Abstract
Objective
To investigate the effects of weight reduction on foot structure, gait, and dynamic plantar loading in obese adults.
Design
In a 3-month randomized-controlled trial, participants were randomized to receive either a weight loss intervention based on portion-controlled meals or a delayed-treatment control.
Participants
41 adults (32 F, 9 M) with a mean + SD age of 56.2 + 4.7 years and a BMI of 35.9 + 4.2 kg/m2.
Measurements
Arch Height Index (AHI), Malleolar Valgus Index (MVI), spatial and temporal gait parameters, plantar peak pressure (PP) and weight were measured at baseline, 3, and 6 months.
Results
The intervention group experienced significantly greater weight loss than did the control group (5.9 ± 4.0 kg versus 1.9 ± 3.2 kg, p = 0.001) after 3 months. There were no differences between the groups in anatomical foot structure or gait. However, the treatment group showed a significantly reduced PP than the control group beneath the lateral arch and the metatarsals 4 (all P values < .05) at 3 months. The change in PP correlated significantly with the change in weight at the metatarsal 2 (r=0.57, p=0.0219), metatarsal 3 (r=0.56, p=0.0064) and the medial arch (r=0.26, p<0.0001) at 6 months.
Conclusion
This was the first RCT designed to assess the effects of weight loss on foot structure, gait, and plantar loading in obese adults. Even a modest weight loss significantly reduced the dynamic plantar loading in obese adults. However, weight loss appeared to have no effects on foot structure and gait.
Keywords: Obesity, weight loss, gait, foot biomechanics, dynamic plantar pressure
INTRODUCTION
Over two thirds of Americans are at least overweight and one third is obese [1]. Globally, obesity has nearly doubled since 1980 [2]. In addition to being a major risk factor for heart disease, diabetes, diminished quality of life, and increased mortality, obesity can have a profound impact on mobility [3, 4].
Obesity accelerates the progression of knee osteoarthritis in the presence of moderate knee malalignment [5–9]. Based on a systematic review of 25 studies, Butterworth and colleagues noted an association between higher body mass index (BMI) and higher rates of chronic heel pain, non-specific foot pain, and tendonitis [10]. Population-based studies suggest that the prevalence of significant foot pain is about 20% [11, 12]. Foot pain was associated with age (50 years or older), gender (female), obesity, and presence of other pain (knee, hip, and lower back pain) [11]. Increased forces and aberrant foot biomechanics may explain the association between obesity and foot pain. A case-controlled study of 80 subjects with chronic heel pain syndrome and 80 age- and gender-matched control subjects found that those with chronic heel pain syndrome were three times more likely to be obese and four times more likely be flatfooted [13].
Studies have shown significant differences in gait and plantar loading between obese and normal weight individuals. A three dimensional gait analysis of obese young Chinese adults revealed that the stride length was significantly shorter and the stance phase and the double support phase of gait were significantly longer in obese (n = 14 with mean age of 35.4 years and BMI of 33.1 kg/m2) than in normal-weight (n = 14 with mean age of 27.6 years and BMI of 21.3 kg/m2) group [14]. A number of other cross-sectional studies showed that plantar pressure was higher in obese subjects compared to non-obese controls, both in standing and walking conditions [15–18].
To date, all published studies examining the relationship between obesity and plantar pressure have been cross sectional and associative. No studies have prospectively examined the effects of weight change on foot structure and function in a randomized controlled trial (RCT). Such data are need to better elucidate the relationship between body weight and lower extremity biomechanics and to inform patients and practitioners whether weight loss can be expected to improve foot structure and function. Therefore, this exploratory RCT was conducted to objectively examine the effects of weight loss on foot structure, temporal and spatial gait parameters, and dynamic plantar loading in obese adults.
SUBJECTS AND METHODS
Participants
Participants were 41 persons (32 women, 9 men) with a mean ± SD age of 56.2 ± 4.7 years and a BMI of 35.9 ± 4.2 kg/m2 (Table 1). Inclusion criteria were ages 50 to 75 years, BMI of 30–45 kg/m2, and body weight of less than 136 kg (due to limitation of optical foot scanner). Participants were excluded if they had any of the followings: diabetes, uncontrolled hypertension (defined as a blood pressure > 180/100 mm Hg), uncontrolled dyslipidemia (triglycerides > 500 mg), established cardiovascular disease or an inflammatory condition, participated in another formal weight loss program within past 6 months, history of using weight-loss inducing medications or dietary supplements within 6 months prior to enrollment, weight loss > 5 kg during the last 6 months, history of surgical or device treatment for obesity, history of alcohol or drug abuse, smoker or tobacco users, major mood disorder, unable to ambulate safely without the use of walking aid, or were unable or unwilling to eat pre-packaged meals. Those with history of surgery on the back, hips, knees, ankles, or feet were also excluded. Baseline characteristics of the sample are described in Table 1.
Table 1.
Baseline Characteristics and Change at 3-months
| Parameters, Baseline and Change at 3 months | Control | Treatment | P-value | ||
|---|---|---|---|---|---|
| Mean | SE | Mean | SE | ||
| Age (years) | 56.25 | 1.29 | 56.24 | 0.80 | 0.9937 |
| N (female) | 20 (15) | 21 (17) | 0.7186 | ||
| Race: White/Black/Hispanic | 7/12/1 | 7/13/1 | 0.9922 | ||
| Education: HS/College/Grad | 8/6/6 | 8/7/6 | 0.7664 | ||
| Body weight (kg) | 99.45 | 3.77 | 99.67 | 2.80 | 0.9632 |
| Δ Body weight (kg) | −1.89 | −0.81 | −5.93 | −0.78 | 0.001 |
| Body Mass Index (kg/m2) | 35.77 | 0.89 | 36.12 | 0.99 | 0.7939 |
| Δ BMI (kg/m2) | −0.66 | −0.29 | −2.15 | −0.29 | 0.0008 |
| Malleolar Valgus Index (%) | 12.96 | 1.29 | 14.95 | 1.37 | 0.2982 |
| Δ MVI (%) | 0.08 | −0.65 | −1.16 | −0.63 | 0.0376 |
| Arch height index, sitting | 0.35 | 0.01 | 0.34 | 0.01 | 0.3876 |
| Δ AHI sitting | 0.00 | 0.00 | −0.01 | 0.00 | 0.2928 |
| Arch height index, standing | 0.32 | 0.01 | 0.31 | 0.01 | 0.592 |
| Δ AHI standing | 0.00 | 0.00 | 0.00 | 0.00 | 0.6933 |
| Arch height flexibility (mm/kN) | 12.62 | 1.01 | 11.54 | 1.02 | 0.4555 |
| Δ AHF (mm/kN) | 1.29 | −0.91 | −0.62 | −0.89 | 0.1424 |
| Walking speed (m/s) | 0.96 | 0.18 | 0.96 | 0.16 | 0.9276 |
| Δ speed (m/s) | 0.06 | −0.02 | 0.04 | −0.02 | 0.3681 |
| Stride length (m) | 1.100 | 0.120 | 1.030 | 0.250 | 0.2524 |
| Δ Stride length (m) | 0.040 | −0.019 | 0.051 | −0.018 | 0.6981 |
| Support base (m) | 0.24 | 0.06 | 0.23 | 0.05 | 0.8606 |
| Δ Support base | 0.003 | −0.005 | −0.019 | −0.005 | 0.0017 |
| Double support time (s) | 0.019 | 0.006 | 0.011 | 0.006 | 0.3418 |
| Δ double support time | −0.038 | −0.015 | −0.021 | −0.010 | 0.2672 |
| Stance phase (%, gait cycle) | 61.84 | 0.34 | 62.65 | 0.42 | 0.3985 |
| Δ percent stance | −1.17 | −1.47 | 1.80 | −1.43 | 0.1558 |
| Cadence (steps/min) | 104.14 | 1.91 | 106.84 | 2.36 | <0.0001 |
| Δ Cadence (steps/min) | 2.80 | −1.14 | 0.07 | −1.11 | 0.1970 |
Analysis was limited to left foot only. Mean and SE at baseline and the mean change and SE at 3 months from the baseline are shown. Negative numbers indicate a decrease at 3-months. Malleolar Valgus Index (MVI) is a measure of hindfoot valgus alignment in resting stance. Arch Height Index (AHI) is the ratio of arch height at half the foot length and the truncated foot length – distance from the heel to the first metatarsal phalangeal joint. Arch height flexibility (mm/kN) is defined as (arch height in sitting –arch height in standing) / (body weight * 0.4)
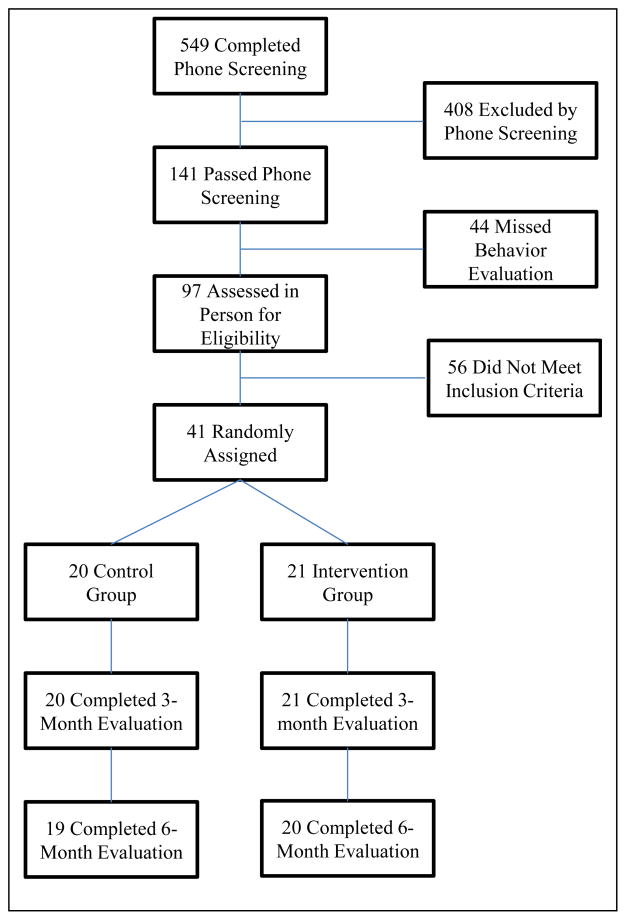
Participant flow for this study is shown in Figure 1. Participants who appeared, via scripted phone screen, to meet eligibility requirements were scheduled to meet with research staff. The staff described the study’s nature and requirements, assessed suitability for participation, and obtained written informed consent. Temple University’s Institutional Review Board approved the protocol.
Figure 1.
Participant Flow chart
Design
Participants were randomly assigned, via stratified randomization procedure based on their BMI (30–39 and 40–45), to either a 3-month weight loss intervention or a delayed treatment control as described below. After 3 months, the control group received a weight loss intervention and the intervention group continued the same weight loss intervention. Postural foot structure, gait, and dynamic plantar pressure in gait were assessed on all participants at baseline, at end of 3 months and 6 months. Primary comparison was at 3 months.
Treatment Group (N= 21)
An experienced group leader (MPH or RD) provided educational sessions in groups of 8–11 participants. Educational sessions consisted of materials specific to making behavioral changes towards weight loss and weight maintenance. Participants received information on diet, exercise, nutrition and related topics. Participants were prescribed energy intakes of 1200–1500 kcal/d (women) and 1500–1800 kcal/d (men) and instructed on behavioral methods for weight control (self-monitoring, stimulus control). Participants received commercially available pre-packaged portion-controlled meals and snacks (NutriSystem, Inc., Fort Washington, PA) and met weekly for group weight loss classes during months 1–3. Exercise was addressed in group sessions and encouraged but was not formally measured due to safety concerns with the study population and the inability to perform exercise testing upon screening and throughout the study. Participants were instructed to engage in physical activity of their choice, typically walking, starting with 40 minutes of physical activity a week and gradually increasing to 180 minutes a week. Participants continued on the NutriSystem meal plan for months 4–6 but only attended monthly group classes.
Control Group (n = 20)
Participants in the control group underwent monthly lifestyle support and education classes during months 1–3 but did not receive portion-controlled pre-packaged meals. Educational sessions included one session each on diet/nutrition, exercise, and stress and time management. These sessions were informational and did not teach behavioral self-regulation skills. The goal was to offer a valuable educational experience to these participants and to respond to their interest in education and support, thereby helping to retain them in the trial. During months 4–6, participants received the NutriSystem portion-controlled pre-package meals and attended weekly group sessions.
Weight and height assessment
Body weight was measured to the nearest 0.1 kg using a digital scale (Seca, Model 882, Hanover, MD) while subjects wore light clothing and barefoot at baseline, 3 months, and 6 months. Height was measured to the nearest 0.1 cm with a Harpenden stadiometer (Holtain Ltd., Crosswell, UK) at baseline.
Structural foot assessment
Arch height and foot length were measured in sitting and standing positions, using a custom-made jig as previously described [19]. The Arch Height Index (AHI) is a ratio of the arch height at half the foot length and the truncated foot length – the distance from heel to the center of the first metatarsophalangeal joint. The arch height flexibility (AHF, mm/kN) was calculated as the difference in arch height from sitting to standing, normalized to change in load, estimated to be 40% of body weight.[20] The Malleolar Valgus Index (MVI), a measure of hindfoot alignment, was also assessed using a flatbed computer scanner at resolution of 100 dpi as previously described [21].
Gait and plantar pressure assessment
Walking speed, cadence, support base, and stride length of gait were measured while participants walked over the 3.8 meter GaitMat™II (E.Q., Inc., Chalfont) at their self-selected comfortable pace in barefoot. Gait parameters were calculated from the mean of four trials. Plantar pressures were collected using the novel emed®-X (novel GmbH, Munich) pressure platform with 4 sensors per square centimeter at 100 Hz. To assess dynamic plantar pressure during mid-gait, participants initiated their walk at a location such that the third step would land over the plantar pressure mat [22]. Four barefoot trials were collected for each foot. Using a novel 12-segment masking analysis, peak pressure (PP) was calculated for each region. This algorithm constructs 12 foot segments (toe 1, toe 2, toes 3–5, metatarsal 1, metatarsal 2, metatarsal 3, metatarsal 4, metatarsal 5, medial arch, lateral arch, medial heel, and lateral heel) based on foot geometry obtained from the maximum pressure throughout the stance phase of gait. In addition, the Center of Pressure Excursion Index (CPEI) was calculated from each trial using a custom-developed Windows program [21].
Statistical analysis
Between-group differences at baseline were assessed with independent-samples t-tests for continuous outcomes and the Pearson chi-square tests for categorical outcomes. Primary analyses were performed with the Analysis of Covariance (ANCOVA) using PROC MIXED in SAS v. 9.2 (SAS Institute Inc, Cary, NC). In the model, differences in change from baseline to 3 months were the outcome and the explanatory variables were a dichotomous indicator for treatment groups. All analysis followed intent-to-treat principle. Parallel slopes assumption was tested with interaction between baseline and treatment group. When the interaction term was significant, differences in treatment effects were evaluated at five levels of baseline values: minimum, 25th, 50th, 75th percentiles, and maximum. When the interaction term was not significant, differences in treatment effects were tested with baseline held fixed at a common mean. An intent-to-treat sensitivity analysis was also employed to assess the impact of missing data. A linear mixed model was constructed with PROC MIXED consisting of a continuous variable for visit, an indicator of treatment group and the visit by group interaction. For all analyses, statistical significance was set at p < 0.05.
For secondary analysis, treatment groups were combined and study participants were divided into three categories based on the percent of weight loss at 6 months: (A) <5%, (B) 5–10%, and (C) > 10%. Differences in change from baseline to 6 months among the three weight loss categories were also tested with the ANCOVA using PROC MIXED. Parallel slopes assumption was tested as an interaction of baseline variable by weight loss category. When the interaction was significant (p<0.05), follow-up pairwise comparisons were performed between groups holding baseline at five specific values: minimum, 25th percentile, 50th percentile (median), 75th percentile, and maximum. Pairwise p-values were adjusted for multiple comparisons with the Tukey method. Linear regression analysis was performed to evaluate the relationship between weight loss and change in dynamic plantar pressure in gait. All analyses were based on data from left feet only to avoid complicating the models with an additional within-subjects factor that was not expected to differentiate treatment groups.
RESULTS
Primary comparison of the control and treatment groups at 3 months
Attrition
All 41 participants successfully completed baseline and 3 months follow-up evaluations.
Body weight
Treatment group lost significantly more weight than the control group at 3 months (5.9 kg versus 1.9 kg; p = 0.001) (Table 1).
Foot structure
There was no significant difference between the groups on changes in the AHI or the AHF. The MVI decreased (became less valgus) by 1.16% in the treatment group while it is increased by 0.08% in the control group (p=0.04) at 3 months (Table 1).
Gait parameters
Treatment group showed significantly greater reduction than the control group in support base at 3 months (−1.9 cm versus 0.3 cm, p =0.002). There were no other significant between-group differences in changes in gait parameters (Table 1).
Dynamic barefoot plantar pressure
Treatment group showed significantly greater reductions than the control group in PP beneath metatarsal 4 and lateral arch at 3 months (Table 2). There was no significant difference between the control and treatment groups in change in the CPEI.
Table 2.
Peak Pressure (N/cm2) at baseline and Change in Peak Pressure at 3-months.
| Peak Pressure (N/cm2), Baseline | Control | Treatment | P-value | Post hoc | ||
|---|---|---|---|---|---|---|
| mean | SE | mean | SE | |||
| Total | 66.08 | 5.59 | 79.53 | 4.88 | 0.1077 | |
| Toe 1 | 54.62 | 5.62 | 50.97 | 6.65 | 0.0008 | |
| Toe 2 | 16.91 | 1.55 | 17.85 | 2.30 | 0.7575 | |
| Toes 3–5 | 12.08 | 1.33 | 12.83 | 2.13 | 0.1030 | |
| Metatarsal 1 | 34.48 | 5.17 | 41.92 | 5.46 | 0.2612 | |
| Metatarsal 2 | 43.55 | 4.04 | 55.80 | 6.48 | 0.4331 | |
| Metatarsal 3 | 38.54 | 4.07 | 45.36 | 4.21 | 0.0235 | |
| Metatarsal 4 | 30.89 | 2.98 | 31.85 | 3.09 | 0.9401 | |
| Metatarsal 5 | 21.69 | 2.81 | 32.22 | 4.99 | 0.2859 | |
| Medial Arch | 14.51 | 0.63 | 14.89 | 0.97 | 0.4498 | |
| Lateral Arch | 20.97 | 3.95 | 17.96 | 0.94 | 0.9350 | |
| Medial Heel | 26.10 | 1.92 | 31.97 | 2.62 | 0.7798 | |
| Lateral Heel | 25.05 | 1.59 | 28.64 | 1.75 | 0.5726 | |
| CPEI (%) | 10.35 | 0.75 | 9.44 | 1.29 | 0.6112 | |
| Change in 3 months | ||||||
| Total | −1.18 | −2.79 | −3.67 | −2.25 | 0.8228 | |
| Toe 1 | −2.13 | −3.11 | −4.80 | −2.16 | 0.2980 | |
| Toe 2 | 0.07 | −1.04 | −0.09 | −0.87 | 0.8957 | |
| Toes 3–5 | 1.04 | −1.39 | −0.02 | −0.79 | 0.1433* | max |
| Metatarsal 1 | −1.92 | −1.25 | 0.96 | −1.80 | 0.1504 | |
| Metatarsal 2 | 4.09 | −1.95 | −0.38 | −1.62 | 0.1751* | 75th, max |
| Metatarsal 3 | 0.54 | −0.99 | −1.25 | −1.75 | 0.6320 | |
| Metatarsal 4 | 2.33 | −1.87 | −3.00 | −1.18 | 0.0238* | 50th, 75th, max |
| Metatarsal 5 | 3.14 | −1.44 | −2.74 | −2.10 | 0.1066* | 75th, max |
| Medial Arch | −0.88 | −0.39 | −1.34 | −0.37 | 0.4311 | |
| Lateral Arch | 1.45 | −1.05 | −1.88 | −0.51 | 0.0417* | 50th, 75th, max |
| Medial Heel | 1.35 | −0.76 | 0.28 | −0.80 | 0.3258 | |
| Lateral Heel | 1.01 | −0.65 | 0.14 | −0.72 | 0.3247 | |
| CPEI (%) | 3.87 | −1.37 | 4.62 | −1.33 | 0.6984 | |
Note: Mean and SE of peak pressure in 12-regions of the left foot are shown.
indicates significant interactions between group at baseline. Therefore, differences between groups were evaluated at 5 baseline values: minimum, 25th, 50th, 75th percentiles, and maximum. Center of Pressure Excursion Index (CPEI, %) is a measure of lateral concavity of center of pressure. Smaller CPEI indicates greater pronatory foot function.
Secondary analysis: effects of weight loss at 6 months
Two subjects (one from each group) were lost to follow up during months 4–6. Baseline characteristics and changes at 6 months of the 3 weight loss categories (<5%, 5–10%, and >10%) are summarized in Table 3. Three weight loss categories consisted of 11, 13, and 15 participants who lost a mean of 2.0 kg, 7.4 kg, and 13.1 kg, respectively. There were no significant differences among the three weight categories in change in foot structure (AHI, AHF, and MVI). Significant differences were observed among the three weight loss categories in change in dynamic PP beneath metatarsal 2, metatarsal 3, medial and lateral arch, and medial heel (Table 4). Change in PP at 6-months correlated linearly with the change in weight in following locations: metatarsal 2 (r=0.57, p=0.0219), metatarsal 3 (r=0.56, p=0.0064) and medial arch (r=0.26, p<0.0001).
Table 3.
Baseline characteristics and change at 6-months across 3 weight loss categories
| Parameters, Baseline and Change at 6 months | <5% | 5–10% | >10% | P-value | Post hoc | |||
|---|---|---|---|---|---|---|---|---|
| Mean | SE | Mean | SE | Mean | SE | |||
| Age (years) | 57.82 | 2.20 | 57.92 | 0.90 | 54.07 | 0.61 | 0.0500 | |
| N (female) | 11 (9) | 13 (12) | 15 (9) | 0.1164 | ||||
| Body weight (kg) | 99.88 | 5.58 | 99.13 | 3.36 | 99.58 | 4.08 | 0.9928 | |
| Δ Body weight (kg) | −2.0 | −2.2 | −7.4 | −1.5 | −13.1 | −2.8 | <0.001 | |
| Body Mass Index (kg/m2) | 36.14 | 1.28 | 36.42 | 1.15 | 35.18 | 1.20 | 0.7359 | |
| Δ BMI (kg/m2) | −0.72 | −0.76 | −2.7 | −0.05 | −4.6 | −0.8 | <0.001 | |
| Malleolar Valgus Index (%) | 13.80 | 2.00 | 14.58 | 1.67 | 13.85 | 1.66 | 0.7785 | |
| Δ MVI (%) | 0.74 | −1.01 | −2.76 | −0.97 | −0.70 | −0.86 | 0.0547 | |
| Arch height index, sitting | 0.34 | 0.01 | 0.34 | 0.01 | 0.34 | 0.01 | 0.9589 | |
| Δ AHI, sitting | −0.00 | −0.01 | 0.00 | −0.01 | 0.00 | 0.00 | 0.9479 | |
| Arch height index, standing | 0.31 | 0.01 | 0.31 | 0.01 | 0.31 | 0.01 | 0.9911 | |
| Δ AHI, standing | 0.00 | −0.01 | 0.00 | −0.01 | 0.00 | 0.00 | 0.7477 | |
| Arch height flexibility (mm/kN) | 11.06 | 1.47 | 12.76 | 1.44 | 12.47 | 0.97 | 0.6342 | |
| Δ AHF (mm/kN) | −0.09 | −1.26 | 0.47 | −1.15 | 0.47 | −1.07 | 0.9309 | |
| Walking speed (m/s) | 0.94 | 0.18 | 0.92 | 0.18 | 1.02 | 0.12 | 0.1380* | |
| Δ speed, min | 0.28 | −0.02 | 0.22 | −0.07 | −0.21 | −0.12 | X, Z | |
| Δ speed, 25th | 0.16 | −0.04 | 0.11 | −0.03 | −0.04 | −0.05 | X, Z | |
| Stride length (m) | 1.022 | 0.058 | 1.198 | 0.653 | 1.166 | 0.032 | 0.0456* | |
| Δ, min | 0.27 | −0.07 | 0.24 | −0.06 | −0.25 | −0.09 | X, Z | |
| Δ, 25th | 0.10 | −0.03 | 0.08 | −0.02 | −0.06 | −0.04 | X, Z | |
| Δ, max | −0.10 | −0.07 | −0.12 | −0.06 | 0.16 | −0.05 | X, Z | |
| Support base (m) | 0.239 | 0.015 | 0.235 | 0.015 | 0.236 | 0.015 | 0.9845 | |
| Δ Support base | −0.014 | −0.006 | −0.018 | −0.005 | −0.026 | −0.005 | 0.2947 | |
| Double support time (s) | 0.161 | 0.022 | 0.178 | 0.038 | 0.159 | 0.018 | 0.5653 | |
| Δ double support time | −0.027 | −0.014 | −0.014 | −0.013 | 0.004 | −0.012 | 0.2133 | |
| Stance phase (%, gait cycle) | 62.015 | 0.414 | 62.487 | 0.537 | 62.246 | 0.525 | 0.8312 | |
| Δ stance phase | −3.151 | −2.883 | −1.556 | −2.659 | 2.520 | −2.486 | 0.3063 | |
| Cadence (steps/min) | 105.8 | 4.0 | 105.8 | 2.5 | 106.1 | 2.0 | <0.0001 | |
| Δ Cadence (steps/min) | 3.61 | −1.49 | 1.63 | −1.37 | 0.42 | −1.28 | 0.2812 | |
Note: Comparison of left side only. Δ indicates changes from the baseline to 6-months. Mean and SE are shown for baseline and the change at 6 month. Negative numbers indicate decrease at 6 months, as compared to the baseline.
indicates significant interactions between weight loss categories at baseline. Therefore, differences between groups were evaluated at 5 baseline values: minimum, 25th, 50th, 75th percentiles, and maximum. Post hoc notation: X = a significant difference between <5% versus >10%, Y between <5% versus 5–10%, Z between 5–10% versus >10% weight loss categories. Malleolar Valgus Index (MVI) is a measure of hindfoot valgus alignment in resting stance. Arch Height Index (AHI) is the ratio of arch height at half the foot length and the truncated foot length. Arch height flexibility (mm/kN) is defined as (arch height in sitting –arch height in standing) / (body weight * 0.4)
Table 4.
Peak Pressure and Δ Peak Pressure at 6-months across 3 weight loss categories
| Peak pressure (N/cm2) Baseline | <5% | 5–10% | >10% | P-value | post hoc | |||
|---|---|---|---|---|---|---|---|---|
| Mean | SE | Mean | SE | Mean | SE | |||
| Total | 73.52 | 7.46 | 71.06 | 7.67 | 75.58 | 6.21 | 0.2056 | |
| Toe 1 | 51.82 | 11.08 | 50.58 | 7.05 | 54.86 | 6.58 | 0.1254 | |
| Toe 2 | 16.2 | 2.62 | 16.83 | 2.48 | 18.46 | 2.51 | 0.1154 | |
| Toe 3–5 | 10.98 | 1.83 | 10.38 | 1.44 | 15.33 | 2.83 | 0.7423 | |
| Metatarsal 1 | 28.14 | 5.14 | 41.09 | 6.15 | 45.13 | 7.58 | 0.8051 | |
| Metatarsal 2 | 43.72 | 5.15 | 53.96 | 8.4 | 52.54 | 6.92 | 0.6005 | |
| Metatarsal 3 | 44.01 | 7.14 | 39.4 | 4.88 | 45.04 | 4.39 | 0.5324 | |
| Metatarsal 4 | 28.49 | 2.68 | 34.31 | 5.65 | 32.5 | 2.3 | 0.3083 | |
| Metatarsal 5 | 28.39 | 6.51 | 22.37 | 3.95 | 31.1 | 5.66 | 0.6363 | |
| Medial arch | 15.35 | 1.12 | 14.9 | 1.39 | 14.12 | 0.54 | 0.3033 | |
| Lateral arch | 16.93 | 1.21 | 24.82 | 5.81 | 17.03 | 1.35 | 0.0258 | |
| Medial heel | 26.2 | 2.5 | 29.68 | 3.31 | 31.48 | 2.87 | 0.0047 | |
| Lateral heel | 25.29 | 2.41 | 26.81 | 2.45 | 28.71 | 1.72 | 0.3878 | |
| CPEI (%) | 8.53 | 1.58 | 11.14 | 0.88 | 9.26 | 1.44 | 0.6122 | |
| Change at 6 months | ||||||||
| Total | 1.27 | −3.59 | 2.85 | −3.04 | 5.31 | −3.33 | 0.6472 | |
| Toe 1 | −3.64 | −3.4 | 1.27 | −2.93 | −0.53 | −3.85 | 0.6317 | |
| Toe 2 | 1.25 | −1.71 | 2.62 | −1.7 | 1.38 | −0.97 | 0.7196 | |
| Toe 3–5 | 0.26 | −1.47 | 0.82 | −0.88 | 0.51 | −0.83 | 0.4714 | |
| Metatarsal 1 | 1.97 | −2.76 | 1.76 | −4.61 | 1.03 | −3.16 | 0.9909 | |
| Metatarsal 2 | 6.77 | −2.71 | 1.56 | −1.81 | −2 | −1.64 | 0.0222* | X |
| Metatarsal 3 | 4.27 | −1.97 | 0.88 | −1.95 | −2.2 | −1.33 | 0.0467* | X |
| Metatarsal 4 | 1.45 | −1.82 | −0.3 | −2.68 | −1.7 | −1.42 | 0.6593 | |
| Metatarsal 5 | −0.70 | −3.31 | 0.56 | −1.92 | 3.17 | −3.14 | 0.3186 | |
| Medial arch | 0.41 | −0.52 | −1.03 | −0.46 | −2.97 | −0.43 | <.0001* | X, Z |
| Lateral arch | 0.93 | −0.9 | −0.35 | −1.9 | −0.19 | −1.56 | 0.0066* | |
| min | 2.79 | −2.34 | −4.15 | −1.26 | −6.01 | −1.54 | X, Y | |
| 25th | 1.49 | −1.32 | −2.98 | −1.14 | −2.04 | −1.03 | Y | |
| 75th | 0.00 | −1.55 | −1.62 | −1.05 | 2.56 | −1.11 | Z | |
| max | −21.69 | −24.69 | 18.06 | −3.65 | 69.21 | −14.45 | X, Z | |
| Medial heel | 2.39 | −0.92 | 0.73 | −1.16 | 2.35 | −1.97 | 0.0464* | |
| max | 7.83 | −6.30 | 2.72 | −3.38 | 16.02 | −3.16 | Z | |
| Lateral heel | 1.68 | −0.47 | 0.02 | −0.82 | 0.28 | −0.91 | 0.1325 | |
| CPEI (%) | 4.56 | −1.84 | 4.13 | −1.70 | 4.14 | −1.56 | 0.9811 | |
Note: Mean and SE of peak pressure in 12-regions of the left foot are shown.
indicates significant interactions between 3 weight loss categories at baseline. Therefore, differences between groups were evaluated at 5 baseline values: minimum, 25th, 50th, 75th percentiles, and maximum. Center of Pressure Excursion Index (CPEI, %) is a measure of lateral concavity of center of pressure. Smaller CPEI indicates greater pronatory foot function. Post hoc notation: X = a significant difference between <5% versus >10%, Y between <5% versus 5–10%, Z between 5–10% versus >10% weight loss categories.
Discussion
This is the first RCT to examine the effects of weight loss on plantar pressure and foot structure. As expected, weekly behavior modification sessions with portion-controlled meals yielded significant weight loss (the mean between-group difference of 4.0 kg) at 3 months. At the end of 6 months, 15 of 39 participants experienced over 10% weight loss while 11 subjects experienced less than 5% of their baseline weight.
Comparing to the previously published references [20, 21], baseline AHI and MVI indicate that the study participants had planus (flat) foot type. Since this study was limited to a small sample size and lacked the normal-weighted control group, it is not clear if the prevalence of flatfoot is associated with obesity, aging or other factors. While the MVI decreased (became less valgus) in the treatment group at 3 months, the change was minimal (1.6%) and most likely not clinically meaningful. No significant difference in change in foot structure measures (AHI and MVI) was observed between the control and treatment groups at 3 months or among the three different weight loss categories at 6 months. One explanation may be that modest weight loss observed in this pilot study was insufficient to restore the foot structure. Alternatively, flatfoot morphology of obese adults may persist even after weight loss, similar to the permanent foot structural changes that occur during pregnancy [23]. Effects of weight gain on foot structure may be different and warrant additional studies.
In gait pattern, treatment group showed significantly narrower support base (1.9 cm) during comfortable-paced walking at 3 months. While this reduction represents only 7.9% of the mean support base of the study participants at baseline, it represents about 33% of the mean support base of healthy non-obese subjects (unpublished data of 61 asymptomatic healthy subjects with mean ± SD age of 35.7 ± 12.07 years and BMI of 23.5 ± 3.75 kg/m2). Although it was not directly measured, decreased thigh girth may have contributed to smaller support base. Decreased support base did not translate into a significant between-group difference in change of walking speed.
Studies have supported the hypothesis that the body weight is associated with dynamic plantar pressure in gait. Obese adults exhibited significantly greater dynamic peak plantar pressure than non-obese adults, with highest PPs localized to the second metatarsal head and hallux [16]. Additionally, temporary placement of 9.1 kg and 18.2 kg weight evenly on the front and back of workout vest on 19 healthy asymptomatic young subjects (31.1 years old) with BMI of 24.2 kg/m2 increased in-shoe PP in all 4 regions (metatarsal 1, metatarsals 2–4, midfoot, and heel) significantly, incrementally, and uniformly [18]. Finally, PP reductions of 9.6, 5.0, and 5.0 N/cm2 were observed under the hallux, the metatarsal head 3, and the metatarsal head 4, respectively following a weight loss intervention on 9 subjects, who lost an average of 19.4 kg [24]. On the other hand, Hillstrom et al showed that biomechanical foot structure can influence dynamic plantar pressure distribution. Specifically, adults with flatfoot exhibited the highest PP at the second metatarsal head and hallux, which was significantly higher than subjects with rectus and cavus foot types [20]. Also, subjects with planus foot type showed a relatively smaller PP under the metatarsal head 1, representing 66% of the PP beneath the metatarsal head 2, than subjects with rectus and cavus foot types.
A number of differences in method and subject characteristics limit direct comparison of the above studies with the current study. Nevertheless, the magnitude and location of PP observed in this study at baseline are similar to those reported by Hill et al. in healthy young obese subjects [17] as well as subjects with flatfoot [20]. Specifically, highest PPs were noted under the second metatarsal head and hallux. The CPEI further suggests that the study participants’ dynamic plantar pressure distribution most closely resembles those subjects with flatfoot. Although the amount of weight loss observed in this study was modest, even moderate weight loss yielded a significant reduction in dynamic PP. Significant PP reduction was not uniform but rather limited to lateral foot (4th metatarsal and lateral arch) at 3 months in the treatment group. In the secondary analysis at 6 months, reduction in PP correlated linearly with the magnitude of weight loss beneath the metatarsals 2 and 3 and the medial arch. These findings are consistent with findings of Hills et al, who observed that BMI was correlated linearly with midfoot PP (r2=0.66). While it is not yet clear which factors attribute to location-specific PP changes, the magnitude of weight loss and the underlying biomechanical foot type may influence these changes in plantar loading.
This was the first prospective RCT designed to explore the effects of weight loss on foot structure, gait, and plantar pressure. This study was limited to asymptomatic obese adults with no significant musculoskeletal disabilities or pain. Small sample size, stringent subject criteria, modest weight loss, and short follow up period limit the clinical utility of this exploratory study. Participants’ foot structure and function most closely resemble those subjects with flatfoot. While no significant and clinically meaningful change was noted on foot structure and gait parameters, the results showed that even a modest weight reduction can yield significant reduction in plantar loading. These dynamic plantar load alterations that accompanied moderate weight loss did not occur uniformly throughout the foot but rather specific to certain regions of the foot in this group of participants with planus foot type. Additional studies are needed to examine the prevalence of foot pain/disability in obese subjects, the role of specific footwear and exercise program, and the significance of foot disability on adherence to healthy lifestyle.
Research highlights.
We conducted a randomized controlled trial on 41 obese adults.
We examined effects of weight loss on foot structure and function.
The intervention group lost 4.0 kg more weight than the control group at 3 months.
No significant difference was noted in change in foot structure.
Even modest weight loss yielded a significant reduction in dynamic plantar pressure.
Acknowledgments
This study was supported by the NIH grant K23DK081021 to Dr. Song and an internal grant from the Temple University’s Center for Obesity and Research.
Footnotes
Conflict of Interest Statements
Dr. Gary Foster was a member of scientific advisor for the Nutrisystem. All other authors declare no potential conflict of interest.
This study has been approved by the Temple University IRB. Nutrisystem Inc. provided the portion-controlled meals for the intervention group.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Flegal KM, et al. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307(5):491–7. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 2.Obesity and overweight: Fact sheets. 2013 Mar; Available from: http://www.who.int/mediacentre/factsheets/fs311/en/
- 3.Doll HA, Petersen SE, Stewart-Brown SL. Obesity and physical and emotional well-being: associations between body mass index, chronic illness, and the physical and mental components of the SF-36 questionnaire. Obes Res. 2000;8(2):160–70. doi: 10.1038/oby.2000.17. [DOI] [PubMed] [Google Scholar]
- 4.Kushner RF, Foster GD. Obesity and quality of life. Nutrition. 2000;16(10):947–52. doi: 10.1016/s0899-9007(00)00404-4. [DOI] [PubMed] [Google Scholar]
- 5.Nguyen US, et al. Increasing prevalence of knee pain and symptomatic knee osteoarthritis: survey and cohort data. Ann Intern Med. 2011;155(11):725–32. doi: 10.1059/0003-4819-155-11-201112060-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Niu J, et al. Is obesity a risk factor for progressive radiographic knee osteoarthritis? Arthritis Rheum. 2009;61(3):329–35. doi: 10.1002/art.24337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Felson DT, et al. The effect of body weight on progression of knee osteoarthritis is dependent on alignment. Arthritis Rheum. 2004;50(12):3904–9. doi: 10.1002/art.20726. [DOI] [PubMed] [Google Scholar]
- 8.Reijman M, et al. Body mass index associated with onset and progression of osteoarthritis of the knee but not of the hip: the Rotterdam Study. Ann Rheum Dis. 2007;66(2):158–62. doi: 10.1136/ard.2006.053538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Powell A, et al. Obesity: a preventable risk factor for large joint osteoarthritis which may act through biomechanical factors. Br J Sports Med. 2005;39(1):4–5. doi: 10.1136/bjsm.2004.011841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Butterworth PA, et al. The association between body mass index and musculoskeletal foot disorders: a systematic review. Obes Rev. 2012;13(7):630–42. doi: 10.1111/j.1467-789X.2012.00996.x. [DOI] [PubMed] [Google Scholar]
- 11.Hill CL, et al. Prevalence and correlates of foot pain in a population-based study: the North West Adelaide health study. J Foot Ankle Res. 2008;1(1):2. doi: 10.1186/1757-1146-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thomas E, et al. The prevalence of pain and pain interference in a general population of older adults: cross-sectional findings from the North Staffordshire Osteoarthritis Project (NorStOP) Pain. 2004;110(1–2):361–8. doi: 10.1016/j.pain.2004.04.017. [DOI] [PubMed] [Google Scholar]
- 13.Irving DB, et al. Obesity and pronated foot type may increase the risk of chronic plantar heel pain: a matched case-control study. BMC Musculoskelet Disord. 2007;8:41. doi: 10.1186/1471-2474-8-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lai PP, et al. Three-dimensional gait analysis of obese adults. Clin Biomech (Bristol, Avon) 2008;23(Suppl 1):S2–6. doi: 10.1016/j.clinbiomech.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 15.Fabris SM, et al. Computerized baropodometry in obese patients. Obes Surg. 2006;16(12):1574–8. doi: 10.1381/096089206779319293. [DOI] [PubMed] [Google Scholar]
- 16.Birtane M, Tuna H. The evaluation of plantar pressure distribution in obese and non-obese adults. Clin Biomech (Bristol, Avon) 2004;19(10):1055–9. doi: 10.1016/j.clinbiomech.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 17.Hills AP, et al. Plantar pressure differences between obese and non-obese adults: a biomechanical analysis. Int J Obes Relat Metab Disord. 2001;25(11):1674–9. doi: 10.1038/sj.ijo.0801785. [DOI] [PubMed] [Google Scholar]
- 18.Vela SA, et al. The effect of increased weight on peak pressures: implications for obesity and diabetic foot pathology. J Foot Ankle Surg. 1998;37(5):416–20. doi: 10.1016/s1067-2516(98)80051-3. discussion 448–9. [DOI] [PubMed] [Google Scholar]
- 19.Butler RJ, et al. Arch height index measurement system: establishment of reliability and normative values. J Am Podiatr Med Assoc. 2008;98(2):102–6. doi: 10.7547/0980102. [DOI] [PubMed] [Google Scholar]
- 20.Hillstrom HJ, et al. Foot type biomechanics part 1: structure and function of the asymptomatic foot. Gait Posture. 2013;37(3):445–51. doi: 10.1016/j.gaitpost.2012.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Song J, et al. Foot type biomechanics: comparison of planus and rectus foot types. J Am Podiatr Med Assoc. 1996;86(1):16–23. doi: 10.7547/87507315-86-1-16. [DOI] [PubMed] [Google Scholar]
- 22.McPoil TG, et al. Variability of plantar pressure data. A comparison of the two-step and midgait methods. J Am Podiatr Med Assoc. 1999;89(10):495–501. doi: 10.7547/87507315-89-10-495. [DOI] [PubMed] [Google Scholar]
- 23.Segal NA, et al. Pregnancy leads to lasting changes in foot structure. Am J Phys Med Rehabil. 2013;92(3):232–40. doi: 10.1097/PHM.0b013e31827443a9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bolte C, et al. Pressure changes under the feet of obese adults after a weight reduction program. Archives of physiology and biochemistry. 2000;108:70. [Google Scholar]