Abstract
Background and Purpose
Studies show that women are more likely to receive do-not-resuscitate (DNR) orders after acute medical illnesses than men. However, the sex differences in the use of DNR orders after acute intracerebral hemorrhage (ICH) has not been described.
Methods
We conducted a retrospective study of consecutive patients hospitalized for acute ICH at a tertiary stroke center between 2006 and 2010. Unadjusted and multivariable logistic regression analyses were performed to test for associations between female sex and early (<24 hours of presentation) DNR orders.
Results
A total of 372 consecutive ICH patients without pre-existing DNR orders were studied. Overall, 82 (22%) patients had early DNR orders after being hospitalized with ICH. In the fully adjusted model, early DNR orders were more likely in women (odds ratio 3.18, 95% CI 1.51 to 6.70), higher age (odds ratio 1.09 per year, 95% CI 1.05 to 1.12), larger ICH volume (odds ratio 1.01 per cm3, 95% CI 1.01 to 1.02), and lower initial GCS score (odds ratio 0.76 per point, 95% CI 0.69 to 0.84). Early DNR orders were less likely when the patients were transferred from another hospital (odds ratio 0.28, 95% 0.11 to 0.76).
Conclusions
Women are more likely to receive early DNR orders after ICH than men. Further prospective studies are needed to determine factors contributing to the sex variation in the use of early DNR order after ICH.
Keywords: End-of-life care, intracerebral hemorrhage, sex differences
INTRODUCTION
The use of “early” (<24 hours from presentation) do-not-resuscitate (DNR) orders after intracerebral hemorrhage (ICH) has been regarded as a form of care limitation1-4 or a proxy for lack of overall aggressiveness of care.1, 2, 4 Prior studies assessing the use of DNR orders in the inpatient settings suggest that women are more likely to receive DNR orders than men after various medical illnesses.3, 5-7 However, the sex differences in the use of early DNR orders specific to ICH patients have not been studied.
METHODS
We conducted a retrospective study of all spontaneous ICH patients hospitalized at a tertiary stroke center in Honolulu, Oahu, between January 1, 2006, and August 31, 2010 to assess sex differences in the use of early DNR orders after ICH. The DNR orders were defined as any plan to limit cardiopulmonary resuscitation in the event of a cardiopulmonary arrest. “Pre-existing DNR” was determined if the electronic medical record prior to admission or the advance directive specified the pre-existing DNR status. “Early DNR” (within 24 hours of presentation) was based on the date/time of the DNR order entry relative to the date/time of patient arrival. The data on withdrawal of life support was also collected.
Statistical Analysis
Multivariable analyses using a logistic regression model were performed using SPSS, version 20.0 (Chicago, IL) to identify factors associated with early DNR orders. All covariates for the models were preselected based on biological plausibility, and included sex, age, initial Glasgow Coma Scale (GCS) score, ICH volume, intraventricular hemorrhage (IVH), infratentorial hemorrhage, admitting team and whether they were transferred from another hospital. The analysis of “time to DNR” decision-making over 30-day period was performed by Kaplan-Meier survival analysis.
RESULTS
A total of 396 consecutive ICH patients with validated spontaneous ICH were identified. Twenty-four patients with pre-existing DNR orders (6 of 218 men (3%) vs. 18 of 178 women (10%), p = 0.002) were excluded. A total of 372 ICH patients without pre-existing DNR orders were included for the final analysis. Demographic and baseline characteristics of those with and without early DNR orders are presented in Table. The comparison of clinical characteristics between men and women showed that women were older (66±17 years vs. 61±16 years, p=0.01) and less likely to smoke (8% vs. 22%, p<0.0001) than men. Furthermore, women were more likely to be admitted to the floor for comfort care compared to men (13% vs. 4%, p=0.003). There was a trend toward less ICU admission among women compared to men (54% vs. 63%, p=0.07).
Table.
Baseline characteristics of ICH Patients
| Early DNR | No Early DNR | P | |
|---|---|---|---|
| No. of patients | 82 | 290 | |
| Age, years | 74±15 | 60±16 | <0.0001 |
| Female | 48 (59) | 112 (39) | 0.001 |
| Race | 0.24 | ||
| White | 15 (18) | 42 (15) | |
| Asian | 55 (67) | 177 (61) | |
| NHPI | 9 (11) | 60 (21) | |
| Other | 3 (4) | 11 (4) | |
| Risk factors | |||
| Hypertension | 62 (76) | 203 (70) | 0.32 |
| Diabetes mellitus | 16 (20) | 66 (23) | 0.53 |
| Atrial fibrillation/Atrial flutter | 6 (7) | 34 (12) | 0.26 |
| Coronary artery disease or prior MI | 10 (12) | 33 (11) | 0.84 |
| Smoking | 5 (6) | 54 (19) | 0.006 |
| Methamphetamine abuse | 4 (5) | 25 (9) | 0.26 |
| Initial GCS Score | 6 [4, 11] | 14 [10, 15] | <0.0001 |
| CT characteristics | |||
| Location | 0.17 | ||
| Basal Ganglia | 38 (46) | 104 (36) | |
| Lobar | 22 (27) | 71 (24) | |
| Thalamus | 12 (15) | 53 (19) | |
| Brainstem | 2 (2) | 20 (7) | |
| Cerebellum | 7 (9) | 24 (8) | |
| Primary intraventricular hemorrhage | 1 (1) | 18 (6) | |
| Infratentorial hemorrhage | 10 (12) | 43 (15) | 0.55 |
| Intraventricular hemorrhage | 55 (67) | 120 (41) | <0.0001 |
| Hematoma Volume (cm3) | 80±72 | 25±36 | <0.0001 |
| ICH Score | 3 [2, 4] | 1 [1, 2] | <0.0001 |
| Transferred from another hospital | 12 (15) | 83 (29) | 0.01 |
| Admission under neurovascular team | 49 (60) | 136 (47) | 0.04 |
| Discharge mortality | 58 (71) | 38(13) | <0.0001 |
ICH, intracerebral hemorrhage; DNR, do-not-resuscitate; NHPI, Native Hawaiians and other Pacific Islanders; MI, myocardial infarction, GCS, Glasgow Coma Scale. Data are n (%), mean±SD, or median (interquartile range).
Unadjusted analysis of early DNR orders showed that women were more likely to receive an early DNR order compared to men (OR 2.24, 95% CI 1.36 to 3.70). Multivariable analysis showed that early DNR orders were more likely in women (OR 3.18, 95% CI 1.51 to 6.70). Higher age (OR 1.09 per year, 95% CI 1.05 to 1.12), larger ICH volume (OR 1.01 per cm3, 95% CI 1.01 to 1.02), and lower initial GCS score (OR 0.76 per point, 95% CI 0.69 to 0.84) were also independently associated with early DNR orders. Early DNR orders were less likely when the patients were transferred from another hospital (OR 0.28, 95% 0.11 to 0.76). Kaplan-Meier curves showed a significant difference in the “time to DNR” between the two sexes (Figure 1).
Figure 1.
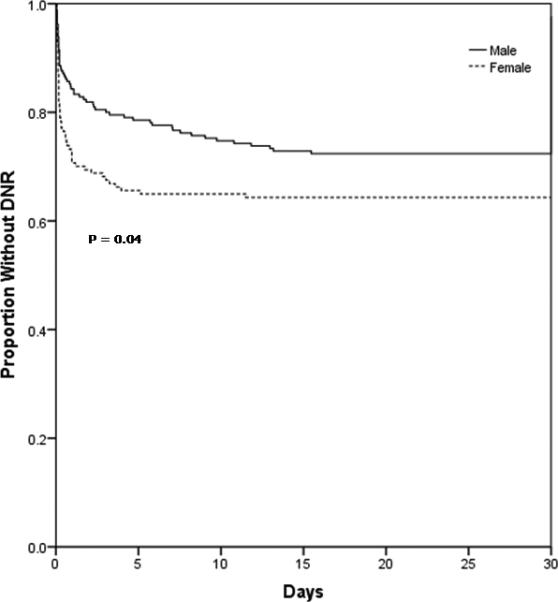
Analysis of “time to DNR” after ICH.
The proportion of ICH patients with early DNR orders, based on the ICH Score, is shown in Figure 2. Even among the patients with less severe ICH Score of 0 to 3 (n = 326), women had higher prevalence of early DNR orders than men (21% vs. 12%, p=0.03). Despite these differences in the prevalence of the early DNR orders, the discharge mortality (26% vs. 26%, p=0.87) and the withdrawal of life support rate (23% vs. 18%, p=0.23) were not different between women and men.
Figure 2.
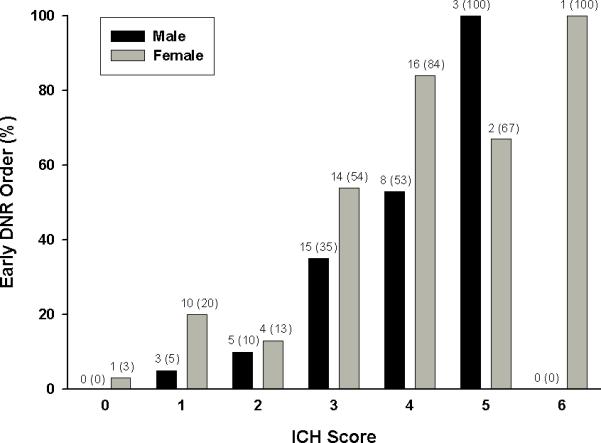
Comparison of early DNR orders between male and female ICH patients based on the ICH Score. Data are n (%).
DISCUSSION
Our study showed that women with ICH are more likely to receive early DNR orders, independent of age and clinical severity, compared to men with ICH. Our results are similar to the prior studies that showed sex differences in the use of DNR orders among patients with other acute medical illnesses5-7 and support the idea that women seek less heroic resuscitative measures upon cardiopulmonary arrest, compared to men.
Since many ICH patients are unable to make important end-of-life decisions due to their neurological impairment, the decision to initiate a DNR order within 24 hours of admission for those without pre-existing DNR orders, in most part, reflects the dialogue of aggressiveness of care between the families and the clinicians. It may be that women, compared to men, are more likely to have already expressed their wishes to the families/surrogate decision-maker and more explicitly advised them how to handle this type of situation, making it easier for the families to decide on the DNR status (no heroic resuscitative measures) early in the hospital course. These explanations are supported by the higher prevalence of pre-existing DNR orders, higher rate of comfort care on admission, and a trend toward less ICU admission among women compared to men.
CONCLUSIONS
Female sex is independently associated with the use of early DNR orders after ICH. Further prospective studies are needed to determine factors contributing to the sex variation in the use of early DNR orders and end-of-life discussion after ICH.
ACKNOWLEDGMENTS
None
SOURCES OF FUNDING
Dr. Nakagawa was supported in part by the American Heart Association (11CRP7160019) and the National Institute on Minority Health and Health Disparities (P20MD000173). Dr. Seto was supported in part by the National Institute on Minority Health and Health Disparities (U54MD007584). Dr. Hemphill was supported in part by the National Institute of Neurological Disorders and Stroke (U10NS058931).
Footnotes
DISCLOSURE
None
REFERENCES
- 1.Hemphill JC, 3rd, Newman J, Zhao S, Johnston SC. Hospital usage of early do-not-resuscitate orders and outcome after intracerebral hemorrhage. Stroke. 2004;35:1130–1134. doi: 10.1161/01.STR.0000125858.71051.ca. [DOI] [PubMed] [Google Scholar]
- 2.Zahuranec DB, Brown DL, Lisabeth LD, Gonzales NR, Longwell PJ, Smith MA, et al. Early care limitations independently predict mortality after intracerebral hemorrhage. Neurology. 2007;68:1651–1657. doi: 10.1212/01.wnl.0000261906.93238.72. [DOI] [PubMed] [Google Scholar]
- 3.Shepardson LB, Youngner SJ, Speroff T, O'Brien RG, Smyth KA, Rosenthal GE. Variation in the use of do-not-resuscitate orders in patients with stroke. Arch Intern Med. 1997;157:1841–1847. [PubMed] [Google Scholar]
- 4.Zahuranec DB, Morgenstern LB, Sanchez BN, Resnicow K, White DB, Hemphill JC., 3rd Do-not-resuscitate orders and predictive models after intracerebral hemorrhage. Neurology. 2010;75:626–633. doi: 10.1212/WNL.0b013e3181ed9cc9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wenger NS, Pearson ML, Desmond KA, Harrison ER, Rubenstein LV, Rogers WH, et al. Epidemiology of do-not-resuscitate orders. Disparity by age, diagnosis, gender, race, and functional impairment. Arch Intern Med. 1995;155:2056–2062. [PubMed] [Google Scholar]
- 6.Eachempati SR, Hydo L, Shou J, Barie PS. Sex differences in creation of do-not-resuscitate orders for critically ill elderly patients following emergency surgery. J Trauma. 2006;60:193–197. doi: 10.1097/01.ta.0000197683.89002.62. discussion 197-198. [DOI] [PubMed] [Google Scholar]
- 7.Jackson EA, Yarzebski JL, Goldberg RJ, Wheeler B, Gurwitz JH, Lessard DM, et al. Donot-resuscitate orders in patients hospitalized with acute myocardial infarction: the Worcester Heart Attack Study. Arch Intern Med. 2004;164:776–783. doi: 10.1001/archinte.164.7.776. [DOI] [PubMed] [Google Scholar]


