Summary
We undertook a comprehensive clinical and biological investigation of serial medulloblastoma biopsies obtained at diagnosis and relapse. Combined MYC family amplifications and P53 pathway defects commonly emerged at relapse, and all patients in this group died of rapidly progressive disease postrelapse. To study this interaction, we investigated a transgenic model of MYCN-driven medulloblastoma and found spontaneous development of Trp53 inactivating mutations. Abrogation of p53 function in this model produced aggressive tumors that mimicked characteristics of relapsed human tumors with combined P53-MYC dysfunction. Restoration of p53 activity and genetic and therapeutic suppression of MYCN all reduced tumor growth and prolonged survival. Our findings identify P53-MYC interactions at medulloblastoma relapse as biomarkers of clinically aggressive disease that may be targeted therapeutically.
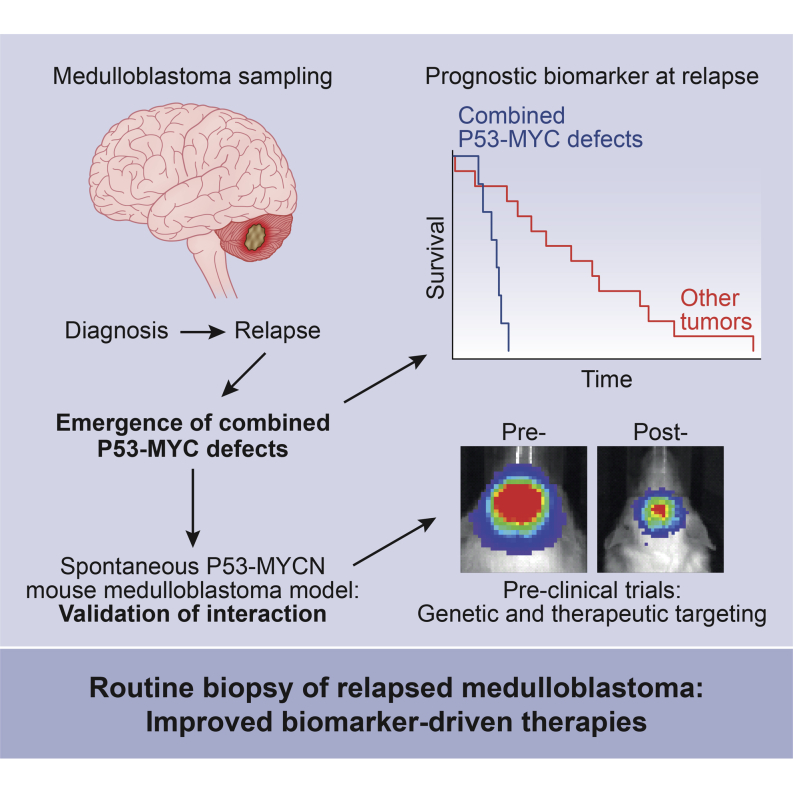
Graphical Abstract
Highlights
-
•
Combined P53 and MYC family defects emerge at medulloblastoma relapse
-
•
P53-MYC defects are a biomarker for rapidly progressive relapsed disease
-
•
Trp53 and MYCN interact to drive aggressive medulloblastoma development in mice
-
•
Targeting MYCN or P53 pathway reactivation reduces tumor growth and prolongs survival
Hill et al. find that coincident MYC amplifications and p53 pathway defects are common in relapsed medulloblastoma (MB) and correlate with poor postrelapse prognosis. The authors go on to explore this MYC-p53 interaction in a mouse MB model and show that these tumors are dependent on both aberrations.
Significance
There are currently no effective therapies for children with relapsed medulloblastoma. Although clinical and biological features of the disease at diagnosis are increasingly well understood, biopsy is rarely performed at relapse, and few biological data are available to guide more effective treatments. Here, we show that medulloblastomas develop altered biology at relapse, which is predictive of disease course and cannot be detected at diagnosis. We have discovered the emergence of P53-MYC interactions at relapse, as biomarkers of clinically aggressive relapsed disease, which can be modeled and targeted therapeutically in genetically engineered mice. These data support the incorporation of biopsy at relapse into routine clinical practice, to direct palliative care and the development of improved treatment strategies.
Introduction
Relapse following conventional treatment is the single most adverse event in medulloblastoma; over 95% of relapsing patients die, accounting for ∼10% of childhood cancer deaths (Pizer and Clifford, 2009). Biological investigations have to date focused on the disease at diagnosis, where disease-wide 5 year survival rates currently stand at 60%–70% (Pizer and Clifford, 2009). These studies have shown medulloblastoma is biologically heterogeneous, comprising four molecular subgroups (WNT [MBWNT], SHH [MBSHH], group 3 [MBGroup3], and group 4 [MBGroup4]) with distinct clinical, pathological, and molecular features (Kool et al., 2012; Taylor et al., 2012). Moreover, disease features have been identified at diagnosis that are consistently associated with clinical outcomes. For high-risk disease, these are MYC gene family (MYC, MYCN) amplification, TP53 mutation, chromosome 17 defects, large-cell anaplastic pathology, metastatic disease, and subtotal surgical resection, whereas favorable-risk disease is defined by the MBWNT subgroup and desmoplastic/nodular pathology in infants (Ellison et al., 2005, 2011; McManamy et al., 2007; Northcott et al., 2012a; Pfister et al., 2009; Pizer and Clifford, 2009; Rutkowski et al., 2009; Ryan et al., 2012; Taylor et al., 2012; Zhukova et al., 2013). Together, these recent advances in understanding of the disease at diagnosis are rapidly informing the design of biologically driven phase III clinical trials aimed at improved outcomes through enhanced disease-risk stratification (Pizer and Clifford, 2009).
Patient management at relapse, however, typically focuses on quality of remaining life rather than curative strategies. This absence of suitable treatment alternatives has stemmed primarily from a lack of clinical and biological data, because biopsy is rarely performed at this stage. Consequently, this has impeded the characterization of mechanisms that drive medulloblastoma relapse, and the relevance of all the established medulloblastoma disease features in the relapsed setting, has not been investigated. Moreover, this has prevented functional validation of molecular targets using animal disease models, and their assessment as biomarkers of disease course, to support the development of more effective treatments.
We therefore assembled a clinical-trials-based cohort of patient-derived medulloblastoma biopsies sampled at relapse and aimed to undertake a comprehensive analysis of their clinical and biological characteristics, in contrast with their diagnostic counterparts. Coupled with the subsequent functional validation of specific biological features which commonly emerge at relapse (combined P53-MYC defects), using genetically engineered mouse models, we further aimed to assess their potential as biomarkers of clinically aggressive relapsed disease, and as therapeutic targets, for the improved management of patients with relapsed medulloblastoma.
Results
Disease Characteristics of Relapsed Medulloblastoma
We undertook a detailed assessment of the clinical, pathological, and molecular characteristics of relapsed medulloblastoma, in a cohort of 29 recurrent tumors and their paired diagnostic samples, recruited from the recent UK Children’s Cancer and Leukemia Group (CCLG) Recurrent PNET (CNS 2000 01) trial (Pizer et al., 2011) and UK CCLG treatment centers. We first assessed all molecular disease features with established significance at diagnosis including chromosome 17 and P53 pathway status (TP53 mutation and p53 nuclear accumulation, CDKN2A [p14ARF] and MDM2 status), MYC gene family (MYC, MYCN) amplification, polyploidy, CTNNB1 mutation, and molecular subgroup status (Table 1; Table S1 available online) (Ellison et al., 2011, 2005; Frank et al., 2004; Jones et al., 2012; Northcott et al., 2012a, 2012b; Pfister et al., 2009; Robinson et al., 2012; Ryan et al., 2012; Taylor et al., 2012; Zhukova et al., 2013). Only the tumor molecular subgroup was unchanged at diagnosis and relapse in all cases (Figure 1A), in agreement with the only other published cohort of medulloblastomas sampled and subgrouped at relapse (Ramaswamy et al., 2013). Subgroup distribution in the cohort of relapsed tumors sampled in our study was also consistent with Ramaswamy et al., as well as an unbiased cohort of relapsing tumors from a trial-based medulloblastoma study that were sampled at diagnosis (Schwalbe et al., 2013) (Table S2).
Table 1.
Detailed Clinical, Pathological, and Molecular Characteristics of 29 Paired Medulloblastomas Sampled at Diagnosis and Relapse Showing Altered and Acquired Features at Relapse
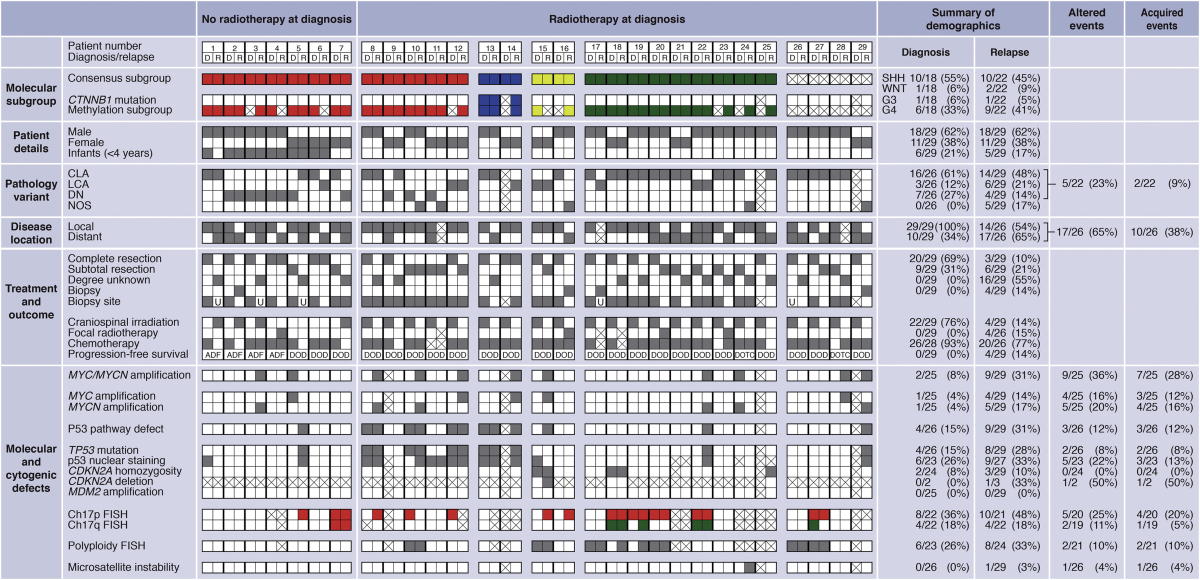
Demographic frequencies and altered and acquired events are shown as a proportion and percentage of the data available for each variable. D, diagnosis; R, relapse. Consensus molecular subgroup: red, SHH/MBSHH; blue, WNT/MBWNT; yellow, G3/MBGroup3; green, G4/MBGroup4. Pathology variant: CLA, classic; LCA, large-cell/anaplastic; DN, desmoplastic/nodular; NOS, medulloblastoma not otherwise specified. Disease location: local, M0/M1; distant, M2+. Biopsy site: gray square, primary tumor biopsied; white square, metastatic site biopsied; U, biopsy site unknown; crossed square, biopsy sample not available. Current status: ADF, alive disease-free; DOD, died of disease; DOTC, died of treatment complications. Chromosome 17 status: red, loss; green, gain. Other categories: gray square, feature present; white square, feature absent; crossed square, data not available. See also Table S1 and S2.
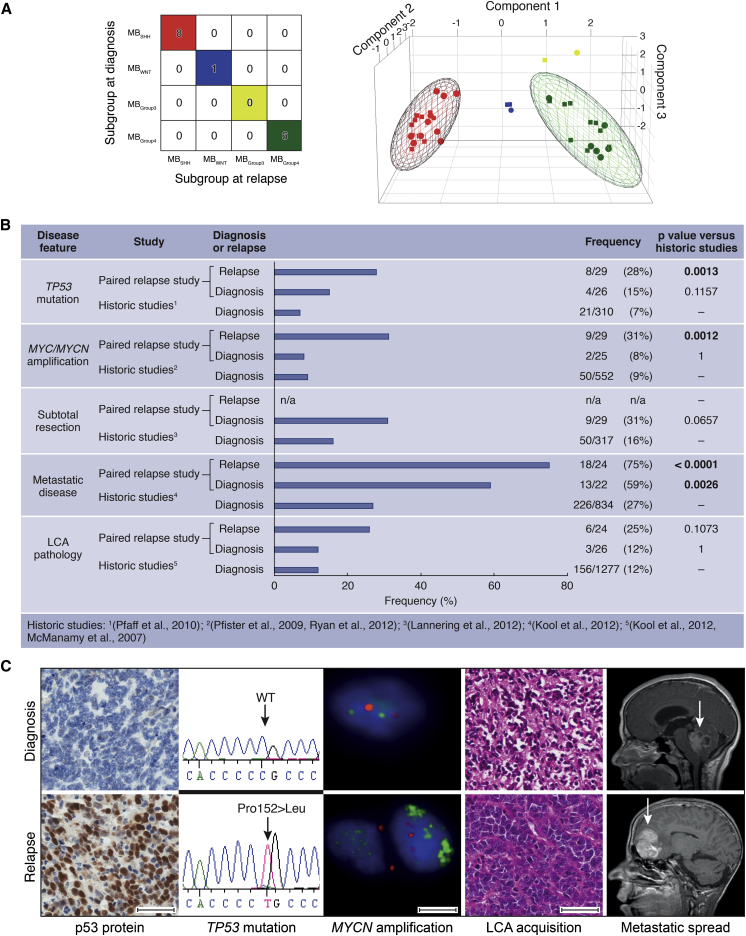
Figure 1.
Relapsed Medulloblastomas Maintain the Molecular Subgroup but Are Enriched for Multiple High-Risk Clinical and Molecular Features
(A) Consensus clustering (left) and principal component analysis (PCA) (right) of medulloblastoma subgroups at diagnosis and relapse. Consensus molecular subgroups: red, MBSHH; blue, MBWNT; yellow, MBGroup3; green, MBGroup4. In the PCA plot, subgroups assigned at diagnosis are represented by circles, and those assigned at relapse are represented by squares.
(B) Frequency of high-risk disease features within the present paired relapse study cohort sampled at diagnosis and relapse, compared to large historic cohorts sampled at disease diagnosis. p, Fisher’s exact test.
(C) Acquisition of molecular and clinical disease features between diagnosis (top) and relapse (bottom). Left to right: immunohistochemical analysis of p53 protein accumulation; TP53 homozygous missense mutation (Pro152Leu); interphase fluorescence in situ hybridization (iFISH) showing MYCN amplification (green versus centromeric control (red); H&E showing LCA acquisition and magnetic resonance imaging (MRI) showing metastatic spread (arrows indicate tumor site). Scale bars, 50 μM (immunohistochemistry, H&E) or 5 μM (iFISH).
All other features examined showed evidence of alteration at relapse, with the majority (30/44, 68%) representing acquired high-risk disease features (Figures 1B and 1C; Table 1; Table S3) (Lannering et al., 2012; McManamy et al., 2007). Distant metastases were significantly enriched at both diagnosis and recurrence in our relapsed study cohort compared to large historic cohorts of tumors taken at diagnosis (p < 0.003), whereas high-risk molecular features (MYC and MYCN gene amplification, TP53 mutation) occurred at significantly greater frequencies at relapse than at diagnosis (Figures 1B and 1C; Figures S1A–S1E; Table S3) (Pfaff et al., 2010; Pfister et al., 2009; Ryan et al., 2012). Aggressive pathology (large-cell anaplastic [LCA] variant) and TP53 mutation were always either maintained from diagnosis to relapse or acquired at relapse. Two of two assessable TP53 mutations tumors were somatic in origin. TP53 mutation was identified in three of six p53-immunopositive tumors sampled at diagnosis (versus 0/17 immunonegative; p = 0.04, Fisher’s exact test) and eight of nine immunopositive tumors sampled at relapse (versus 0/18 immunonegative; p = 4 × 10−6, Fisher’s exact test, Table 1). Relapse following upfront radiotherapy (RT) was fatal in all cases (22/22). The only long-term survivors were infants receiving RT at recurrence (four of four, median overall survival 17 years (range 8.9–19.2 years); Figures S1F–S1H; Table 1).
Combined MYC and P53 Defects Commonly Emerge at Medulloblastoma Relapse
P53 pathway defects (TP53 mutation, CDKN2A deletion) and MYC gene family amplification were the only disease features, which were significantly associated at relapse (Figure S2A). In patients receiving standard upfront radiotherapy and chemotherapy, these defects emerged in combination and were significantly more frequent at relapse (32% [seven of 22]) compared to diagnosis (0/19; p = 0.01, Fisher’s exact test, Figures 2A and 2B). Single MYC gene family (n = 1) or P53 pathway aberrations (n = 1) were rarely observed in isolation at relapse in this treatment group (Figure 2A).
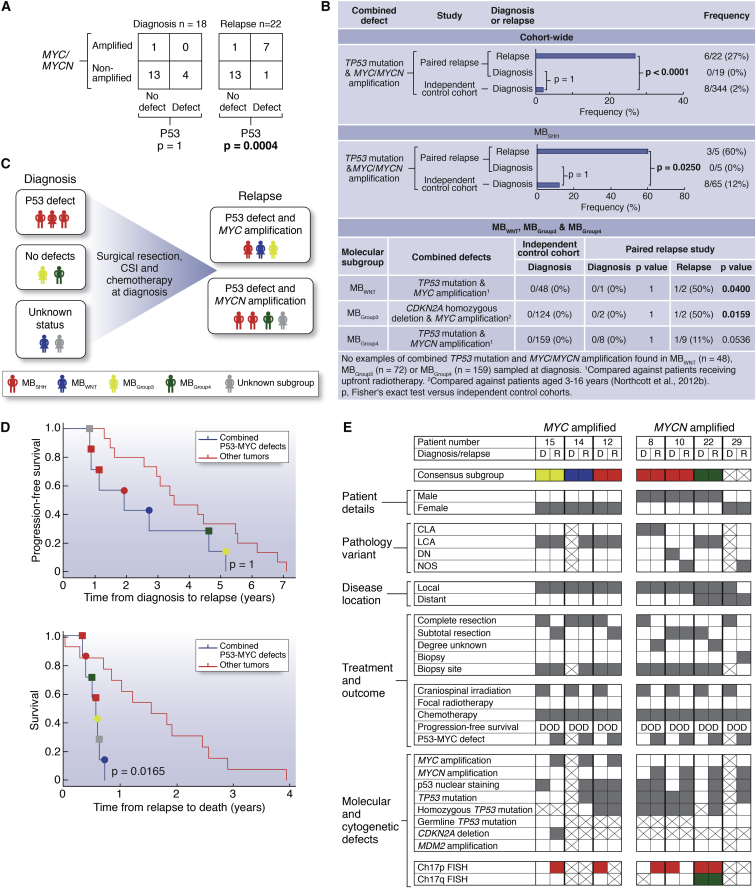
Figure 2.
Combined P53 Pathway Defects and MYC/MYCN Amplification Commonly Emerge following Standard Upfront Radiotherapy and Chemotherapy and Correlate with Rapid Disease Progression after Relapse
(A–C) Association (A), frequency of occurrence and distribution within molecular subgroups (B), and patterns of emergence (C), of combined P53 pathway defects and MYC/MYCN amplification at diagnosis and relapse.
(D) Survival of patients with tumors harboring combined P53-MYC gene family defects versus other tumors, showing time from diagnosis to relapse (top) and relapse to death (bottom). Circle, P53-MYC; square, P53-MYCN. p, log rank test, Bonferroni corrected.
(E) Detailed clinical, pathological, and molecular demographics of patients with combined P53-MYC gene family defects at relapse. D, diagnosis; R, relapse. Consensus molecular subgroup (red, MBSHH; blue, MBWNT; yellow, MBGroup3; green, MBGroup4). Pathology variant: CLA, classic; LCA, large-cell/anaplastic; DN, nodular/desmoplastic; NOS, medulloblastoma not otherwise specified. Disease location: local, M0/M1; distant, M2+. Biopsy site: gray square, primary tumor biopsied; white square, metastatic site biopsied; crossed square, biopsy sample not available. Current status: DOD, died of disease. Chromosome 17 status: red, loss; green, gain. Other categories: gray square, feature present; white square, feature absent; crossed square, data not available.
Combined P53-MYC defects characterized relapsed tumors of all molecular subgroups and occurred in combinations of specific defects that are not observed at diagnosis. Only combined TP53 mutation/MYCN amplification in MBSHH have previously been observed at diagnosis (∼6% of MBSHH) (Zhukova et al., 2013). Direct comparison with the incidence of P53-MYC defects in our own large cohort (n = 344) of uniformly characterized primary medulloblastomas, sampled and subgrouped at diagnosis, showed significant enrichment of these combined defects in relapsed MBSHH subgroup tumors following treatment with standard chemotherapy and radiotherapy (60% [three of five] versus 12% [eight of 65] at diagnosis [p = 0.0250, Figure 2B]). Equivalent trends were observed for the instances of combined P53-MYC alterations detected in relapsed MBWNT and MBGroup3 tumors (one of two tumors in both groups); these defects were not observed in any tumor sampled at diagnosis (0/48 [p = 0.0400] and 0/124 [p = 0.0159], respectively, Figure 2B). Combined defects observed at relapse in MBGroup4 following conventional therapy were apparently less frequent than in MBSHH (one of nine versus three of five; p = 0.095, Fisher’s exact test). Moreover, combinations of specific P53-MYC defects were uniquely observed at relapse and were not observed at diagnosis in our large control cohorts, or in previously reported studies (Pfaff et al., 2010) (e.g., CDKN2A deletion and MYC amplification in a relapsed MBGroup3 tumor; TP53 mutation and MYC amplification in a relapsed MBSHH tumor; TP53 mutation and MYCN amplification in a relapsed MBGroup4 tumor; TP53 mutation and MYC amplification in a relapsed MBWNT tumor).
P53 pathway and MYC gene family defects combined at relapse, both through maintenance of defects from diagnosis (P53 pathway) and/or the emergence at relapse (P53 pathway, MYC gene family) of one or both events (Figure 2C). Assessments of intratumoral molecular heterogeneity by single-cell iFISH and deep sequencing supported both de novo acquisition and clonal enrichment as mechanisms of defect emergence at relapse and demonstrated the occurrence of both defects in the same cell (Figure S2B).
P53-MYC Interactions Characterize Locally Aggressive Relapsed Disease
Importantly, the co-occurrence of P53 pathway and MYC gene family defects at relapse defined a population of patients with clinically aggressive tumors in which time to relapse was equivalent to that of other patients, but time to death (TTD) was significantly more rapid postrecurrence (Figure 2D; Table S4). These combined P53-MYC defects were the most significant independent predictor of TTD in multivariate survival analysis, which included tumor molecular subgroup. This group of patients all died quickly within 9 months following relapse (0.57 years [0.33–0.72 years range] median time to death post-relapse, versus 1.22 years for other tumors [0.02–2.9 years]; p = 0.0165). Moreover, MYC-P53 and MYCN-P53 defects remained significantly associated with TTD when considered in isolation against patients without combined defects (p = 0.0183 and 0.0039, respectively, log rank test).
Relapsed tumors with P53-MYC defects were significantly associated with adverse LCA pathology (Ellison et al., 2011; McManamy et al., 2007) (four of five assessable tumors, 80%, p = 0.0099, Fisher’s exact test), but most did not have distant metastases (five of seven, 71%), suggesting locally aggressive disease (Figure 2E). Moreover, these tumors could not be distinguished by their clinical and pathological features and require biopsy and staging at the molecular level. In summary, our findings demonstrate that the emergence of combined MYC gene family amplification and P53 pathway defects is a common event at relapse following standard upfront therapy, associated with an aggressive clinical course, and can occur in tumors from all molecular disease subgroups and in specific combinations of genetic events that are not observed at diagnosis. Such patients could potentially be targeted using biomarker-driven, individualized therapeutic approaches.
Trp53 and MYCN Interact Directly in Medulloblastoma Development
These clinical observations and previous modeling of medulloblastoma in mice suggested that aberrant activation of the MYC gene family synergizes with inactivation of p53 or Rb in the genesis of biologically aggressive medulloblastoma (Kawauchi et al., 2012; Pei et al., 2012; Shakhova et al., 2006). The hypothesis that MYC or MYCN specifically interacts with p53 loss of function was established in recent studies in which Trp53-inactivated murine cerebellar stem or progenitor cells were transformed by forced overexpression of exogenous Myc or Mycn, driving formation of aggressive tumors resembling human medulloblastoma following transplantation into the cerebellum (Kawauchi et al., 2012; Pei et al., 2012). To investigate whether the P53-MYC interaction could be directly responsible for the genesis of spontaneous tumors within a native anatomic and developmental context, we examined Trp53 status using a transgenic MYCN-driven mouse model (GTML; Glt1-tTA/TRE-MYCN-Luc) (Swartling et al., 2010). Selection of this experimental system was of particular interest given that GTML is a native transgenic model of medulloblastoma driven by fully reversible expression of MYCN, allowing direct assessment of its role in spontaneous tumor development. Somatic Trp53 DNA-binding domain mutations were found in 83% of tumors examined (ten of 12) (Figure S3A; Table S5). We next tested directly whether tumor growth was dependent on both p53 and MYCN by generating GTML mice deficient in functional p53, using a mouse model in which the endogenous Trp53 gene is replaced with a knockin allele (Trp53KI) encoding a 4-hydroxytamoxifen (4-OHT)-regulatable p53ERTAM fusion protein (Christophorou et al., 2005). Mice completely deficient for p53 (GTML/Trp53KI/KI) developed tumors with dramatically increased penetrance and significantly decreased overall survival (100%, 43/43 versus 6%, three of 50 in GTML, p < 0.0001, Figure 3A). Medulloblastomas from GTML/Trp53KI/WT and GTML/Trp53KI/KI mice uniformly displayed aggressive clinical and pathological features (high mitotic index, LCA pathology) equivalent to that of tumors in GTML mice with spontaneous Trp53 mutations (Figure 3B). Moreover, tumors of all three genotypes were representative of the locally aggressive disease features (i.e., nonmetastatic, LCA) of the majority of P53-MYC-associated relapsed human tumors (Figures 2E, 3B, and S3B) and displayed gene expression profiles characteristic of human MBGroup3 (Figures 3C and S3C).
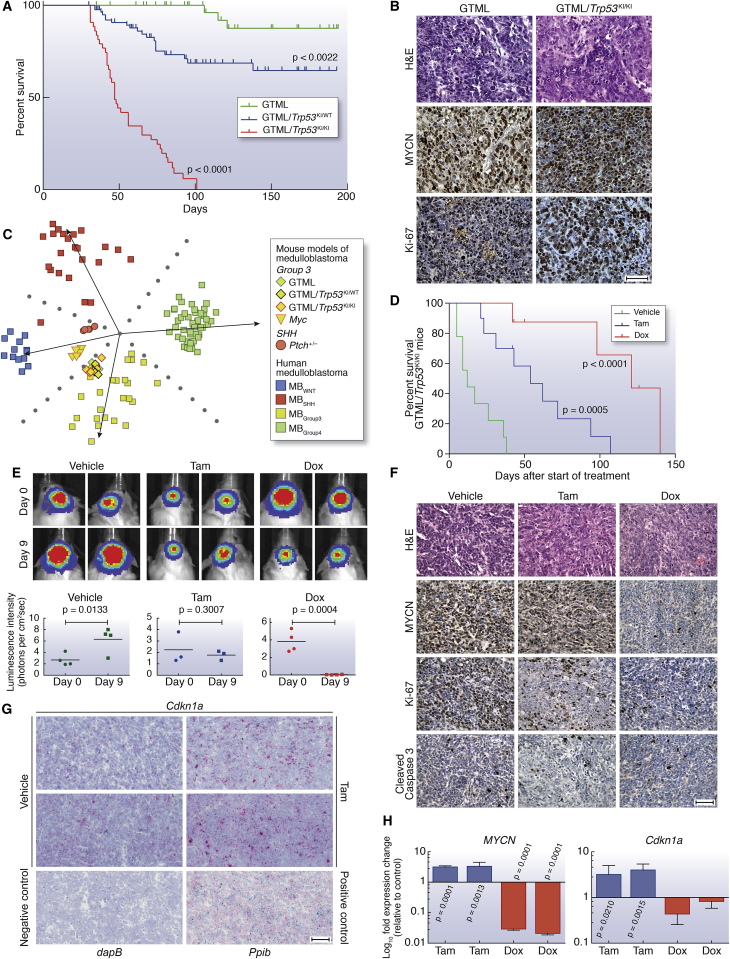
Figure 3.
Aberrant Expression of MYCN in Combination with p53 Loss of Function Drives Highly Penetrant and Aggressive Medulloblastoma
(A) Kaplan-Meier survival curves for GTML/Trp53KI/KI (n = 43), GTML/Trp53KI/WT (n = 83), or GTML transgenic mice (n = 50) mice as indicated. p, log rank test.
(B) H&E and immunohistochemical staining indicating levels of MYCN protein and cell proliferation (Ki-67) in GTML/Trp53KI/KI and GTML transgenic mice.
(C) Subgroup classification of mouse expression profiles using a support vector machine trained on human medulloblastoma expression profiles and nonnegative matrix factorization for cross-species projection.
(D) Kaplan-Meier survival for GTML/Trp53KI/KI mice treated with doxycycline (Dox, n = 8) or tamoxifen (Tam, n = 10) compared to vehicle (n = 9) as indicated. p, log rank test.
(E) GTML/Trp53KI/KI mice coexpressing firefly luciferase (FLuc) were treated with Tam, Dox, or vehicle for 9 days. Bioluminescent imaging of GTML/Trp53KI/KI mice after 9 days treatment with Dox or Tam as indicated (top). Luminescence intensity at days 0 and 9 are shown (bottom). Data points represent individual mice. p, unpaired t test.
(F) H&E and immunohistochemical staining indicating levels of MYCN, Ki-67, or apoptosis (cleaved caspase 3) in GTML/Trp53KI/KI mice after treatment with Dox or Tam.
(G) RNAscope 2-plex chromogenic assay. Cdkn1a expression (red) was analyzed on brain sections from GTML/Trp53KI/KI mice treated with either Tam or vehicle control as indicated. Samples were costained for expression of the Ubc (ubiquitin C) housekeeping gene (green). Expression of Ppib (Peptidylprolyl Isomerase B, Cyclophilin B) (red) and Polr2a (DNA-directed RNA polymerase II subunit RPB1) (green) were used as positive controls. Expression of dapB (dihydrodipicolinate) reductase gene from B. subtilis was used as a negative control. Sections were counterstained with Gill’s hematoxylin.
(H) Fold difference of human MYCN or mouse Cdkn1a mRNA levels in tumor tissues treated with either Dox or Tam. (p, unpaired t test.)
Scale bars, 50 μm. Error bars represent mean ± SD. See also Figure S3 and Table S5.
MYCN-Driven Murine Tumor Maintenance Is Dependent on p53 and MYCN Status
Both p53 loss of function and expression of MYCN were required for maintenance of GTML/Trp53KI/KI tumors. Addition of either tamoxifen (Tam), which is metabolized to 4-OHT in the liver leading to reactivation of p53, or Dox (suppression of MYCN expression) resulted in loss of clonogenic capacity and reduced growth in GTML/Trp53KI/KI medulloblastoma-derived neurospheres, associated with loss of MYCN expression and induction of p53 target genes, respectively (Figures S3D–S3F). In vivo, administration of either drug led to increased survival in GTML/Trp53KI/KI mice, relating to inhibition of tumor growth (Tam) or induction of tumor regression (Dox) (Figures 3D and 3E). Treatment with either Dox or Tam led to dramatic tumor-specific reductions in the Ki-67 cellular proliferation marker, Dox-specific loss of MYCN expression, or Tam-specific induction of the p53 target Cdkn1a (Figures 3F–3H; Figure S3G). Together, these findings validate the critical dependency of MYCN-driven murine tumor growth on TP53 defects. The continued dependency on this interaction for tumor maintenance offers the potential for therapeutic intervention in relapsed human medulloblastomas.
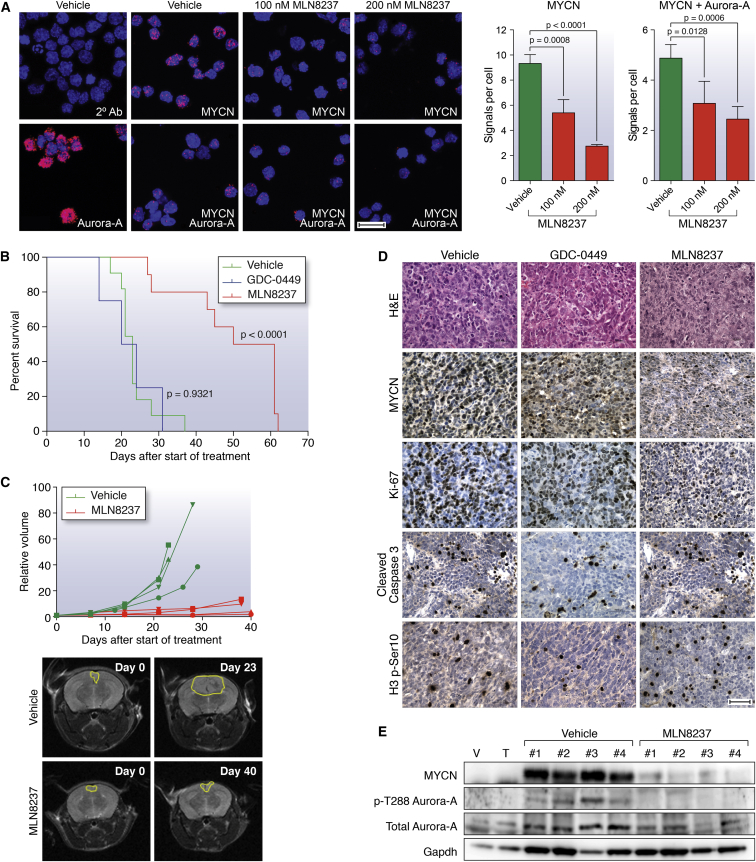
Therapeutic Targeting with Aurora-A Kinase Inhibitors
We recently showed that small molecules that target the kinase domain of Aurora-A, a MYCN-binding protein and gatekeeper of MYCN oncoprotein stability, can induce regression and differentiation of MYCN-driven neuroblastoma (Brockmann et al., 2013), highlighting the clinical feasibility of targeting MYCN using this class of inhibitor. In vitro treatment of GTML/Trp53KI/KI medulloblastoma-derived neurospheres with the Aurora-A kinase inhibitor MLN8237 (Alisertib) destabilized MYCN via disruption of the Aurora-A/MYCN complex and caused growth inhibition comparable to doxycycline-mediated genetic suppression of MYCN expression (Figure 4A; Figures S4A–S4C). Consistent with their relationship to human MBGroup3, GTML/Trp53KI/KI tumors lack sonic hedgehog (SHH) signaling as evidenced by absence of Gli1 expression (Figure S4D). Thus, treatment with the SHH antagonist GDC-0449 (Vismodegib), which specifically targets medulloblastoma of granule cell origin driven by SHH expression, had no effect on MYCN and failed to reduce clonogenic capacity or growth of GTML/Trp53KI/KI-derived medulloblastoma neurospheres (Figures S4A, S4B, and S4E). Moreover, MLN8237 but not GDC-0449 significantly prolonged survival in medulloblastoma-bearing GTML/Trp53KI/KI mice (Figure 4B). Treatment with MLN8237 completely inhibited tumor growth as measured by MRI (Figure 4C). In vivo compound measurement revealed both MLN8237 and GDC-0449 achieved blood-brain barrier penetration (Figure S4F). MLN8237 treatment led to an increase in phosphorylated histone H3 (indicative of an accumulation in G2 and mitosis due to Aurora-A inhibition) as well as specific reductions in both MYCN and Ki-67, but not an increase in cleaved caspase-3 (Figures 4D and 4E). Together, these results demonstrate the target-dependent activity of MLN8237 against GTML/Trp53KI/KI medulloblastomas and suggest clinical benefit in treating relapsed P53-MYC medulloblastoma with agents that target aberrant expression of MYCN.
Figure 4.
Therapeutic Targeting of the MYCN/Aurora-A Interaction Inhibits Tumor Growth and Prolongs Survival in GTML/Trp53KI/KI Mice
(A) Proximity ligation assay (PLA) analyzing MYCN/Aurora-A complexes in GTML/Trp53KI/KI neurospheres following MLN8237 treatment (48 hr). Left panel shows close proximity (<40 nm) of antibody conjugated PLA probes that have been ligated, amplified, and detected with complementary fluorescent probes. Red dots represent the presence of MYCN or Aurora-A protein, or MYCN/Aurora-A interactions as indicated. Antibodies used are indicated by white text (2° Ab, secondary antibody control). Scale bar, 20 μm. Right panel shows mean values of signals (red dots) per cell representing MYCN expression or MYCN/Aurora-A interactions. Values are derived from triplicate biological replicates, and error bars represent SDs. p, unpaired t test.
(B) Kaplan-Meier survival for GTML/Trp53KI/KI mice treated with MLN8237 (n = 10), GDC-0449 SHH antagonist (n = 4), or vehicle (n = 11) as indicated. (p, log rank test.)
(C) Longitudinal MRI analysis of tumor volume (n = 4) on the axial plane (top). Representative MRIs of the axial plane of MLN8237-treated animals compared to vehicle as indicated at day 0 and last day of treatment (bottom).
(D) H&E and immunohistochemical staining indicating levels of MYCN protein, cell proliferation (Ki-67), apoptosis (cleaved caspase 3), or mitotic activity as measured by phosphorylated Ser10 on histone H3 (H3 p-S10) after treatment with GDC-0449 or MLN8237. Scale bar, 50 μm.
(E) Immunoblotting of MYCN protein levels, and total and phosphorylated Thr288 on Aurora-A (p-T288 Aurora-A) in MLN8237-treated tumor tissues. For (D) and (E), animals were treated with vehicle, GDC-0449, or MLN8237 for 48 hr, and samples were taken 2 hr after final administration of agent.
Error bars represent mean ± SD. See also Figure S4.
Discussion
Patients with medulloblastoma who relapse following upfront radiotherapy rarely survive, irrespective of therapy received postrecurrence (Pizer et al., 2011). Importantly, here we show that, whereas tumor subgroup did not change, clinical, pathological, and other molecular disease features were commonly altered at relapse. The emergence of combined P53-MYC gene family defects at relapse following standard upfront therapy is a common feature that occurs across disease subgroups, involves specific combinations of events not observed at diagnosis, and is associated with rapid progression to death. The validation of these combined mutations as therapeutically targetable molecular drivers of tumorigenesis in genetically engineered mice demonstrates the development of effective therapies for relapsed medulloblastoma will require strategies tailored to the unique molecular features of these tumors.
This study shows GTML/Trp53KI/KI mice to be an important model for understanding and targeting P53-MYC family interactions in medulloblastoma. Our preclinical investigations targeting Aurora-A kinase inhibition with MLN8237 in GTML/Trp53KI/KI mice, together with recent research describing CD532 (an Aurora-A inhibitor structurally distinct from MLN8237) (Gustafson et al., 2014), demonstrate proof-of-principle for indirect therapeutic targeting of MYCN in medulloblastoma and its advancement to the clinic. Establishment of their wider relevance to medulloblastoma at diagnosis, alongside other MYC/MYCN amplified and overexpressing malignancies, is paramount. Furthermore, the essential role of loss of functional p53 in GTML/Trp53KI/KI tumor growth suggests additional opportunities for intervention with emerging therapeutics that reactivate wild-type P53 by inhibiting the P53-MDM2 interaction (Carol et al., 2013; Chène, 2003; Van Maerken et al., 2014).
Our continuously collected and centrally reviewed trials-based cohort of 29 relapsed medulloblastomas is both representative of other reported relapse cohorts and reflective of the expected subgroup distribution of tumors at relapse (Table S2). Its investigation has enabled a comprehensive characterization of the clinical, pathological, and biological features of relapsed medulloblastoma and important discoveries with immediate implications for future clinical and research strategies. Although subgroup stability at relapse supports the use of diagnostic biopsy to define subgroup-directed therapies at relapse (e.g., SHH pathway inhibitors) (Rudin et al., 2009), we now understand that medulloblastomas display unique and emergent biology at relapse, which cannot be predicted at diagnosis. The identification of critical biomarkers such as P53-MYC defects in relapsed tumors will allow us, in the short term, to adapt palliative strategies tailoring therapy to predicted disease course and quality of remaining life. Looking to the future, the discovery of additional clinically relevant biomarkers will inform the further development and stratified use of targeted therapies. We particularly note MBGroup3 tumors are less commonly sampled at medulloblastoma relapse (this study; Ramaswamy et al., 2013), likely reflecting their associated early, disseminated pattern of relapse (Ramaswamy et al., 2013) and a clinical decision not to biopsy. The routine sampling of relapsed medulloblastoma is therefore now essential to expand our findings, inform comprehensive biological investigations across all clinical and molecular disease demographics, and direct clinical management and future therapeutic advances aimed at improved outcomes for children with relapsed medulloblastoma.
Experimental Procedures
Tumor Material and Clinical Data
Clinical data and tumor tissue were obtained for 29 patients from UK CCLG institutions and collaborating centers (Table 1), encompassing patients enrolled on the Recurrent PNET (CNS 2000 01) trial (Pizer et al., 2011). The median age at diagnosis was 8.6 years (range 0.1–33.7 years), and median age of recurrence was 10.7 years (range 2.4–36.3 years) with a median time to relapse of 2.6 years (range 0.5–7.1 years). Within the cohort, six of 29 (21%) children at diagnosis were infants (<4 years old). Metastatic stage was determined according to Chang’s criteria and pathology was centrally reviewed by a panel of neuropathologists from UK Children’s Cancer and Leukemia Group (CCLG) according to current WHO criteria (Chang et al., 1969; Louis et al., 2007). Clinical data were collated and centrally reviewed. Genomic DNA was extracted using standard methods, and validation of paired sample identity was performed using a panel of microsatellite markers (see below). Human tumor samples were provided by the UK CCLG as part of CCLG-approved biological study BS-2007-04; informed consent was obtained from all subjects. Human tumor investigations were conducted with approval from Newcastle/North Tyneside Research Ethics Committee (study reference 07/Q0905/71).
Selection and Assessment of Critical Medulloblastoma Molecular Features
Established medulloblastoma molecular features, with validated relationships to disease molecular pathology and prognosis, were assessed. These comprised (1) the four consensus medulloblastoma molecular subgroups associated with distinct molecular events, clinicopathological features, and prognosis (Taylor et al., 2012); (2) MYC and MYCN amplification (predominant in MBGroup3 and MBSHH/Group4, respectively), and associated with poor outcome (Ellison et al., 2011; Northcott et al., 2012a; Pfister et al., 2009; Pizer and Clifford, 2009; Ryan et al., 2012); (3) TP53, one of the most frequently mutated genes in medulloblastoma, associated with MBWNT/SHH, and reduced survival rates in the MBSHH subgroup (Northcott et al., 2012a; Zhukova et al., 2013); (4) additional defects of the P53 pathway (CDKN2A deletion/methylation, MDM2 amplification, and p53 nuclear accumulation) linked to poor outcome in other pediatric embryonal tumors including relapsed neuroblastoma (Carr-Wilkinson et al., 2010; Frank et al., 2004); (5) CTNNB1 mutation, associated with MBWNT (Taylor et al., 2012); (6) polyploidy, associated with genomic instability, MBGroup3/MBGroup4 and poor prognosis (Jones et al., 2012; Northcott et al., 2012a); and (7) defects of chromosome 17, including the most common medulloblastoma cytogenetic abnormalities (i.e., gains of 17q, isochromosome 17q [i{17q}], and loss of 17p; Ellison et al., 2011; Pfister et al., 2009; Taylor et al., 2012), associated with MBGroup3/MBGroup4 and poor survival (Pfister et al., 2009; Shih et al., 2014).
Molecular Subgroup Status
All samples, where DNA was of sufficient quantity and quality as assessed by PicoGreen dsDNA quantitation assay (Life Technologies), were processed on the 450K methylation array (Illumina). Subgrouping according to methylation status was achieved using established methods (Hovestadt et al., 2013; Schwalbe et al., 2013). Consensus nonnegative matrix factorization (NMF) clustering of a 225 member primary medulloblastoma training cohort was used to define four methylation-dependent disease subgroups by identifying subgroup-specific metagenes. A support vector machine (SVM) classifier to assign subgroup for additional diagnostic and relapsed medulloblastoma samples, based on their projected metagene profiles (Tamayo et al., 2007), was developed using previously published methods (Schwalbe et al., 2013). Confidence of the classifier call made for these samples was assessed by repeated sampling of 80% of the training cohort to rederive the classifier. Mutational analysis of CTNNB1 (Table S1) (Taylor et al., 2012) was performed as previously described (Ellison et al., 2005, 2011) (see Supplemental Experimental Procedures).
Copy-Number Analysis in Clinical Samples
Copy-number estimates were carried out using iFISH, microsatellite typing, or multiplex ligation-dependent probe amplification (MLPA) using SALSA reagents (MRC-Holland). Copy-number assessment by iFISH of MYC (8q24.21 probes), MYCN (2p24.3 probes), and chromosome 17 imbalances (17p13.3 and 17q12 probes) versus respective centromeric reference loci was performed on available material as previously described (Lamont et al., 2004; Langdon et al., 2006; Nicholson et al., 2000). One hundred nonoverlapping nuclei were scored by two independent assessors, and amplification was defined as previously reported (Ryan et al., 2012).
Copy-number assessment by MLPA of MYC, MYCN, and MDM2 were measured relative to four independent reference loci (B2M, TBP, 7q31, and 14q22). Normal diploid control samples were used to define cutoffs for the detection of elevated copy numbers (>95% confidence interval of the normal distribution). Tumor samples showing reproducibly elevated copy numbers (in multiple replicates and versus three or more reference loci) were deemed to have copy-number elevation. Samples with evidence of raised copy number by MLPA were validated by iFISH on available material against a panel of normal copy-number tumor controls.
Copy-number analysis of CDKN2A (p14ARF) was performed using polymorphic microsatellite markers for chromosome 9p21 (d9s942 and d9s1748) as previously reported (Randerson-Moor et al., 2001). Copy-number status of three cases homozygous for both polymorphic microsatellite markers, suggestive of chromosomal deletion at the CDKN2A locus (Berggren et al., 2003), was further assessed by 450K methylation array (Sturm et al., 2012) (n = 2) or the Illumina Human Omniexpress array (Illumina (n = 1). Methylation of CDKN2A was also assessed by 450K methylation array.
Analysis of TP53 Status in Clinical Samples
Immunohistochemistry (IHC) in human samples for p53 immunopositivity, previously associated with TP53 mutation (Pfaff et al., 2010; Tabori et al., 2010), was performed on formalin-fixed, paraffin-embedded (FFPE) samples (M7001, Dako) using the Menapath Polymer HRP Detection system (A. Menarini Diagnostics). All samples were analyzed by a neuropathologist, blind to mutation status, and by a nuclear stain algorithm (Spectrum, Aperio Technologies). TP53 mutation status was assessed by direct PCR-based DNA sequence analysis, and one tumor pair was assessed by next-generation sequencing (see Supplemental Experimental Procedures).
Statistical Analysis of Clinical Samples
Chi-square and Fisher’s exact tests were used to assess associations between clinicopathological and molecular features, and p values were corrected for multiple testing using the Bonferroni procedure (Abdi, 2007). The log rank test was used to assess all univariate survival markers. Cox proportional hazards models were used to investigate the significance of variables for event-free survival (EFS), overall survival (OS), and time to death (TTD) analyses in (1) univariate and (2) multivariate models using forward likelihood-ratio testing.
In Vivo Studies
All experimental protocols were monitored and approved by The Institute of Cancer Research Animal Welfare and Ethical Review Body, in compliance with guidelines specified by the UK Home Office Animals (Scientific Procedures) Act 1986 and the United Kingdom National Cancer Research Institute guidelines for the welfare of animals in cancer research (Workman et al., 2010). GTML mice have been described previously (Swartling et al., 2010). The Trp53KI/KI mice were kindly provided by G.I. Evan (Christophorou et al., 2005) and crossed with GTML animals into a background of the FVB/NJ inbred strain (Taketo et al., 1991). To image for bioluminescence expression, animals were injected with 75 mg/kg D-luciferin in saline (PerkinElmer) prior to imaging in the IVIS Lumina (PerkinElmer) using Living Image Software. Transgenic GTML/Trp53KI/KI animals with bioluminescence signals higher than 1.5 × 10−9 photons/seconds (20–30 days of life) were randomized to treatment groups and treated with 30 mg/kg MLN8237 (Alisertib, Millennium) or 50 mg/kg GDC-0449 (Vismodegib, LC Laboratories). MLN8237, GDC-0449, and the respective vehicles were dosed orally on a daily basis. Doxycycline was given via chow at 1,250 mg/kg diet to provide a daily dose of approximately 160 mg/kg. Restoration of wild-type p53 was achieved by administration of either 1 mg of tamoxifen dissolved in 100 μl peanut oil carrier daily by intraperitoneal injection or via chow at 400 mg/kg diet to provide a daily dose of approximately 64 mg/kg. Animals were monitored twice a week for bioluminescence signal and were sacrificed upon detection of a signal higher than 9 × 10−9 photons/second or overt signs of intracranial expansion associated with tumor growth. Mice were allowed access to food and water ad libitum.
In Vivo Imaging
Multislice 1H MRI was performed on a 7T horizontal bore microimaging system (Bruker Instruments) using a 3 cm birdcage coil and a 2.5 × 2.5 cm field of view. Anesthesia was induced with a 10 ml/kg intraperitoneal injection of fentanyl citrate (0.315 mg/ml) plus fluanisone (10 mg/ml, Hypnorm, Janssen Pharmaceutical), midazolam (5 mg/ml, Hypnovel, Roche), and sterile water (1:1:2). Core body temperature was maintained by warm air blown through the magnet bore. Magnetic-field homogeneity was optimized by shimming over the entire brain using an automated shimming routine (FASTmap). T2-weighted images acquired using a rapid acquisition with refocused echoes (RARE) sequence (12 contiguous 1 mm sagittal slices or 20 contiguous 1 mm axial slices, 256 × 256 matrix, four averages, echo times [TE] = 36 and 132 ms, repetition time [TR] = 4.5 s, RARE factor = 8) were used for localization of the tumor and measurement of tumor volume.
Neurosphere Isolation and Culture
Tissue isolated from GTML/Trp53KI/KI tumors was transferred into cold HBSS, cut into 2–3 mm2 pieces and dissociated before trituration in medium and filtration through 70 μm mesh. To generate neurospheres, cells were cultured under self-renewal conditions in DMEM/F12 medium (Life Technologies) supplemented with 2% B27 supplement (Life Technologies), 20 ng/ml epidermal growth factor (Sigma-Aldrich), and 20 ng/ml fibroblast growth factor (Life Technologies). For in vitro analyses, cells were treated with the following drug concentrations: 100 nM 4-OHT (Sigma-Aldrich), 1 μg/ml doxycycline (Sigma-Aldrich), 100 nM MLN8237, and 500 nM GDC-0449. Neurosphere formation was assessed by performing limiting dilutions from 1,000 to 60 cells and imaging using a Celigo S Imaging Cell Cytometer (Brooks Life Science Systems).
Western Blot Analysis and IHC
Western blot analysis of mouse tissues and neurospheres was performed as previously described (Brockmann et al., 2013; Chesler et al., 2006). For IHC of mouse tissues, samples were fixed in 4% paraformaldehyde in phosphate buffered saline for at least 24 hr, decalcified with 0.3 M EDTA, and processed using a Leica ASP300S tissue processor. Sections were cut at 4 μM for hematoxylin and eosin staining (H&E) staining and immunohistochemistry as previously described (Chesler et al., 2006). Antibodies used were MYCN (OP-13, Merck-Millipore), Ki-67 (556003, BD Biosciences), GFAP (Z0334, DAKO), Cleaved Caspase 3 (9664, Cell Signaling Technology), Synaptophysin (180130, Life Technologies), Phospo-S10-Histone H3 (9706, Cell Signaling), phospho-AurkABC (2914, Cell Signaling), AurkA (4718, Cell Signaling), Sonic Hedgehog (ab73958, Abcam), Gli-1 (2534, Cell Signaling), and GAPDH (2118, Cell Signaling).
Author Contributions
L.C. and S.C.C. conceived the study. S.L.N. and S.C. collected and processed human tissue cohorts. D.H., B.P., D.W.E., and A.M. provided human tumor samples. S.B., S.C.C., and R.M.H. collected and centrally reviewed clinical data. R.M.H., J.C.L., and S.C.C. designed experiments on human tumor cohorts, which were carried out by R.M.H., J.C.L., and S.L.R. E.C.S. planned and executed human 450K methylation array analysis. R.M.H., J.C.L., E.C.S., and S.C.C. planned and carried out all other analyses of human tumor data. T.S.J., K.R., and S.B.W. performed central pathology review of human tumors. A.J. performed p53 immunohistochemistry analysis. S.K., K.P., F.J.S., W.A.W., and L.C. planned mouse experiments, which were carried out by S.K. and A.H. MRI of tumors was planned by J.K.R.B. and S.P.R. and carried out by J.K.R.B. In vivo compound measurement was planned by R.R. and F.I.R. and carried out by R.R. S.K., K.P., and L.C. planned experiments to characterize tumor biology and response to therapeutics, which were executed by S.K., K.B., Z.A., E.P., L.H., and C.K.; S.K., K.P., and L.C. analyzed these data. D.W. planned and executed gene expression analysis of mouse tumors. Histopathological analysis of mouse tumors was performed by T.S.J. K.P., R.M.H., L.C., and S.C.C. wrote the manuscript.
Acknowledgments
This study was supported by grants from Cancer Research UK (grants C34648/A12054, C8464/A13457, and C1060/A10334), Action Medical Research (RTF1414), Sparks (09NCL02), The Brain Tumour Charity (grants SDR004X and 16/164), the JGW Patterson Foundation, and Christopher’s Smile (CXC002H) and was undertaken as part of the INSTINCT network, cofunded by The Brain Tumour Charity, Great Ormond Street Children’s Charity, and Children with Cancer UK (grant 16/193). T.S.J. is supported by the National Institute for Health Research and a Great Ormond Street Hospital UCL Biomedical Research Centre award. F.I.R. and R.R. are employees of the Institute of Cancer Research and are involved in the development of aurora kinase inhibitors.
Footnotes
This is an open access article under the CC BY license (http://creativecommons.org/licenses/by/3.0/).
Contributor Information
Louis Chesler, Email: louis.chesler@icr.ac.uk.
Steven C. Clifford, Email: steve.clifford@ncl.ac.uk.
Accession Numbers
The Gene Expression Omnibus (GEO) accession number for 450K DNA methylation array profiles used for the determination of human medulloblastoma molecular subgroup status is GSE62618. The GEO accession number for microarray expression profiles of mouse medulloblastomas is GSE62625. The GEO SuperSeries accession number for this study is GSE62626.
Supplemental Information
References
- Abdi H. Bonferroni and Sidak corrections for multiple comparisons. In: Salkind N.J., editor. Encyclopedia of Measurement and Statistics. Sage; Thousand Oaks, CA: 2007. [Google Scholar]
- Berggren P., Kumar R., Sakano S., Hemminki L., Wada T., Steineck G., Adolfsson J., Larsson P., Norming U., Wijkstrom H., Hemminki K. Detecting homozygous deletions in the CDKN2A(p16(INK4a))/ARF(p14(ARF)) gene in urinary bladder cancer using real-time quantitative PCR. Clin. Cancer Res. 2003;9:235–242. [PubMed] [Google Scholar]
- Brockmann M., Poon E., Berry T., Carstensen A., Deubzer H.E., Rycak L., Jamin Y., Thway K., Robinson S.P., Roels F. Small molecule inhibitors of aurora-a induce proteasomal degradation of N-myc in childhood neuroblastoma. Cancer Cell. 2013;24:75–89. doi: 10.1016/j.ccr.2013.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carol H., Reynolds C.P., Kang M.H., Keir S.T., Maris J.M., Gorlick R., Kolb E.A., Billups C.A., Geier B., Kurmasheva R.T. Initial testing of the MDM2 inhibitor RG7112 by the Pediatric Preclinical Testing Program. Pediatr. Blood Cancer. 2013;60:633–641. doi: 10.1002/pbc.24235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr-Wilkinson J., O’Toole K., Wood K.M., Challen C.C., Baker A.G., Board J.R., Evans L., Cole M., Cheung N.K., Boos J. High Frequency of p53/MDM2/p14ARF Pathway Abnormalities in Relapsed Neuroblastoma. Clin. Cancer Res. 2010;16:1108–1118. doi: 10.1158/1078-0432.CCR-09-1865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang C.H., Housepian E.M., Herbert C., Jr. An operative staging system and a megavoltage radiotherapeutic technic for cerebellar medulloblastomas. Radiology. 1969;93:1351–1359. doi: 10.1148/93.6.1351. [DOI] [PubMed] [Google Scholar]
- Chène P. Inhibiting the p53-MDM2 interaction: an important target for cancer therapy. Nat. Rev. Cancer. 2003;3:102–109. doi: 10.1038/nrc991. [DOI] [PubMed] [Google Scholar]
- Chesler L., Schlieve C., Goldenberg D.D., Kenney A., Kim G., McMillan A., Matthay K.K., Rowitch D., Weiss W.A. Inhibition of phosphatidylinositol 3-kinase destabilizes Mycn protein and blocks malignant progression in neuroblastoma. Cancer Res. 2006;66:8139–8146. doi: 10.1158/0008-5472.CAN-05-2769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christophorou M.A., Martin-Zanca D., Soucek L., Lawlor E.R., Brown-Swigart L., Verschuren E.W., Evan G.I. Temporal dissection of p53 function in vitro and in vivo. Nat. Genet. 2005;37:718–726. doi: 10.1038/ng1572. [DOI] [PubMed] [Google Scholar]
- Ellison D.W., Onilude O.E., Lindsey J.C., Lusher M.E., Weston C.L., Taylor R.E., Pearson A.D., Clifford S.C. beta-Catenin status predicts a favorable outcome in childhood medulloblastoma: the United Kingdom Children’s Cancer Study Group Brain Tumour Committee. J. Clin. Oncol. 2005;23:7951–7957. doi: 10.1200/JCO.2005.01.5479. [DOI] [PubMed] [Google Scholar]
- Ellison D.W., Kocak M., Dalton J., Megahed H., Lusher M.E., Ryan S.L., Zhao W., Nicholson S.L., Taylor R.E., Bailey S., Clifford S.C. Definition of disease-risk stratification groups in childhood medulloblastoma using combined clinical, pathologic, and molecular variables. J. Clin. Oncol. 2011;29:1400–1407. doi: 10.1200/JCO.2010.30.2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank A.J., Hernan R., Hollander A., Lindsey J.C., Lusher M.E., Fuller C.E., Clifford S.C., Gilbertson R.J. The TP53-ARF tumor suppressor pathway is frequently disrupted in large/cell anaplastic medulloblastoma. Brain Res. Mol. Brain Res. 2004;121:137–140. doi: 10.1016/j.molbrainres.2003.11.016. [DOI] [PubMed] [Google Scholar]
- Gustafson W.C., Meyerowitz J.G., Nekritz E.A., Chen J., Benes C., Charron E., Simonds E.F., Seeger R., Matthay K.K., Hertz N.T. Drugging MYCN through an allosteric transition in Aurora kinase A. Cancer Cell. 2014;26:414–427. doi: 10.1016/j.ccr.2014.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hovestadt V., Remke M., Kool M., Pietsch T., Northcott P.A., Fischer R., Cavalli F.M., Ramaswamy V., Zapatka M., Reifenberger G. Robust molecular subgrouping and copy-number profiling of medulloblastoma from small amounts of archival tumour material using high-density DNA methylation arrays. Acta Neuropathol. 2013;125:913–916. doi: 10.1007/s00401-013-1126-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones D.T., Jäger N., Kool M., Zichner T., Hutter B., Sultan M., Cho Y.J., Pugh T.J., Hovestadt V., Stütz A.M. Dissecting the genomic complexity underlying medulloblastoma. Nature. 2012;488:100–105. doi: 10.1038/nature11284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawauchi D., Robinson G., Uziel T., Gibson P., Rehg J., Gao C., Finkelstein D., Qu C., Pounds S., Ellison D.W. A mouse model of the most aggressive subgroup of human medulloblastoma. Cancer Cell. 2012;21:168–180. doi: 10.1016/j.ccr.2011.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kool M., Korshunov A., Remke M., Jones D.T., Schlanstein M., Northcott P.A., Cho Y.J., Koster J., Schouten-van Meeteren A., van Vuurden D. Molecular subgroups of medulloblastoma: an international meta-analysis of transcriptome, genetic aberrations, and clinical data of WNT, SHH, Group 3, and Group 4 medulloblastomas. Acta Neuropathol. 2012;123:473–484. doi: 10.1007/s00401-012-0958-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamont J.M., McManamy C.S., Pearson A.D., Clifford S.C., Ellison D.W. Combined histopathological and molecular cytogenetic stratification of medulloblastoma patients. Clin. Cancer Res. 2004;10:5482–5493. doi: 10.1158/1078-0432.CCR-03-0721. [DOI] [PubMed] [Google Scholar]
- Langdon J.A., Lamont J.M., Scott D.K., Dyer S., Prebble E., Bown N., Grundy R.G., Ellison D.W., Clifford S.C. Combined genome-wide allelotyping and copy number analysis identify frequent genetic losses without copy number reduction in medulloblastoma. Genes Chromosomes Cancer. 2006;45:47–60. doi: 10.1002/gcc.20262. [DOI] [PubMed] [Google Scholar]
- Lannering B., Rutkowski S., Doz F., Pizer B., Gustafsson G., Navajas A., Massimino M., Reddingius R., Benesch M., Carrie C. Hyperfractionated versus conventional radiotherapy followed by chemotherapy in standard-risk medulloblastoma: results from the randomized multicenter HIT-SIOP PNET 4 trial. J. Clin. Oncol. 2012;30:3187–3193. doi: 10.1200/JCO.2011.39.8719. [DOI] [PubMed] [Google Scholar]
- Louis D.N., Ohgaki H., Wiestler O.D., Cavenee W.K., Burger P.C., Jouvet A., Scheithauer B.W., Kleihues P. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007;114:97–109. doi: 10.1007/s00401-007-0243-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McManamy C.S., Pears J., Weston C.L., Hanzely Z., Ironside J.W., Taylor R.E., Grundy R.G., Clifford S.C., Ellison D.W. Nodule formation and desmoplasia in medulloblastomas-defining the nodular/desmoplastic variant and its biological behavior. Brain Pathol. 2007;17:151–164. doi: 10.1111/j.1750-3639.2007.00058.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholson J., Wickramasinghe C., Ross F., Crolla J., Ellison D. Imbalances of chromosome 17 in medulloblastomas determined by comparative genomic hybridisation and fluorescence in situ hybridisation. Mol. Pathol. 2000;53:313–319. doi: 10.1136/mp.53.6.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Northcott P.A., Jones D.T., Kool M., Robinson G.W., Gilbertson R.J., Cho Y.J., Pomeroy S.L., Korshunov A., Lichter P., Taylor M.D., Pfister S.M. Medulloblastomics: the end of the beginning. Nat. Rev. Cancer. 2012;12:818–834. doi: 10.1038/nrc3410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Northcott P.A., Shih D.J., Peacock J., Garzia L., Morrissy A.S., Zichner T., Stütz A.M., Korshunov A., Reimand J., Schumacher S.E. Subgroup-specific structural variation across 1,000 medulloblastoma genomes. Nature. 2012;488:49–56. doi: 10.1038/nature11327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pei Y., Moore C.E., Wang J., Tewari A.K., Eroshkin A., Cho Y.J., Witt H., Korshunov A., Read T.A., Sun J.L. An animal model of MYC-driven medulloblastoma. Cancer Cell. 2012;21:155–167. doi: 10.1016/j.ccr.2011.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfaff E., Remke M., Sturm D., Benner A., Witt H., Milde T., von Bueren A.O., Wittmann A., Schöttler A., Jorch N. TP53 mutation is frequently associated with CTNNB1 mutation or MYCN amplification and is compatible with long-term survival in medulloblastoma. J. Clin. Oncol. 2010;28:5188–5196. doi: 10.1200/JCO.2010.31.1670. [DOI] [PubMed] [Google Scholar]
- Pfister S., Remke M., Benner A., Mendrzyk F., Toedt G., Felsberg J., Wittmann A., Devens F., Gerber N.U., Joos S. Outcome prediction in pediatric medulloblastoma based on DNA copy-number aberrations of chromosomes 6q and 17q and the MYC and MYCN loci. J. Clin. Oncol. 2009;27:1627–1636. doi: 10.1200/JCO.2008.17.9432. [DOI] [PubMed] [Google Scholar]
- Pizer B.L., Clifford S.C. The potential impact of tumour biology on improved clinical practice for medulloblastoma: progress towards biologically driven clinical trials. Br. J. Neurosurg. 2009;23:364–375. doi: 10.1080/02688690903121807. [DOI] [PubMed] [Google Scholar]
- Pizer B., Donachie P.H., Robinson K., Taylor R.E., Michalski A., Punt J., Ellison D.W., Picton S. Treatment of recurrent central nervous system primitive neuroectodermal tumours in children and adolescents: results of a Children’s Cancer and Leukaemia Group study. Eur. J. Cancer. 2011;47:1389–1397. doi: 10.1016/j.ejca.2011.03.004. [DOI] [PubMed] [Google Scholar]
- Ramaswamy V., Remke M., Bouffet E., Faria C.C., Perreault S., Cho Y.J., Shih D.J., Luu B., Dubuc A.M., Northcott P.A. Recurrence patterns across medulloblastoma subgroups: an integrated clinical and molecular analysis. Lancet Oncol. 2013;14:1200–1207. doi: 10.1016/S1470-2045(13)70449-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randerson-Moor J.A., Harland M., Williams S., Cuthbert-Heavens D., Sheridan E., Aveyard J., Sibley K., Whitaker L., Knowles M., Bishop J.N., Bishop D.T. A germline deletion of p14(ARF) but not CDKN2A in a melanoma-neural system tumour syndrome family. Hum. Mol. Genet. 2001;10:55–62. doi: 10.1093/hmg/10.1.55. [DOI] [PubMed] [Google Scholar]
- Robinson G., Parker M., Kranenburg T.A., Lu C., Chen X., Ding L., Phoenix T.N., Hedlund E., Wei L., Zhu X. Novel mutations target distinct subgroups of medulloblastoma. Nature. 2012;488:43–48. doi: 10.1038/nature11213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudin C.M., Hann C.L., Laterra J., Yauch R.L., Callahan C.A., Fu L., Holcomb T., Stinson J., Gould S.E., Coleman B. Treatment of medulloblastoma with hedgehog pathway inhibitor GDC-0449. N. Engl. J. Med. 2009;361:1173–1178. doi: 10.1056/NEJMoa0902903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutkowski S., Gerber N.U., von Hoff K., Gnekow A., Bode U., Graf N., Berthold F., Henze G., Wolff J.E., Warmuth-Metz M. Treatment of early childhood medulloblastoma by postoperative chemotherapy and deferred radiotherapy. Neuro-oncol. 2009;11:201–210. doi: 10.1215/15228517-2008-084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan S.L., Schwalbe E.C., Cole M., Lu Y., Lusher M.E., Megahed H., O’Toole K., Nicholson S.L., Bognar L., Garami M. MYC family amplification and clinical risk-factors interact to predict an extremely poor prognosis in childhood medulloblastoma. Acta Neuropathol. 2012;123:501–513. doi: 10.1007/s00401-011-0923-y. [DOI] [PubMed] [Google Scholar]
- Schwalbe E.C., Williamson D., Lindsey J.C., Hamilton D., Ryan S.L., Megahed H., Garami M., Hauser P., Dembowska-Baginska B., Perek D. DNA methylation profiling of medulloblastoma allows robust subclassification and improved outcome prediction using formalin-fixed biopsies. Acta Neuropathol. 2013;125:359–371. doi: 10.1007/s00401-012-1077-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shakhova O., Leung C., van Montfort E., Berns A., Marino S. Lack of Rb and p53 delays cerebellar development and predisposes to large cell anaplastic medulloblastoma through amplification of N-Myc and Ptch2. Cancer Res. 2006;66:5190–5200. doi: 10.1158/0008-5472.CAN-05-3545. [DOI] [PubMed] [Google Scholar]
- Shih D.J., Northcott P.A., Remke M., Korshunov A., Ramaswamy V., Kool M., Luu B., Yao Y., Wang X., Dubuc A.M. Cytogenetic prognostication within medulloblastoma subgroups. J. Clin. Oncol. 2014;32:886–896. doi: 10.1200/JCO.2013.50.9539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sturm D., Witt H., Hovestadt V., Khuong-Quang D.A., Jones D.T., Konermann C., Pfaff E., Tönjes M., Sill M., Bender S. Hotspot mutations in H3F3A and IDH1 define distinct epigenetic and biological subgroups of glioblastoma. Cancer Cell. 2012;22:425–437. doi: 10.1016/j.ccr.2012.08.024. [DOI] [PubMed] [Google Scholar]
- Swartling F.J., Grimmer M.R., Hackett C.S., Northcott P.A., Fan Q.W., Goldenberg D.D., Lau J., Masic S., Nguyen K., Yakovenko S. Pleiotropic role for MYCN in medulloblastoma. Genes Dev. 2010;24:1059–1072. doi: 10.1101/gad.1907510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabori U., Baskin B., Shago M., Alon N., Taylor M.D., Ray P.N., Bouffet E., Malkin D., Hawkins C. Universal poor survival in children with medulloblastoma harboring somatic TP53 mutations. J. Clin. Oncol. 2010;28:1345–1350. doi: 10.1200/JCO.2009.23.5952. [DOI] [PubMed] [Google Scholar]
- Taketo M., Schroeder A.C., Mobraaten L.E., Gunning K.B., Hanten G., Fox R.R., Roderick T.H., Stewart C.L., Lilly F., Hansen C.T. FVB/N: an inbred mouse strain preferable for transgenic analyses. Proc. Natl. Acad. Sci. USA. 1991;88:2065–2069. doi: 10.1073/pnas.88.6.2065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamayo P., Scanfeld D., Ebert B.L., Gillette M.A., Roberts C.W., Mesirov J.P. Metagene projection for cross-platform, cross-species characterization of global transcriptional states. Proc. Natl. Acad. Sci. USA. 2007;104:5959–5964. doi: 10.1073/pnas.0701068104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor M.D., Northcott P.A., Korshunov A., Remke M., Cho Y.J., Clifford S.C., Eberhart C.G., Parsons D.W., Rutkowski S., Gajjar A. Molecular subgroups of medulloblastoma: the current consensus. Acta Neuropathol. 2012;123:465–472. doi: 10.1007/s00401-011-0922-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Maerken T., Rihani A., Van Goethem A., De Paepe A., Speleman F., Vandesompele J. Pharmacologic activation of wild-type p53 by nutlin therapy in childhood cancer. Cancer Lett. 2014;344:157–165. doi: 10.1016/j.canlet.2013.11.002. [DOI] [PubMed] [Google Scholar]
- Workman P., Aboagye E.O., Balkwill F., Balmain A., Bruder G., Chaplin D.J., Double J.A., Everitt J., Farningham D.A.H., Glennie M.J., Committee of the National Cancer Research Institute Guidelines for the welfare and use of animals in cancer research. Br. J. Cancer. 2010;102:1555–1577. doi: 10.1038/sj.bjc.6605642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhukova N., Ramaswamy V., Remke M., Pfaff E., Shih D.J., Martin D.C., Castelo-Branco P., Baskin B., Ray P.N., Bouffet E. Subgroup-specific prognostic implications of TP53 mutation in medulloblastoma. J. Clin. Oncol. 2013;31:2927–2935. doi: 10.1200/JCO.2012.48.5052. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.