Abstract
Data are limited concerning the dietary factors that influence appetite control in older adults. This study examined the effects of food form (FF) and portion size (PS) on appetite in 43 older adults (age: 72±1 y; BMI: 25.6±0.3 kg/m2). Subjects were assigned to groups based on PS of the test-meal (12.5% (n=18) vs. 25% (n=25) of estimated energy need). Subjects randomly consumed, on 2 separate days, the respective solid (S) or beverage (B) test-meal. Appetite sensations and hormonal responses were measured over 4 h. Main effects of FF (p<0.05) and/or PS (p<0.05) were observed for each appetite sensation. Postprandial hunger and desire to eat were greater following B vs. S and between 12.5% vs. 25%, whereas fullness was lower after B vs. S (p<0.05). Main effects of FF and/or PS were observed for glucose, insulin, and ghrelin. Postprandial glucose and insulin concentrations were lower after B vs. S and between 12.5% vs. 25% (all comparisons, p<0.05) while B led to greater 4-h ghrelin vs. S (p=0.09). No main effects were observed for GLP-1 or CCK. When adjusting for age, FF remained significant for postprandial hunger and fullness; PS remained significant for postprandial glucose. Greater hunger and reduced satiety with accompanying glucose, insulin, and ghrelin following the beverage vs. solid meals, and to some extent, in smaller vs. larger portions suggest that appetite control is influenced by food form and portion size in older adults. These findings may enhance the development of appropriate dietary strategies to help regulate energy balance.
Keywords: food rheology, portion sizes, elderly, appetite, beverages, ghrelin
Introduction
More than 36 million Americans are currently over the age of 65 years and this segment of the population is growing (1). Aging is accompanied by disruptions in the appetitive, metabolic, and hormonal processes that regulate energy balance (2). While these alterations are more pronounced in obese and underweight older adults, healthy, normal weight individuals may also experience similar alterations (2). Thus, it is imperative to identify the effects of specific dietary factors on the homeostatic mechanisms that regulate appetite and food intake in older adults.
Food form significantly impacts appetite and food intake in young and middle-aged adults. Beverage consumption leads to reduced appetite sensations, hormonal responses, and dietary compensation compared to solid foods (3-7). Limited data exist concerning the appetitive sensations and hormonal responses to food form in older individuals. We previously examined whether iso-energetic beverage versus solid meal-replacement products differentially affected appetite in older adults (8). Increased hunger and desire to eat along with reduced fullness were observed following the consumption of the beverage meal-replacement versus the solid version. Postprandial elevations in total plasma ghrelin concentrations, a reported orexigenic hormone (9, 10), were also observed following the beverage vs. solid meal-replacement. These data suggest differential appetitive and endocrine responses to food form in older adults. While the meal-replacements in our previous study were iso-energetic, the beverage contained a significantly larger amount of dietary carbohydrates, protein, and fiber along with a smaller amount of dietary fat potentially influencing our findings. The primary aim of the current study was to more closely examine the appetitive sensations and hormonal responses following consumption of beverages and solid foods matched for energy content, fiber content, and macronutrient composition.
Another dietary factor that significantly influences appetite and food intake is portion size. Young and middle-aged adults consume more energy when provided with a larger portion meal and may exhibit incomplete compensation over the remaining day compared to smaller portions (11-13). Often there is little difference in appetitive sensations between these meals (11-13). Whether this phenomenon also occurs in healthy older adults is generally unknown. Our secondary aim was to further examine the influence of portion size on the appetitive sensations and hormonal responses in healthy, non-obese, older adults.
Methods and Procedures
Subjects
Subjects were recruited through newspaper advertisements. Eligibility was based on the following criteria: 1) men and women ≥ 65 y; 2) body mass index (BMI) between 20 and 29 kg/m2; 3) not dieting and no weight loss or gain (>2 kg) within the past six months; 4) non-smoking; 5) non-diabetic; 6) clinically normal blood profiles (normal liver and kidney function; normal complete blood count; fasting blood glucose <110 mg/dL); and 7) maintained a free-living, sedentary lifestyle. There were 224 men who were initially interested in the study. Twenty-seven men met all study procedures and began the study, whereas only 13 subjects completed all study procedures. The subject characteristics are presented in Table 1. Each subject was informed of the purpose, procedures, and potential risks of participation in the study before signing an informed consent form approved by the Purdue University Biomedical Institutional Review Board.
Table 1.
Subject characteristics1
| 12.5% Portion Size (n=18) | 25% Portion Size (n=25) | |
|---|---|---|
| Sex | ||
| Male (n) | 9 | 11 |
| Female (n) | 9 | 14 |
| Age (y)* | 75 (66-84) | 70 (64-84) |
| Height (cm) | 171 (155-188) | 170 (157-188) |
| Weight (kg) | 75.4 (57.0-96.5) | 74.0 (51.5-93.9) |
| BMI (kg/m2) | 25.8 (22.7-29.7) | 25.5 (20.8-29.9) |
| Fasting glucose (mg/dL) | 95 (84-106) | 94 (80-106) |
Data expressed as mean and range
One-way ANOVA: (p<0.05)
12.5% Portion Size Group vs. 25% Portion Size Group
Experimental Design
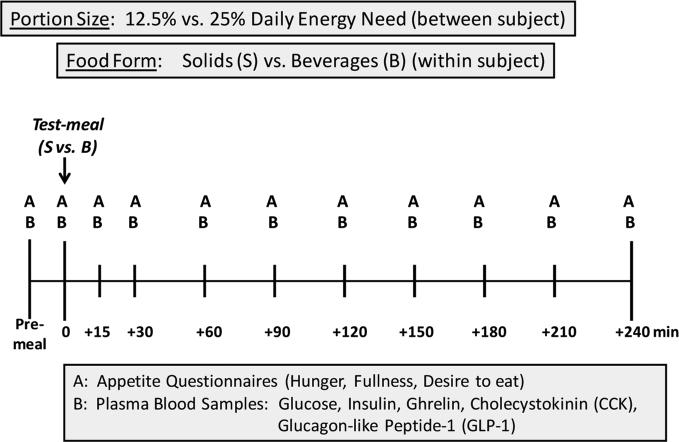
This is a semi-randomized, partial cross-over design study incorporating food form (within subject) and portion size (between subject) comparisons. In the spring of 2006, 25 men and women completed 2 testing days separated by at least 48 h. Subjects arrived at the laboratory following an overnight fast, voided, and were placed in a supine position. A catheter was placed in an antecubetal vein of the non-dominant arm and kept patent for the remainder of the testing period by saline drip. A baseline (fasting) blood sample was taken and an appetite questionnaire was completed. At time 0 (approximately 0800 h), the subjects randomly consumed a test meal containing 25% of estimated daily energy need in solid or beverage form along with 88.7 mL of water. They had 15 minutes to consume the test meal. Blood sampling and completion of appetite questionnaires were repeated over the next 4 hours. See Figure 1 for more detail. In the fall of 2006, 18 different men and women completed the same 2 testing days except that the test meal contained 12.5% of estimated daily energy need. Re-stated, while all subjects consumed the solid and beverage test meals, 25 subjects consumed these in 25% portion sizes while 18 other subjects consumed these in 12.5% portions. Subject characteristics are described according to the experimental groups (Table 1).
Figure 1.
Experimental Design
Test-meals
The test meals were in the form of a “meal-replacement shake” (beverage) or a “meal-replacement nutrition bar” (solid) specifically developed for this study by The Solae Company® (St. Louis, MO). By design, there were no differences in the energy content and macronutrient compositions between the beverage and solid forms of each of the respective portion sizes. Further, there was no dietary fiber in either the beverage or solid. The characteristics of the test meals are shown in Table 2. Daily energy need, required to determine the amount of food to provide to the subjects, was estimated from the sex-specific Harris Benedict equation*1.5 activity factor (14).
Table 2.
Test meal characteristics based on the portion size groups1 (12.5% vs. 25%)
| 12.5% Portion Size | 25% Portion Size | |||
|---|---|---|---|---|
| Solid | Beverage | Solid | Beverage | |
| Energy Content (kcal/test-meal) | 264 ± 8 | 264 ± 8 | 533 ± 14 | 533 ± 14 |
| Total mass (g/test-meal) | 130 ± 4 | 626 ± 17 | 260 ± 8 | 1252 ± 34 |
| Macronutrient Composition1 | ||||
| CHO (g/test-meal) | 36 ± 1 | 36 ± 1 | 73 ± 2 | 73 ± 2 |
| Sugar (g/test-meal) | 20 ± 1 | 24 ± 1 | 40 ± 1 | 48 ± 1 |
| Fiber (g/test-meal) | 0 | 0 | 0 | 0 |
| PRO (g/test-meal) | 13 ± 1 | 13 ± 1 | 27 ± 1 | 27 ± 1 |
| Fat (g/test-meal) | 8 ± 1 | 8 ± 1 | 16 ± 1 | 16 ± 1 |
| Palatability2 (au) | 7 ± 1 | 7 ± 1 | 7 ± 1 | 6 ± 1 |
| Viscosity-Beverage3 (cP) | NA | 21.5 | NA | 21.5 |
| Hardness-Solid4 (g) | 1013 | NA | 1013 | NA |
Data expressed as mean ± SEM
Palatability expressed as arbitrary units (scale 1-9)
Measured with a Brookfield Rheometer (RVDV) (Brookfield, Corp.; Middleboro, Massachusetts)
Measured with a Texture Analyzer (TA-TX2) (Texture Technologies Corp; Scarsdale, NY)
Prior to the first testing day, each subject completed a “taste-test” of the study treatments, rating the palatability of the solid and beverage using a scale from 1-9 (1, extremely unpleasant; 9, extremely pleasant). The palatability of each test meal is shown in Table 2.
Appetite Sensations
Appetite questionnaires, assessing appetitive sensations (i.e., hunger, fullness, desire to eat) were completed at various time points throughout the testing period (Figure 1). A 13-point numerical rating scale with the left anchor ‘1’ of “not at all” and the right anchor ‘13’ of “extremely” was used to assess each sensation (5). Participants were instructed to circle the vertical dash along the horizontal line corresponding to their feelings at that moment. The results are reported using arbitrary units (au).
Blood Sampling and Hormonal Indices
Eleven blood samples were taken during each testing period (Figure 1). The samples were collected into tubes containing ethylenediaminetetraacetic acid (EDTA) and centrifuged at 3000 RPM and −4°C for 15 minutes. The plasma was then separated and stored in microcentrifuge tubes at −80°C for future analysis. Plasma glucose concentration was measured by enzymatic colorimetry using an oxidase method on a COBAS Integra 400 analyzer (Roche Diagnostic Systems, Indianapolis, IN, USA). Plasma insulin concentration was measured by an electrochemiluminescence immunoassay method on the Elecsys 2010 analyzer (Roche Diagnostic Systems, Indianapolis, IN, USA). Plasma total ghrelin, cholecystokinin (CCK), and glucagon-like peptide-1 (GLP-1) were analyzed through enzyme immunoassay (EIA) techniques utilizing EIA kits and the standard manufacturers’ protocol (Phoenix Pharmaceuticals, Belmont, CA, USA). All samples from a given subject were tested in duplicate and analyzed within the same assay.
Data and Statistical Analyses
All data were examined as percent change from baseline (fasting) and analyzed according to the area under the curve (AUC) throughout the 4-h postprandial period. AUC measurements were calculated using the trapezoidal rule (15). A two-way mixed factorial ANCOVA was performed on the appetite sensations and hormonal responses to examine the between subject (independent) effects of portion size (12.5 vs. 25%) and the within-subject (repeated measures) effects of food form (solid vs. beverage test meals) when adjusting for age (i.e., age defined as a categorical variable consisting of 4 categories of 5-y intervals). The sample size of 43 subjects (25 in the 25% portion size and 18 in the 12.5% portion) provided >80% power to detect differences in appetite sensations between portion sizes and between the solid and beverage test foods using the statistical approach mentioned. Pearson's correlation analyses were performed to identify the relationship between the appetite sensations and hormonal responses. All measurements are expressed as mean ± SEM. An alpha level of p<0.05, two-tailed, was considered statistically significant. Statistical analyses were performed using the SPSS (Statistical Package for the Social Sciences; version 15.0; SPSS Inc.; Chicago, IL).
Results
Appetite sensations
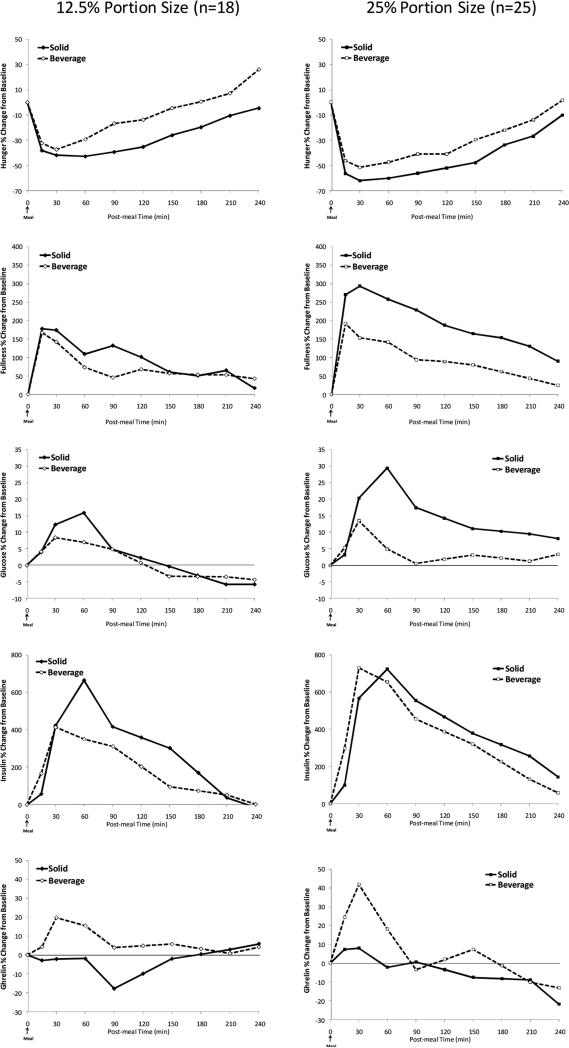
Regardless of food form or portion size, within 15 minutes of meal consumption, hunger and desire to eat declined while fullness increased (See Figure 2). This was followed by a gradual rise in hunger and desire to eat and a decline in fullness throughout the remaining testing period.
Figure 2.
Time course of the appetite sensations and hormonal responses over the 4-h period following the solid vs. beverage test-meals between subjects consuming portion sizes of 12.5% vs. 25% in solid vs. beverage forms.
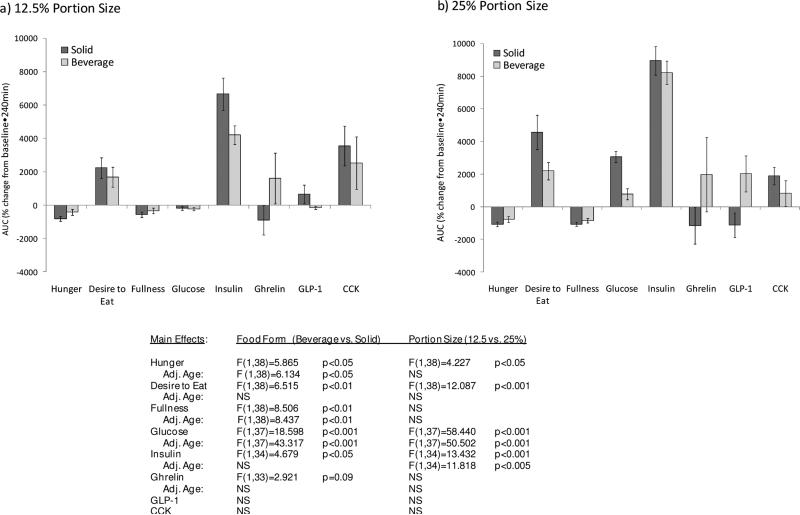
Main effects of food form and portion size were observed for hunger sensations (Figure 3). Postprandial hunger was higher after the first hour (1-h AUC data not shown) and remained higher over the entire 4-h period following the beverage compared to solid (4-h AUC, p<0.05) and 12.5% versus 25% portion size (4-h AUC, p<0.05) (Figure 3). Similar findings were observed for desire to eat. The main effect of food form, not portion size was observed for fullness (satiety). Specifically, fullness was lower after the first hour (1-h AUC data not shown) and remained lower over the entire 4-h period for the beverage versus solid food forms (4-h AUC, p<0.01) (Figure 3). When adjusting for age, the main effects of food form on 4-h hunger and fullness remained but disappeared for desire to eat while the main effects of portion size no longer existed for any of these variables (Figure 3).
Figure 3.
Area Under the Curve (AUC) for the appetite sensations and hormonal responses over the 4-h period following the solid vs. beverage test-meals between subjects consuming portion sizes of 12.5% vs. 25% in solid (S) vs. beverage (B) form. Negative results (i.e., values below zero) indicate a reduction from the fasting (pre-meal) state.
Hormonal Responses
The glucose and hormonal responses across the 4-h test period are shown in Figure 2. Meal-related responses were observed within 15 minutes of meal-initiation for all indices. Food form and portion size led to significant reductions in glucose and insulin responses after the first hour (1-h AUC data not shown; p<0.05) and throughout the 4-h period when comparing the beverage vs. solid meals and 12.5% vs. 25% portion sizes (4-h AUC, p<0.05) (Figure 3). When adjusting for age, the main effects of food form and portion size for the 4-h glucose responses remained whereas insulin was only found to differ between portion size groups (Figure 3). The initial ghrelin response (i.e., ghrelin at 60 min) was higher following the beverage (1275 ± 539 %•60 min) vs. the solid meal (44 ± 194 %•60 min; p<0.05) and tended to remain higher over the 4-h period (B: 1803 ± 1395 %•240 min vs. S: -1048 ± 737 %•240 min, p=0.09). No difference in ghrelin was observed when comparing portion size. The main effects of food form no longer remained after adjusting for age (Figure 3). Concerning the GLP-1 and CCK responses, no differences were observed between food form or portion size over the 4-h period with and without adjusting for age (Figure 3).
Relationship between the Appetite Sensations and Hormonal Responses
Postprandial hunger was found to be positively associated with postprandial desire to eat (r=0.870; p<0.001) and ghrelin (r=0.263; p<0.05) and negatively associated with postprandial fullness (r=−0.585; p<0.001) and insulin (r=−0.277; p<0.01). Fullness was positively associate with postprandial insulin (r=0.301; p<0.01) and negatively associated with postprandial desire to eat (r=−0.495; p<0.001) and CCK (r=−0.266; p<0.05).
Discussion
The current study sought to identify whether the homeostatic mechanisms involved with appetite control are operational in healthy, non-obese, older adults as indexed by sensitivity to manipulations of food form and portion size. Greater hunger and/or reduced satiety with accompanying glucose, insulin, and ghrelin responses were observed following the beverage vs. solid test meals in smaller vs. larger portions. Additionally, perceived appetite was found to be associated with two key appetite-regulating hormones (i.e., insulin and ghrelin). These findings suggest that the homeostatic mechanisms surrounding appetite control appear to be largely operational in older, healthy adults. Our data also suggest that older adults appear to have reduced sensitivity to beverages when consumed in smaller portions.
Obesity and under-nutrition, stemming from the anorexia of aging, are two opposing phenomena that afflict the older adult population. While opposite, in nature, both are characterized by alterations in the metabolic and hormonal processes that control appetite and food intake and lead to a dysregulation of energy balance. These imbalances can increase the risk of disease, infection, and other health complications that reduce quality of life (16). Healthy, non-obese, older adults exhibit similar alterations in energy balance, but to a lesser extent, as obese and/or under-nourished older adults. Specifically, non-obese, older adults experience reduced pre-meal hunger (17-19) and elevated postprandial fullness (satiety) sensations (19) along with reduced fasting and postprandial glucose, insulin, and ghrelin concentrations which may lead to impaired appetite and diminished food intake (20-22). While these alterations exist, the data from our current study suggest that, regardless of the impairment, appetite can be influenced by both food form and portion size in healthy, non-obese, older adults.
Numerous (3-6, 8, 23, 24), albeit not all (24) studies in younger adults report reduced postprandial satiety, glucose, and insulin responses following beverage vs. solid meals. In our previous study involving older adults (age 61 ± 3 y), postprandial hunger and desire to eat sensations were elevated following the beverage vs. solid meals; these responses were accompanied by elevated insulin and ghrelin concentrations with no change in CCK concentrations (8). Unlike the test meals used in our previous study, the beverage and solid test meals in our current study were closely matched for energy content, fiber content, and macronutrient composition which allowed for a more accurate examination surrounding the effects of food form on appetite. Our current study led to similar findings in that greater postprandial hunger and desire to eat sensations along with reduced satiety were observed following the beverage vs. solid meals. The beverage meal also led to elevated postprandial insulin and ghrelin concentrations with no change in CCK and GLP concentrations compared to the solid meal. Taken together these data suggest that beverage consumption leads to reduced satiety and greater hunger sensations potentially due to the inability of beverages to suppress ghrelin and insulin secretion. Thus, in older adults, the differential appetitive sensations observed in response to food form appear to involve other mechanisms not including the peripheral hormones GLP-1 and CCK.
Several studies have been performed to evaluate the long-term effects of consuming a beverage supplement on body weight in under-nourished older individuals. Following the 4-6 month interventions, the daily consumption of a beverage supplement led to greater weight gain compared to individuals not consuming the supplement (25, 26). Our study was an acute, mechanistic study and not designed to examine whether beverages lead to weight gain in undernourished adults. However, the differential responses observed following the solid vs. beverage meals suggests that food form may be a key component when developing beneficial strategies to establish energy balance in older adults.
Moderating portion size has been shown to significantly influence perceived appetite and glucose and insulin concentrations in older adults (20, 27, 28). In a study involving healthy, normal weight older women (72 ± 2 y), circulating glucose and insulin were assessed over a 5-h period after the consumption of the following test meals: 0 (fasting), 250 kcal (snack-size meal), 500 kcal (small meal), 1000 kcal (large meal). Compared to fasting and the snack-size meal, the subjects showed exaggerated responses and a delayed return to pre-meal glucose and insulin concentrations following the larger meals (20). Two additional studies examined the impact of reducing portion size on appetite in older adults (27, 28). Both hypothesized that the large quantities of food commonly provided to older individuals may actually lead to a reduction in appetite; thus, reducing portion size would potentially improve these feelings and lead to an increase in food consumption. (27, 28). In one study, reducing the size of the meal led to reductions in food consumption with no improvements in appetite sensations suggesting that simply reducing meal size may not be beneficial (27). However, in a more recent study, meal size was reduced along with increased energy density. Using this design, the smaller, energy-dense meal provided 14% more energy than the larger meal. The smaller, energy dense meal led to a 25% increase in food consumption compared to the larger meal suggesting that altering portion sizes along with other food properties may be a potential strategy to reestablish energy balance in older adults. The previously mentioned studies included older men and women who were either hospitalized or living in a long-term care community. Our current study included self-care, home-dwelling, healthy, non-obese older individuals. While postprandial hunger and desire to eat sensations along with postprandial glucose and insulin concentrations were reduced following the smaller vs. larger portions, many of these differences no longer existed after adjusting for age. Due to the experimental design, it is difficult to determine whether the subjects in their late sixties and early seventies had a differential response to the 12.5% vs. 25% portion size compared to those in their late seventies and early eighties. However, because age was a significant covariate and was associated with many of the appetite sensations and hormonal responses, the data would suggest that age significantly impacts the ability to differentiate between smaller vs. larger portion meals.
Limitations
Several study limitations have been identified. First, this was a semi-randomized, partial cross-over experimental design approach. While all subjects consumed the solid and beverage test meals, different subjects consumed these in the 12.5% vs. 25% portion sizes. Additionally, the 12.5% portion size group was significantly older than the 25% portion size group. Thus caution is warranted when interpreting the food form results between portion sizes as unintentional differences in the appetite sensations and hormonal responses may have existed between the subject groups. By incorporating a two-way mixed factor ANOVA, we were able to accurately examine the within and between-subject comparisons of food form and portion size, respectively. To truly identify the influence of age on the portion size effects, a complete crossover is warranted.
We also chose to include individuals who were non-obese which encompassed both normal weight and overweight individuals (BMI: 20 and 29 kg/m2). Even though the range is somewhat large, the individuals within this range typically experience normal and/or functioning appetite control and hormonal responses to test foods. According to Mourao et al. (4), BMI has not been shown to influence appetitive responses. When examining the possible relationship between our outcome measures (appetite sensations and hormonal responses) and BMI, no associations were observed. Taken together, we are confident that the incorporation of normal to overweight (i.e., non-obese) men and women led to meaningful findings.
While the incorporation of the smaller and larger portion bars and beverages in an acute-testing, controlled setting allowed examination of the influence of food form and portion size on appetite, the extrapolation of the findings to whole foods and meals in a free-living environment is uncertain (29). Because only healthy older men and women participated in this study, future work is needed to identify whether similar responses occur in obese and lean older individuals. Additionally, while data in younger lean and obese subjects indicate a significant influence of food form on the satiating properties of dietary protein, carbohydrates, and fat (4), future studies are also needed to determine whether differential responses to various macronutrients occur in older adults.
This study provides a first, but vital step, in identifying whether manipulations in food form and portion size result in beneficial changes in perceived appetite and hormonal responses in healthy, non-obese, older adults. However, to more comprehensively examine the underlying mechanisms involved with food form and portion size, future research including the measurements of gastric emptying and motility is warranted.
Conclusions
The results from our current study indicate that older adults experience greater hunger and desire to eat sensations along with reduced feelings of fullness (satiety) when consuming beverages vs. solid foods. The elevated ghrelin and reduced insulin responses following the beverage test meal coincide with these sensations. Thus, older individuals appear to have reduced sensitivity to beverage versus solid food form properties. Additionally, appetite varied with portion size as indicated by the greater hunger and desire to eat sensations experienced following the smaller vs. larger portions but was influenced by age. Taken together, these data suggest that incorporating solid meals may be beneficial when developing weight-loss strategies in overweight/obese individuals while beverages could promote essential weight gain in under-nourished older men and women.
Acknowledgments
The authors would like to thank the study participants for their dedication and compliance during the testing days; Kristin Duke-Simpson for her efforts in performing the day-to-day activities for this study; Arthur Rosen, MD, who provided medical coverage; and Doug Maish, EMT-P, who performed all catheter insertions and provided clinical laboratory services. Wayne W. Campbell and Richard D. Mattes originated the study, secured the funding, and provided overall supervision of the research. Heather J. Leidy and John Apolzan were involved with the development of the study purpose and design, and performed the clinical testing and data analysis. Dr. Leidy drafted the manuscript and all co-authors contributed to data interpretation and finalization of the manuscript. This study was funded through the NIH R01 AG021911 (awarded to WWC). The Solae Company® manufactured and provided the solid and beverage products tested. Support for Heather Leidy was provided, in part, by an Ingestive Behavior Research Center post-doctoral fellowship from Purdue University.
Footnotes
This study has been registered under ClinicalTrials.Gov:
Study #: NCT00798408; Title: The Body's Response to Food Intake in Older Adults.
Disclosure Statement None of the authors had any personal or financial conflicts of interest.
References
- 1.Facts for Features. Office CBsPI; 2006. www.census.gov/Press-Release. [Google Scholar]
- 2.Roberts SB, Rosenberg I. Nutrition and aging: changes in the regulation of energy metabolism with aging. Physiol Rev. 2006;86:651–67. doi: 10.1152/physrev.00019.2005. [DOI] [PubMed] [Google Scholar]
- 3.Mattes RD, Rothacker D. Beverage viscosity is inversely related to postprandial hunger in humans. Physiol Behav. 2001;74:551–7. doi: 10.1016/s0031-9384(01)00597-2. [DOI] [PubMed] [Google Scholar]
- 4.Mourao DM, Bressan J, Campbell WW, Mattes RD. Effects of food form on appetite and energy intake in lean and obese young adults. Int J Obes. 2007:1–8. doi: 10.1038/sj.ijo.0803667. [DOI] [PubMed] [Google Scholar]
- 5.DiMeglio DP, Mattes RD. Liquid versus solid carbohydrate: effects on food intake and body weight. Int J Obes Relat Metab Disord. 2000;24:794–800. doi: 10.1038/sj.ijo.0801229. [DOI] [PubMed] [Google Scholar]
- 6.Santangelo A, Peracchi M, Conte D, Fraquelli M, Porrini M. Physical state of meal affects gastric emptying, cholecystokinin release and satiety. Br J Nutr. 1998;80:521–7. doi: 10.1017/s0007114598001615. [DOI] [PubMed] [Google Scholar]
- 7.Peracchi M, Santangelo A, Conte D, et al. The physical state of a meal affects hormone release and postprandial thermogenesis. Br J Nutr. 2000;83:623–8. doi: 10.1017/s0007114500000799. [DOI] [PubMed] [Google Scholar]
- 8.Tieken SM, Leidy HJ, Stull AJ, Mattes RD, Schuster RA, Campbell WW. Effects of solid versus liquid meal-replacement products of similar energy content on hunger, satiety, and appetite-regulating hormones in older adults. Horm Metab Res. 2007;39:389–94. doi: 10.1055/s-2007-976545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Murphy K, Dhillo WS, Bloom S. Gut peptides in the regulation of food intake and energy homeostasis. Endocrin Reviews. 2006;27:719–727. doi: 10.1210/er.2006-0028. [DOI] [PubMed] [Google Scholar]
- 10.Chaudhri OB, Wynne K, Bloom SR. Can gut hormones control appetite and prevent obesity? Diabetes Care. 2008;31(Suppl 2):S284–9. doi: 10.2337/dc08-s269. [DOI] [PubMed] [Google Scholar]
- 11.Flood JE, Roe LS, Rolls BJ. The effect of increased beverage portion size on energy intake at a meal. J Am Diet Assoc. 2006;106:1984–1990. doi: 10.1016/j.jada.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 12.Rolls BJ, Roe LS, Meengs RD. Larger portion sizes lead to a sustained increase in energy intake over 2 days. J Am Diet Assoc. 2006;106:543–549. doi: 10.1016/j.jada.2006.01.014. [DOI] [PubMed] [Google Scholar]
- 13.Rolls BJ, Roe LS, Meengs RD, Wall DE. Increasing the portion size of a sandwich increases energy intake. J Am Diet Assoc. 2004;104:367–372. doi: 10.1016/j.jada.2003.12.013. [DOI] [PubMed] [Google Scholar]
- 14.Harris J, Benedict F. A biometric study of basal metabolism in man. Carnegie Institute of Washington; Washington, D.C.: 1919. [Google Scholar]
- 15.Wolever TM, Jenkins DJ, Jenkins AL, Josse RG. The glycemic index: methodology and clinical implications. Am J Clin Nutr. 1991;54:846–54. doi: 10.1093/ajcn/54.5.846. [DOI] [PubMed] [Google Scholar]
- 16.Zamboni M, Mazzali G, Zoico E, et al. Health consequences of obesity in the elderly: a review of four unresolved questions. Int J Obes (Lond) 2005;29:1011–29. doi: 10.1038/sj.ijo.0803005. [DOI] [PubMed] [Google Scholar]
- 17.Moriguti JC, Das SK, Saltzman E, et al. Effects of a 6-week hypocaloric diet on changes in body composition, hunger, and subsequent weight regain in healthy young and older adults. J Gerontol A Biol Sci Med Sci. 2000;55:B580–7. doi: 10.1093/gerona/55.12.b580. [DOI] [PubMed] [Google Scholar]
- 18.Rolls BJ, Dimeo KA, Shide DJ. Age-related impairments in the regulation of food intake. Am J Clin Nutr. 1995;62:923–31. doi: 10.1093/ajcn/62.5.923. [DOI] [PubMed] [Google Scholar]
- 19.Clarkston WK, Pantano MM, Morley JE, Horowitz M, Littlefield JM, Burton FR. Evidence for the anorexia of aging: gastrointestinal transit and hunger in healthy elderly vs. young adults. Am J Physiol. 1997;272:R243–8. doi: 10.1152/ajpregu.1997.272.1.R243. [DOI] [PubMed] [Google Scholar]
- 20.Melanson KJ, Greenberg AS, Ludwig DS, Saltzman E, Dallal GE, Roberts SB. Blood glucose and hormonal responses to small and large meals in healthy young and older women. J Gerontol A Biol Sci Med Sci. 1998;53:B299–305. doi: 10.1093/gerona/53a.4.b299. [DOI] [PubMed] [Google Scholar]
- 21.MacIntosh CG, Andrews JM, Jones KL, et al. Effects of age on concentrations of plasma cholecystokinin, glucagon-like peptide 1, and peptide YY and their relation to appetite and pyloric motility. Am J Clin Nutr. 1999;69:999–1006. doi: 10.1093/ajcn/69.5.999. [DOI] [PubMed] [Google Scholar]
- 22.Golden JK, Das S, McCrory MA, Roberts SB, Saltzman E. Fasting ghrelin change after weight loss is attenuated in the elderly. Obes Res. 2005;13:A141. [Google Scholar]
- 23.Almiron-Roig E, Chen Y, Drewnowski A. Liquid calories and the failure of satiety: how good is the evidence? Obes Rev. 2003;4:201–12. doi: 10.1046/j.1467-789x.2003.00112.x. [DOI] [PubMed] [Google Scholar]
- 24.Mattes R. Fluid calories and energy balance: the good, the bad, and the uncertain. Physiol Behav. 2006;89:66–70. doi: 10.1016/j.physbeh.2006.01.023. [DOI] [PubMed] [Google Scholar]
- 25.Wouters-Wesseling W, Van Hooijdonk C, Wagenaar L, Bindels J, de Groot L, Van Staveren W. The effect of a liquid nutrition supplement on body composition and physical functioning in elderly people. Clin Nutr. 2003;22:371–7. doi: 10.1016/s0261-5614(03)00034-7. [DOI] [PubMed] [Google Scholar]
- 26.Payette H, Boutier V, Coulombe C, Gray-Donald K. Benefits of nutritional supplementation in free-living, frail, undernourished elderly people: a prospective randomized community trial. J Am Diet Assoc. 2002;102:1088–95. [PubMed] [Google Scholar]
- 27.Cluskey M, Dunton N. Serving meals of reduced portion size did not improve appetite among elderly in a personal-care section of a long-term-care community. J Am Diet Assoc. 1999;99:733–5. doi: 10.1016/S0002-8223(99)00177-7. [DOI] [PubMed] [Google Scholar]
- 28.Barton AD, Beigg CL, Macdonald IA, Allison SP. A recipe for improving food intakes in elderly hospitalized patients. Clin Nutr. 2000;19:451–4. doi: 10.1054/clnu.2000.0149. [DOI] [PubMed] [Google Scholar]
- 29.Cohen D, Farley TA. Eating as an automatic behavior. Prev Chronic Dis. 2008;5:A23. [PMC free article] [PubMed] [Google Scholar]