Abstract
Background
Substance use is highly prevalent among transgender (trans*) females and has been associated with negative health outcomes, including HIV infection. Little is known about psychosocial risk factors that may influence the onset of substance use among trans*female youth, which can contribute to health disparities during adulthood.
Methods
We conducted a secondary data analysis of a study on HIV risk and resilience among trans*female youth (N=292). Prevalence of substance use was assessed and multivariable logistic regression models were used to examine the relationship between posttraumatic stress disorder (PTSD), psychological distress, gender-related discrimination, parental drug or alcohol problems (PDAP) and multiple substance use outcomes.
Results
Most (69%) of the trans*female youth reported recent drug use. In multivariable analyses, those with PTSD had increased odds of drug use [AOR=1.94 (95%CI=1.09–3.44)]. Those who experienced gender-related discrimination had increased odds of drug use [AOR=2.28 (95%CI=1.17–4.44)], drug use concurrent with sex [AOR=2.35 (95%CI=1.11–4.98)] and use of multiple drugs [AOR=3.24 (95%CI=1.52–6.88)]. Those with psychological distress had increased odds of using multiple heavy drugs [AOR=2.27 (95%CI=1.01–5.12)]. Those with PDAP had increased odds of drugs use [AOR=2.62 (95%CI=1.43–4.82)], drug use concurrent with sex [AOR=2.01 (95%CI, 1.15–3.51)] and use of multiple drugs [AOR=2.10 (95%CI=1.22–3.62)].
Conclusions
Substance use is highly prevalent among trans*female youth and was significantly associated with psychosocial risk factors. In order to effectively address substance use among trans*female youth, efforts must address coping related to gender-based discrimination and trauma. Furthermore, structural level interventions aiming to reduce stigma and gender-identity discrimination might also be effective.
Keywords: substance use, transgender, trans*female youth, posttraumatic stress disorder, discrimination, health disparities
1. INTRODUCTION
Substance use, which has been associated with a wide range of negative health outcomes and societal consequences, is highly prevalent among gender and sexual minority populations, including trans*females (Bowers et al., 2011; Garofalo et al., 2006; Marshall et al., 2011; Rapues et al., 2013; Rehm et al., 2009; Sevelius et al., 2009; U.S. Department of Health and Human Services, 2014). Weighted estimates of trans*female samples in the United States reveal high prevalence of crack and other illicit drug use (26.7%) and marijuana use (20.2%) as well as a higher prevalence of problems with alcohol and other drugs (13.7%) relative to the general population (Grant et al., 2004; Herbst et al., 2008). Furthermore, substance use has been associated with HIV-related sexual risk behaviors and HIV infection among trans*females, who have 34.21 fold greater odds of HIV infection compared to the US general adult population (Baral et al., 2013; Reback and Fletcher, 2014; Santos et al., 2014; Sevelius et al., 2009). Given the link between substance use and negative health outcomes in this population, including HIV infection, it is imperative to understand risk factors that may contribute to the use of illicit drugs. This is particularly important among trans*female youth, when events that develop early in life and cause later risk can be intervened upon. Based on limited data from non-probability-based estimates, there is a sharp increase in the prevalence of HIV infection between samples of trans*female youth (4%–19%) and trans*female adults in the US (27.7%), highlighting the critical nature of HIV risk factors that influence behaviors during adolescence and early adulthood (Herbst et al., 2008; Wilson, 2014). Furthermore, compared to both males and females, trans*females have the lowest five-year survival probability after AIDS in San Francisco, suggesting that this increase in prevalence from youth to adulthood cannot be fully explained by the increase in cumulative HIV prevalence in older age groups (San Francisco Department of Public Health, 2012). Moreover, adolescent onset of drug and alcohol consumption has been shown to predict consumption levels in early and later adulthood (Clark et al., 1998; Grant and Dawson, 1998; Grant et al., 2001; Hingson et al., 2006a, b; Moss et al., 2014; Swift et al., 2008).
However, despite the high burden of substance use and HIV among the overall trans*female population, little is known about the prevalence and correlates of substance use in trans*female youth (Conron et al., 2014; Hotton et al., 2013). Due to the limitations in the classification of gender in broader surveillance surveys in the US, significant gaps in the understanding of the unique health and risk patterns among trans*females remain (Conron et al., 2014). Compounding the problem, the limited data for trans*females are also rarely disaggregated by age (Herbst et al., 2008; Hotton et al., 2013). These gaps make gender minorities—particularly young gender minorities—a vastly understudied population, hindering the development of effective public health interventions that specifically target trans*female and youth-specific health issues (Conron et al., 2014; Institute of Medicine, 2011).
Trans*female youth may face a unique set of challenges that make them particularly vulnerable to substance use. Certain mental health outcomes, associated sequelae, and traumatic experiences may be more prevalent among young trans*females, including elevated prevalence of suicide, engagement in sex work, and victimization by violence and trauma (Bradford et al., 2013; Budge et al., 2013; Clements-Nolle et al., 2001; Garofalo et al., 2006; Grant, 2011; Grossman and D'Augelli, 2007; Hoffman, 2014; Testa, 2012; Wilson et al., 2009). In turn, these co-morbidities have been associated with substance use; for example, posttraumatic stress disorder (PTSD), psychological distress and depression have been associated with the use of individual substances as well as multiple substances (Booth et al., 2010; Conway et al., 2006; Deykin and Buka, 1997; Falck et al., 2002; Glasner-Edwards et al., 2009; Grant et al., 2004; Haller and Chassin, 2014; Hien et al., 2005; Tang et al., 2007). Similarly, perceived discrimination has been linked to substance use in multiple populations (Clark, 2014; Hunte and Finlayson, 2013; Otiniano Verissimo et al., 2014; Respress et al., 2013). Additionally, drug and alcohol use of parents has been shown to predict adolescent drug and alcohol use (Bahr et al., 2005; Li et al., 2002; Merikangas et al., 1998; Patrick et al., 2014; Rhee et al., 2003; Yu, 2003; Yule et al., 2013). The role of these psychosocial conditions among trans*female youth has not yet been fully elucidated. This study sought to address these gaps in the literature by describing the prevalence of substance use in a sample of trans*female youth, age 16 to 24 years at enrollment, in an on-going cohort study. This study also sought to explore the relationships between psychosocial risk factors and substance use outcomes in this population.
In this article, we have used the word “trans*females” throughout, but we should note that participants identified both as transgender, female, genderqueer and a variety of other genders along the transgender spectrum. Our decision to use “trans*females” is the result of a community process that was undertaken in San Francisco, California, to agree on the most inclusive terms to capture the spectrum of male-to-female transgender identities while also respecting individuals along the age spectrum (Rapues et al., 2013).
2. MATERIALS AND METHODS
2.1 Study Sample and Data Collection
The SHINE study is a longitudinal study of HIV risk and resilience among trans*female youth; the present analysis uses baseline data from enrollment visits between August, 2012 and December, 2013 as a cross-sectional sample. The target sample size for the study was 300. Study participants were initially recruited using a peer-referral method to obtain a diverse sample of this hard-to-reach population. Slow recruitment chains resulted in adaptations to the sampling methodology including allowance of e-referrals and expanding the number of referrals that successful recruiters could have (Truong et al., 2013). In total, 100 participants were recruited through peer referral. In addition to peer referral, participants were recruited through outreach on social networking sites (e.g., Facebook, Tumblr) and in person at events attended by trans*female youth (e.g., Trans March, Queer Prom) as well as with referrals from both community-based organizations that provide social services to transgender women and youth and gender-specific health clinics. Individuals were eligible for the study if they [1] self-identified as any gender other than that associated with their assigned male sex at birth, [2] were 16–24 years of age, and [3] lived in the San Francisco Bay Area. Informed consent was obtained before starting the behavioral survey, which was administered via hand-held tablet computers. All study procedures were approved by the Institutional Review Board at the University of California, San Francisco. Written consent was obtained from all youths aged 18 years or older and written assent was given by younger participants (in accordance with a review board waiver of parental consent).
2.2 Measures
Psychosocial exposures measured included PTSD, psychological distress, gender-related discrimination and a parental drinking or drug problem (PDAP). PTSD symptoms were determined by use of the four-item Primary Care PTSD Screen (PC-PTSD) with a cutoff of three out of four symptoms in the last twelve months (Boscarino et al., 2011). Psychological distress was measured with the 18 item version of the Brief Symptom Inventory (BSI-18), converting the BSI-18 Global Severity Index (GSI) to Tscores and using a validated clinical cutoff of T > 62 for symptomatic psychological distress in the last seven days (Asner-Self et al., 2006; Derogatis, 2000; Mustanski et al., 2011). The BSI-18 T-scores calculated in this study had high internal consistency (Cronbach’s alpha=0.91). Gender-related discrimination was determined by questions that asked whether participants had ever experienced poor treatment from parents/caregivers, faced difficulties obtaining employment, lost a job/career or educational opportunity, changed schools and/or dropped out of school, or moved away from friends or family as a result of gender identity or gender presentation. Experience of any of the above types of discrimination at any time was defined as having gender-related discrimination in a dichotomous variable for this exposure. PDAP was determined by a single question based on the DSM-IV criteria for substance abuse, which asked whether parents or immediate caregivers had ever “had a drinking or drug problem that got in the way of their work and/or relationships” (American Psychiatric Association, 1994).
Socioeconomic status was determined using self-reported household annual income while accounting for the number of individuals dependent on that income using the US Department of Housing and Urban Development’s FY2014 Income Limits for the San Francisco, CA HUD Metro Federal Market Rent (FMR) Area (Department of Housing and Urban Development, 2013). HIV status was obtained by rapid HIV testing. Rapid finger prick tests were offered by the research assistants to all participants (The Clearview® HIV 1/2 STATPAK ®, Alere, Waltham, MA, USA) regardless of self-reported HIV status. Participants were asked to stay for their results but were not required. All participants who tested positive were referred to the San Francisco Department of Public Health Linkage Integration Navigation Comprehensive Services program which provides and coordinates comprehensive HIV care for newly tested positives and known positives who are currently out of care. Other measures such as whether or not participants had been sexually active in the last six months, highest level of education completed, immigration status, and length of time in the San Francisco Bay Area were also collected.
2.3 Outcomes
Primary outcomes of interest were [1] drug use, defined as any use of marijuana, methamphetamine, crack, cocaine, non-prescribed prescription drugs, ecstasy, GHB, ketamine, heroin or poppers; [2] alcohol use; [3] drug use before or during sex, measured by the question, “how often did you use drugs other than alcohol before or during sex in the last 6 months?”, which was converted into a binary variable to assess presence or absence of any drug use before or during sex; [4] use of multiple drugs; [5] use of multiple light substances and no heavy drugs; and [6] use of multiple heavy drugs, regardless of the use of light substances, in the last six months. “Light” substances included marijuana, poppers and alcohol. “Heavy” drugs included methamphetamine, crack, cocaine, ecstasy, GHB, ketamine and heroin. These definitions, except for the alcohol use (outcome 2) and use of multiple light substances (outcome 5), exclude the use of alcohol and are consistent with prior analyses of polydrug use (Patterson et al., 2005). We use the term “substances” to refer to both drugs and alcohol, whereas we use the term “drugs” to refer to drugs exclusive of alcohol. Although not a primary outcome, binge drinking was defined as 5 or more drinks on one occasion.
2.4 Statistical Analysis
We used multivariable logistic regression models to examine the relationship between the psychosocial measures of interest and the primary substance use outcomes. Our predictors of interest were highly correlated, as were our outcomes. To avoid collinearity issues, we fitted separate regression models that included one substance use outcome (e.g., drug use, alcohol use, drug use before or during sex, use of multiple drugs, etc.) as the dependent variable, one psychosocial measure (e.g., PTSD, psychological distress, gender-related discrimination, or PDAP) as an independent variable and controlled for potential confounders such as age, race/ethnicity and socioeconomic status.
3. RESULTS
3.1 Sample Characteristics
As shown in Table 1, our sample included 292 trans*female youth. A total of 306 participants were recruited but 14 were excluded from this analysis due to ineligibility based on age or gender identity. The mean age was 21 (SD=2) and the sample was racially and ethnically diverse (37% White, 13% Black, 21% Latina/Hispanic, 8% Asian/Pacific Islander, and 21% other/mixed race). Most participants (79%) had been sexually active in the last six months. Among those who had been tested, the prevalence of HIV infection was 4% as determined by rapid HIV test. The majority (61%) of the sample had an annual income of less than $20,000, with two-thirds (66%) categorized as having extreme low income per our measure of socioeconomic status. 16% of the youth in our sample were born outside of the United States and one-third (33%) had been in the San Francisco Bay Area for 1 year or less.
Table 1.
Baseline Characteristics of trans*female youth in San Francisco
| Baseline Characteristics | N (%) | |
|---|---|---|
| Total | 292 | (100) |
| Age, mean (SD) | 21 | (2) |
| Race/ethnicity | ||
| White | 107 | (37) |
| Black | 38 | (13) |
| Latina/Hispanic | 62 | (21) |
| Asian/Pacific Islander | 24 | (8) |
| Other/Mixed | 61 | (21) |
| Sexually Active in Last Six Months | 230 | (79) |
| HIV Positive | 13 | (4) |
| Annual Household Income Per Year | ||
| <$20,000 | 178 | (61) |
| $20,000–30,000 | 32 | (11) |
| $31,000–45,000 | 16 | (5) |
| $46,000–60,000 | 10 | (3) |
| $61,000–75,000 | 3 | (1) |
| $76,000–100,000 | 7 | (2) |
| $101,000–150,000 | 11 | (4) |
| >$150,000 | 7 | (2) |
| Extreme Low Income | 194 | (66) |
| Highest Level of Education Completed | ||
| Grades 1–8 | 1 | (0) |
| Grades 9–11 | 54 | (18) |
| Completed high school or GED | 101 | (35) |
| Some college, AA degree or technical degree | 104 | (36) |
| Bachelors Degree | 28 | (10) |
| Any Post-graduate studies | 4 | (1) |
| Immigration Status | ||
| Foreign Born | 47 | (16) |
| U.S. Born | 244 | (84) |
| Length of Time in San Francisco Bay Area | ||
| 1 year or less | 95 | (33) |
| More than 1 Year | 196 | (67) |
3.2 Psychosocial Measures
As shown in Table 2, most (61%) demonstrated symptoms of PTSD as determined by the PC-PTSD Screen; whereas 14% demonstrated symptoms of psychological distress as determined using the BSI-18. The majority of the sampled youth (80%) had experienced some form of gender-related discrimination in their lifetime and 46% reported PDAP.
Table 2.
Psychosocial Risk Factors and Substance Use among trans*female youth in the San Francisco Bay Area
| Psychosocial Risk Factors | N (%) | |
| Psychosocial Measures | ||
| PTSD | 179 | (61) |
| BSI | 42 | (14) |
| Gender Related Discrimination | 233 | (80) |
| Parental Drug/Alcohol Problem | 133 | (46) |
| Substance Use Measures For Last Six Months | N (%) | |
| Any Drug Use (Excluding Alcohol) | 202 | (69) |
| Alcohol Use | 238 | (82) |
| Binge Drinking (5 or more drinks on one occasion) | 150 | (51) |
| Drug Use Before or During Sex | 96 | (33) |
| Multiple Drug Use | 106 | (36) |
| Multiple Light Substance Use | 93 | (32) |
| Multiple Heavy Drug Use | 44 | (15) |
| Specific Substances | ||
| Marijuana | 183 | (63) |
| Cigarettes | 137 | (47) |
| Ecstacy/GHB/Ketamine | 59 | (20) |
| Non-Prescribed Prescription Drugs | 59 | (20) |
| Crack/Cocaine | 47 | (16) |
| Methamphetamine | 37 | (13) |
| Poppers | 29 | (10) |
| Heroin | 9 | (3) |
3.3 Substance Use Measures
Most (69%) of the sampled youth reported using any drugs in the last six months. The most commonly used drugs were marijuana (63%), “club drugs” such as ecstasy, GHB, or ketamine (20%), non-prescribed prescription drugs (20%), crack/cocaine (16%), and methamphetamine (13%). Most (81%) drank alcohol in the last six months whereas half (51%) engaged in binge drinking. Roughly a third (33%) of the entire sample reported using drugs before or during sex in the last six months (42% among those who had been sexually active). Over half of drug users (52%) used more than one drug, which corresponds to 36% of the entire sample. Additionally, 32% used multiple light substances and no heavy drugs whereas 15% used multiple heavy drugs. Measures for other specific substances are reported in Table 2.
3.4 Multivariable Analysis
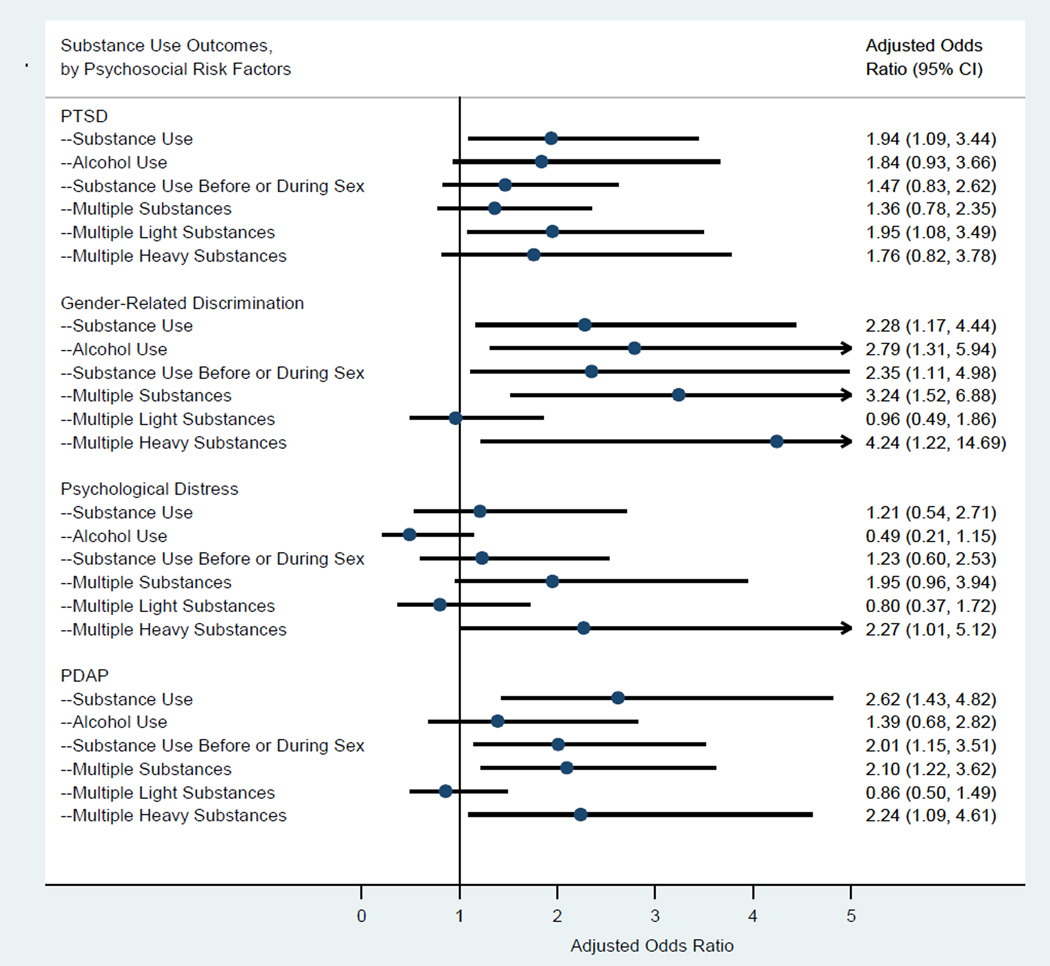
The results of the multivariable analyses are summarized in Figure 1. Trans*female youth who had symptoms of PTSD had nearly twice the odds of engaging in drug use as compared to those without symptoms of PTSD [AOR, 1.94 (95% CI, 1.09–3.44; p-value, 0.02)], independent of age, race/ethnicity and socioeconomic status. Similarly, those with PTSD also had increased odds of using multiple light substances [AOR, 1.95 (95% CI, 1.08–3.49; p-value, 0.03)].
Figure 1.
Multivariable logistic regression analyses: Substance use outcomes and Psychosocial Risk Factors among trans*female youth in the San Francisco Bay Area. All models adjusted for age, race/ethnicity and socioeconomic status.
Trans*female youth who had experienced gender-related discrimination had significantly increased odds for drug use [AOR, 2.28 (95% CI, 1.17–4.44; p-value, 0.02)], alcohol use [AOR, 2.79 (95% CI, 1.31–5.94; p-value, 0.01)], drug use before or during sex [AOR, 2.35 (95% CI, 1.21–4.98; p-value, 0.03)], multiple drug use [AOR, 3.24 (95% CI, 1.52–6.88; p-value, 0.002)], and multiple heavy drug use [AOR, 4.24 (95% CI, 1.22–14.69; p-value, 0.02)] compared to those who had not experienced genderrelated discrimination, while controlling for age, race/ethnicity and socioeconomic status.
Trans*female youth who reported symptoms of psychological distress had increased odds of using multiple heavy drugs [AOR, 2.27 (95% CI, 1.01–5.12; p-value, 0.05)] while adjusting for age, race/ethnicity and socioeconomic status; however, there was no statistically significant relationship between psychological distress and odds of drug use, alcohol use, drug use before or during sex, multiple drug use, or multiple light substance use.
Trans*female youth who reported PDAP showed significantly increased odds for drug use [AOR, 2.62 (95% CI, 1.43–4.82; p-value, 0.002)], drug use before or during sex [AOR, 2.01 (95% CI, 1.15–3.51; pvalue, 0.01)], multiple drug use [AOR, 2.10 (95% CI, 1.22–3.62; p-value, 0.01)], and multiple heavy drug use [AOR, 2.24 (95% CI, 1.09–4.61; p-value, 0.03)] compared to those who did not report such a problem.
4. DISCUSSION
In this sample of trans*female youth, we observed a high prevalence of substance use; use of multiple substances was also common. The prevalence of substance use among our sample was greater than that of the general U.S. adolescent population. For example, in the Youth Risk Behavior Surveillance System, 41% of high school adolescents used marijuana, 7% used ecstasy, 18% used non-prescribed prescription drugs, 6% used cocaine, and 3% used methamphetamine, whereas among our sample of trans*female youth, 63% used marijuana, 20% used “club drugs” such as ecstasy, 20% used non-prescribed prescription drugs, 16% used cocaine/crack, and 13% used methamphetamine (Centers for Disease Control and Prevention, 2014). Although the elevated prevalences in our sample could be partially explained by differences in sampling methods between the compared studies, they are consistent with other studies of trans*female youth (Garofalo et al., 2006; Wilson et al., 2009). We also note that the prevalence of substance use among trans*female youth approached levels reported by trans*female adults in San Francisco and studies of other adult transwomen populations, indicating very early onset (Clements-Nolle et al., 2006; Santos et al., 2014; Xavier et al., 2007). Additionally, we found that roughly one in three trans*female youth reported using drugs in conjunction with sexual intercourse. Thus, the association between PTSD, gender-related discrimination, PDAP and drug use before or during sex is of particular importance because situational use of drugs or alcohol before or during sex has been associated with an increased risk of HIV infection and may be part of the explanation for the extremely high prevalence of HIV among transwomen (Leigh and Stall, 1993). Given the acute and long-term consequences associated with substance use in adolescence, including substance use later in life and increased risk for HIV infection, developing targeted interventions to reduce substance use and associated harm among trans*female youth is a pressing public health issue (Clark et al., 1998; Gillespie et al., 2009; Grant and Dawson, 1998; Grant et al., 2001; Hingson et al., 2006a, b; Moss et al., 2014; Reback and Fletcher, 2014; Santos et al., 2014; Sevelius et al., 2009; Swift et al., 2008).
In this study, trans*female youth also reported high prevalence of PTSD, gender-related discrimination, psychological distress, and PDAP, which were in turn independently and positively associated with drug use in general, as well as use before or during sex. The significant relationship between PTSD and substance use is consistent with prior studies among young people, which have found that PTSD was a significant predictor of substance use (Breslau et al., 2003; Deykin and Buka, 1997; Reed et al., 2007; Wolitzky-Taylor et al., 2012). Researchers have postulated that substances may be used by youth to cope with symptoms of posttraumatic stress—a process described as the “selfmedicating” hypothesis (Chilcoat and Breslau, 1998; Haller and Chassin, 2014; Jacobsen et al., 2001; Reynolds et al., 2005). This hypothesis may also explain the association between gender-related discrimination, psychological distress and increased likelihood of substance use. Indeed, discrimination has been implicated as a contributing factor in substance use in general (Gibbons et al., 2012). It is plausible that trans*female youth use substances to cope with stress and transphobia they experience due to their gender identity. Research on racial discrimination, for instance, has found that engaging in substance use to cope with racial discrimination moderated the relationship between discrimination and substance use over time (Gerrard et al., 2012). Psychological distress related to a young person’s gender identity may similarly influence substance use as a method of coping (Garland et al., 2013). These relationships could also be explained by the “minority stress” theory, which describes how chronic stress—including discrimination and trauma—experienced by minority groups can lead to negative health outcomes and increased risk behaviors (Hatzenbuehler, 2009; Hatzenbuehler et al., 2008; Meyer, 1995, 2003).
Studies exploring the motivations behind the use of various substances can further elucidate the impact of discrimination and trauma on substance use outcomes. Unfortunately, few studies have explored the role of discrimination and trauma on substance use outcomes among trans*female youth (Conron et al., 2014; Hotton et al., 2013). Future studies should endeavor to examine how psychosocial stressors influence substance use and evaluate the long-term impact of these co-morbidities on the health outcomes of trans*female youth. In the interim, interventions that provide and support alternative coping skills may have some success in reducing substance use as a method of dealing with stressors related to gender-based discrimination (Bonica and Daniel, 2003; Goyal et al., 2014).
Because trans*female youth are particularly susceptible to the assessed psychosocial risk factors, linkages represent important avenues through which to focus interventions to curb substance use and associated risk behaviors in this population. Structural level interventions aimed at reducing stigma and gender-identity discrimination may be needed to prevent substance use in this uniquely vulnerable group. Similarly, interventions that give parents the skills to prepare their children to recognize and cope with gender-based (and racial) discrimination may reduce the negative reactions to such stigma and reduce the need for coping, as has been shown in programs and research related to racial and cultural socialization practices of parents (Fisher et al., 2000; Hughes et al., 2006; Yasui and Dishion, 2007).
Furthermore, our findings highlight the potential harmful effect of PDAP on trans*female youth. Our findings, though cross-sectional, are consistent with the documented influence of familial substance abuse on substance use among youth in general, which has been observed in many studies (Clark et al., 1998; Gillespie et al., 2009; Grant and Dawson, 1998; Grant et al., 2001; Hingson et al., 2006a, b; Moss et al., 2014; Swift et al., 2008). Researchers posit that the familial influence may be due to youth modeling their behaviors after that of their substance-using parents, as explained by social learning theory (Akers, 1998; Akers, 1999). Hence, screening for substance abuse and providing referrals to treatment for substance-using parents may translate to reductions in substance use among their offspring.
This study has several limitations. First, the cross-sectional design of the study limits our ability to make causal inferences related to the psychosocial risk factors and substance use among our sample. As the on-going cohort progresses, our analysis provides the framework and opportunity to assess the causal relationships between the strong correlations described here and subsequent risk. Second, our sample was limited to the San Francisco Bay Area so is not generalizable to trans*female youth in other geographic regions. In addition, the self-reported data from this study may be subject to social desirability and recall bias. Also, due to the exploratory nature of this analysis, we did not formally adjust for multiple tests of association. Thus, findings with marginal p-values, such as the association between PTSD and use of multiple light substances (p-value = 0.03) or psychological distress and the use of multiple heavy drugs (p-value = 0.05), should be interpreted with caution. Although the link between alcohol use and increased sexual risk behavior has been well documented in other populations, we did not assess this association in our sample, a limitation which highlights the importance of this link in future research among trans*female youth (Shuper et al., 2009; Vosburgh et al., 2012; Woolf and Maisto, 2009).
Furthermore, this is a non-probability sample which limits our findings from being generalizable to the broader population of trans*female youth in the San Francisco Bay Area. In particular, the overrepresentation of trans*female youth of color (63%) may limit the generalizability of our findings. However, we note that the proportion of participants of color is low relative to a recently conducted population-based study of trans*females in San Francisco, where women of color made up 82% of the sample (Rapues et al., 2013). Moreover, because trans*females of color are disproportionately affected by HIV in San Francisco, it is important to have a high percentage of youth of color represented in these data (Rapues et al., 2013). Although our analyses controlled for potential confounding by race/ethnicity and socioeconomic status in order to focus on gender-related discrimination, it is important for future studies to explore the intersectional effects of multiple dimensions of inequality, such as gender, race/ethnicity and socioeconomic status.
Regardless of these limitations, this study provides important insights into the prevalence and correlates of substance use among an understudied and marginalized population, which has a practical implications for research and public health programming. Future research should explore the societal, institutional and interpersonal bases of PTSD and gender-related discrimination to better understand how they interact with personal coping and substance use among trans*female youth. The illumination of these pathways has the potential to inform the development of policies and programs aiming to mitigate the rampant health disparities facing trans*female adults. Additionally, the potential link between parental drinking or drug problems and substance use among trans*female youth merits further investigation and draws attention to the potential value of inter-generational and familial interventions.
Highlights.
Substance use was highly prevalent among trans*female youth
Psychosocial risk factors were associated with increased odds of substance use
Understanding these psychosocial mechanisms can inform substance use interventions
Targeting substance use represents a possible avenue to mitigate health disparities
Acknowledgements
The authors would like to thank the participants of the SHINE study for taking part in this study.
Role of Funding Source
Funding for this study was awarded by the US National Institute of Mental Health (R01MH095598)
This study's funding source had no role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors All authors contributed to the interpretation of data, and revising the manuscript for important intellectual content. CR led the drafting of the manuscript and conducted the statistical analysis. CR, GMS, and ECW conceived the data analysis plan. WC and ECW conceived and designed the parent cohort study for this baseline data analysis.
Conflict of Interest. No conflict declared
References
- Akers RL. Social Learning and Social Structure: A General Theory of Crime and Deviance. Boston, MA: Northeastern University Press; 1998. [Google Scholar]
- Akers RLLG. Age, social learning, and social bonding in adolescent substance use. Deviant Behav. 1999;20:1–25. [Google Scholar]
- American Psychiatric Association. DSM-IV: Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Asner-Self KK, Schreiber JB, Marotta SA. A cross-cultural analysis of the Brief Symptom Inventory-18. Cultur. Divers. Ethnic Minor. Psychol. 2006;12:367–375. doi: 10.1037/1099-9809.12.2.367. [DOI] [PubMed] [Google Scholar]
- Bahr SJ, Hoffmann JP, Yang X. Parental and peer influences on the risk of adolescent drug use. J. Prim. Prev. 2005;26:529–551. doi: 10.1007/s10935-005-0014-8. [DOI] [PubMed] [Google Scholar]
- Baral SD, Poteat T, Stromdahl S, Wirtz AL, Guadamuz TE, Beyrer C. Worldwide burden of HIV in transgender women: a systematic review and meta-analysis. Lancet Infect. Dis. 2013;13:214–222. doi: 10.1016/S1473-3099(12)70315-8. [DOI] [PubMed] [Google Scholar]
- Bonica C, Daniel JH. Helping adolescents cope with stress during stressful times. Curr. Opin. Pediatrics. 2003;15:385–390. doi: 10.1097/00008480-200308000-00005. [DOI] [PubMed] [Google Scholar]
- Booth BM, Curran G, Han X, Wright P, Frith S, Leukefeld C, Falck R, Carlson RG. Longitudinal relationship between psychological distress and multiple substance use: results from a three-year multisite natural-history study of rural stimulant users. J. Stud. Alcohol Drugs. 2010;71:258–267. doi: 10.15288/jsad.2010.71.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Kirchner HL, Hoffman SN, Sartorius J, Adams RE, Figley CR. A brief screening tool for assessing psychological trauma in clinical practice: development and validation of the New York PTSD Risk Score. Gen. Hosp. Psychiatry. 2011;33:489–500. doi: 10.1016/j.genhosppsych.2011.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowers JR, Branson CM, Fletcher J, Reback CJ. Differences in substance use and sexual partnering between men who have sex with men, men who have sex with men and women and transgender women. Cult. Health Sex. 2011;13:629–642. doi: 10.1080/13691058.2011.564301. [DOI] [PubMed] [Google Scholar]
- Bradford J, Reisner SL, Honnold JA, Xavier J. Experiences of transgender-related discrimination and implications for health: results from the Virginia Transgender Health Initiative Study. Am. J. Public Health. 2013;103:1820–1829. doi: 10.2105/AJPH.2012.300796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N, Davis GC, Schultz LR. Posttraumatic stress disorder and the incidence of nicotine, alcohol, and other drug disorders in persons who have experienced trauma. Arch. Gen. Psychiatry. 2003;60:289–294. doi: 10.1001/archpsyc.60.3.289. [DOI] [PubMed] [Google Scholar]
- Budge SL, Adelson JL, Howard KA. Anxiety and depression in transgender individuals: the roles of transition status, loss, social support, and coping. J. Consult. Clin. Psychol. 2013;81:545–557. doi: 10.1037/a0031774. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Youth Risk Behavior Surveillance - United Sates, 2013. MMWR. 2014;63:1–168. [PubMed] [Google Scholar]
- Chilcoat HD, Breslau N. Posttraumatic stress disorder and drug disorders: testing causal pathways. Arch. Gen. Psychiatry. 1998;55:913–917. doi: 10.1001/archpsyc.55.10.913. [DOI] [PubMed] [Google Scholar]
- Clark DB, Kirisci L, Tarter RE. Adolescent versus adult onset and the development of substance use disorders in males. Drug Alcohol Depend. 1998;49:115–121. doi: 10.1016/s0376-8716(97)00154-3. [DOI] [PubMed] [Google Scholar]
- Clark TT. Perceived discrimination, depressive symptoms, and substance use in young adulthood. Addict. Behav. 2014;39:1021–1025. doi: 10.1016/j.addbeh.2014.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clements-Nolle K, Marx R, Guzman R, Katz M. HIV prevalence, risk behaviors, health care use, mental health status of transgender persons: implications for public health intervention. Am. J. Public Health. 2001;91:915–921. doi: 10.2105/ajph.91.6.915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clements-Nolle K, Marx R, Katz M. Attempted suicide among transgender persons: the influence of gender-based discrimination and victimization. J. Homosex. 2006;51:53–69. doi: 10.1300/J082v51n03_04. [DOI] [PubMed] [Google Scholar]
- Conron KJ, Landers SJ, Reisner SL, Sell RL. Sex and gender in the US health surveillance system: a call to action. Am. J. Public Health. 2014;104:970–976. doi: 10.2105/AJPH.2013.301831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conway KP, Compton W, Stinson FS, Grant BF. Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J. Cliin. Psychiatry. 2006;67:247–257. doi: 10.4088/jcp.v67n0211. [DOI] [PubMed] [Google Scholar]
- Department of Housing and Urban Development. FY2014 FMR Geography Summary for San Francisco, CA HUD Metro FMR Area. [accessed on June 17 2014];2013 http://www.huduser.org/portal/datasets/fmr/fmr_il_history/data_summary.odn?inputname=METRO41860MM7360*San+Francisco%2C+CA+HUD+Metro+FMR+Area%2B0608199999&data=2014&fmrtype=%24fmrtype%24&incpath=%24incpath%24&path=C%3A\huduser\wwwmain\datasets\fmr\fmr_il_history&fmr_year=2014&il_year=2014&area_choice=hmfa&hmfa=Yes>. [Google Scholar]
- Derogatis LR. BSI-18: Administration, Scoring And Procedures Manual. Minneapolis, MN: National Computer Systems; 2000. [Google Scholar]
- Deykin EY, Buka SL. Prevalence and risk factors for posttraumatic stress disorder among chemically dependent adolescents. Am. J. Psychiatry. 1997;154:752–757. doi: 10.1176/ajp.154.6.752. [DOI] [PubMed] [Google Scholar]
- Falck RS, Wang J, Carlson RG, Eddy M, Siegal HA. The prevalence and correlates of depressive symptomatology among a community sample of crack-cocaine smokers. J. Psychoactive Drugs. 2002;34:281–288. doi: 10.1080/02791072.2002.10399964. [DOI] [PubMed] [Google Scholar]
- Fisher C, Wallace S, Fenton R. Discrimination distress during adolescence. J. Youth Adolesc. 2000;29:679–695. [Google Scholar]
- Garland EL, Pettus-Davis C, Howard MO. Self-medication among traumatized youth: structural equation modeling of pathways between trauma history, substance misuse, and psychological distress. J. Behav. Med. 2013;36:175–185. doi: 10.1007/s10865-012-9413-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garofalo R, Deleon J, Osmer E, Doll M, Harper GW. Overlooked, misunderstood and at-risk: exploring the lives and HIV risk of ethnic minority male-to-female transgender youth. J. Adolesc. Health. 2006;38:230–236. doi: 10.1016/j.jadohealth.2005.03.023. [DOI] [PubMed] [Google Scholar]
- Gerrard M, Stock ML, Roberts ME, Gibbons FX, O'Hara RE, Weng CY, Wills TA. Coping with racial discrimination: the role of substance use. Psychol. Addict. Behav. 2012;26:550–560. doi: 10.1037/a0027711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons FX, O'Hara RE, Stock ML, Gerrard M, Weng CY, Wills TA. The erosive effects of racism: reduced self-control mediates the relation between perceived racial discrimination and substance use in African American adolescents. J. Pers. Soc. Psychol. 2012;102:1089–1104. doi: 10.1037/a0027404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillespie NA, Neale MC, Kendler KS. Pathways to cannabis abuse: a multi-stage model from cannabis availability, cannabis initiation and progression to abuse. Addiction. 2009;104:430–438. doi: 10.1111/j.1360-0443.2008.02456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasner-Edwards S, Marinelli-Casey P, Hillhouse M, Ang A, Mooney LJ, Rawson R Methamphetamine Treatment Project Corporate, A. Depression among methamphetamine users: association with outcomes from the Methamphetamine Treatment Project at 3-year follow-up. J. Nerv. Ment. Dis. 2009;197:225–231. doi: 10.1097/NMD.0b013e31819db6fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goyal M, Singh S, Sibinga EM, Gould NF, Rowland-Seymour A, Sharma R, Berger Z, Sleicher D, Maron DD, Shihab HM, Ranasinghe PD, Linn S, Saha S, Bass EB, Haythornthwaite JA. Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Intern. Med. 2014;174:357–368. doi: 10.1001/jamainternmed.2013.13018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Dawson DA. Age of onset of drug use and its association with DSM-IV drug abuse and dependence: results from the National Longitudinal Alcohol Epidemiologic Survey. J. Subst. Abuse. 1998;10:163–173. doi: 10.1016/s0899-3289(99)80131-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch. Gen. Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Harford TC. Age at onset of alcohol use and DSM-IV alcohol abuse and dependence: a 12-year follow-up. J. Subst. Abuse. 2001;13:493–504. doi: 10.1016/s0899-3289(01)00096-7. [DOI] [PubMed] [Google Scholar]
- Grant JMM, L A, Tanis J, Harrison J, Herman JL, Keisling M. Injustice At Every Turn: A Report Of The National Transgender Discrimination Survey. Washington, DC: National Center For Transgender Equality And National Gay And Lesbian Task Force; 2011. [Google Scholar]
- Grossman AH, D'Augelli AR. Transgender youth and life-threatening behaviors. Suicide Life Threat. ehav. 2007;37:527–537. doi: 10.1521/suli.2007.37.5.527. [DOI] [PubMed] [Google Scholar]
- Haller M, Chassin L. Risk pathways among traumatic stress, posttraumatic stress disorder symptoms, and alcohol and drug problems: a test of four hypotheses. Psychol. Addict. Behav. 2014;28:841–851. doi: 10.1037/a0035878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML. How does sexual minority stigma "get under the skin"? A psychological mediation framework. Psychol. Bull. 2009;135:707–730. doi: 10.1037/a0016441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Nolen-Hoeksema S, Erickson SJ. Minority stress predictors of HIV risk behavior, substance use, depressive symptoms: results from a prospective study of bereaved gay men. Health Psychol. 2008;27:455–462. doi: 10.1037/0278-6133.27.4.455. [DOI] [PubMed] [Google Scholar]
- Herbst JH, Jacobs ED, Finlayson TJ, McKleroy VS, Neumann MS, Crepaz N, Team HAPRS. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS Behav. 2008;12:1–17. doi: 10.1007/s10461-007-9299-3. [DOI] [PubMed] [Google Scholar]
- Hien D, Cohen L, Campbell A. Is traumatic stress a vulnerability factor for women with substance use disorders? Clinical Psychol. Rev. 2005;25:813–823. doi: 10.1016/j.cpr.2005.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hingson RW, Heeren T, Winter MR. Age at drinking onset and alcohol dependence: age at onset, duration, and severity. Arch. Pediatr. Adolesc. Med. 2006a;160:739–746. doi: 10.1001/archpedi.160.7.739. [DOI] [PubMed] [Google Scholar]
- Hingson RW, Heeren T, Winter MR. Age of alcohol-dependence onset: associations with severity of dependence and seeking treatment. Pediatrics. 2006b;118:e755–e763. doi: 10.1542/peds.2006-0223. [DOI] [PubMed] [Google Scholar]
- Hoffman B. An overview of depression among transgender women. Depress. Res. Treat. 2014;2014:394283. doi: 10.1155/2014/394283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hotton AL, Garofalo R, Kuhns LM, Johnson AK. Substance use as a mediator of the relationship between life stress and sexual risk among young transgender women. AIDS Educ. Prev. 2013;25:62–71. doi: 10.1521/aeap.2013.25.1.62. [DOI] [PubMed] [Google Scholar]
- Hughes D, Rodriguez J, Smith EP, Johnson DJ, Stevenson HC, Spicer P. Parents' ethnic-racial socialization practices: a review of research and directions for future study. Dev. Psychol. 2006;42:747–770. doi: 10.1037/0012-1649.42.5.747. [DOI] [PubMed] [Google Scholar]
- Hunte HE, Finlayson TL. The relationship between perceived discrimination and psychotherapeutic and illicit drug misuse in Chicago, IL, USA. J. Urban Health. 2013;90:1112–1129. doi: 10.1007/s11524-013-9822-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. The health Of Lesbian, Gay, Bisexual, And Transgender People: Building A Foundation For Better Understanding. Washington, DC: The National Academies Press; 2011. [PubMed] [Google Scholar]
- Jacobsen LK, Southwick SM, Kosten TR. Substance use disorders in patients with posttraumatic stress disorder: a review of the literature. Am. J. Psychiatry. 2001;158:1184–1190. doi: 10.1176/appi.ajp.158.8.1184. [DOI] [PubMed] [Google Scholar]
- Leigh BC, Stall R. Substance use and risky sexual behavior for exposure to HIV. Issues in methodology, interpretation, and prevention. Am. Psychol. 1993;48:1035–1045. doi: 10.1037//0003-066x.48.10.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li C, Pentz MA, Chou CP. Parental substance use as a modifier of adolescent substance use risk. Addiction. 2002;97:1537–1550. doi: 10.1046/j.1360-0443.2002.00238.x. [DOI] [PubMed] [Google Scholar]
- Marshall BD, Wood E, Shoveller JA, Patterson TL, Montaner JS, Kerr T. Pathways to HIV risk and vulnerability among lesbian, gay, bisexual, and transgendered methamphetamine users: a multi-cohort gender-based analysis. BMC Public Health. 2011;11:20. doi: 10.1186/1471-2458-11-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, Stolar M, Stevens DE, Goulet J, Preisig MA, Fenton B, Zhang H, O'Malley SS, Rounsaville BJ. Familial transmission of substance use disorders. Arch. Gen. Psychiatry. 1998;55:973–979. doi: 10.1001/archpsyc.55.11.973. [DOI] [PubMed] [Google Scholar]
- Meyer IH. Minority stress and mental health in gay men. J. Health Soc. Behav. 1995;36:38–56. [PubMed] [Google Scholar]
- Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, bisexual populations: conceptual issues and research evidence. Psychol. Bull. 2003;129:674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss HB, Chen CM, Yi HY. Early adolescent patterns of alcohol, cigarettes, and marijuana polysubstance use and young adult substance use outcomes in a nationally representative sample. Drug Alcohol Depend. 2014;136:51–62. doi: 10.1016/j.drugalcdep.2013.12.011. [DOI] [PubMed] [Google Scholar]
- Mustanski B, Newcomb M, Garofalo R. Mental health of lesbian, gay, bisexual youth: A developmental resiliency perspective. J. Gay Lesbian Soc. Serv. 2011;23:204–225. doi: 10.1080/10538720.2011.561474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otiniano Verissimo AD, Grella CE, Amaro H, Gee GC. Discrimination and substance use disorders among latinos: the role of gender, nativity, and ethnicity. Am. J. Public Health. 2014:e1–e8. doi: 10.2105/AJPH.2014.302011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Maggs JL, Greene KM, Morgan NR, Schulenberg JE. The Link between mother and adolescent substance use: intergenerational findings from the British Cohort Study. Longit. Life Course Stud. 2014;5:56–63. doi: 10.14301/llcs.v5i1.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson TL, Semple SJ, Zians JK, Strathdee SA. Methamphetamine-using HIV-positive men who have sex with men: correlates of polydrug use. J. Urban Health. 2005;82:i120–i126. doi: 10.1093/jurban/jti031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapues J, Wilson EC, Packer T, Colfax GN, Raymond HF. Correlates of HIV infection among transfemales, San Francisco, 2010: results from a respondent-driven sampling study. Am. J. Public Health. 2013;103:1485–1492. doi: 10.2105/AJPH.2012.301109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reback CJ, Fletcher JB. HIV prevalence, substance use, sexual risk behaviors among transgender women recruited through outreach. AIDS Behav. 2014;18:1359–1367. doi: 10.1007/s10461-013-0657-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed PL, Anthony JC, Breslau N. Incidence of drug problems in young adults exposed to trauma and posttraumatic stress disorder: do early life experiences and predispositions matter? Arch. Gen. Psychiatry. 2007;64:1435–1442. doi: 10.1001/archpsyc.64.12.1435. [DOI] [PubMed] [Google Scholar]
- Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373:2223–2233. doi: 10.1016/S0140-6736(09)60746-7. [DOI] [PubMed] [Google Scholar]
- Respress BN, Small E, Francis SA, Cordova D. The role of perceived peer prejudice and teacher discrimination on adolescent substance use: a social determinants approach. J. Ethn. Subst. Abuse. 2013;12:279–299. doi: 10.1080/15332640.2013.836728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds M, Mezey G, Chapman M, Wheeler M, Drummond C, Baldacchino A. Co-morbid post-traumatic stress disorder in a substance misusing clinical population. Drug Alcohol Depend. 2005;77:251–258. doi: 10.1016/j.drugalcdep.2004.08.017. [DOI] [PubMed] [Google Scholar]
- Rhee SH, Hewitt JK, Young SE, Corley RP, Crowley TJ, Stallings MC. Genetic and environmental influences on substance initiation use, problem use in adolescents. Arch. Gen. Psychiatry. 2003;60:1256–1264. doi: 10.1001/archpsyc.60.12.1256. [DOI] [PubMed] [Google Scholar]
- San Francisco Department of Public Health. 2011 HIV/AIDS Epidemiology Annual Report. San Francisco, CA: San Francisco Department of Public Health; 2012. [Google Scholar]
- Santos GM, Rapues J, Wilson EC, Macias O, Packer T, Colfax G, Raymond HF. Alcohol and substance use among transgender women in San Francisco: prevalence and association with human immunodeficiency virus infection. Drug Alcohol Rev. 2014;33:287–295. doi: 10.1111/dar.12116. [DOI] [PubMed] [Google Scholar]
- Sevelius JM, Reznick OG, Hart SL, Schwarcz S. Informing interventions: the importance of contextual factors in the prediction of sexual risk behaviors among transgender women. AIDS Educ. Prev. 2009;21:113–127. doi: 10.1521/aeap.2009.21.2.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shuper PA, Joharchi N, Irving H, Rehm J. Alcohol as a correlate of unprotected sexual behavior among people living with HIV/AIDS: review and meta-analysis. AIDS Behav. 2009;13:1021–1036. doi: 10.1007/s10461-009-9589-z. [DOI] [PubMed] [Google Scholar]
- Swift W, Coffey C, Carlin JB, Degenhardt L, Patton GC. Adolescent cannabis users at 24 years: trajectories to regular weekly use and dependence in young adulthood. Addiction. 2008;103:1361–1370. doi: 10.1111/j.1360-0443.2008.02246.x. [DOI] [PubMed] [Google Scholar]
- Tang YL, Kranzler HR, Gelernter J, Farrer LA, Cubells JF. Comorbid psychiatric diagnoses and their association with cocaine-induced psychosis in cocaine-dependent subjects. Am. J. Addict. 2007;16:343–351. doi: 10.1080/10550490701525723. [DOI] [PubMed] [Google Scholar]
- Testa RJ, Sciacca LM, Wang F, Hendricks M, Goldblum P, Bradford J, Bongar B. The effects of violence on transgender people. Prof. Psychol. Res. Pr. 2012;43:4520459. [Google Scholar]
- Truong HM, Grasso M, Chen YH, Kellogg TA, Robertson T, Curotto A, Steward WT, McFarland W. Balancing theory and practice in respondent-driven sampling: a case study of innovations developed to overcome recruitment challenges. PloS One. 2013;8:e70344. doi: 10.1371/journal.pone.0070344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Substance abuse. [accessed on June 18 2014];2014 http://www.healthypeople.gov/2020/LHI/substanceAbuse.aspx>.
- Vosburgh HW, Mansergh G, Sullivan PS, Purcell DW. A review of the literature on event-level substance use and sexual risk behavior among men who have sex with men. AIDS Behav. 2012;16:1394–1410. doi: 10.1007/s10461-011-0131-8. [DOI] [PubMed] [Google Scholar]
- Wilson EC. SHINE Baseline Dataset. United Kingdom: Rand; 2014. [Google Scholar]
- Wilson EC, Garofalo R, Harris RD, Herrick A, Martinez M, Martinez J, Belzer M Transgender Advisory, C., the Adolescent Medicine Trials Network for, H.I.V.A.I. Transgender female youth and sex work: HIV risk and a comparison of life factors related to engagement in sex work. AIDS Behav. 2009;13:902–913. doi: 10.1007/s10461-008-9508-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolitzky-Taylor K, Bobova L, Zinbarg RE, Mineka S, Craske MG. Longitudinal investigation of the impact of anxiety and mood disorders in adolescence on subsequent substance use disorder onset and vice versa. Addict. Behav. 2012;37:982–985. doi: 10.1016/j.addbeh.2012.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf SE, Maisto SA. Alcohol use and risk of HIV infection among men who have sex with men. AIDS Behav. 2009;13:757–782. doi: 10.1007/s10461-007-9354-0. [DOI] [PubMed] [Google Scholar]
- Xavier J, Honnold JA, Bradford J. The Health, health-related needs, and lifecourse experiences of transgender Virginians. Richmond: Virginia HIV Community Planning Committee and Virginia Department of Health; 2007. [Google Scholar]
- Yasui M, Dishion TJ. The ethnic context of child and adolescent problem behavior: implications for child and family interventions. Clin. Child family Psychol. Rev. 2007;10:137–179. doi: 10.1007/s10567-007-0021-9. [DOI] [PubMed] [Google Scholar]
- Yu J. The association between parental alcohol-related behaviors and children's drinking. Drug Alcohol Depend. 2003;69:253–262. doi: 10.1016/s0376-8716(02)00324-1. [DOI] [PubMed] [Google Scholar]
- Yule AM, Wilens TE, Martelon MK, Simon A, Biederman J. Does exposure to parental substance use disorders increase substance use disorder risk in offspring? A 5-year follow-up study. Am. J. Addict. 2013;22:460–465. doi: 10.1111/j.1521-0391.2013.12048.x. [DOI] [PubMed] [Google Scholar]