Abstract
Surgical sterilization is a relatively permanent form of contraception that has been disproportionately used by Black, Hispanic, and Native American women in the United States in the past. We use a nationally representative sample of 4,609 women ages 25 to 45 to determine whether sterilization continues to be more common and consequential by race for reproductive-age women. Results indicate that Native American and Black women are more likely to be sterilized than non-Hispanic White women, and Hispanic and Native American women are more likely than non-Hispanic White women to report that their sterilization surgeries prevent them from conceiving children they want. Reasons for sterilization differ significantly by race. These findings suggest that stratified reproduction has not ended in the United States and that the patterns and consequences of sterilization continue to vary by race.
Keywords: Sterilization, Reproduction, Regret, Race, Ethnicity, Stratification
1. Introduction
The second most common form of contraception in the United States is surgical sterilization. Not all sterilizations, however, are performed for contraceptive reasons. Sterility, the inability to have (additional) children, is frequently the consequence of treating a health condition that might make pregnancy or childbearing difficult or impossible. An estimated 10.3 million American women are sterilized in the U.S. (Chandra et al. 2005). From the mid-1960s through the mid-1980s, sterilization changed from being an unpopular method of contraception to being the favored method for over 40% of contracepting couples (Bumpass 1987).
Yet sterilization rates vary by race, with Black and Native American women twice as likely as White women to have undergone tubal sterilization (Volscho 2010). The differential rates are particularly surprising given that women who identify as belonging to a marginalized racial/ethnic group are less likely to have health insurance, receive reproductive health care, or be satisfied with the quality of their health care (Ebrahim et al. 2009). The over-representation of women from racial/ethnic minority groups among women who are sterilized raises the possibility of “stratified reproduction” (Colen 1990; Ginsburg and Rapp 1991). Stratified reproduction describes how reproduction is structured across social and cultural boundaries in ways that provide some women more ability to realize their reproductive goals than other women. In an attempt to understand disproportionate racial sterilization patterns, Shapiro and colleagues (1983) outlined several competing theories that we draw from in this study. This stratification could be the result of medical bias or social pressure to limit fertility. It could also be the result of socioeconomic factors that prevent women from being able to afford as many children as they would like to have or of health disparities related to socioeconomic status (SES) or lifestyle behaviors. On the other hand, differential sterilization rates could simply reflect differential childbearing and family structure patterns or fertility limitation desires by race. In order to shed light on the racial dynamics of sterilization rates, it is essential to try and determine why women undergo sterilization surgery and whether the surgery prevents them from having desired children.
In this study, we use data from the National Survey of Fertility Barriers (NSFB), a survey of 4,787 women that is representative of reproductive age women in the United States. We measure patterns of sterilization, reasons for sterilization, and unrealized desires for a wanted child due to sterilization by race/ethnicity. The study includes sterilization, regret, and race for all surgeries resulting in female sterilization. There are five racial groups with sufficient numbers of cases for analyses (e.g., Black, Hispanic, White, Asian, and Native American), and we limit the sample to heterosexual women. We include women whose partners had a vasectomy because partner situation could explain racial differences in sterilization experiences. Because many characteristics associated with fertility differ by race/ethnicity, we include socioeconomic status (e.g., education and household income); life course (e.g., age, relationship status, employment and education status); fertility history (e.g., pregnancy before age 18, history of unplanned pregnancy, number of children, partner vasectomy); and values/attitudes (e.g. religiosity, importance of motherhood1, importance of career, and importance of leisure) in our analyses. We include additional sterilization characteristics (e.g., type of surgery, time since sterilization, young age at sterilization, and reasons for sterilization) in the analysis of sterilization regret.
1.1. Historical and contemporary reproduction
Female sterilization surgery is a technology with the potential to either enhance or reduce control over reproduction (Schoen 2005). Sterilization can offer women a sense of reproductive control and empowerment if freely chosen, but many women have been surgically sterilized as a result of overt or subtle coercion, often at the time of having a child (Gutierrez 2008; Lawrence 2000; Lopez 2008; Schoen 2005; Solinger 2005; Stern 2005; Torpy 2000). Reproductive politics has always been part and parcel of the process of racial formation in the U.S. (Collins 1990; Roberts 1997; Solinger 2005). Negative characterizations of sexuality and reproductive behavior of less privileged social groups of women continue to be used to justify both the meaning of racial categories and differential treatment of less privileged racial groups (Chavez 2004; Hartouni 1994; Roberts 1997; Solinger 2005; Szkupinski-Quiroga 2007). There are documented connections between sexuality, reproduction, and racial formation among Black Americans (Roberts 1997; Collins 2000). Before Emancipation, Black women were exploited economically for their labor and ability to produce offspring as slaves, as well as sexually by White men (King 1988). Collins (2000) posits that negative stereotypes about female slaves’ hypersexuality and hyperfertility provided a justification for their sexual exploitation. Black women today live with these lingering stereotypes in the form of negative public images that depict Black women as sexually promiscuous or aggressive; overly fecund and irresponsibly having too many babies; and neglectful, lazy mothers (Collins 2000).
In more recent U.S. history, there is evidence of overt and subtle coercion leading to sterilization among Mexican American (Guitierrez 2008), Puerto Rican (Lopez 2008), Native American, and Black women (Solinger 2005). From the 1920s through the 1970s, scientists and doctors who deemed certain women “unsuitable” to reproduce followed eugenic logic and coerced those women to become sterilized, regardless of their desire for more children. From the 1950s through the 1970s, these tactics were especially aimed at marginalized women, including Black, Native American, Hispanic, immigrant and poor women of all racial groups, including White women (Gutierrez 2008; Lawrence 2000; Lopez 2008; Schoen 2005; Solinger 2005; Stern 2005; Torpy 2000). Medical personnel and government employees who believed individual women and society as a whole would be better off restricting reproduction primarily to White women with more economic means often pressured or coerced marginalized women into sterilizations (Bell 2009; Roberts 1997; Stern 2005; Torpy 2000). In addition, women who were not explicitly coerced into surgical sterilization still often felt economic pressure to have fewer children than they wanted, due in part to a dearth of policy supports such as paid maternity leave and expensive child care, and they often felt they had access to few options other than sterilization for limiting births (King and Meyer 1997; Solinger 2005).
In the United States, raising children can be costly. The Health and Human Services’ “Poverty Guidelines” suggest that the cost is around $4,000 a year (HHS 2013). One major reason that women seek abortions is the concern that they cannot afford to care for a(nother) child (Finer et al. 2005)). The common idea that children, particularly single women having children when they are young, causes poverty is not supported by evidence (Lichter and Crowley 2002). Yet recent proposed and realized policies target women’s fertility as a way to address poverty (Cozzarelli et al. 2001). For example, during the 1990s, 35 states proposed financial reimbursements for women on welfare who were implanted with a long-term birth control method, Norplant (Thomas 1998). Currently, 23 states have implemented family caps for welfare recipients, which limit or eliminate the incremental cash assistance associated with additional family members; supporters have argued (erroneously) that family caps incentivize women on welfare to limit their fertility (Wallace 2009). Economically disadvantaged women often internalize beliefs about fertility control and social problems as well. For example, a study of homeless women in Appalachia showed that though they were young and many would have liked more children, the large majority did not think that they had any practical alternatives to sterilization (Badagliacco 1999).
1.2. Explanations for racialized sterilization patterns
In an attempt to ascertain whether there are systematic and persistent differences in who is sterilized, Shapiro and colleagues (1983) outlined and examined several competing theories that might explain historical and contemporary racial differences in sterilization rates. The fertility thesis proposes that racially marginalized women have higher rates of sterilization because they have more children and at younger ages; thus minority women are less likely to desire more children. The altruistic thesis asserts that there are racial differences in sterilization rates because there are racial differences in proportions of women who want to be sterilized. The racial argument claims that there is reproductive racism; racially marginalized women are more likely to be sterilized because they are more likely to be pressured or recommended to be sterilized. Finally, the class argument proposes that women of lower socioeconomic status—who are also more likely to be racially marginalized—are more likely to be sterilized because of reproductive practices and policies aimed at preventing women from having children that they cannot support. Whereas the first two theories suggest that sterilizations are meeting needs which happen to be greater for racially marginalized women, the latter two theories imply stratified reproduction (Shapiro et al. 1983).
Shapiro and colleagues found strong support for the class theory, but they argued that “future conceptual efforts in this area need to develop more elaborate frameworks” (1983:1853). Much of the theorizing in the nearly three decades since has focused on stratified reproduction and reproductive policies and programs, but empirical studies on sterilization differences tend to focus on economic or demographic factors.
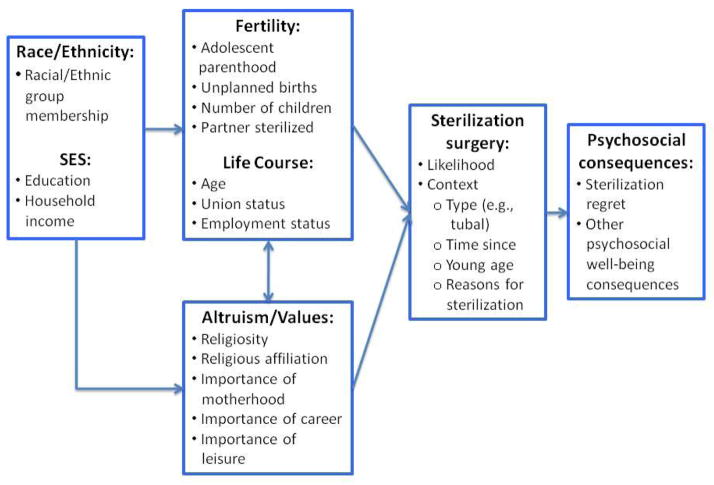
We propose to extend Shapiro and colleagues’ (1983) framework with additional correlates from more recent sterilization studies (see Figure 1). We bring in a life course perspective with the addition of age, union status, and fertility history. We also attempt to tease apart the “altruistic” hypothesis to include attitudes and values considerations for why women may prefer (or not prefer) sterilization. Finally, we examine sterilization context as well as likelihood and suggest that there are important psychosocial outcomes following sterilization that are dependent upon context. We examine the following research questions:
Figure 1.
Conceptual Model of Sterilization Odds, Context, and Psychosocial Consequences.
Note: Expanded from Shapiro et al. (1983) framework.
Do perceived reasons for sterilization differ by race?
Can racial differences in sterilization rates be explained by socioeconomic, life course, fertility history, and attitudes/values variables?
Do perceptions of sterilization as a barrier to childbearing (regret) differ by race, and if so, can racial differences be explained by socioeconomic, fertility/life course, attitudes/values, and sterilization history (including reason for sterilization surgery) variables?
1.3. Correlates of Surgical Sterilization and Racial/Ethnic Differences
Surgical sterilization is a common form of contraception in the United States, although not all sterilizing surgeries are for contraception. The majority of sterilization surgeries for women are tubal ligations (69%), followed by hysterectomies (17 %); other surgeries comprise 11% of all surgeries resulting in female sterilization (Chandra et al. 2005). Prior research has identified a variety of correlates of sterilization surgery. Surgical sterilization is more common among those with lower incomes and lower educational levels. Women with more children (higher parity) and women who intend no more children are more likely to undergo sterilization (Mosher et al. 2004). Married women are somewhat more likely than cohabiting women, and considerably more likely than never-married-non-cohabiting women, to get sterilized (Mosher et al. 2004). More religious women are less likely to be sterilized (Bumpass et al. 2000). Parity at the time of last wanted birth is strongly associated with sterilization (Bumpass et al. 2000). Sterilizations are more common for women on Medicaid and for women living in rural areas (Bass and Warehime 2009).
Race/ethnicity continues to consistently predict sterilization odds. According to national surveys, Black and Native American women are about twice as likely to have had tubal sterilization as non-Hispanic Whites (Borrero et al. 2010; Volscho 2010). As our data is similarly nationally representative, we expect to find similar racial/ethnic differences in sterilization patterns.
Prior research has determined that some of the racial/ethnic differences in sterilization rates are explained by socio-demographic characteristics that differ by race/ethnicity. Partner vasectomy is one example; non-Hispanic White married men are nearly 3.5 times more likely to have vasectomies than married men of other races/ethnicities (Anderson et al., 2010), which accounts for some of the racial difference in women’s tubal ligation rates. However, Black women remain more likely to undergo tubal sterilization than White women after controlling for partner vasectomy status (Borrero et al. 2009b). Sterilization rates are also higher among older women. Black women, however, continue to be sterilized at much younger ages than White women; 31% of never married Black women have been sterilized by the age of 30 compared to only 10% of never married White women (Bumpass et al. 2000).
Because many of the characteristics associated with sterilization are also associated with race/ethnicity, it is possible that race/ethnicity associations are more indirect, stemming from broader social patterns, than being directly due to racial bias. For example, Borrero et al. (2010) found that, after controlling for a history of unintended pregnancies, the relationship between race and sterilization was no longer significant. Volscho (2010), however, found that race differences in sterilization rates persisted when he controlled for social class, parity, age, marital status and insurance status. We hope to shed light on these inconsistencies by using a large sample with more comprehensive fertility history and value/attitude measures.
1.4. Reasons for Sterilization and Regret
We expect that women undergo surgical sterilization for a variety of reasons. Many women voluntarily undergo sterilization surgeries because they do not want more children and view sterilization as a preferred method of contraception. These women often associate sterilization with such social outcomes as improvements in marital relationships and more enjoyable sex (Miller et al. 1989). Another reason may be counsel by a medical provider suggesting sterilization (Badagliacco and Ruiz 2006). Contraceptive options presented by medical providers differ by race, and Hispanic women are particularly likely to be counseled regarding sterilization (Borrero et al. 2009a; Downing, LaVeist, and Bullock, 2007). When women report that they were sterilized for a medical reason, it is often unclear if the procedures were really medically necessary or if they were presented as such but were really coercion (see e.g. Guitierrez 2008). To our knowledge, racial/ethnic differences in reasons for sterilization surgery have not been studied using a national data set.
Because sterilization is a relatively permanent form of contraception, women who use this method for contraception may later wish that they could conceive and therefore see sterilization as preventing childbearing. Other women may undergo sterilization surgery for a medically necessary reason despite desiring more children. Sterilization regret is usually assessed by asking people if they desire more children, by asking if they would like to have the procedure reversed or by studying women who present themselves for sterilization reversal or in-vitro fertilization (IVF). Using the 1982 National Survey of Family Growth (NSFG), Henshaw and Singh (1986) found that 26% of couples who had a tubal ligation or vasectomy desired more children, and 10% expressed a desire for sterilization reversal. A study of women who received surgical sterilizations at fifteen medical centers in nine cities found that 14.3% of the women requested information about the possibility of a reversal over a fourteen-year period (Schmidt et al. 1999).
Prior research has identified several correlates predicting sterilization regret or desire for sterilization reversal. Women who have tubal ligations at younger ages are significantly more likely to experience sterilization regret than are older women (Boring et al. 1988: Curtis et al. 2006; Kariminia et al. 2002; Marcil-Gratton 1988; Miller et al. 1991, 1993). Change in marital status and a concomitant desire to have children with a new partner, perceived pressure to have the surgery, and sterilization based on medical necessity are also associated with higher odds of regretting sterilization surgery (Boring et al. 1988; Kariminia et al. 2002; Miller et al. 1991, 1993). Poor women of all races are more likely to opt for sterilization without fully weighing the long-term personal costs, such as the possibility of being unable to conceive a new baby in the event of entering into a new relationship (Young 1999).
Several studies have examined racial/ethnic differences in sterilization regret or desire for reversal. The 1982 NSFG (Henshaw and Singh 1986) revealed that both Black and Hispanic women were over-represented among those who wished to have the procedure reversed. A study of Puerto Rican women in New York City found that women’s reproductive decisions were limited by their lack of knowledge about their reproductive systems and their ability to evaluate their physician’s advice (Lopez 2008). Lopez (2008) suggested that the women in her sample made a distinction between “tying” and “cutting” fallopian tubes, often believing that if their tubes are tied, they will be able to get pregnant again. Language, education, options and resources are associated with misunderstandings about the consequences of this procedure. Age at sterilization can affect desire for sterilization reversal; Borrero and colleagues (2008) found that older Black women are more likely than White women to desire reversal. Further, a study of 191 Black and White women who had undergone tubal sterilization found that Black women were nearly twice as likely as White women to think that sterilization reversal could easily restore fertility (62% vs. 36%) and nearly three times as likely to believe that a woman’s sterilization would reverse itself after five years (60% vs. 23%) (Borrero et al. 2011).
When sterilization is not freely chosen, as is the case for many surgeries due to medical problems, it can lead to regret and psychological distress for women and couples. A longitudinal study of 1140 premenopausal women who underwent hysterectomy surgery revealed that over 10% of the women expressed regret about not being able to have (more) children, and these women exhibited higher levels of depression, anxiety, anger, and confusion that persisted during the two years that the study followed them after their surgeries (Leppert et al. 2007). However, the study did not examine racial/ethnic differentials in sterilization regret or psychosocial well-being. We extend knowledge on racial/ethnic differences in sterilization regret with our analysis using contemporary national data, inclusion of racial and ethnic groups beyond White, Black, and Hispanic, and a comprehensive set of correlates, including fertility history and sterilization history characteristics.
1.5. Statement of the problem
After we account for economic, life course and fertility history factors, is sterilization still more common and more consequential among racially “other” women compared to White women in the United States, and do the reasons for sterilization differ between groups? Civil rights activists (Solinger 2005), law suits (Guitierrez 2008), changing federal guidelines (Solinger 2005), and increased awareness of health disparities (Smedley et al. 2002) should have contributed to more consistent medical practices across racial/ethnic subgroups. The history of coercive sterilization practices aimed at marginalized women in the United States, however, suggests that Black, Hispanic, and Native American women may still be subject to subtle pressures to become sterilized. Alternatively, sterilization rates and regrets may differ by race for socioeconomic or health reasons, or fertility history. If women constructed as “racially other” experience more pressure to be sterilized or have more reproductive or other health-related problems than non-Hispanic White women, then wanting to conceive at some point after the sterilization surgery should also be more likely among women in racially marginalized groups.
2. The current study: Materials and methods
2.1. Data
Our data come from the National Survey of Fertility Barriers (NSFB), a random digit dialing telephone survey of 4,787 women of childbearing ages (25 to 45) and a subset of their husbands/partners. Collected in 2005–2006 by the Survey Research Center at the Pennsylvania State University and the Bureau for Sociological Research at the University of Nebraska at Lincoln, the data are nationally representative, with an oversample of Black and Hispanic women and women with fertility problems. Internal review board approval was obtained from both institutions. Methodological information can be accessed at: http://sodapop.pop.psu.edu/codebooks/nsfb/wave1/. The public data files can be accessed at: http://sodapop.pop.psu.edu/data-collections/nsfb. Our sample is restricted to 4,609 White, Black, Hispanic, Asian, and Native American women who responded to the questions regarding surgical sterilizations.
The study was designed to assess social and health factors related to reproductive choices and fertility for U.S. women. A “planned missing” design was used during interviews to minimize respondent burden. This design was applied to several of the scales that we use in this study. Respondents were asked two-thirds of multi-item scales with one third of the items omitted randomly by design. Because these items were missing completely at random (Allison 2002), they do not bias results. The mean of available items is used in creating final scale scores for scales with planned missing items. The response rate was 53.7% (AAPOR RR4), which is typical for RDD telephone surveys conducted in the last several years (McCarty et al. 2006). Extensive comparisons with Census data indicate the NSFB weighted sample is representative of women aged 25–45 in the United States.
Remaining missing data were imputed with ICE in Stata. Ten imputed datasets were created and estimates from each dataset were combined using the MIM procedure. The r-square values were estimated as the average r-square from the ten datasets. Descriptive analyses are weighted to account for the oversamples and differential nonresponse. Weights are not used in the logistic regression analyses as the variables used to generate the weights are included as independent variables in the models, yielding more efficient estimates than when weights are used (Winship and Radbill 1994).
2.2. Concepts and measures
Dependent Variables
Our dichotomous measure of Sterilization comes from the question, “Have you ever had a surgery that makes it difficult or impossible to have a baby?” where 1=yes and 0=no. This allows for a broader measure of surgical sterilization than in much of the literature, which is often restricted to tubal ligation surgeries. There are two main reasons for using this broader measure of sterilization. First, many of the coercive sterilizations of the past were not tubal ligations but hysterectomies. Second, using a broader definition of sterilization allows us to examine the full range of reasons for sterilizing surgeries and to examine whether the reasons for sterilization are associated with later wanting a child and therefore perceiving sterilization as a barrier to childbearing. Regret is a dichotomous measure (1=yes; 0=no) based on the question, “Did this surgery prevent you from having children that you wanted to have?”
Independent and Control Variables
We assessed race using two standard questions based on Census wording: “What race or races do you consider yourself to be?” and “Do you consider yourself to be either Hispanic or Latino or neither one?” Individuals who reported more than one race were classified according to coding rules that gave first priority to identification as “Native American,” second priority to identification as “Hispanic,” and third priority to identification as “Black.” Based on this coding, we constructed dummy variables for Black, Hispanic, Asian, and Native American compared to White, the reference category. Those indicating “other” were eliminated from the analysis due to small cell counts. We recognize that all race groups contain heterogeneous subgroups, but use these larger categories as indicators of gross distinctions, indicating primary patterns of racial formation in the U.S.
We included two measures of socioeconomic status. Education is a continuous variable, measured in years. Household income is an ordinal variable ranging from 1 (lowest) to 12 (highest). A number of life course variables were also included. Age is measured in years and ranges from 25 to 45. Union status is measured in different ways depending on the dependent variable by two dummy variables: Ever married is the indicator variable in the sterilization patterns analysis, whereas new relationship is the union variable in the sterilization regret analysis. Pregnant younger than 18 is a dichotomous variable indicating whether the respondent’s first pregnancy occurred when she was 17 or younger. For each pregnancy, respondents were asked if they were “trying to, trying not to, or okay either way” about getting pregnant. Ever unplanned pregnancy is a dichotomous variable in which a “trying not to” response for any pregnancy is coded as a 1. Parity is measured by four indicator variables: No children (the reference category), one child, two children, and three or more children. To assess whether a partner’s vasectomy is associated with sterilization patterns or regret, a dichotomous variable indicating a “partner vasectomy” is coded as a 1.
Several additional variables related to the experience of the sterilization surgery are included as control variables in the sterilization regret analysis. Respondents were also asked for the date of sterilization, and Years since sterilization was calculated based on the date given and the date of the interview. There was a skip pattern problem and the date of sterilization was not asked for a subset of cases who reported that sterilization was not a barrier to having more children and were in a union (N = 280). These cases were included in the analysis with the date imputed. Young age at sterilization is a dichotomous variable indicating young age at sterilization surgery (1 = younger than 30 at the time of the surgery). A measure of the type of sterilization based on the question, “What type of surgery was this,” is a dichotomous measure where 1= tubal ligation surgery and 0=other type of surgery resulting in sterilization.
Reasons for being sterilized
The survey instrument included the question, “Women have these surgeries for a variety of reasons. Why did you have this surgery?” This question appeared in the interview schedule if the respondent indicated that she had been surgically sterilized. Interviewers had been previously trained to “check all that apply” to a list of 12 possible reasons, which had been created using prior research or drawn from the National Survey of Family Growth (NSFG). The list included reasons such as “I had all that I wanted,” “My spouse/partner had all he wanted,” “Financial reasons,” and “Problems with my female organs.” In addition, the interviewer could select “Other,” and type in the appropriate response(s). Of the 1,191 women who reported reasons for being sterilized, 201 responses were coded as “other” at the time of the interview and recorded as open-ended data. The authors read all of the open-ended responses and created additional categories reflecting reasons for being sterilized that were not included in the original set of options, resulting in a total of 16 categories (see Table 2).
Table 2.
Percentage Distribution of Sterilization Reasons by Race (N = 1,191), Weighted.
| Reason for sterilization | White | Black | Hispanic | Asian | Native American |
|---|---|---|---|---|---|
| Voluntary reasons | 44.20 | 53.50 | 39.60 | 23.70 | 33.30 |
|
|
|||||
| 1. Had all that I wanted | 43.70 | 53.50 | 39.60 | 23.70 | 33.30 |
| 2. All done | .50 | .00 | .00 | .00 | .00 |
| Situational reasons | 7.20 | 4.20 | 11.30 | 4.10 | 3.80 |
|
|
|||||
| 3. Financial reasons | 2.40 | .80 | 5.50 | .00 | .00 |
| 4. Age | 2.00 | 1.40 | 1.90 | 4.10 | 1.90 |
| 5. Relationship issues | 2.80 | 2.00 | 3.90 | .00 | 1.90 |
| Health reasons | 54.10 | 37.20 | 44.70 | 5.90 | 50.40 |
|
|
|||||
| 6. Reproductive health problem | 34.50 | 24.70 | 26.50 | .00 | 25.50 |
| 7. Would probably lose a pregnancy | 8.30 | 5.20 | 10.40 | 5.90 | 8.70 |
| 8. Would probably have an unhealthy child | 1.00 | .80 | .50 | .00 | .00 |
| 9. Complications in prior pregnancies/deliveries | 1.20 | 1.10 | .00 | .00 | .00 |
| 10. Health problem (non-reproductive) | 9.10 | 5.40 | 7.30 | .00 | 16.20 |
| Pressured by others | 8.30 | 3.60 | 6.20 | 49.40 | 13.30 |
|
|
|||||
| 11. Partner had all that he wanted | 1.40 | .40 | 1.50 | 4.10 | 4.00 |
| 12. Family pressure | .20 | 1.50 | .00 | .00 | 4.00 |
| 13. Dr. recommended | 6.70 | 1.70 | 4.70 | 45.30 | 5.30 |
| Other reason | 2.00 | 3.50 | 9.50 | 25.10 | 6.30 |
|
|
|||||
| 14. Other reason | 1.80 | 1.40 | 8.80 | 25.10 | 6.30 |
| 15. Don’t know | .00 | .00 | .70 | .00 | .00 |
| 16. Refused | .20 | 2.10 | .00 | .00 | .00 |
| No. of cases (N) | (647) | (288) | (212) | (9) | (35) |
Note: Percentages are weighted; Ns are unweighted. Percentages for underlined reasons indicate the sum for all responses in that group.
Percentages add to over 100% due to opportunity for selecting more than one reason.
Because reasons do not straightforwardly map onto “voluntary” and “involuntary,” we did not simply dichotomize reasons into these two categories. Situational reasons, health reasons, and pressure from others are associated with something less than full “voluntariness,” but they may represent varying degrees of “involuntariness.” Medical options often involve constrained choices (Bird and Rieker 2008). For example, women who are sterilized due to situational reasons may feel like they have more of a “choice” than those who see their sterilizations as undesirable but unavoidable because of health reasons. Those who feel pressured by others into surgical sterilization may feel more remorse due to lack of control (Elson 2008). The various categories were therefore collapsed into a set of five more general categories. These categories are similar to those used in the National Survey of Family Growth (see Groves et al. 2009), though we include additional categories of “situational” and “pressure from others.” The final scheme consists of voluntary sterilization (including “had all I wanted” and “all done”) (N=393), situational sterilization (including “financial reasons,” “age,” and “relationship issues”) (N=62), health-related sterilization (including “problem with female organs,” “probably would not have a healthy pregnancy,” “probably would not have a healthy child,” “health problems unrelated to reproductive problems,” and “difficult prior pregnancies/deliveries”) (N=514), and pressure from others (including “partner had all he wanted,” “doctor recommended sterilization,” and “pressure from family members other than spouse/partner” (N=96). Other reason (N=41) includes those who reported “Don’t know” and “Refused” as well as 38 women who could not be classified into another category due to interviewer data entry error and missing data.
Because women’s perceptions of their sterilization experiences are open to interpretation, we consider these “fuzzy” categories that capture respondents’ statements in a general way only. We may interpret women’s statements somewhat differently than they intended. For example, two doctors could recommend sterilization for health reasons to two women, but one woman might report “health reasons” and the other “doctor recommended.” The “pressure from others” category is particularly problematic. How do we know whether family pressure is more or less influential, for example, than a doctor’s recommendation? The degree of coercion involved in some of these reasons is especially hard to assess. Doctors may recommend surgery for sound health reasons or they might use their medical influence to coax a woman to make a decision they think is socially desirable. Likewise, “health reasons’ could indicate the existence of a valid medical reason for sterilization, but doctors could also cite “health reasons’ as a means of influencing a woman to make the decision to be sterilized. Further, women in different racial/ethnic groups may interpret the same recommendation from a health care provider in different ways due to cultural factors, such as communication styles or trust in providers. Finally, even a reason such as “had all I wanted” could be less voluntary than it would seem at first glance. If women say that they had all the children they wanted, are they speaking in terms of their general desires or of limited opportunities and circumstances? Nonetheless, we suspect that the level of coercion involved in the “voluntary” category is less than the level of coercion involved in the other categories.
Because women could select more than one reason for sterilization, we created a hierarchy to generate mutually exclusive and all-encompassing groups. In this coding system (Other reason → voluntary → situational → health → pressure from others), “pressure from others” was treated as the most inclusive category and “other reason” as the least inclusive, residual category. Women who reported sterilization due to others’ pressure were classified into the “pressure from others” category, regardless of any other reasons they provided. Women who gave a “health-related” reason, but not a “pressure from others” reason were classified as “health-related,” and so on.
We also included several measures of values. Religiosity is a 4-item scale made up of the following questions: 1) “How often do you attend religious services?” 2) “About how often do you pray?” 3) “How close do you feel to God most of the time?” and 4) “In general, how much would you say your religious beliefs influence your daily life? Would you say…Very much to none.” Because religiosity questions had differences in answer categories, the variables were 1) coded so that higher numbers indicate greater religiosity, 2) standardized, and 3) added to form a scale. These items form a single factor and have a high reliability (α =.78 for the total sample). Because the Catholic religion has specific teachings about birth control, we include an indicator of Catholic (=1) versus all other religions (=0). Importance of motherhood is a 4-item scale composed of the following items: 1) “Having children is important to my feeling complete as a woman;” 2) “I always thought I’d be a parent;” 3) “I think my life will be or is more fulfilling with children;” and 4) “It is important for me to have children.” Responses ranged from “Strongly Disagree” to “Strongly Agree” and were added to form a scale where higher values indicate greater importance of motherhood. The Cronbach’s alpha is high (α=.86 for the entire sample). Importance of successful career (“How important is being successful in your line of work?” 1 = not at all important to 4 = very important) and importance of leisure (“How important is having leisure time to enjoy your own interests?” 1 = not at all important to 4 = very important) are included as continuous variables.
2.3. Analytic strategy
We compared proportion sterilized, proportion regretting sterilization, and the other characteristics in the analyses by race/ethnicity using Tukey’s HSD post hoc test to assess significant differences between racial/ethnic groups. To assess the direct and adjusted associations between the race/ethnicity categories and the odds of sterilization or sterilization regret, we used binary logistic regression. The analyses of the reasons for sterilization and the odds of regret used only the subset of women who were sterilized, introducing a risk of selection effects influencing the results. Therefore, we ran analyses including Mills’ ratio from a Heckman model to adjust for selection effects. Because the central significant effects were consistent across the models, we present the original results. The Heckman analyses results are available upon request.
3. Results
3.1. Descriptive Statistics
Table 1 summarizes descriptive statistics by race. The results indicate that surgical sterilization rates differ considerably by race. Surgical sterilization is more common among Native American (42%) and Black women (36%) compared to White women (30%). Surgical sterilization is less likely among Asian women (17%) than all other groups. Among women who have been surgically sterilized, more White (32%), Hispanic (41%) and Native American women (60%) wanted a child after sterilization compared to Black women (26%). Although rates of sterilization are much lower among Asian women, over a third of the women who were sterilized now want more children.
Table 1.
Weighted Descriptive Statistics of Study Variables (N = 4,609)
| Variables | White (N=2649) | Black (N = 916) | Hispanic (N = 836) | Asian (N = 106) | Native American (N = 85) | Post hoc | |
|---|---|---|---|---|---|---|---|
|
|
|
|
|
||||
| M or % | M or % | M or % | M or % | M or % | p | Tukey’s HSD | |
| Surgically sterilized | 30.32% | 36.12% | 31.69% | 17.03% | 42.40% | *** | NA>B>H,W>A |
| Sterilization regret3 | 32.47% | 25.62% | 40.68% | 38.04% | 59.53% | *** | NA>H,A>W,B |
| Socioeconomic status | |||||||
| Years of education | 14.18 | 13.46 | 11.41 | 16.29 | 13.08 | *** | A>W>B,NA>H |
| Household income (median) | 61398 | 39404 | 36732 | 64147 | 43543 | *** | A,W>NA>B,H |
| Life course | |||||||
| Age | 36.07 | 35.14 | 33.96 | 34.69 | 35.35 | *** | W>NA,B,A>H |
| Union status | |||||||
| Ever married | 86.16% | 53.12% | 75.70% | 82.34% | 67.47% | *** | W>A>H,NA>B |
| New relationship | 27.04% | 37.68% | 15.54% | 0.00% | 66.89% | *** | NA>B,W>H,A |
| Employment status | |||||||
| Not working | 27.06% | 22.45% | 35.88% | 15.89% | 32.14% | *** | H>NA>W,B>A |
| In school | 2.38% | 6.90% | 8.25% | 5.30% | 7.38% | *** | H>NA>B>A>W |
| Part-time | 16.06% | 9.94% | 14.40% | 9.55% | 8.30% | *** | W>H>B>A,NA |
| Full-time | 54.50% | 60.70% | 41.47% | 69.26% | 52.17% | *** | A,B,NA>W>H |
| Fertility history | |||||||
| Pregnant younger than 18 | 20.24% | 35.32% | 35.42% | 4.90% | 35.59% | *** | NA,H,B>W>A |
| Ever unplanned pregnancy | 37.50% | 62.59% | 51.25% | 23.04% | 59.18% | *** | B,NA,H>W,A |
| Parity | |||||||
| No children | 21.46% | 17.52% | 10.47% | 34.44% | 23.72% | *** | A>NA,W,B>H |
| 1 child | 19.16% | 19.86% | 15.39% | 29.42% | 11.01% | *** | A>B,W>H,NA |
| 2 children | 33.87% | 27.96% | 28.91% | 31.04% | 30.66% | * | W,A,NA>H,B |
| 3+ children | 25.52% | 34.66% | 45.23% | 5.10% | 34.62% | *** | H>B,NA>W>A |
| Partner vasectomy | 17.06% | 2.65% | 4.43% | 2.49% | 7.78% | *** | W>NA,HB,A |
| Values/Attitudes | |||||||
| Religiosity | −.13 | .31 | .09 | −.24 | .13 | *** | B>NA>H>W,A |
| Catholic | 22.15% | 7.58% | 61.91% | 18.89% | 12.80% | *** | H>W,A>NA,B |
| Importance of motherhood | 3.31 | 3.07 | 3.19 | 3.37 | 3.26 | *** | A,NA,W>H>B |
| Importance of career | 3.18 | 3.50 | 3.45 | 3.38 | 3.48 | *** | B,NA,H,A>W |
| Importance of leisure | 3.15 | 3.34 | 3.24 | 3.18 | 3.35 | *** | NA,B,H,A>W |
| Sterilization history1 | |||||||
| Years since sterilization | 7.98 | 8.90 | 7.37 | 5.54 | 10.68 | ** | NA>B,W>H,A |
| Young age at sterilization | 45.43% | 35.84% | 42.36% | 19.00% | 65.35% | *** | NA>W,H,B>A |
| Tubal sterilization | 60.29% | 66.18% | 57.43% | 64.62% | 66.42% | ||
| Reason for sterilization | |||||||
| Voluntary | 33.45% | 48.94% | 29.00% | 18.50% | 30.57% | *** | B>W,NA>H>A |
| Situational | 5.76% | 3.61% | 9.00% | 0.00% | 1.83% | * | H>W,B>NA,A |
| Health-related | 43.44% | 32.94% | 34.17% | 5.54% | 46.29% | *** | NA,W>H,B>A |
| Pressured by others | 8.27% | 3.60% | 6.12% | 46.77% | 8.95% | *** | A>NA,W>H,B |
| Other reason | 1.90% | 3.45% | 9.34% | 23.79% | 6.13% | *** | A>H>NA>B,A |
Note: Means are weighted; N are unweighted; Women who reported “other race” as their only race/ethnicity are excluded.
Note:
Restricted to women who have been surgically sterilized. W=White; B=Black; H=Hispanic; A=Asian; NA=Native American
p<.05.
p<.01.
p<.001.
Years of education and household income also vary by race. Asian women have the highest average educational attainment, followed by White, Black, Native American, and Hispanic women. Asian and White women have significantly higher household incomes than Black and Native American women. There are also significant differences by race among the life course variables. Average age in this sample is higher among White women and lower among Hispanic women than women in the other groups. Marriage rates differ considerably between the groups: the proportion ever married is much lower among Black women (53%) compared to 86% among white women and 82% among Asian women. Hispanic women are over-represented among the unemployed and least likely to be working full-time.
Racial differences in fertility history variables are also quite striking. First pregnancies before age 18 are less common among Asian (5%) and White (20 %) women than among Black (35%), Hispanic (35%), and Native American (36%) women. Ever experiencing an unplanned pregnancy also varies considerably by race; a minority of Asian (23%) and White (38%) women reported that they were “trying not to” get pregnant for at least one pregnancy, whereas a majority of Black (63%), Hispanic (52%), and Native American (59%) women have experienced a pregnancy that they were try to avoid. Parity differences are also large; for example more Asian (34%) and Native American (24%) women have no children, but Hispanic women (10%) are less likely to have no children. White women (17%) are significantly more likely than women in other racial/ethnic groups to have a partner who has had a vasectomy.
There are also differences in values by race. Black women have the highest religiosity scores and Asian and White women the lowest. The majority of Hispanic women (62%) are Catholic. Importance of motherhood also varies by race: White, Asian, and Native American women have the highest and Black women the lowest importance of motherhood scores. Black, Native American, and Hispanic women are most likely and White women are least likely to say that career success is very important. White women are the least likely to say that leisure is very important.
Among women who are sterilized, retrospective reports of reasons for sterilization as well as contextual factors vary by race/ethnicity, except for having had tubal sterilization, which does not differ significantly by race/ethnicity. More Native American women (65%) report being under 30 when they were sterilized. Table 2 presents a more detailed view of the coded categories created from women’s retrospective reports of reasons why they underwent surgical sterilization by race. The bolded numbers in the table provide the total percentage for the general five categories and the remaining numbers show the detailed percentages of specific statements within each category. The bolded categories sum to more than 100% because women could report more than one reason, but in the multivariate analyses they are placed in only one category as described above.
The majority of Native American women who had been sterilized reported reproductive and other health problems (50%). Approximately one-third of Native American women reported being surgically sterilized because they had had all the children they wanted. Among the very few Asian women who had been surgically sterilized, the majority reported the reason as suggestion or pressure from others, followed by “other reasons”, and no desire for more children. Hispanic women were more likely to report financial reasons for their sterilization than other groups, but this is still not a common reason (5.5%). No desire for more children is the most common specific reason among Hispanic women, although more women reported health reasons overall. Black women were the most likely to say that no desire for additional children motivated their sterilization, followed by health reasons, particularly reproductive health problems. Very few Black women said that financial reasons motivated their decision to be surgically sterilized. White women were most likely to be sterilized for health reasons, primarily reproductive health reasons, although many also chose sterilization because they did not desire more children.
We also examined how type of sterilization surgery was associated with race/ethnicity. The vast majority of sterilization surgeries that were not tubal ligation (e.g., hysterectomy, ovaries removed or other type of surgery) were due to health reasons for women in all racial/ethnic groups. Reasons for tubal ligation surgery differed by race/ethnicity, however (see Figure 2). Among women who had tubal ligations, white and black women were more likely to attribute their surgeries to voluntary reasons. A greater percentage of Hispanic women with tubal ligations reported situational reasons for their surgeries. A particularly high percentage of Asian women with tubal ligation surgeries reported pressure or suggestions from others, but the overall low number of Asian women with tubal ligation surgeries does not allow us to presume conclusions from these findings.
Figure 2.
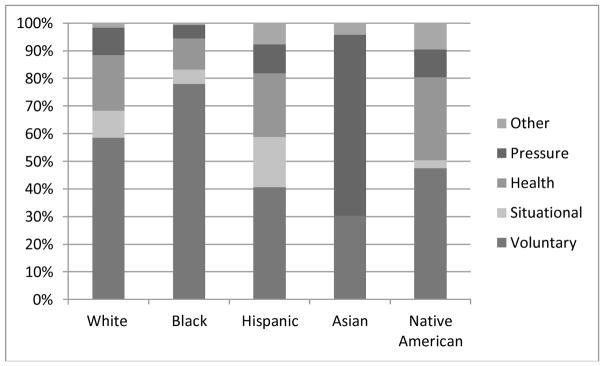
Reasons for Tubal Ligation Surgery by Race/Ethnicity.
3.2. Is race associated with the odds of sterilization?
Table 3 presents the binary logistic regression analysis of the odds of sterilization. Model 1 displays coefficients for race categories before control variables are entered. Compared to White women, Black (exp(B) = 1.52; p<.001) and Native American women (exp(B) = 2.43; p<.01) have higher odds and Asian women have lower odds (exp(B)=.49; p<.001) of surgical sterilization. There is no difference between Hispanic and White women in this baseline model. This model accounts for only a very small proportion of the variation in sterilization rates (Pseudo R2 =.01; BIC=5562.9). Adding education and income does not make the race coefficients non-significant, but it does alter them. For example, in Model 1 the coefficient for Hispanic was positive and non-significant, but in Model 2 it is negative and significant (exp(B) =.73; p<.001), indicating that Hispanic women are less likely to have surgical sterilization after controlling for socioeconomic status. Controlling for education and income, Asian women no longer have a statistically significant likelihood of sterilization surgery than White women. The coefficients for the other groups are in the same direction and still statistically significant, but are now weaker, suggesting that some of the effect is mediated by socioeconomic status. Women with more education (exp(B) =.85; p<.001) and greater household income (exp(B) = .95; p<.01) have significantly lower odds of sterilization. Model 2 still accounts for only a small proportion of the variance (Pseudo R2 =.05; BIC=5359.1).
Table 3.
Logistic Regression of the Likelihood of Being Surgically Sterile (N = 4,567).
| Variables | Model 1
|
Model 2
|
Model 3
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| B | SE | Exp(B) | B | SE | Exp(B) | B | SE | Exp(B) | |
| Race/Ethnicity (White) | |||||||||
| Black | .42 | .08 | 1.52 *** | .25 | .09 | 1.29 ** | −.04 | .10 | .96 |
| Hispanic | .12 | .09 | 1.13 | −.32 | .10 | .73 ** | −.28 | .11 | .76 * |
| Asian | −.72 | .27 | .49 ** | −.41 | .28 | .66 | −.29 | .29 | .75 |
| Native American | .89 | .21 | 2.43 *** | .69 | .22 | 1.99 ** | .54 | .25 | 1.72 * |
| Socioeconomic status | |||||||||
| Years of education | −.16 | .01 | .85 *** | −.09 | .02 | .91 *** | |||
| Household income | −.05 | .01 | .95 ** | −.05 | .02 | .95 ** | |||
| Life course | |||||||||
| Age | .09 | .01 | 1.10 *** | ||||||
| Union status | |||||||||
| Ever married | −.19 | .10 | .83 | ||||||
| Employment status (Not employed) | |||||||||
| In school | −.31 | .19 | .73 | ||||||
| Part-time | −.51 | .12 | .60 *** | ||||||
| Full-time | −.21 | .09 | .81 * | ||||||
| Fertility History | |||||||||
| Pregnant younger than 18 | .32 | .09 | 1.37 ** | ||||||
| Ever unplanned pregnancy | .28 | .08 | 1.32 ** | ||||||
| Parity (No children) | |||||||||
| 1 child | .14 | .15 | 1.15 | ||||||
| 2 children | 1.07 | .13 | 2.91 *** | ||||||
| 3+ children | 1.24 | .14 | 3.46 *** | ||||||
| Partner vasectomy | −1.23 | .14 | .29 *** | ||||||
| Values | |||||||||
| Religiosity | .00 | .01 | 1.00 | ||||||
| Catholic | −.38 | .09 | .68 *** | ||||||
| Importance of motherhood | .01 | .02 | 1.01 | ||||||
| Importance of successful career | .10 | .05 | 1.10 * | ||||||
| Importance of leisure | −.04 | .05 | .96 | ||||||
| Constant | −1.06 | .04 | *** | 1.71 | .21 | −3.14 | .45 | *** | |
|
| |||||||||
| Pseudo R2 | .01 | .05 | .16 | ||||||
| BIC | 5562.9 | 5359.1 | 4884.9 | ||||||
Note: Reference categories in parentheses.
p<.001;
p>.01;
p<.05.
Model 3 shows the coefficients for the race/ethnicity groups after adding adjustments for life course, fertility history, and values measures. This model accounts for a larger proportion of the variation in sterilization (Pseudo R2 =.17), and the lower Bayesian information criterion (BIC) of 4884.9 suggests a better model fit. For all groups, there are only minor changes in the odds ratios in this model, but the coefficient for Black women is no longer statistically significant. This suggests that most of the higher odds of sterilization for Black women stems from indirect associations through differential life course timing and patterns -- particularly regarding fertility and employment -- as well as differences in values that are associated with sterilization. For the remaining groups, the persistence of an association for Native American and Hispanic women suggests that “race/ethnicity” captures social processes that contribute to racialized reproductive practices. Education and income continue to have a negative association with the odds of sterilization (exp(B)=.91; p<.001 and exp(B)=.95; p<.01, respectively).
Most of the life course and fertility history variables are associated with the odds of sterilization. Each additional year of age is associated with a 10% increase in the odds of sterilization (exp(B)=1.10; p<.001). Women with part-time (exp(B)=.60; p<.001) and full-time employment are less likely to be sterilized than unemployed women (exp(B)=.81; p<.05). Women who were pregnant when they were younger than 18 (exp(B)=1.37; p<.001) and women who have ever had an unplanned pregnancy (exp(B)=1.32; p<.01) are more likely to be sterilized. Women with two children (exp(B)=2.91; p<.001) and women with 3 or more children (exp(B)=3.46; p<.001) are considerably more likely than women without children to be surgically sterilized. Women who have a current partner who has had a vasectomy are significantly less likely to be sterilized (exp(B)=.29; p<.001).
Only two values indicators are associated with the odds of sterilization. Women who are Catholic have lower odds of sterilization compared to women in other religious denominations (exp(B) =.68; p<.001), and women who place a high value on career success have higher odds of sterilization (exp(B) = 1.10; p<.05). Model 3, therefore, shows that both social class and race are associated with the odds of sterilization. These results suggest that some, but not all, of the apparent race associations reflect social class differences related to timing of childbearing and marital status differences between groups.
3.3. Is race associated with the odds of perceiving sterilization as a barrier to conceiving a child?
In Table 4, we show the binary logistic regression analysis of the association between sterilization regret measured by a desire to have children among women who have been sterilized (N = 1,191). Variables are added in the same sequence used in the analysis of the odds of sterilization. Contrary to expectations, Black women do not report that sterilization prevented them from having desired children more often than White women – the odds are lower but not significantly different once life course, fertility history, and values are added into the analysis in Model 3. Hispanic and Native American women, however, do have significantly higher odds of viewing sterilization as a barrier to having desired children, and these associations are not mediated by any of the variables included in the analyses. As Model 4 indicates, the odds of perceiving sterilization as blocking the realization of childbearing desires are almost double for Hispanic (exp(B) = 1.74; p<.01) and Native American women (exp(B)=2.43; p<.05) compared to White women. Education and income are not associated with perceiving sterilization as blocking the realization of childbearing desires (regret) in any of the models.
Table 4.
Logistic Regression of the Likelihood of Sterilization Regret (N = 1,191).
| Variables | Model 1
|
Model 2
|
Model 3
|
Model 4
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | Exp(B) | B | SE | Exp(B) | B | SE | Exp(B) | B | SE | Exp(B) | |
| Race/Ethnicity (White) | ||||||||||||
| Black | −.34 | .16 | .71 * | −.35 | .16 | .71 * | −.23 | .18 | .79 | −.12 | .19 | .89 |
| Hispanic | .58 | .16 | 1.79 *** | .54 | .17 | 1.72 ** | .63 | .19 | 1.88 ** | .55 | .20 | 1.74 ** |
| Asian | .67 | .71 | 1.96 | .71 | .71 | 2.03 | .98 | .73 | 2.67 | .59 | .76 | 1.81 |
| Native American | .89 | .34 | 2.43 * | .87 | .34 | 2.39 * | .87 | .36 | 2.38 * | .89 | .37 | 2.43 * |
| Socioeconomic status | ||||||||||||
| Years of education | −.03 | .03 | .97 | −.04 | .03 | .96 | −.02 | .03 | .98 | |||
| Household income | .00 | .02 | 1.00 | .00 | .03 | 1.00 | −.02 | .03 | .98 | |||
| Life course | ||||||||||||
| Age | .00 | .01 | 1.00 | −.01 | .02 | .99 ** | ||||||
| Union status | ||||||||||||
| New relationship | .49 | .16 | 1.63 ** | −.23 | .19 | .79 | ||||||
| Employment status (Not employed) | ||||||||||||
| In school | −.33 | .33 | .72 | −.50 | .34 | .61 | ||||||
| Part-time | −.41 | .23 | .67 | −.41 | .24 | .66 | ||||||
| Full-time | −.29 | .16 | .75 | −.29 | .17 | .75 | ||||||
| Fertility history | ||||||||||||
| Pregnant younger than 18 | .38 | .15 | 1.47 * | .26 | .16 | 1.30 | ||||||
| Ever unplanned pregnancy | −.24 | .14 | .78 | −.21 | .15 | .81 | ||||||
| Parity (No children) | ||||||||||||
| 1 child | −.51 | .28 | .60 | −.38 | .29 | .68 | ||||||
| 2 children | −1.37 | .25 | .25 *** | −1.20 | .27 | .30 *** | ||||||
| 3+ children | −1.50 | .26 | .22 *** | −1.27 | .29 | .28 *** | ||||||
| Partner vasectomy | .01 | .29 | 1.01 | −.20 | .30 | .82 | ||||||
| Values | ||||||||||||
| Religiosity | .06 | .03 | 1.06 * | .04 | .03 | 1.04 | ||||||
| Catholic | .22 | .16 | 1.25 | .22 | .17 | 1.24 | ||||||
| Importance of motherhood | .13 | .03 | 1.14 *** | .14 | .03 | 1.15 *** | ||||||
| Importance of successful career | .14 | .09 | 1.15 | .16 | .09 | 1.17 | ||||||
| Importance of leisure | −.17 | .08 | .84 * | −.20 | .08 | .82 * | ||||||
| Sterilization history | ||||||||||||
| Years since sterilization | .05 | .02 | 1.06 *** | |||||||||
| Under 30 when sterilized | .78 | .25 | 2.19 | |||||||||
| Tubal sterilization | −.52 | .18 | .60 ** | |||||||||
| Reason for sterilization (Voluntary) | ||||||||||||
| Situational | 1.15 | .30 | 3.15 *** | |||||||||
| Health problem | .51 | .18 | 1.66 * | |||||||||
| Suggested/pressured by others | 1.32 | .26 | 3.74 *** | |||||||||
| Other reason | .64 | .38 | 1.90 * | |||||||||
| Constant | −.67 | .08 | *** | −.27 | .35 | −.46 | .80 | .19 | .85 | |||
|
| ||||||||||||
| Psuedo R2 | .02 | .02 | .08 | .15 | ||||||||
| BIC | 1536 | 1548.9 | 1570 | 1512.9 | ||||||||
Note: Reference categories in parentheses.
p<.001;
p<.01;
p<.05.
Among the life course measures, being in a new relationship (since sterilization) is significant until sterilization is accounted for. Younger age (exp(B) =.95; p<.01) is associated with greater regret in the final model, and employment status is not associated with sterilization regret. In the full model, parity remains a significant predictor of lower regret; having two or more (exp(B) =.30; p<.001), or three or more (exp(B) =.28; p<.001) children are associated with lower odds of perceiving sterilization as blocking the realization of childbearing desires. Only two measures of values are associated with blocked desire for a child in the final model: importance of motherhood is associated with higher odds of viewing sterilization as a barrier to having desired children (exp(B)= 1.15; p<.001) and importance of leisure with lower odds (exp(B) =.82; p<.05).
Indicators specific to the sterilization surgery are also associated with the odds of women perceiving sterilization as a barrier to having desired children. Women whose sterilization occurred in the more distant past are significantly more likely (exp(B)=1.06; p<.001) to want a child after sterilization than women whose sterilization was more recent. Women who had a tubal ligation have lower odds (exp(B) =.60; p<.01) of an unrealized desire for a child than women who had other kinds of sterilizing surgeries. Compared to voluntary reasons, women who reported all other reasons are significantly more likely to report wanting a child after the surgery. The odds are highest for women who report that they had the sterilization because it was suggested by or they felt pressure from others (exp(B)= 3.74; p<.001), followed by situational reasons (exp(B) = 3.15; p<.001), other reasons (exp(B) = 1.90; p<.05), and health-related reasons (exp(B) = 1.66; p<.05). The associations for different reasons emerged even controlling for many potentially confounding variables (social class, fertility/life course and values indicators).
4. Discussion and Conclusion
Although not specially designed for our questions, the NSFB proved useful for an analysis of racial patterns in sterilization and sterilization regret. Patterns of associations from this large, nationally representative sample provide unique insights regarding race, social class status and sterilization in the United States. This sample provides information on groups less frequently included in studies of race and health (Asian and Native American women), and information on reasons for women’s sterilizations and whether their sterilizations prevent them from having children that they want to have. We find that race/ethnicity is indeed associated with sterilization rates and unrealized desires for children for Hispanic and Native American women.
Native American women have the highest odds of sterilization, and the association, unlike that for Black women, is not explained by socioeconomic status, life course, fertility history, or values indicators. Hispanic women are significantly less likely to be sterilized than White women after controlling for socioeconomic status, but among those who are sterilized, Hispanic and Native American women are significantly more likely to report that their sterilization surgery has prevented them from having children they want to have. Our results suggest that sterilization may be perceived as especially problematic for Hispanic and Native American women. For Black women, it may not be perceived as being as problematic, as they have lower odds of perceiving sterilization as a barrier to having desired children than White women. Though Asian women have the lowest sterilization rate overall, they are more likely to report pressure to be sterilized than women in any other racial/ethnic category. These results, therefore, do not support any one theory from Shapiro et al. (1983)’s framework as the explanation for racial differences in sterilization patterns, but instead highlight the importance of a variety of contextual influences, including race, social class, life course, fertility history, and attitudes/values. There appears to be some support for the fertility and altruism theories to explain Black/White sterilization differences; as suggested by the fertility thesis, though Black women are more likely to be sterilized, they also are more likely to have had unplanned pregnancies, pregnancies under 18, and more children. The altruistic thesis, that a higher proportion of women in some racial groups may have a greater preference for sterilization, may also be valid as Black women are not more likely to report that their sterilizations prevent them from having wanted children despite higher sterilization rates. Native American women, on the other hand, are more likely to be sterilized–and at younger ages—and to perceive the sterilization as preventing them from having wanted children. Social pressure is not a common reason for sterilization for women in any of the racial groups, but the reasons proffered by Hispanic and Native American women do tend to fall somewhat more toward the less voluntaristic end of the continuum of reasons. As socioeconomic status, life course factors, fertility history, values, and sterilization factors do not reduce the odds of perceiving sterilization as a barrier, our results are at least consistent with the racial theory for Hispanic and Native American women.
We hope that the overt coercive sterilization practices of the 1970s and earlier (e.g., Gutierrez 2008; Lawrence 2000; Roberts 1997; Schoen 2005; Solinger 2005) have ended, but our results suggest the possibility that the higher sterilization rates among some racially marginalized groups may reflect stratified reproduction rather than differential preferences regarding contraceptive options or different fertility patterns. Of greatest potential concern is differences by race in the percentage of women who were sterilized and then later want a child. That Hispanic and Native American women are more likely to want children after they are sterilized raises the possibility that their surgeries were premature. Our data cannot fully tease out, however, whether these racialized reproduction patterns reveal sterilizations that are unwanted but necessary to address health problems, whether they are due to limited options related to public funding for more permanent contraceptives, or whether they occur because of the intention of the health care provider is to stop reproduction. These are important distinctions that must be examined in future research because of the policy/program implications; the first possibilities suggest that more strategies are needed to improve the overall and reproductive health of some racially-marginalized women, including expanding contraceptive options that are publicly funded and awareness of the options (Borrero et al. 2011), whereas the latter possibility would justify calls for programs to ensure that women are not coerced into undergoing sterilization surgeries before they have completed their childbearing.
These patterns say little about the individual experiences of women but suggest the need to examine race-specific patterns rather than assuming that all non-White women are sterilized for the same reasons or face similar unrealized desires for childbearing. Despite having a large and representative sample of American women, there are still insufficient numbers of cases in our sample to assess important details about specific ethnic groups (e.g. Cuban, Mexican, Puerto Rican or South American women, women from specific Native American groups, etc.). From a cultural perspective, these differences are likely to matter a great deal, but from the perspective of differential treatment by health care professionals, these distinctions are less likely to be as meaningful.
Volscho (2010) has argued that racial differentials in sterilization and sterilization regret support the assertion that “reproductive racism” is still widespread in the United States. Although our research cannot fully uncover the motivations that lie behind racial differences in sterilization and sterilization regret, our findings are consistent with the argument that some non-White women still experience a lesser degree of reproductive control than non-Hispanic White women. We were surprised, however, to find that after controlling for fertility, life course, and attitudinal factors, Black women do not have significantly higher rates of sterilization or unrealized desires for children. Perhaps this finding is linked to recent efforts to ensure consistent treatment for all patients -- with a focus on Blacks -- in healthcare. For example, recent research indicates that Black women are more likely than White women or women of other races/ethnicities to have regular physicians and to view them as caring, though it is unclear whether physicians are actually more caring or if Black women have lower expectations regarding treatment by their health care providers (Shreffler et al. 2009). Because the control variables with the biggest effects involve childbearing (pregnant under 18, ever having an unplanned pregnancy, and parity), however, the lack of significant differences between White and Black women on the likelihood of sterilization and sterilization regret should not be perceived as an indication of similar childbearing patterns or similar levels of reproductive control.
We do not have concrete evidence that coercive practices are taking place among Native American or Hispanic women, but certainly higher rates of sterilization surgeries and regret are cause for concern. As noted above in the measurement description, to be categorized as receiving pressure from others to be sterilized required women to explicitly report pressure. Cultural differences in perceptions regarding health care recommendations may partially explain the dramatic differences in reasons given for sterilizations between Native American, Hispanic, and Asian women. Cultural differences in communication styles may be important as well; a qualitative study on recommendations for health care providers when working with Native American patients highlighted that providers need to be aware that Native Americans tend to ask few direct questions and have been taught to not question healers as a sign of respect (Garwick and Auger 2000). Our results suggest that it is important to go beyond Black/White comparisons to understand complex patterns of reproductive experiences of women in the United States. We argue that a “one-size-fits-all” approach to understanding racial differences in sterilization patterns is not appropriate.
We readily acknowledge, however, that our findings -- while consistent with the assertion that non-White women still experience subtle forms of reproductive coercion – cannot provide conclusive evidence. Such proof would require much more detail about sterilization decision-making processes and social contexts. Future qualitative inquiry examining the patterns in reasons for sterilization by race/ethnicity identified in this paper can help uncover the dynamics underlying these patterns. In addition, future research is needed to examine whether differential family structures by racial/ethnic group affect the degree and extent of familial or partner pressure. The role of public and familial support should be examined in further detail as well; women with few supports for raising children (e.g., no publicly funded child care, lack of health care, limited resources to purchase contraceptives, few policies to facilitate employment and child rearing, and/or lack of gender equity in child rearing) may choose sterilization over having children or using other forms of birth control, even if they want more children. Qualitative studies of health care providers who perform sterilization surgeries, or with women who are sterilized, could reveal if there are incentives to sterilize or if physician attitudes towards different groups of women contribute to disproportionate sterilization for some groups. Finally, because our samples of Asian and Native American women are small and heterogeneous (i.e., we are unable to discern cultural background or nativity), future research on sterilized women in these groups is prudent, particularly regarding reasons for sterilization surgeries and the meaning of health care recommendations. Better data is required to improve our limited understanding of fertility and sterilization processes of Asian and Native American women.
Despite the need for additional research, our study provides important initial information that race and social class are associated with rates of sterilization, reasons for undergoing sterilization surgeries, and unrealized childbearing desires following sterilization. Racialized reproductive patterns reveal important differences among women in terms of their reproductive pathways, options and consequences. Though our measures do not directly indicate the influence of racially-motivated coercion, bias, and pressure on these racialized patterns, the consequences—particularly for Hispanic and Native American women—are striking and suggest that continuing efforts in terms of both race and gender sensitive social policies and practices are needed to bring an end to racialized and stratified reproduction in the United States. These results provide critically important insights regarding the complexity of racialized fertility patterns and reproduction in the United States, and provide some support for the theory that implicit attitudes in reproductive health care persist for at least some racial/ethnic minority groups in the United States.
Highlights.
We examine sterilization patterns and regret by race among U.S. women.
Native American women have the highest odds of sterilization and of regret.
Sterilization regret is also higher for Hispanic women who are sterilized.
Reasons for sterilization surgery differ by race and impact odds of regret.
Footnotes
This research was supported in part by grant R01-HD044144 “Infertility: Pathways and Psychosocial Outcomes” funded by NICHD (Lynn White and David R. Johnson, Co-PIs).
Though we apply attitudes and values of religiosity and importance of motherhood as causally prior to sterilization, the process or outcome of sterilization could also shape attitudes and values, particularly the importance of motherhood, and should be examined in future studies with longitudinal data.
To determine whether racial coding rules had an effect on outcomes, we also ran all analyses with coding “Black” as first priority and “Hispanic” as second priority. Changing the racial/ethnic categories in this way had small effects on coefficients but did not change direction or level of significant findings.
To determine whether our ordering of reasons for sterilization had an effect on regret, we reverse-ordered our mutually exclusive categories and also ran analyses with our current hierarchy ordering where “suggested/pressured” was the reference category rather than “voluntary.” Changing the ordering did not change the direction of results, though it reduced the significance of the smaller categories. Analyses indicated that women with surgery for health or voluntary reasons were significantly less likely than women with surgery for suggested/pressured reasons to report regret.
In Table 1, the percentages of reasons for sterilization are slightly different from the percentages in Table 2 because they are restricted into only one category.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Karina M. Shreffler, Email: karina.shreffler@okstate.edu, Oklahoma State University, 700 N. Greenwood Ave. Tulsa, OK 74106, 918-594-8389
Julia McQuillan, Email: jmcquillan2@unlnotes.unl.edu, The University of Nebraska at Lincoln, 706 Oldfather Hall, Lincoln, NE 68588, 402-730-1935
Arthur L. Greil, Email: fgreil@alfred.edu, Alfred University, 1 Saxon Drive, Alfred, NY 14802, 607-871-2085
David R. Johnson, Email: drj10@psu.edu, The Pennsylvania State University, 211 Oswald Tower, University Park, PA 16802, 814-865-9564
References
- Allison Paul. Missing Data. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- Anderson John E, Warner Lee, Jamieson Denise J, Kissin Dmitry M, Nangia Ajay K, Macaluso M. Contraceptive Sterilization Use among Married Men in the United States: Results from the Male Sample of the National Survey of Family Growth. Contraception. 2010;82(3):230–5. doi: 10.1016/j.contraception.2010.03.018. [DOI] [PubMed] [Google Scholar]
- Badagliacco Joanna M. He’s Not Mr. Right, He’s More Like Mr. Now: Patrifocal and Matrifocal Discourses among Homeless Mothers in Kentucky. Journal of Sociology and Social Welfare. 1999;26(3):71–104. [Google Scholar]
- Badagliacco Joanna M, Ruiz Carey. Impoverished Appalachia and Kentucky Genomes: What is at Stake? How Do Feminists Reply? New Genetics & Society. 2006;25(2):209–26. [Google Scholar]
- Bass Loretta E, Nicole Warehime M. Do Health Insurance and Residence Pattern the Likelihood of Tubal Sterilization among American Women? Population Research and Policy Review. 2009;28(2):237–49. [Google Scholar]
- Bell Ann. It’s Way Out of My League: Low Income Women’s Experiences of Medicalized Infertility. Gender & Society. 2009;23(5):688–709. [Google Scholar]
- Bird Chloe E, Rieker Patricia P. Gender and Health: The Effects of Constrained Choice and Social Policies. Cambridge, UK: Cambridge University Press; 2008. [Google Scholar]
- Boring Catherine Chase, Bochat Robert W, Becerra Jose. Sterilization Regret among Puerto Rican Women. Fertility and Sterility. 1988;49(6):973–81. [PubMed] [Google Scholar]
- Borrero Sonya B, Abebe Kaleab, Dehlendorf Christine, Schwarz Eleanor B, Creinin Mitchell D, Nikolajski Cara, Ibrahim Said. Racial Variation in Tubal Sterilization Rates: Role of Patient-Level Factors. Fertility and Sterility. 2011;95(1):17–22. doi: 10.1016/j.fertnstert.2010.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrero Sonya B, Moore Charity G, Qin Li, Schwarz Eleanor B, Akers Aletha. Unintended Pregnancy Influences Racial Disparity in Tubal Sterilization Rates. Journal of General Internal Medicine. 2010;25(2):122–8. doi: 10.1007/s11606-009-1197-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrero Sonya B, Reeves Matthew F, Schwarz Eleanor B, Bost James E, Creinin Mitchell D, Ibrahim Said A. Race, Insurance Status, and Desire for Tubal Sterilization Reversal. Fertility and Sterility. 2008;90(2):272–7. doi: 10.1016/j.fertnstert.2007.06.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrero Sonya B, Schwarz Eleanor B, Creinin Mitchell D, Ibrahim Said A. The Impact of Race and Ethnicity on Receipt of Family Planning Services in the United States. Journal of Women’s Health. 2009a;18(1):91–6. doi: 10.1089/jwh.2008.0976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrero Sonya B, Schwarz Eleanor B, Reeves Matthew F, Bost James E, Creinin Mitchell D, Ibrahim Said A. Does Vasectomy Explain the Difference in Tubal Sterilization Rates Between Black and White Women? Fertility and Sterility. 2009b;91(5):1642–5. doi: 10.1016/j.fertnstert.2008.01.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bumpass Larry L. The Risk of an Unwanted Birth: The Changing Context of Contraceptive Sterilization in the U.S. Population Studies. 1987;41(3):347–63. [Google Scholar]
- Bumpass Larry L, Thomson Elizabeth, Godecker Amy L. Women, Men, and Contraceptive Sterilization. Fertility and Sterility. 2000;73(5):937–46. doi: 10.1016/s0015-0282(00)00484-2. [DOI] [PubMed] [Google Scholar]
- Chandra Anjani, Martinez Gladys M, Mosher William D, Abma Joyce C, Joyce C, Jones Jo. Fertility, Family Planning, and Reproductive Health of U.S. Women: Data from the 2002 National Survey of Family Growth. Vital Health Statistics. 2005;23:1–160. [PubMed] [Google Scholar]
- Chavez Leo R. A Glass Half Empty: Latina Reproduction and Public Discourse. Human Organization. 2004;63(2):173–88. [Google Scholar]
- Colen Shellee. Housekeeping for the Green Card: West Indian Household Workers, the State, and Stratified Reproduction in New York. In: Sanjek Roger, Colen Shellee., editors. At Work in Homes: Household Workers in World Perspective. Washington, DC: American Anthropological Association; 1990. pp. 89–118. [Google Scholar]
- Collins Patricia Hill. Black Feminist Thought. 2. Boston: Unwin Hyman; 2000. [Google Scholar]
- Cozzarelli Catherine, Wilkinson Anna V, Tagler Michael J. Attitudes Toward the Poor and Attributions for Poverty. Journal of Social Issues. 2001;57:207–27. [Google Scholar]
- Curtis Kathryn M, Mohllajee Anshu P, Peterson Herbert B. Regret Following Female Sterilization at a Young Age: A Systematic Review. Contraception. 2006;73(2):205–10. doi: 10.1016/j.contraception.2005.08.006. [DOI] [PubMed] [Google Scholar]
- Downing Roberta A, LaVeist Thomas A, Bullock Heather E. Intersections of Ethnicity and Social Class in Provider Advice Regarding Reproductive Health. American Journal of Public Health. 2007;97(10):1803–1807. doi: 10.2105/AJPH.2006.092585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebrahim Shahul H, Anderson John E, Correa-d-Araujo Rosaly, Posner Samuel F, Atrash Hani K. Overcoming Social and Health Inequalities among U.S. Women of Reproductive Age—Challenges to the Nation’s Health in the 21st Century. Health Policy. 2009;90(2–3):196–205. doi: 10.1016/j.healthpol.2008.09.011. [DOI] [PubMed] [Google Scholar]
- Elson Jean. Am I still a woman? Hysterectomy and Gender Identity. Philadelphia: Temple University Press; 2008. [Google Scholar]
- Finer Lawrence B, Frohwirth Lori F, Douphinee Lindsay A, Singh Susheela, Moore Ann M. Reasons U.S. Women Have Abortions: Quantitative and Qualitative Perspectives. Perspectives on Sexual and Reproductive Health. 2005;37(3):110–118. doi: 10.1363/psrh.37.110.05. [DOI] [PubMed] [Google Scholar]
- Garwick Ann, Auger Sally. What do Providers Need to Know about American Indian Culture? Recommendations from Urban Indian Family Caregivers. Families, Systems, & Health. 2000;18(2):177–89. [Google Scholar]
- Ginsburg Faye D, Rapp Rayna. The Politics of Reproduction. Annual Review of Anthropology. 1991;20:311–43. doi: 10.1146/annurev.an.20.100191.001523. [DOI] [PubMed] [Google Scholar]
- Groves Robert M, Mosher William D, Lepkowski J, Kirgis NG. Planning and Development of the Continuous National Survey of Family Growth. National Center for Health Statistics. Vital Health Statistics. 2009;1(48) [PubMed] [Google Scholar]
- Gutierrez Elena. Fertile Matters: The Racial Politics of Mexican-Origin Women’s Reproduction. Austin: University of Texas Press; 2008. [Google Scholar]
- Hartouni Valerie. Breached Birth: Reflections of Race, Gender, and Reproductive Discourse in the 1980s. Configuration. 1994;2(1):73–88. [Google Scholar]
- Health and Human Services. Annual Update of the HHS Poverty Guidelines. Federal Register. 2013;78(16):5182–3. [Google Scholar]
- Henshaw Stanley K, Singh Susheela. Sterilization Regret among U.S. Couples. Family Planning Perspectives. 1986;18(5):238–40. [PubMed] [Google Scholar]
- Kariminia Azar, Saunders Douglas M, Chamberlain Marie. Risk Factors for Strong Regret and Subsequent IVF Request after Having Tubal Ligation. Australia and New Zealand Journal of Obstetrics and Gynaecology. 2002;42(5):526–9. doi: 10.1111/j.0004-8666.2002.00526.x. [DOI] [PubMed] [Google Scholar]
- King Deborah. Multiple Jeopardy, Multiple Consciousness: The Context of a Black Feminist Ideology. Signs. 1988;19(1):42–72. [Google Scholar]
- King Leslie, Meyer Madonna Harrington. The Politics of Reproductive Benefits: U.S. Insurance Coverage of Contraceptive and Infertility Treatments. Gender & Society. 1997;11(1):8–30. doi: 10.1177/089124397011001002. [DOI] [PubMed] [Google Scholar]
- Lawrence Jane. The Indian Health Service and the Sterilization of Native American Women. American Indian Quarterly. 2000;24(3):400–19. doi: 10.1353/aiq.2000.0008. [DOI] [PubMed] [Google Scholar]
- Leppert Phyllis C, Legro Richard S, Kjerulff Kristen H. Hysterectomy and Loss of Fertility: Implications for Women’s Mental Health. Journal of Psychosomatic Research. 2007;63(3):269–274. doi: 10.1016/j.jpsychores.2007.03.018. [DOI] [PubMed] [Google Scholar]
- Lichter Daniel T, Crowley Martha L. Population Bulletin. 2. Vol. 57. Washington, DC: Population Reference Bureau; 2002. Poverty in America: Beyond Welfare Reform. [Google Scholar]
- Lopez Iris. Matters of Choice: Puerto Rican Women’s Struggle for Reproductive Freedom. New Brunswick, NJ: Rutgers University Press; 2008. [Google Scholar]
- Marcil-Gratton Nicole. Sterilization Regret among Women in Metropolitan Montreal. Family Planning Perspectives. 1988;20(5):223–7. [PubMed] [Google Scholar]
- McCarty Christopher, House Mark, Harman Jeffery, Richards Scott. Effort in Phone Survey Response Rates: The Effects of Vendor and Client-Controlled Factors. Field Methods. 2006;18(2):172–88. [Google Scholar]
- Miller Warren B, Shain Rochelle N, Pasta David J. The Sterilization Decision in a U.S. Sample. In: Bulatao Rudolfo A, Palmore James A, Ward Sandra E., editors. Choosing a Contraceptive: Method Choice in Asia and the United States. Boulder, CO: Westview; 1989. pp. 257–73. [Google Scholar]
- Miller Warren B, Shain Rochelle N, Pasta David J. The Prediction of Post-Sterilization Regret in Married Women. Journal of Applied Social Psychological. 1991;21(13):1083–110. [Google Scholar]
- Miller Warren B, Shain Rochelle N, Pasta David J. A Model of Pre-Sterilization Ambivalence and Post-Sterilization Regret in Married Couples. Advances in Population: Psychosocial Perspectives. 1993;1:173–206. [PubMed] [Google Scholar]
- Mosher William D, Martinez Gladys M, Anjani Chandra, Abma Joyce C, Wilson Stephanie J. Use of Contraception and Use of Family Planning Services in the United States:1982–2002. Advance Data From Vital and Health Statistics. 2004:350. [PubMed] [Google Scholar]
- Roberts Dorothy. Killing the Black Body: Race, Reproduction, and the Meaning of Liberty. New York: Pantheon; 1997. [Google Scholar]
- Schmidt Johannes, Hillis Susan D, Marchbanks Polly A, Jeng Gary, Peterson Herbert P. Requesting Information about and Obtaining Reversal after Tubal Sterilization: Findings from the U.S. Collaborative Review of Sterilization. Fertility and Sterility. 1999;74(5):892–8. doi: 10.1016/s0015-0282(00)01558-2. [DOI] [PubMed] [Google Scholar]
- Schoen Johanna. Choice & Coercion: Birth Control, Sterilization, and Abortion in Public Health and Welfare. Chapel Hill: University of North Carolina Press; 2005. [Google Scholar]
- Shapiro Thomas M, Fisher William, Diana Augusto. Family Planning and Female Sterilization in the United States. Social Science and Medicine. 1983;17(23):1847–55. doi: 10.1016/0277-9536(83)90161-2. [DOI] [PubMed] [Google Scholar]
- Shreffler Karina M, McQuillan Julia, Greil Arthur L, Lacy Naomi L, Ngaruiya Christina. Odds of Having a Regular Physician and Perceptions of Caring: Ethnic Patterns among Women Aged 25 to 45. Family Medicine. 2009;41(4):248–53. [PubMed] [Google Scholar]
- Smedley Brian D, Stith Adrienne Y, Nelson Alan R. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: The National Academies Press; 2002. [PubMed] [Google Scholar]
- Solinger Rickie. Pregnancy and Power: A Short History of Reproductive Politics in America. New York: New York University Press; 2005. [Google Scholar]
- Stern Alexandra Minna. Sterilized in the Name of Public Health: Race, Immigration, and Reproductive Control in Modern California. American Journal of Public Health. 2005;95(9):1128–38. doi: 10.2105/AJPH.2004.041608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szkupinski-Quiroga Seline. Blood is Thicker than Water: Policing Donor Insemination and the Reproduction of Whiteness. Hypatia. 2007;22(2):143–61. [Google Scholar]
- Thomas Susan L. Race, Gender, and Welfare Reform: The Antinatalist Response. Journal of Black Studies. 1998;28(4):419–46. [Google Scholar]
- Torpy Sally J. Native American Women and Coerced Sterilization: On the Trail of Tears in the 1970’s. American Indian Culture and Research Journal. 2000;24(2):1–22. [Google Scholar]
- Volscho Thomas W. Sterilization Racism and Pan-Ethnic Disparities of the Last Decade: the Continued Encroachment on Reproductive Rights. Wicazo Sa Review: A Journal of Native American Studies. 2010;25(1):17–31. [Google Scholar]
- Wallace Geoffrey L. The Effects of Family Caps on the Subsequent Fertility Decisions of Never-Married Mothers. Journal of Population Research. 2009;26:73–101. [Google Scholar]
- Winship Christopher, Radbill Larry. Sampling Weights and Regression Analysis. Sociological Methods and Research. 1994;23(2):230–57. [Google Scholar]
- Young Tycie. Quinacrine: Sterilizing the Poor. Off Our Backs. 1999;29(Oct):5–6. [Google Scholar]