisposing factors.
Keywords: patellofemoral joint, articular cartilage, instability
Introduction
The articular cartilage of the patellofemoral (PF) joint is the thickest in the human body, with patella cartilage thickness up to 7.5 mm and trochlea cartilage thickness up to 3.5 mm measured in normal subjects.1 The joint is subjected to large compressive loads of up to 8 times body weight during squatting2 and 5972 N when landing after a jump.3
The incidence of first time patellofemoral dislocation is 7 per 100,000 across all age groups,4 but as high as 107 per 100,000 between ages 9 and 15 years.5 Dislocation may occur in normal knees secondary to trauma; however, patients are frequently found to have predisposing factors such as trochlear dysplasia, patella alta, increased tibial tuberosity-trochlear grove (TT-TG) distance or ligament hyperlaxity.6,7 Acute dislocation almost uniformly damages the soft tissue restraints,8 in particular the medial patellofemoral ligament (MPFL), which provides 50% to 60% of resistance to lateral displacement.9,10 Further dislocations, termed episodic patella dislocations (EPDs), occur in 40% to 70% with nonoperative management.11-13 Chondral damage has been reported in more than 90% of patients with EPD.14
Pathogenesis of Chondral Injury
Chondral damage in patellofemoral dislocation may result from acute traumatic events, altered joint loading caused by ongoing instability and preexisting anatomical abnormalities, and iatrogenic injury due to surgical intervention.
Acute, macroscopic chondral injury includes osteochondral or chondral fractures and fissures occurring at the time of dislocation or reduction. These injuries may be detected in up to 95% of acute dislocations.15 Resultant loose bodies may be visible on radiological investigations, and have traditionally been regarded as an indication for early operative intervention.7 Loose bodies have been reported in 31% to 58% after a first dislocation.16-18 The high incidence of osteochondral as opposed to chondral fractures in this generally young group may be due to age related properties of the subchondral bone, calcified cartilage, and cartilage layers.19
Ongoing chondral damage occurs after the acute injury, and involves cell death and extracellular matrix degradation. Cell death occurs by both chondrocyte necrosis and apoptosis,20 and continues for 48 to 96 hours after injury.21,22 Chondrocytes may undergo a specific type of apoptosis, termed chondroptosis, and the intracellular signaling pathways may differ from those seen in other cell types.23 Extracellular matrix degradation occurs because of upregulation of matrix metalloproteinases. Numerous chemical mediators are involved in this process, including mitogen-activated protein kinases, p38, extracellular signal-regulated kinases, and c-Jun N-terminal kinases.24
Delayed chondral damage, or posttraumatic osteoarthritis (OA), occurs in the setting of chronic loading abnormalities.25 Despite the long-standing clinical association between joint injury and subsequent arthrosis, the exact processes involved are poorly understood. Joint instability has been shown to increase peak contact stresses in vitro,26 and the degree of instability to correlate with cartilage degeneration in an animal model.27 Stephen et al.28 have recently demonstrated a significant increase in lateral facet peak contact pressure in early flexion after sectioning of the MPFL, associated with increased lateral patella tilt and translation. Lateral tilt and translation are predictive of PF OA progression.29 Preexisting joint structural abnormalities are also associated with cartilage damage. In hip dysplasia, cumulative contact stress–time exposure correlates with the development of secondary OA, with more than 90% risk for exposures over 10 MPa-years compared with only 20% below this level.30 Jungmann et al.31 have demonstrated trochlear dysplasia to be associated with more severe patellofemoral OA in 304 patients from the Osteoarthritis Initiative longitudinal study. Indeed, Noehren et al.32 found the radiological risk factors for lateral PF degenerative disease in young patients to be almost identical those for PF instability, including trochlear dysplasia, patella alta, and increased TT-TG distance.
Surgical treatment of PF instability has been associated with secondary OA, increased pain, and even medial patella dislocation.33 Direct chondral injury may occur during surgery, for instance, because of drill penetration. Patella fracture has been reported after MPFL reconstruction.34 Medial PF degeneration has been demonstrated in long term follow-up after patella realignment surgery35,36 and may be due to excessive medialization.37 Increased medial PF joint pressures have also been documented with small increases in tension in MPFL reconstruction38; however, these techniques may result in less secondary degenerative change than realignment procedures.39,40
Diagnosis of Chondral Lesions
Chondral lesions in acute and episodic patella dislocation may be diagnosed radiologically or at operation by either arthroscopy or arthrotomy.
Plain radiographs provide valuable information regarding predisposing factors in PF instability and the development of arthrosis over the longer term; however, they are poor for the detection of osteochondral injuries. Stanitski and Paletta18 found only 32% of arthroscopically proven lesions diagnosed on preoperative radiographs. Similarly, Dainer et al.41 discovered osteochondral defects not visible on plain radiographs in 40%.
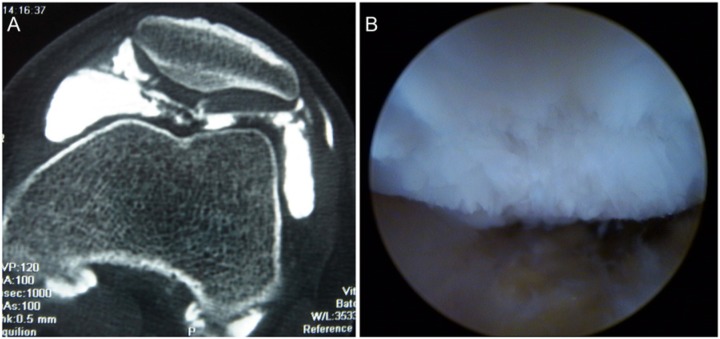
Similar to plain radiographs, computed tomography (CT) gives poor cartilage detail but allows assessment of other indices such as TT-TG. CT arthrography (Fig. 1), however, allows diagnosis of chondral injury with similar accuracy to magnetic resonance imaging (MRI) and may be more accurate in previously operated knees.42
Figure 1.
(A) Computed tomography arthrogram demonstrating central and medial patella chondral damage with loose cartilage in the patellofemoral joint. (B) Arthroscopic view in the same patient demonstrating chondral injury to the central and medial patella with loss of the patella ridge.
Magnetic resonance imaging is able to diagnose chondral and osteochondral lesions noninvasively. Medial soft tissue injuries and bone bruising patterns characteristic of patella dislocation may also be apparent,43 as well as unsuspected ligament and meniscal injuries.16,44 A recent systematic review found MRI to be 87% sensitive and 86% specific in diagnosing patella chondral lesions, and 72% sensitive and 89% specific for trochlear lesions when compared with arthroscopy.45 von Engelhardt et al.46 compared the accuracy of MRI diagnosis with that of arthroscopy in acute and episodic dislocations. They found MRI to be more accurate in acute compared to episodic cases. Accuracy was also better for higher grade lesions. Other authors, however, have reported false positives,47 and found MRI to underestimate the size of cartilage lesions after debridement.48
Specific cartilage sequences, such as dGEMRIC (delayed gadolinium-enhanced MRI of cartilage) and T2 mapping, may have a role in the diagnosis and management of patellofemoral cartilage injuries in the future,49-51 as may newer technologies, such as delayed quantitative CT arthrography (dQCTA)52 and SPECT/CT (single photon emission computed tomography with conventional computed tomography).53,54
Arthroscopy remains the gold standard for diagnosis of chondral lesions of the PF joint.45,47,55 When performed in conjunction with stabilization procedures, it allows diagnosis of meniscal and other internal derangements which may be missed at arthrotomy.56 Arthroscopy is, however, an invasive surgical procedure, and the role of operative intervention in first time dislocation remains controversial.13,57-59
Distribution of Chondral Lesions
Damage to the patella articular cartilage has been reported in up to 95% of first time dislocations15 and 96% in EPD14; however, most authors report rates between 70% and 80%.16,18,56,60 The central and medial areas are the most commonly affected. The injury may occur because of shear at the time of dislocation as the patella moves over the lateral aspect of the femur, by impaction against the femur in the dislocated position, or by a combination thereof during reduction. Luhmann et al.56 examined 41 knees arthroscopically, 7 after acute dislocations and 34 with EPD. They found patella lesions in 30 (73%), of which 16 involved the apex, 12 the medial facet, and 2 the inferior pole. The average lesion size was 112 mm2 (25-256 mm2). Vollnberg et al.60 studied MRI findings in 129 knees divided into 3 groups: acute dislocations, recurrent dislocations (2-9 episodes), and chronic dislocations (>10 episodes). They found 79.8% had patella chondral lesions. The central region was affected in 75% overall, with 51.9% of these involving both the central and medial areas. Interestingly, they found the medial facet involved most frequently in acute events, but an increasing rate of lateral facet involvement with recurrent dislocations, suggesting the development of PF OA. They also found more chondral damage and other signs of OA with increasing numbers of dislocations. Nomura et al.,14,15 in arthroscopic studies in both acute and episodic dislocations, found that patella chondral lesions were almost universal and always occurred in the inferior half to two-thirds of the patella. These inferior lesions may relate to patella alta, with the patella only partially engaged with the trochlea at the time of dislocation. They also found predominantly medial lesions in acute cases and more lateral involvement in episodic dislocation; however, there was no development of new lateral lesions in a subsequent second-look study in either group.61 There was more progression in the EPD group.
Lesions affecting the cartilage on the femoral side are less common, with reported rates from 5% to 32%.15,16,56,60 Interestingly, this is opposite to the pattern of bone bruising found on MRI, where the lateral femoral condyle is affected much more frequently than the patella.43 Femoral lesions almost always occur in combination with patella lesions, although they have been reported to occur in isolation in up to 5%.60 The majority of femoral lesions affect the lateral aspect of the lateral femoral condyle or trochlea, however, the weightbearing surface of the lateral condyle may also be affected.62 Mashoof et al.63 described 7 cases of osteochondral injury to the weightbearing portion of the lateral femoral condyle, ranging in size from 1.5 to 6.75 cm2.
Medial PF joint degeneration has been reported following both proximal and distal realignment procedures.35,36 The acutely damaged medial patella cartilage may be especially sensitive to the significant force increases seen with excessive medialization, particularly in the absence of medial femoral condylar hypoplasia.
Of note, associated injuries are commonly reported in both MRI and arthoscopic studies with an incidence of 11% to 31%.16,44,56 Meniscal injuries, collateral ligament injuries and even partial anterior cruciate ligament tears have been reported.
Treatment Options
Treatment options depend on the type, location, and chronicity of the chondral lesion (Table 1) .
Table 1.
Chondral Lesions and Treatment Options in Patellofemoral Instability.
| Instability Type | Lesion Location | Lesion Types | Cartilage Treatment Options |
|---|---|---|---|
| Acute | Medial/central > lateral patella | Osteochondral/chondral fractures | Internal fixation |
| Lateral femoral condyle | Loose bodies | Debridement | |
| Lateral trochlea | Chondral cracks | Microfracture | |
| Chondral flaps | Mosaicplasty | ||
| Autologous chondrocyte implantation ± treatment of instability/osteotomy | |||
| Episodic | ↑Lateral patella | As above, plus | As above, plus |
| Lateral trochlea | Chondral fissuring | Bulk allograft | |
| Chondral fibrillation | Arthroplasty | ||
| Chondral erosion | |||
| Osteophyte formation |
Nonoperative Therapies
Nonoperative treatment, including analgesic medication, physiotherapy and intra-articular injections of corticosteroids, is the first line of treatment. Viscosupplementation has been shown to reduce pain and improve function in PF OA.64 The exact mechanism of action is unclear. In vitro research has suggested a disease modifying effect65,66; however, a recent trial using dGEMRIC MRI in the tibiofemoral compartments failed to demonstrate any structural or compositional change in the articular cartilage.67 The role of viscosupplementation in acute cartilage lesions and instability is unknown.
Cartilage Procedures
Osteochondral fractures may be amenable to reduction and internal fixation. A variety of fixation methods may be used, including conventional metal screws, headless compression screws, and bioabsorbable pins. Chondrocytes in osteochondral fragments undergo significant necrosis and apoptosis, which may affect the outcome of fixation procedures.20 Lee et al.68 found that patients undergoing internal fixation of patella osteochondral fragments did worse than those without fixation, although this may be explained by the larger size of the internally fixed lesions. Seeley et al.17 found the functional outcome for fixation of osteochondral lesions following PF dislocation to be worse when the weightbearing portion of the lateral femoral condyle was affected17.
Chondral defects may be treated by reparative techniques, such as marrow stimulation and osteochondral transplantation, or restorative procedures such as autologous chondrocyte implantation. In general, the results of these techniques in the PF joint have been inferior to other compartments of the knee.69-71 Some data exist regarding cartilage procedures in association with PF realignment, although instability is rarely specifically identified as a indication or prognostic factor.72-74 No study mentions ongoing instability after cartilage surgery. It makes inherent sense that repair techniques would have poorer outcomes in the setting of ongoing instability.
Marrow stimulation techniques, such as microfracture, Pridie drilling, and abrasion arthoplasty, rely on blood clot containing mesenchymal stem cells from bone marrow to fill chondral defects. These techniques are inexpensive, however, the resultant repair tissue is biomechanically inferior to hyaline cartilage, larger lesions do poorly and results tend to deteriorate over time.75,76 While generally considered safe, complications such as intralesional osteophytes do occur.77 In a study investigating the effect of patient age on microfracture results, Kreuz et al.69 found PF lesions were most likely to deteriorate regardless of age. Periosteal flaps have been used to contain repair tissue, with improved results demonstrated over abrasion techniques for the patella.78 More recently, scaffolds have been employed to improve the quality of repair tissue. Porcine collagen and synthetic polymer scaffolds coupled with growth factors and bone marrow concentrates are already in use.79,80 In a multicenter randomized clinical trial using the scaffold-based BST-CarGel treatment compared with microfracture alone for femoral condylar lesions, Stanish et al.81 demonstrated superior lesion filling and repair tissue quality at 1 year, although clinical superiority was not shown. Multiphasic and gradient scaffolds are also being developed aiming to recreate the tidemark and cartilage–bone interface.82
Osteochondral transplantation, such as mosaicplasty, can result in high-quality repair tissue with rapid healing; however, donor site morbidity limits the defect size that may be treated.83 Hangody et al.,84 reporting their 10-year experience with the mosaicplasty technique, reported 79% good-to-excellent results in 118 procedures involving the PF compartment, compared with 87% to 92% elsewhere in the knee. Gawęda et al.72 studied the results of 19 patients with EPD and significant patella chondral defects (International Cartilage Repair Society [ICRS] grades III and IV) treated with single stage extensor realignment and autologous osteochondral grafting. Compared with a control group treated with realignment only (chondral lesions ICRS grades I and II), the treatment group had significantly worse preoperative Marshall scores (36.3 ± 2.1 vs. 40.7 ± 3.7) but comparable results at 24 months (46.2 ± 1.8 vs. 47.1 ± 1.6). Osteochondral bulk allograft may also be used in the PF joint, however, this should be viewed as a salvage procedure, with high rates of failure due to graft non-incorporation.85,86
Autologous chondrocyte implantation (ACI) is a 2-stage procedure involving chondrocyte harvest, expansion by culture and subsequent reimplantation. These techniques offer the potential for more durable repair with true hyaline cartilage tissue.87 The techniques have evolved from liquid chondrocyte solution injection under a sutured periosteal flap to the greatly simplified implantation of a biodegradable, chondrocyte seeded matrix, although only weak evidence supports the newer generations to date.88 In 1994, Brittberg et al.71 reported good-to-excellent results in only 2 of 7 patients treated for patella lesions with first-generation techniques. Bentley et al.,70 in a randomized control trial of ACI versus mosaicplasty, reported 85% excellent or good clinical results for ACI compared with 60% for mosaicplasty for patella lesions using the modified Cincinatti rating system, although this did not reach statistical significance. Gobbi et al.89 reported results for 38 patients treated with second-generation ACI (Hylograft C) for lesions of the PF joint, 17 of whom had previous or simultaneous patella realignment procedures. They reported 32 of 34 objectively normal or near normal knees at 2 years, and 31 of 34 at 5 years. Patients with patella lesions, however, had a significant decline in International Knee Documentation Committee (IKDC) scores from 2 to 5 years. Filardo et al.90 recently reported comparative results for patella and trochlear lesions treated with matrix-assisted autologous chondrocyte transplantation. Patients with PF malalignment were excluded. They found better results in trochlear lesions than patella lesions at 5-year follow-up, with IKDC scores of 89.6 ± 12.7 and 69.7 ± 17.6, respectively.
A number of factors may influence the result of ACI procedures. Kreuz et al.91 demonstrated inferior outcomes in female patients and for patella lesions, despite the exclusion of PF malalignment. Filardo et al.92 found that females had not only lower raw IKDC scores following matrix-assisted autologous chondrocyte transplantation but also a higher incidence of patella lesions, and that the sex difference was not apparent after matched-pair analysis. Minas et al.77 have demonstrated an increased failure of ACI procedures after previous marrow stimulation techniques, with failure rates three times that of untreated lesions. Pascual-Garrido et al.,93 however, found no difference in outcome for those with previous cartilage surgery, although more than half the patients in their study underwent simultaneous anteromedialization (AMZ) of the tibial tuberosity. Platelet-rich plasma may also have a role in improving repair tissue quality.94
Of particular relevance to PF instability, Niemeyeret al.95 demonstrated significantly better results for lateral facet lesions, compared with lesions involving the medial or both facets, as seen most commonly after acute PF dislocations. They have also described a “double eye” technique for ACI treatment of patella lesions to maintain the height of the patella ridge and minimize shear forces on the repair tissue.96 In a study of 11 patients treated with this technique, Lysholm scores were 75 compared with 60 for the control group.
Realignment Procedures
Realignment procedures have long been known to affect the outcome of cartilage lesions in the PF joint. In 1997, Pidoriano et al.97 correlated the results of AMZ to the location of PF chondral lesions. Of the 36 patients, 57% had at least 1 PF dislocation. They found poorer results in those with medial and diffuse lesions (Fulkerson type III and IVB). A recent systematic review demonstrated a greater improvement in outcome measures for patients undergoing combined ACI and osteotomy compared with ACI alone.98 In 2006, Henderson and Lavigne74 reported on 44 patients with either patella ACI or patella ACI with medializing tibial tuberosity osteotomy based on unspecified clinical and radiological indicators of malalignment. At an average of 2 years of follow-up, the combined group had better modified Cincinnati knee scores (4.5 vs. 1.7 points), better SF-36 physical component scores (70.9 vs. 55.4 points), and higher IKDC scores (85.2 vs. 60.6 points) compared with the ACI only group. They felt that malalignment may have been underdiagnosed in the ACI only group, and that a realignment procedure may be desirable in some patients even with normal PF tracking. Gigante et al.73 reported on 14 knees treated with matrix-seeded ACI and AMZ. Malalignment was defined as TT-TG >20 mm on CT scans. Average Lysholm score improved from 55 to 92.5, and Tegner Activity Scale from 1 to 4. Pascual-Garrida et al.93 reported the results of PF ACI in 52 patients, 28 of whom had simultaneous AMZ. Exact indications for AMZ were not specified. Patients undergoing AMZ showed a greater improvement in Lysholm scores (33 to 67 vs. 31 to 57) and better final IKDC scores (63 vs. 46) at average 4 years’ follow-up. Interestingly, those with a previous failed microfracture had the highest average final Lysholm score of 70. There are no studies into the effect of tibial tuberosity distalisation or MPFL reconstruction on the result of cartilage surgery in the PF joint.
The improvement seen with realignment may not be without risk. Vasiliadis et al.99 reported the results of 92 patients treated with ACI for PF lesions at a mean follow-up of 12.6 years. In this retrospective study, 38 patients had some type of realignment procedure. Results in the 2 groups were similar (Lysholm score 70.5 and Tegner 3 with realignment, 70 and 3 ACI only); however, the rate of serious complications was 29% in the realignment group compared with 13% in the ACI only group. It is also unclear if the benefit of combined ACI and realignment is also observed in the predominantly medial sided lesions seen in acute PF dislocation, particularly as increased medial degenerative change has been reported after realignment procedures.35
Arthroplasty
In advanced PF arthrosis, particularly in cases of trochlear dysplasia, arthroplasty may be an appropriate salvage procedure.100 A number of PF prostheses are available, with inlay and onlay designs. There is some controversy over the choice between PF arthroplasy and total knee arthroplasty in isolated PF arthrosis, particularly in older patients.
Future Directions
An improved understanding of the mechanisms of cell death and matrix degradation in acute chondral injury may afford the opportunity for early, nonsurgical intervention to limit cartilage damage.101-103 A number of studies in animal models104-106 and human cartilage107,108 have demonstrated reduced cell death and cartilage degradation with the use of agents such as P188 surfactant, bone morphogenic proteins (BMP-7), N-acetylcysteine, and capsase inhibitors.
Conclusion
Patellofemoral instability is common and affects a predominantly young age group. Acute chondral injury frequently occurs, most commonly affecting the inferomedial patella. Biomechanical abnormalities, such as trochlear dysplasia, patella alta, and increased tibial tuberosity-trochlear groove distance, predispose to both recurrent dislocations and patellofemoral arthrosis.32
Given the increased severity of chondral lesions and progression to OA seen with recurrent dislocations,60,61 careful consideration should be given to early stabilisation in patients with these predisposing factors. Although older stabilisation procedures were associated with increased rates of OA, recent evidence suggests thatthis is not the case with newer, more anatomical techniques.39
In general, chondral repair and restoration techniques demonstrate inferior outcomes in the PF joint compared with other compartments of the knee. Little evidence exists regarding the outcomes specifically in instability syndromes. Results of combined extensor mechanism realignment by AMZ and ACI are superior to ACI alone for patella lesions in malalignment; however, this may not hold true for the predominantly medial lesions seen after acute PF dislocation. The effects of MPFL reconstruction and tibial tuberosity distalization on PF cartilage procedures are unknown.
Improved understanding of the cellular mechanisms involved in chondral cell death and matrix degradation may allow early nonsurgical intervention to reduce cartilage damage after an acute injury.
Footnotes
Acknowledgments and Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1. Draper C, Besier T, Gold G, Fredericson M, Fiene A, Beaupre A, et al. Is cartilage thickness different in young subjects with and without patellofemoral pain? Osteoarthritis Cartilage. 2006;14(9):931-7. [DOI] [PubMed] [Google Scholar]
- 2. Mason JJ, Leszko F, Johnson T, Komistek RD. Patellofemoral joint forces. J Biomech. 2008;41(11):2337-48. [DOI] [PubMed] [Google Scholar]
- 3. Simpson K, Jameson E, Odum S. Estimated patellofemoral compressive forces and contact pressures during dance landings. J Appl Biomech. 1996;12;1-14. [Google Scholar]
- 4. Atkin DM, Fithian DC, Marangi KS, Stone ML, Dobson BE, Mendelsohn C. Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am J Sports Med. 2000;28(4):472-9. [DOI] [PubMed] [Google Scholar]
- 5. Nietosvaara Y, Aalto K, Kallio PE. Acute patellar dislocation in children: incidence and associated osteochondral fractures. J Pediatr Orthop. 1994;14(4):513-5. [DOI] [PubMed] [Google Scholar]
- 6. Dejour H, Walch G, Nove-Josserand L, Guier CH. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2(1):19-26. [DOI] [PubMed] [Google Scholar]
- 7. Stefancin JJ, Parker RD. First-time traumatic patellar dislocation. Clin Orthop Relat Res. 2007;(455):93-101. [DOI] [PubMed] [Google Scholar]
- 8. Nomura E. Classification of lesions of the medial patello-femoral ligament in patellar dislocation. Int Orthop. 1999;23(5):260-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26(1):59-65. [DOI] [PubMed] [Google Scholar]
- 10. Hautamaa PV, Fithian DC, Kaufman KR, Daniel DM, Pohlmeyer AM. Medial soft tissue restraints in lateral patellar instability and repair. Clin Orthop Relat Res. 1998;(349):174-82. [DOI] [PubMed] [Google Scholar]
- 11. Camanho GL, Viegas AC, Bitar AC, Demange MK, Hernandez AJ. Conservative versus surgical treatment for repair of the medial patellofemoral ligament in acute dislocations of the patella. Arthroscopy. 2009;25(6):620-5. [DOI] [PubMed] [Google Scholar]
- 12. Mäenpää H, Huhtala H, Lento MU. Recurrence after patellar dislocation. Redislocation in 37/75 patients followed for 6-24 years. Acta Orthop. 1997;68(5):424-6. [DOI] [PubMed] [Google Scholar]
- 13. Palmu S. Acute patellar dislocation in children and adolescents: a randomized clinical trial. J Bone Joint Surg Am. 2008;90(3):463-70. [DOI] [PubMed] [Google Scholar]
- 14. Nomura E. Cartilage lesions of the patella in recurrent patellar dislocation. Am J Sports Med. 2004;32(2):498-502. [DOI] [PubMed] [Google Scholar]
- 15. Nomura E, Inoue M, Kurimura M. Chondral and osteochondral injuries associated with acute patellar dislocation. Arthroscopy. 2003;19(7):717-21. [DOI] [PubMed] [Google Scholar]
- 16. Elias DA, White LM, Fithian DC. Acute lateral patellar dislocation at MR imaging: injury patterns of medial patellar soft-tissue restraints and osteochondral injuries of the inferomedial patella. Radiology. 2002;225(3):736-43. [DOI] [PubMed] [Google Scholar]
- 17. Seeley MA, Knesek M, Vanderhave KL. Osteochondral injury after acute patellar dislocation in children and adolescents. J Pediatr Orthop. 2013;33(5):511-8. [DOI] [PubMed] [Google Scholar]
- 18. Stanitski CL, Paletta GA. Articular cartilage injury with acute patellar dislocation in adolescents. Arthroscopic and radiographic correlation. Am J Sports Med. 1998;26(1):52-5. [DOI] [PubMed] [Google Scholar]
- 19. Buckwalter JA. Articular cartilage injuries. Clin Orthop Relat Res. 2002;(402):21-37. [DOI] [PubMed] [Google Scholar]
- 20. Hembree WC, Ward BD, Furman BD, Zura RD, Nichols LA, Guilak F, et al. Viability and apoptosis of human chondrocytes in osteochondral fragments following joint trauma. J Bone Joint Surg Br. 2007;89(10):1388-95. [DOI] [PubMed] [Google Scholar]
- 21. Tochigi Y, Buckwalter JA, Martin JA, Hillis SL, Zhang P, Vaseenon T, et al. Distribution and progression of chondrocyte damage in a whole-organ model of human ankle intra-articular fracture. J Bone Joint Surg Am. 2011;93(6):533-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. D’Lima DD, Hashimoto S, Chen PC, Lotz MK, Colwell CW. Cartilage injury induces chondrocyte apoptosis. J Bone Joint Surg Am. 2001;83-A(Suppl 2, Pt 1):19-21. [DOI] [PubMed] [Google Scholar]
- 23. Roach HI, Aigner T, Kouri JB. Chondroptosis: a variant of apoptotic cell death in chondrocytes? Apoptosis. 2004;9(3):265-77. [DOI] [PubMed] [Google Scholar]
- 24. Ding L, Heying E, Nicholson N, Stroud NJ, Homandberg GA, Buckwalter JA, et al. Mechanical impact induces cartilage degradation via mitogen activated protein kinases. Osteoarthritis Cartilage. 2010;18(11):1509-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Buckwalter JA, Anderson DD, Brown TD, Tochigi Y, Martin JA. The roles of mechanical stresses in the pathogenesis of osteoarthritis: implications for treatment of joint injuries. Cartilage. 2013;4(4):286-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. McKinley TO, Borrelli J, D’Lima DD, Furman BD, Giannoudis PV. Basic science of intra-articular fractures and posttraumatic osteoarthritis. J Orthop Trauma. 2010;24(9):567-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Tochigi Y. Instability dependency of osteoarthritis development in a rabbit model of graded anterior cruciate ligament transection. J Bone Joint Surg Am. 2011;93(7):640-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Stephen JM, Kader D, Lumpaopong P, Deehan DJ, Amis AA. Sectioning the medial patellofemoral ligament alters patellofemoral joint kinematics and contact mechanics. J Orthop Res. 2013;31(9):1423-9. [DOI] [PubMed] [Google Scholar]
- 29. Hunter DJ, Zhang YQ, Niu JB, Felson DT, Kwoh K, Newman A, et al. Patella malalignment, pain and patellofemoral progression: the Health ABC Study1. Osteoarthritis Cartilage. 2007;15(10):1120-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hadley NA, Brown TD, Weinstein SL. The effects of contact pressure elevations and aseptic necrosis on the long-term outcome of congenital hip dislocation. J Orthop Res. 1990;8(4):504-13. [DOI] [PubMed] [Google Scholar]
- 31. Jungmann PM, Tham S-C, Liebl H, Nevitt MC, McCulloch CE, Lynch J, et al. Association of trochlear dysplasia with degenerative abnormalities in the knee: data from the Osteoarthritis Initiative. Skeletal Radiol. 2013;42(10):1383-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Noehren B, Duncan S, Lattermann C. Radiographic parameters associated with lateral patella degeneration in young patients. Knee Surg Sports Traumatol Arthrosc. 2012;20(12):2385-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Miller PR, Klein RM, Teitge RA. Medial dislocation of the patella. Skeletal Radiol. 1991;20(6):429-31. [DOI] [PubMed] [Google Scholar]
- 34. Dhinsa BS, Bhamra JS, James C, Dunnet W, Zahn H. Patella fracture after medial patellofemoral ligament reconstruction using suture anchors. Knee. 2013;20(6):605-8. [DOI] [PubMed] [Google Scholar]
- 35. Sillanpää PJ, Mattila VM, Visuri T, Mäenpää H, Pihlajamäki H. Patellofemoral osteoarthritis in patients with operative treatment for patellar dislocation: a magnetic resonance-based analysis. Knee Surg Sports Traumatol Arthrosc. 2010;19(2):230-5. [DOI] [PubMed] [Google Scholar]
- 36. Schüttler KF, Struewer J, Roessler PP, Gesslein M, Rominger MB, Ziring E, et al. Patellofemoral osteoarthritis after Insall’s proximal realignment for recurrent patellar dislocation. Knee Surg Sports Traumatol Arthrosc. 2013. Epub Apr 2, 2013. 10.1007/s00167-013-2485-0. [DOI] [PubMed] [Google Scholar]
- 37. Kuroda R, Kambic H, Valdevit A, Andrish JT. Articular cartilage contact pressure after tibial tuberosity transfer. A cadaveric study. Am J Sports Med. 2001;29(4):403-9. [DOI] [PubMed] [Google Scholar]
- 38. Beck P, Brown NA, Greis PE, Burks RT. Patellofemoral contact pressures and lateral patellar translation after medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35(9):1557-63. [DOI] [PubMed] [Google Scholar]
- 39. Nomura E, Inoue M, Kobayashi S. Long-term follow-up and knee osteoarthritis change after medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2007;35(11):1851-8. [DOI] [PubMed] [Google Scholar]
- 40. Sillanpää P, Mattila VM, Visuri T, Mäenpää H, Pihlajamäki H. Ligament reconstruction versus distal realignment for patellar dislocation. Clin Orthop Relat Res. 2008;466(6):1475-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Dainer RD, Barrack RL, Buckley SL, Alexander AH. Arthroscopic treatment of acute patellar dislocations. Arthroscopy. 1988;4(4):267-71. [DOI] [PubMed] [Google Scholar]
- 42. De Filippo M, Bertellini A, Pogliacomi F, Sverzellati N, Corradi D, Garlaschi G, et al. Multidetector computed tomography arthrography of the knee: diagnostic accuracy and indications. Eur J Radiol. 2009;70(2):342-51. [DOI] [PubMed] [Google Scholar]
- 43. Sallay PI, Poggi J, Speer KP, Garrett WE. Acute dislocation of the patella: a correlative pathoanatomic study. Am J Sports Med. 1996;24(1):52-60. [DOI] [PubMed] [Google Scholar]
- 44. Kirsch MD, Fitzgerald SW, Friedman H, Rogers LF. Transient lateral patellar dislocation: diagnosis with MR imaging. AJR Am J Roentgenol. 1993;161(1):109-13. [DOI] [PubMed] [Google Scholar]
- 45. Harris JD, Brophy RH, Jia G, Price B, Knopp M, Siston RA, et al. Sensitivity of magnetic resonance imaging for detection of patellofemoral articular cartilage defects. Arthroscopy. 2012;28(11):1728-37. [DOI] [PubMed] [Google Scholar]
- 46. von Engelhardt LV, Raddatz M, Bouillon B, Spahn G, Dàvid A, Haage P, et al. How reliable is MRI in diagnosing cartilaginous lesions in patients with first and recurrent lateral patellar dislocations? BMC Musculoskelet Disord. 2010;11(1):149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Handelberg F, Shahabpour M, Casteleyn PP. Chondral lesions of the patella evaluated with computed tomography, magnetic resonance imaging, and arthroscopy. Arthroscopy. 1990;6(1):24-9. [DOI] [PubMed] [Google Scholar]
- 48. Gomoll AH, Yoshioka H, Watanabe A, Dunn JC, Minas T. Preoperative measurement of cartilage defects by MRI underestimates lesion size. Cartilage. 2011;2(4):389-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Burstein D, Gray M. New MRI techniques for imaging cartilage. J Bone Joint Surg Am. 2003;85(Suppl 2):70-7. [DOI] [PubMed] [Google Scholar]
- 50. Nojiri T, Watanabe N, Namura T, Narita W, Ikoma K, Suginoshita T, et al. Utility of delayed gadolinium-enhanced MRI (dGEMRIC) for qualitative evaluation of articular cartilage of patellofemoral joint. Knee Surg Sports Traumatol Arthrosc. 2006;14(8):718-23. [DOI] [PubMed] [Google Scholar]
- 51. Hannila I, Nieminen MT, Rauvala E, Tervonen O, Ojala R. Patellar cartilage lesions: comparison of magnetic resonance imaging and T2 relaxation-time mapping. Acta Radiol. 2007;48(4):444-8. [DOI] [PubMed] [Google Scholar]
- 52. Hirvasniemi J, Kulmala KA, Lammentausta E, Ojala R, Lehenkari P, Kamel A, et al. In vivo comparison of delayed gadolinium-enhanced MRI of cartilage and delayed quantitative CT arthrography in imaging of articular cartilage. Osteoarthritis Cartilage. 2013;21(3):434-42. [DOI] [PubMed] [Google Scholar]
- 53. Hirschmann MT, Davda K, Iranpour F, Rasch H, Friederich NF. Combined single photon emission computerised tomography and conventional computerised tomography (SPECT/CT) in patellofemoral disorders: a clinical review. Int Orthop. 2010;35(5):675-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Schön SN, Afifi FK, Rasch H, Amsler F, Friederich NF, Arnold MP, et al. Assessment of in vivo loading history of the patellofemoral joint: a study combining patellar position, tilt, alignment and bone SPECT/CT. Knee Surg Sports Traumatol Arthrosc. Epub Oct 11, 2013. 10.1007/s00167-013-2698-2. [DOI] [PubMed] [Google Scholar]
- 55. Smith TO, Drew BT, Toms AP, Donell ST, Hing CB. Accuracy of magnetic resonance imaging, magnetic resonance arthrography and computed tomography for the detection of chondral lesions of the knee. Knee Surg Sports Traumatol Arthrosc. 2012;20(12):2367-79. [DOI] [PubMed] [Google Scholar]
- 56. Luhmann SJ, Schoenecker PL, Dobbs MB, Gordon JE. Arthroscopic findings at the time of patellar realignment surgery in adolescents. J Pediatr Orthop. 2007;27(5):493-8. [DOI] [PubMed] [Google Scholar]
- 57. Panni AS, Vasso M, Cerciello S. Acute patellar dislocation. What to do? Knee Surg Sports Traumatol Arthrosc. 2012;21(2):275-8. [DOI] [PubMed] [Google Scholar]
- 58. Sillanpaa PJ, Maenpaa HM, Mattila VM, Visuri T, Pihlajamaki H. Arthroscopic surgery for primary traumatic patellar dislocation: a prospective, nonrandomized study comparing patients treated with and without acute arthroscopic stabilization with a median 7-year follow-up. Am J Sports Med. 2008;36(12):2301-9. [DOI] [PubMed] [Google Scholar]
- 59. Sillanpää PJ. Treatment with and without initial stabilizing surgery for primary traumatic patellar dislocation: a prospective randomized study. J Bone Joint Surg Am. 2009;91(2):263-73. [DOI] [PubMed] [Google Scholar]
- 60. Vollnberg B, Koehlitz T, Jung T, Scheffler S, Hoburg A, Khandker D, et al. Prevalence of cartilage lesions and early osteoarthritis in patients with patellar dislocation. Eur Radiol. 2012;22(11):2347-56. [DOI] [PubMed] [Google Scholar]
- 61. Nomura E, Inoue M. Second-look arthroscopy of cartilage changes of the patellofemoral joint, especially the patella, following acute and recurrent patellar dislocation. Osteoarthritis Cartilage. 2005;13(11):1029-36. [DOI] [PubMed] [Google Scholar]
- 62. Rorabeck CH, Bobechko WP. Acute dislocation of the patella with osteochondral fracture: a review of eighteen cases. J Bone Joint Surg Br. 1976;58(2):237-40. [DOI] [PubMed] [Google Scholar]
- 63. Mashoof AA, Scholl MD, Lahav A, Greis PE, Burks RT. Osteochondral injury to the mid-lateral weight-bearing portion of the lateral femoral condyle associated with patella dislocation. Arthroscopy. 2005;21(2):228-32. [DOI] [PubMed] [Google Scholar]
- 64. Clarke S, Lock V, Duddy J, Sharif M, Newman JH, Kirwan JR. Intra-articular hylan G-F 20 (Synvisc®) in the management of patellofemoral osteoarthritis of the knee (POAK). Knee. 2005;12(1):57-62. [DOI] [PubMed] [Google Scholar]
- 65. Kawasaki K, Ochi M, Uchio Y, Adachi N, Matsusaki M. Hyaluronic acid enhances proliferation and chondroitin sulfate synthesis in cultured chondrocytes embedded in collagen gels. J Cell Physiol. 1999;179(2):142-8. [DOI] [PubMed] [Google Scholar]
- 66. Stöve J, Gerlach C, Huch K, Günther K-P, Puhl W, Scharf H-P. Effects of hyaluronan on proteoglycan content of osteoarthritic chondrocytes in vitro. J Orthop Res. 2002;20(3):551-5. [DOI] [PubMed] [Google Scholar]
- 67. van Tiel J, Reijman M, Bos PK, Hermans J, van Buul GM, Bron EE, et al. Delayed gadolinium-enhanced MRI of cartilage (dGEMRIC) shows no change in cartilage structural composition after viscosupplementation in patients with early-stage knee osteoarthritis. PLoS One. 2013;8(11):e79785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Lee BJ, Christino MA, Daniels AH, Hulstyn MJ, Eberson CP. Adolescent patellar osteochondral fracture following patellar dislocation. Knee Surg Sports Traumatol Arthrosc. 2012;21(8):1856-61. [DOI] [PubMed] [Google Scholar]
- 69. Kreuz PC, Erggelet C, Steinwachs MR, Krause SJ, Lahm A, Niemeyer P, et al. Is microfracture of chondral defects in the knee associated with different results in patients aged 40 years or younger? Arthroscopy. 2006;22(11):1180-6. [DOI] [PubMed] [Google Scholar]
- 70. Bentley G, Biant LC, Carrington RW, Akmal M, Goldberg A, Williams AM, et al. A prospective, randomised comparison of autologous chondrocyte implantation versus mosaicplasty for osteochondral defects in the knee. J Bone Joint Surg Br. 2003;85(2):223-30. [DOI] [PubMed] [Google Scholar]
- 71. Brittberg M, Lindahl A, Nilsson A, Ohlsson C, Isaksson O, Peterson L. Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. N Engl J Med. 1994;331(14):889-95. [DOI] [PubMed] [Google Scholar]
- 72. Gawęda K, Walawski J, Węgłowski R, Drelich M, Mazurkiewicz T. Early results of one-stage knee extensor realignment and autologous osteochondral grafting. Int Orthop. 2005;30(1):39-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Gigante A, Enea D, Greco F, Bait C, Denti M, Schonhuber H, et al. Distal realignment and patellar autologous chondrocyte implantation: mid-term results in a selected population. Knee Surg Sports Traumatol Arthrosc. 2008;17(1):2-10. [DOI] [PubMed] [Google Scholar]
- 74. Henderson IJ, Lavigne P. Periosteal autologous chondrocyte implantation for patellar chondral defect in patients with normal and abnormal patellar tracking. Knee. 2006;13(4):274-9. [DOI] [PubMed] [Google Scholar]
- 75. Gobbi A, Karnatzikos G, Kumar A. Long-term results after microfracture treatment for full-thickness knee chondral lesions in athletes. Knee Surg Sports Traumatol Arthrosc. Epub Sep 20, 2013. 10.1007/s00167-013-2676-8. [DOI] [PubMed] [Google Scholar]
- 76. Goyal D, Keyhani S, Lee EH, Hui JH. Evidence-based status of microfracture technique: a systematic review of level I and II studies. Arthroscopy. 2013;29(9):1579-88. [DOI] [PubMed] [Google Scholar]
- 77. Minas T, Gomoll AH, Rosenberger R, Royce RO, Bryant T. Increased failure rate of autologous chondrocyte implantation after previous treatment with marrow stimulation techniques. Am J Sports Med. 2009;37(5):902-8. [DOI] [PubMed] [Google Scholar]
- 78. Spahn G, Kirschbaum S. Operative treatment of deep chondral defects of the patella: results after abrasive arthroplasty and periosteal arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2005;13(5):352-6. [DOI] [PubMed] [Google Scholar]
- 79. Anders S, Volz M, Frick H, Gellissen J. Suppl 4: a randomized, controlled trial comparing autologous matrix-induced chondrogenesis (AMIC®) to microfracture: analysis of 1- and 2-year follow-up data of 2 centers. Open Orthop J. 2013;7:133-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Gigante A, Cecconi S, Calcagno S, Busilacchi A, Enea D. Arthroscopic knee cartilage repair with covered microfracture and bone marrow concentrate. Arthrosc Tech. 2012;1(2):e175-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Stanish WD, McCormack R, Forriol F, Mohtadi N, Pelet S, Desnoyers J, et al. Novel scaffold-based BST-CarGel treatment results in superior cartilage repair compared with microfracture in a randomized controlled trial. J Bone Joint Surg Am. 2013;95(18):1640-50. [DOI] [PubMed] [Google Scholar]
- 82. Nukavarapu SP, Dorcemus DL. Osteochondral tissue engineering: current strategies and challenges. Biotechnol Adv. 2013;31(5):706-21. [DOI] [PubMed] [Google Scholar]
- 83. Matricali GA, Dereymaeker GP, Luyten FP. Donor site morbidity after articular cartilage repair procedures: a review. Acta Orthop Belg. 2010;76(5):669-74. [PubMed] [Google Scholar]
- 84. Hangody L, Vásárhelyi G, Hangody LR, Sükösd Z, Tibay G, Bartha L, et al. Autologous osteochondral grafting—technique and long-term results. Injury. 2008;39(Suppl 1):S32-9. [DOI] [PubMed] [Google Scholar]
- 85. Jamali AA, Emmerson BC, Chung C, Convery FR, Bugbee WD. Fresh osteochondral allografts. Clin Orthop Relat Res. 2005;(437):176-85. [PubMed] [Google Scholar]
- 86. Spak RT, Teitge RA. Fresh osteochondral allografts for patellofemoral arthritis. Clin Orthop Relat Res. 2006;(443):193-200. [DOI] [PubMed] [Google Scholar]
- 87. Peterson L, Brittberg M, Kiviranta I, Akerlund EL, Lindahl A. Autologous chondrocyte transplantation. Biomechanics and long-term durability. Am J Sports Med. 2002;30(1):2-12. [DOI] [PubMed] [Google Scholar]
- 88. Goyal D, Goyal A, Keyhani S, Lee EH, Hui JH. Evidence-based status of second- and third-generation autologous chondrocyte implantation over first generation: a systematic review of level I and II studies. Arthroscopy. 2013;29(11):1872-8. [DOI] [PubMed] [Google Scholar]
- 89. Gobbi A, Kon E, Berruto M, Filardo G, Delcogliano M, Boldrini L, et al. Patellofemoral full-thickness chondral defects treated with second-generation autologous chondrocyte implantation: results at 5 years’ follow-up. Am J Sports Med. 2009;37(6):1083-92. [DOI] [PubMed] [Google Scholar]
- 90. Filardo G, Kon E, Andriolo L, Di Martino A, Zaffagnini S, Marcacci M. Treatment of “patellofemoral” cartilage lesions with matrix-assisted autologous chondrocyte transplantation: a comparison of patellar and trochlear lesions. Am J Sports Med. 2014;42(3):626-34. [DOI] [PubMed] [Google Scholar]
- 91. Kreuz PC, Muller S, von Keudell A, Tischer T, Kaps C, Niemeyer P, et al. Influence of sex on the outcome of autologous chondrocyte implantation in chondral defects of the knee. Am J Sports Med. 2013;41(7):1541-8. [DOI] [PubMed] [Google Scholar]
- 92. Filardo G, Kon E, Andriolo L, Vannini F, Buda R, Ferruzzi A, et al. Does patient sex influence cartilage surgery outcome? Analysis of results at 5-year follow-up in a large cohort of patients treated with matrix-assisted autologous chondrocyte transplantation. Am J Sports Med. 2013;41(8):1827-34. [DOI] [PubMed] [Google Scholar]
- 93. Pascual-Garrido C, Slabaugh MA, L’Heureux DR, Friel NA, Cole BJ. Recommendations and treatment outcomes for patellofemoral articular cartilage defects with autologous chondrocyte implantation: prospective evaluation at average 4-year follow-up. Am J Sports Med. 2009;37(1 Suppl):33S-41S. [DOI] [PubMed] [Google Scholar]
- 94. Petrera M, De Croos JNA, Iu J, Hurtig M, Kandel RA, Theodoropoulos JS. Supplementation with platelet-rich plasma improves the in vitro formation of tissue-engineered cartilage with enhanced mechanical properties. Arthroscopy. 2013;29(10):1685-92. [DOI] [PubMed] [Google Scholar]
- 95. Niemeyer P, Steinwachs M, Erggelet C, Kreuz PC, Kraft N, Köstler W, et al. Autologous chondrocyte implantation for the treatment of retropatellar cartilage defects: clinical results referred to defect localisation. Arch Orthop Trauma Surg. 2007;128(11):1223-31. [DOI] [PubMed] [Google Scholar]
- 96. Niemeyer P, Kreuz PC, Steinwachs M, Köstler W, Mehlhorn A, Kraft N, et al. Technical note: the “double eye” technique as a modification of autologous chondrocyte implantation for the treatment of retropatellar cartilage defects. Knee Surg Sports Traumatol Arthrosc. 2007;15(12):1461-8. [DOI] [PubMed] [Google Scholar]
- 97. Pidoriano AJ, Weinstein RN, Buuck DA, Fulkerson JP. Correlation of patellar articular lesions with results from anteromedial tibial tubercle transfer. Am J Sports Med. 1997;25(4):533-7. [DOI] [PubMed] [Google Scholar]
- 98. Trinh TQ, Harris JD, Siston RA, Flanigan DC. Improved outcomes with combined autologous chondrocyte implantation and patellofemoral osteotomy versus isolated autologous chondrocyte implantation. Arthroscopy. 2013;29(3):566-74. [DOI] [PubMed] [Google Scholar]
- 99. Vasiliadis HS, Lindahl A, Georgoulis AD, Peterson L. Malalignment and cartilage lesions in the patellofemoral joint treated with autologous chondrocyte implantation. Knee Surg Sports Traumatol Arthrosc. 2011;19:452-7. [DOI] [PubMed] [Google Scholar]
- 100. Leadbetter WB, Mont MA. Patellofemoral arthroplasty: a useful option for recalcitrant symptomatic patellofemoral arthritis. Semin Arthroplast. 2009;20(3):148-60. [Google Scholar]
- 101. Natoli RM, Athanasiou KA. Traumatic loading of articular cartilage: mechanical and biological responses and post-injury treatment. Biorheology. 2009;46(6):451-85. [DOI] [PubMed] [Google Scholar]
- 102. Zaslav K, McAdams T, Scopp J, Theosadakis J, Mahajan V, Gobbi A. New frontiers for cartilage repair and protection. Cartilage. 2011;3(1 Suppl):77S-86S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Anderson DD, Chubinskaya S, Guilak F, Martin JA, Oegema TR, Olson SA, et al. Post-traumatic osteoarthritis: improved understanding and opportunities for early intervention. J Orthop Res. 2011;29(6):802-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Rundell SA, Baars DC, Phillips DM, Haut RC. The limitation of acute necrosis in retro-patellar cartilage after a severe blunt impact to the in vivo rabbit patello-femoral joint. J Orthop Res. 2005;23(6):1363-9. [DOI] [PubMed] [Google Scholar]
- 105. Martin JA. N-Acetylcysteine inhibits post-impact chondrocyte death in osteochondral explants. J Bone Joint Surg Am. 2009;91(8):1890-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Hurtig M, Chubinskaya S, Dickey J, Rueger D. BMP-7 protects against progression of cartilage degeneration after impact injury. J Orthop Res. 2009;27(5):602-11. [DOI] [PubMed] [Google Scholar]
- 107. D’Lima DD, Hashimoto S, Chen PC, Lotz MK, Colwell CW., Jr. Prevention of chondrocyte apoptosis. J Bone Joint Surg Am. 2001;83(2 Suppl 1):S25-6. [DOI] [PubMed] [Google Scholar]
- 108. Pascual-Garrido C, Hakimiyan AA, Rappoport L, Oegema TR, Wimmer MA, Chubinskaya S. Anti-apoptotic treatments prevent cartilage degradation after acute trauma to human ankle cartilage. Osteoarthritis Cartilage. 2009;17(9):1244-51. [DOI] [PMC free article] [PubMed] [Google Scholar]