Abstract
Despite documented common use of traditional healers and efforts to scale up ART in sub-Saharan Africa, evidence on whether medical pluralism predicts ART use is inconclusive and restricted to clinic settings. This study quantitatively assesses whether medical pluralism predicts ART use among parents in need of ART in South Africa. 2477 parents or primary caregivers of children were interviewed in HIV-endemic communities of KwaZulu-Natal. Analysis used multiple logistic regression on a subsample of 435 respondents in need of ART, who reported either medical pluralism (24.6%) or exclusive public healthcare use (75.4%). Of 435 parents needing ART, 60.7% reported ART use. Medical pluralism emerged as a persistent negative predictor of ART utilization among those needing it (AOR [95% CI]= .556 [.344 – .899], p=.017). Use of traditional healthcare services by those who need ART may act as a barrier to treatment access. Effective intersectoral collaboration at community level is urgently needed.
Keywords: antiretrovirals, ART, traditional healers, medical pluralism, South Africa
INTRODUCTION
Antiretroviral treatment (ART) has averted 1.8 million deaths in sub-Saharan Africa1. ART effectively delays mortality2, reduces horizontal3–5 and vertical6 HIV-transmission, prevents HIV-associated tuberculosis7 and enhances the quality of life for HIV-positive people8,9. South Africa has the largest ART programme in the world, with 83% coverage10. Full ART coverage requires continued efforts to design effective implementation strategies based on scientific evidence.
Medical pluralism or use of multiple healthcare modalities by HIV-positive people is common in South Africa: 51.3% in a 2008 survey of HIV-positive patients within three public hospitals in KwaZulu-Natal (n=618)11. Medical pluralism has been associated with delayed HIV testing12 and heightened healthcare expenditure and increased likelihood of debt13. In a study using systematic sampling of ART patients, 90% of participants reported that their healthcare provider was not aware that they were taking herbal therapies14. Over time, people living with HIV in South Africa have been found to use multiple healthcare modalities both concurrently and sequentially12. Higher HIV symptomatology, family members not contributing to main source of household income, access to health insurance and the disability grant, perceived disrespect by staff and lack of privacy in health facilities and rural residence have been associated with higher likelihood of use of traditional medicine among HIV-positive patients13,14.
However, quantitative evidence on whether medical pluralism predicts ART use remains scarce throughout sub-Saharan Africa. A case-control study in a Ugandan ART clinic found that those who sought care from traditional/spiritual healers before coming to the clinic were more likely to have late ART initiation (CD4 < 50 cells/µL) than individuals who did not report seeking care from traditional/spiritual healers15. Conversely, another Ugandan study of 450 ART patients found that seeking care from traditional healers/spiritual healers was not significantly associated with lower CD4 counts at ART initiation16, suggesting that use of traditional healers did not delay ART initiation. Further research examining whether medical pluralism predicts ART use is clearly required.
Existing studies utilized clinic-based samples of patients who were either on ART or in the process of initiating treatment, by definition excluding people who have never initiated treatment or who have dropped-out of care. Therefore evidence from community samples will valuably add to clinic data. Additionally, few studies have focused on parents, despite potential intergenerational benefits of sustaining the health and wellbeing of this population17–19. This study aims to address gaps in available evidence by quantitatively exploring whether medical pluralism predicts ART use in a community-based sample of parents in need of ART.
METHODS
PROCEDURES
A cross-sectional survey was administered in 2010 in rural and peri-urban communities (>30% antenatal HIV prevalence) of KwaZulu-Natal, South Africa. 2477 households were selected through stratified systematic random sampling of census enumeration or tribal authority areas. Parents from households within randomised enumeration areas were recruited through door-to-door sampling. Because the larger study in which this current study is nested assessed the impact of parental AIDS on adolescents, only households with at least one child aged 10 – 17 were eligible. Parents were interviewed if they were above the age of 18 and if they provided primary care for at least one child. Primary care was defined as taking on responsibilities for childcare duties; the parent could therefore be a biological or foster parent. If more than one eligible adult was identified in the same household, random selection was used to decide which parent to interview.
Ethical approval was obtained from Universities of KwaZulu-Natal (May 2010) and Oxford (August 2009), and the KwaZulu-Natal Department of Health (August 2009). Participants completed 45 – 60 minutes face-to-face interviews with research assistants trained in research ethics. Questionnaires were translated into Zulu and back-translated to assure accuracy and cultural equivalence20. Participation was voluntary with informed written consent obtained from all respondents. Financial remuneration was not provided but respondents received refreshments and certificates of thanks regardless of participating. To avoid stigmatization, we mentioned HIV only within general health questions. These questions were prefaced with reminders that participants could stop the interview or skip questions without consequence to them, their family, or services. Irrespective of whether they reported being HIV-positive, respondents reporting severe morbidity were offered referrals and transport to healthcare facilities with testing and treatment.
DETERMNING ART NEED AT COMMUNITY LEVEL
We designed a strategy to assess ART need within a community that followed low CD4 count (< 200 cells/µL) requirements for ART initiation. To avoid stigmatization, we did not use biomarkers and respondents were asked about HIV only within general health questions. Respondents were considered to be in need of ART if they met any of the following criteria: i) a conservative threshold of display of 3 or more AIDS-related symptoms, ii) self-reported ART use or iii) self-reported CD4 count < 200 cells/µL. AIDS-related symptomatology was measured via response to Verbal Autopsy, a questionnaire developed to identify symptoms of AIDS in areas with over 20% HIV prevalence and where data on cause of death or illness is unavailable or unreliable21,22. Verbal Autopsy is increasingly used for determining AIDS mortality in generalized epidemics21,23,24 and recent research found it to have 75% – 83% sensitivity and 74% – 79% specificity among adult subjects25. The ART use and CD4 count criteria were based on South Africa’s ART eligibility guidelines at the time of the survey26.
MEASURES
ART use was operationalised as “Do you use antiretrovirals?” in the questionnaire; responses were coded as a binary variable (0:‘No’; 1:‘Yes)’. Medical pluralism was determined based on self-reported healthcare use. Respondents were asked whether they had used public hospitals, public clinics or traditional healers in the past 6 months. Traditional healers were defined as traditional practitioners who treat illnesses through the use of traditional products and methods as medicine (‘umelaphi wendabuko’ in isiZulu)27. Medical pluralism was defined as having used both public healthcare (public hospitals or public clinics) and traditional healers, whereas exclusive public healthcare use was defined as having used public healthcare and not having used traditional healers. A dichotomous variable was created to contrast medical pluralism to exclusive public healthcare use (0:‘exclusive public healthcare use’; 1:‘medical pluralism’.
Potential covariates
We measured potential confounding factors of age, gender, rural residency, employment status, years of education, mental health, poverty, perceived stigma, social support and disability grant receipt28–34. The clinical cut-off for disability grant receipt applied in most hospitals and clinics in South Africa is an AIDS-defining illness or CD4 count < 20035. Grant receipt is discontinued when CD4 counts increase under the rationale that once patients regain health they are able to work for a wage36.
Socio-demographic variables (age, gender, population, language, education) were collected using items modeled on the South African National Census37 and the KwaZulu-Natal Income Dynamics Study questionnaire38. Household poverty was measured via response to the 25-item South African economic asset index39 from the Demographic and Health Surveys. The index has been shown to be equally or more reliable than other conventional measures of poverty40,41.
Depression was measured using the 20-item Centre for Epidemiological Studies Depression Scale (CES-D). CES-D has been used and validated in South African populations42,43 and displayed strong internal consistency in this study sample (α=.94). Anxiety was measured using the 21-item Beck Anxiety Inventory (BAI), which has been validated with Xhosa participants44. It displayed strong internal consistency in this study sample (α=.95).
Perceived social support was measured via response to the 19-item Medical Outcome Study Social Support Survey (MOS-SSS)45 including emotional, tangible, and affectionate support, as well as positive social interaction. MOS-SSS has displayed strong internal consistency α=.91 to .97 and test-retest reliability α=.72 to .78)45. Within this study sample, MOS-SSS displayed strong internal consistency (α=.99). Perceived stigma was measured through responses to 17-item USAID HIV stigma indicators (e.g. ‘In the past year, have you or your family been gossiped about’)46. We added a prompt asking about how the respondents were treated ‘if [they were] sick or because someone in [their] family has been sick or died’. The indicators displayed strong internal consistency within this sample (α=.81).
ANALYSIS STRATEGY
Overall 451 respondents were identified to be in need of ART. Analyses included data from 435 respondents. Respondents in need of ART but reporting non-use of any public healthcare (n=14 respondents using neither public nor traditional healthcare and 2 respondents using only traditional healthcare) were excluded from the analysis as not pertinent to the investigation of medical pluralism.
The analysis strategy consisted of two phases. First, an exploratory phase determined variables to be included in the final model. Hypothesized covariates were independently entered into bivariate logistic regressions as independent variables, with ART use (outcome of interest) and medical pluralism (predictor of interest) as dependent variables. Only covariates for which significant associations (at the p < .05 level) were observed with either medical pluralism or ART use were included in the final model.
Second, the final model determined whether medical pluralism predicts ART use. This was a multiple logistic regression, with variables identified in the exploratory phase entered simultaneously as covariates in the final multivariate model and medical pluralism entered as the independent variable. ART use was entered as the dependent variable. Missing data for all variables were verified and found to be less than 0.5%. Therefore advanced missing data management procedures were not necessary47 and missing cases were excluded listwise.
RESULTS
SAMPLE CHARACTERISTICS
We report on the subsample of 435 respondents included in the analysis. Of the 435 respondents in need of ART, 60.7% (n=264) reported ART use. The mean age of respondents was 41 years for ART users and 43 years among non-ART users. 89.4% of ART users and 87.7% of non-ART users were female. All respondents identified themselves as Black African. 96.6% of ART users and 94.7% of non-ART users spoke Zulu as their first language. 51.9% of ART users and 52.6% of non-ART users reported household material deprivation of at least 2 items on the economic asset index. 12.5% of respondents reported being recipients of the disability grant (14.8% of ART users and 8.8% of non-ART users). 89.8% of ART users and 93.0% of non-ART users reported receipt of any welfare grant at the household level (Table 1).
Table 1.
Socio-Demographic Characteristics by ART use (n=435)
| ART users (n=171) | Non-ART users (n=264) | ||||||
|---|---|---|---|---|---|---|---|
| % (n) | Mean | SD | % (n) | Mean | SD | p | |
| Age | - | 41.1 | 8.3 | 43.2 | 12.5 | .035 | |
| Gender | |||||||
| Female | 89.4% (153) | - | - | 87.7% (232) | - | - | .590 |
| Male | 10.6% (18) | - | - | 12.3% (32) | - | - | |
| Population | |||||||
| African/Black | 100% (171) | - | - | 100% (264) | - | - | |
| Language | |||||||
| Zulu | 96.6% (165) | - | - | 94.7% (250) | - | - | .153 |
| Xhosa | 2.7% (5) | - | - | 2.3% (6) | - | - | |
| Other | 0.7% (1) | - | - | 3.0% (8) | - | - | |
| Education | |||||||
| Primary or less | 58.8% (101) | - | - | 66.7% (176) | - | - | .145 |
| Any secondary | 41.2% (70) | - | - | 33.3% (88) | - | - | |
| Household location | |||||||
| Rural | 34.5% (59) | - | - | 30.4% (80) | - | - | .380 |
| Urban | 65.5% (112) | - | - | 69.6% (184) | - | - | |
| Asset deprivation | |||||||
| Deprivation of 2+ items | 51.9% (89) | - | - | 52.6% (139) | - | - | .881 |
| Grant assistance | |||||||
| Disability grant receipt | 14.8% (25) | - | - | 8.8% (23) | - | - | .064 |
| Any grant receipt | 89.8% (154) | - | - | 93.0% (246) | - | - | .253 |
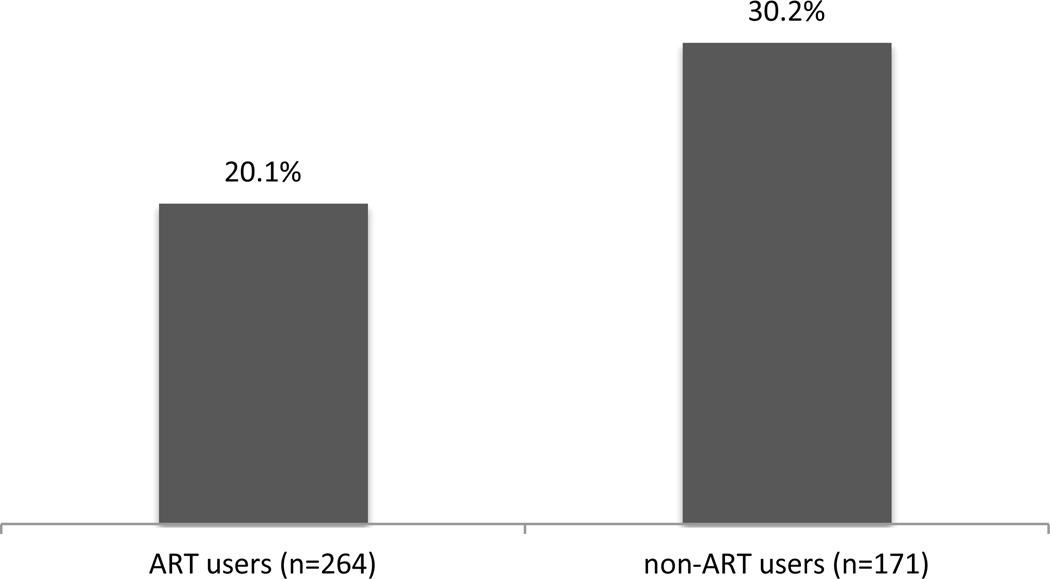
Just under a quarter (24.6%, n=107) of respondents reported medical pluralism use while 75.4% (n=328) reported exclusive public healthcare use in the past six months. The proportion of medical pluralists among ART users was 20.1%, compared to 30.2% among non-ART users (r=−.130, p=.006) (Figure 1).
Fig. 1.
Differential rates of medical pluralism among users and non-users of ART
EXPLORATORY RESULTS: DETERMINING VARIABLES TO BE INCLUDED IN THE FINAL MODEL (Table 2)
Table 2.
Determining confounders to be included in final model: Predictors of medical pluralism and ART use
| Predictors of Medical Pluralism |
Predictors of ART use |
|||||||
|---|---|---|---|---|---|---|---|---|
|
95% CI |
95% CI |
|||||||
| OR | Lower | Upper | p | OR | Lower | Upper | p | |
| Age | 1.004 | .982 | 1.025 | .742 | .980 | .962 | .999 | .037 |
| Gender 1.00 (female, n=385) | .709 | .370 | 1.360 | .319 | 1.180 | .647 | 2.154 | .590 |
| Years of education | .931 | .890 | .975 | .002 | .995 | .973 | 1.017 | .624 |
| Employment status 1.00 (employed, n=337) | 1.141 | .683 | 1.907 | .614 | 1.088 | .685 | 1.729 | .720 |
| Household location 1.00 (rural, n= 139) | 3.594 | 2.020 | 6.392 | .000 | .831 | .550 | 1.256 | .379 |
| Household poverty | 1.194 | .924 | 1.143 | .273 | .943 | .754 | 1.179 | .604 |
| Depression score | 1.027 | 1.010 | 1.043 | .002 | .980 | .965 | .994 | .006 |
| Anxiety score | 1.029 | 1.013 | 1.045 | .000 | .999 | .985 | 1.013 | .877 |
| Social support | .995 | .989 | 1.002 | .162 | .999 | .993 | 1.005 | .680 |
| Perceived stigma | 1.077 | .989 | 1.171 | .390 | .960 | .887 | 1.038 | .304 |
| Disability grant receipt 1.00 (receives grant, n=48) | .495 | .226 | 1.086 | .079 | 1.803 | .961 | 3.383 | .067 |
| Number of AIDS-related symptoms | 1.121 | 1.010 | 1.244 | .032 | .808 | .733 | .890 | .000 |
Table 2 summarizes results of our exploratory regressions used to determine variables to be included in the final model. Fewer years of education (OR [95%CI]=.931 [.890 –.975], p=.002),rural household location (OR [95%CI]=3.594 [2.020-6.392], p < .001), heightened depression (OR [95%CI]= 1.027 [1.010-1.043], p=.002) and anxiety scores (OR [95%CI]=1.029 [1.013-1.045], p < .001), and more AIDS-related symptoms (OR [95%CI]=1.121 [1.010-1.244], p=.032) were independently associated with greater odds of medical pluralism. Age, gender, employment status, household poverty, social support, perceived stigma and disability grant receipt were not independently associated with medical pluralism. Younger age (OR [95%CI]= .980 [.962 –.999], p < .001), lower depression scores (OR [95%CI]=.980 [.965 –.994], p=.006) and fewer AIDS-related symptoms (OR [95%CI]=.808 [.733–.890], p < .001) were independently associated with greater odds of ART use. Gender, years of education, employment status, rural location, household poverty, anxiety scores, social support, perceived stigma, disability grant receipt and number of AIDS-related symptoms were not independently associated with ART use. Variables that were not independently associated with medical pluralism or ART use were excluded from further analysis.
FINAL MODEL RESULTS: ASSESSING WHETHER MEDICAL PLURALISM PREDICTS ART USE (Table 3)
Table 3.
Final model results: medical pluralism predicts ART use
|
95% CI |
||||
|---|---|---|---|---|
| AOR | Lower | Upper | p | |
| Age | .974 | .954 | .995 | .014 |
| Years of education | .979 | .950 | 1.008 | .159 |
| Rural household location | .925 | .571 | 1.500 | .753 |
| Depression score | .975 | .956 | .994 | .010 |
| Anxiety score | 1.026 | 1.006 | 1.045 | .009 |
| Number of AIDS-related symptoms | .817 | .736 | .906 | .000 |
| Medical pluralism | .556 | .344 | .899 | .017 |
| 1.00 (medical pluralism, n=107) | ||||
Table 3 summarizes results of our final model assessing whether medical pluralism predicts ART use. After controlling for covariates identified in exploratory regressions, medical pluralism was associated with lower odds of ART use (AOR [95%CI]=.556 [.344–.899], p=.017). Younger age (AOR [95%CI]=.974 [.954 – .994], p=.014), lower depression scores (AOR [95%CI]=.975 [.956 – .994], p=.01), higher anxiety scores (AOR [95%CI]=1.026 [1.006-1.045], p=.009) and fewer AIDS-related symptoms (AOR [95%CI]=.817 [.736 – .906], p < .001) remained associated with greater odds of ART use, whereas years of education and rural household location became non-significant.
DISCUSSION
Comparable to 2010 national ART coverage estimates of 60-65%48, prevalence of ART use was 60.7% in this study sample. Medical pluralism emerged as a persistent negative predictor of ART utilization among those needing it. The proportion of medical pluralists among non-ART users was 30.2%, compared to 20.1% among ART users. This might be explained by delayed HIV testing12 or ART dropout resulting from conflict between traditional and clinic treatment advice33. However, the mixed state of quantitative evidence on the relationship between medical pluralism and ART uptake15,16 mandates further research before firm inferences can be made.
Compared to earlier South African studies with clinical HIV-positive samples, we found substantively lower rates of medical pluralism (< 25% compared to > 50%)14. This difference might reflect improved health policies and treatment access since 2009 and the community-based sample. Nonetheless, our findings indicate that adults in need of ART continue to use multiple healthcare modalities for their health, more so than the general population49. Thereby our finding that medical pluralism acts as a predictor for non-ART use warrants concern, particularly as it was robust to the removal of effects of mental health, physical health and socio-economic covariates.
Consistent with clinic-based research from South Africa13, the present study suggested that respondents residing in rural areas were more likely to utilize multiple healthcare modalities than respondents from urban settlements. This might be partly explained by lower density of clinics in rural areas, as well as quality of care factors13. Depression and anxiety were also associated with greater odds of engaging in medical pluralism. These findings complement research from Uganda, which detected high prevalence of psychological distress among users of traditional healthcare services (65.1%)50, suggesting a need for improved psychological support in the public healthcare sector. Inconsistent with clinic-based findings from South Africa13, we did not find an association between disability grant receipt and medical pluralism. Given that our community-based sample included people not accessing ART as well, the disability grant might not be facilitating medical pluralism among the broader population of people living with HIV. Respondents with fewer years of education and more AIDS-related symptoms were also more likely to use multiple healthcare modalities. Access to education might play a role in increasing ART use amongst people in need of treatment through increasing reliance on the public healthcare system. The association between AIDS symptomatology and medical pluralism should be interpreted with caution, as bi-directionality is likely. Namely, if people using multiple healthcare modalities are less likely to use ART as our final model suggests, they are also more likely to display higher symptomatology due to lack of treatment.
In addition to medical pluralism, older age, higher depression scores, lower anxiety scores and fewer AIDS-related symptoms were weakly associated with lower odds of ART use. Lower depression scores amongst those on ART is in line with previous research, which suggests that patients with depressive symptoms are less likely to obtain CD4 counts after testing for HIV51 as well as that, once on ART, patients experience reductions in depressive symptoms52. Findings of lower ART uptake in older parents reflects South African estimates that ART use declines in 55+ age groups53. Fewer AIDS-related symptoms among ART users is a likely reflection of treatment efficacy.
Anxiety scores generated a positive, albeit very weak association with ART use (95% CI: 1.006, 1.045). Anxiety has been positively associated with greater condom use54, possibly through heightened risk perception55. It is possible to hypothesize that such a mechanism might exist between anxiety and ART uptake, however earlier studies have found a negative association between anxiety and ART adherence56. Further research examining these constructs is required.
Additional research is needed to disentangle causes of the potentially adverse relationship between medical pluralism and ART use, and to inform interventions aimed at increasing ART use. It is also essential to explore whether medical pluralism is associated with time of ART initiation, uptake, dropout, or a combination of these outcomes. Longitudinal research with more robust data (i.e. viral load and ART detection) would more firmly establish associations and causality. Supplementary qualitative data may also elucidate the link between these variables or facilitate the development of new hypotheses57 to explain why medical pluralism is a predictor of non-ART use and help identify areas for intervention.
Results should be interpreted with caution given the cross-sectional nature of the data. While measuring, assessing and controlling for potential covariates sought to minimize bias, other unmeasured variables, such as factors pertaining to quality of care13 may have confounded findings. Our study did not ask participants about reasons for health care seeking behaviors, which could have increased our ability to further explain our findings. Marital status could have confounded our findings by positively affecting men’s and negatively affecting women’s uptake of HIV testing58. However, South African data suggest that while HIV-positive men rely on their partners for social support during illness, women rely on their family members59. We therefore resorted to measuring and controlling for social support instead of marital status. It is also possible that declines in medical pluralism post ART initiation12 influenced the directionality of our findings. Second, all data relied on self-reported measures. Fear of stigma may have hindered reporting of ART use by asymptomatic respondents60. As Verbal Autopsy by definition identifies only symptomatic respondents, we were not able to include in the analysis ART-eligible but asymptomatic respondents unless they reported ART use. Only parents of adolescents were included, possibly compromising generalizability of findings.
Given the historical and current importance of traditional medicine in South Africa and the lack of effective interventions to increase traditional healer referrals to biomedical practice28, these findings call for further research to guide intervention design. As envisaged by South Africa’s Plan for Comprehensive HIV/AIDS Care, Management and Treatment61, effective intersectoral collaboration at community level is urgently needed but such endeavors should be coupled with rigorous process and outcome evaluation. Enhanced communication and psychological support from biomedical practitioners could also help minimize poor outcomes associated with opposing care and treatment.
Acknowledgements
The authors would like to thank the fieldwork teams and the families who welcomed us into their homes. MP led the data analysis and writing. LC conceptualized the study, and contributed to data collection, analysis and writing. MB, ET and MM contributed to data analysis and writing. CK conceptualized the study, managed data collection and contributed to writing. This study was funded by the Economic and Social Research Council (UK), the National Research Foundation (SA), the Health Economics AIDS Research Division (HEARD) at the University of KwaZulu-Natal, the National Department of Social Development (SA), the Claude Leon Foundation and the John Fell Fund. Additional support for CK was made possible by Grant Number K01 MH096646 (PI: Kuo) from the National Institute of Mental Health and Grant Number L30 MH098313 (PI: Kuo) from the National Institutes of Health Division of Loan Repayment. We are also thankful for Rocio Herrero’s and Victor Marin Webb’s Spanish translation of the abstract. MP is grateful for the support from Nevia Pavletic during manuscript preparation. All authors have read and approved this text as submitted to AIDS and Behavior.
REFERENCES
- 1.UNAIDS. Epidemic update and health sector progress towards Universal Access. 2011 [Google Scholar]
- 2.Bor J, Herbst AJ, Newell M-L, Bärnighausen T. Increases in adult life expectancy in rural South Africa: valuing the scale-up of HIV treatment. Science (80-) 2013;339(6122):961–965. doi: 10.1126/science.1230413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reynolds SJ, Makumbic F, Nakigozid G, et al. HIV-1 transmission among HIV-1 discordant couples before and after the introduction of antiretroviral therapy. AIDS. 2012;25(4):473–477. doi: 10.1097/QAD.0b013e3283437c2b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cohen MS, Chen Yq, Hosseinipour MC, et al. Prevention of HIV-1 Infection with Early Antiretroviral Therapy. N Engl J Med. 2011;365(6):493–505. doi: 10.1056/NEJMoa1105243. Available at: http://www.nejm.org/doi/pdf/10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tanser F, B√§rnighausen T, Grapsa E, Zaidi J, Newell M-L. High coverage of ART associated with decline in risk of HIV acquisition in rural KwaZulu-Natal, South Africa. Science (80-) 2013;339(6122):966–971. doi: 10.1126/science.1228160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chigwedere P, Seage GR, Lee T-H, Essex M. Efficacy of antiretroviral drugs in reducing mother-to-child transmission of HIV in Africa: a meta-analysis of published clinical trials. AIDS Res Hum Retroviruses. 2008;24(6):827–837. doi: 10.1089/aid.2007.0291. [DOI] [PubMed] [Google Scholar]
- 7.Suthar AB, Lawn SD, del Amo J, et al. Antiretroviral therapy for prevention of tuberculosis in adults with HIV: a systematic review and meta-analysis. PLoS Med. 2012;9(7):e1001270. doi: 10.1371/journal.pmed.1001270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.D’Adda G, Goldstein M, Zivin JG, Nangami M, Thirumurthy H. ARV Treatment and Time Allocation to Household Tasks: Evidence from Kenya. African Dev Rev. 2009;21(1):180–208. doi: 10.1111/j.1467-8268.2009.00207.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosen S, Larson B, Brennan A, et al. Economic outcomes of patients receiving antiretroviral therapy for HIV/AIDS in South Africa are sustained through three years on treatment. PLoS One. 2010;5(9):1–11. doi: 10.1371/journal.pone.0012731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.WHO. GLOBAL UPDATE ON HIV TREATMENT 2013: RESULTS, IMPACT AND OPPORTUNITIES. Kuala Lumpur, Malaysia: 2013. [Google Scholar]
- 11.Friend-du Preez N, Peltzer K. HIV symptoms and health-related quality of life prior to initiation of HAART in a sample of HIV-positive South Africans. AIDS Behav. 2010;14(6):1437–47. doi: 10.1007/s10461-009-9566-6. [DOI] [PubMed] [Google Scholar]
- 12.Moshabela M, Pronyk P, Williams N, Schneider H, Lurie M. Patterns and implications of medical pluralism among HIV/AIDS patients in rural South Africa. AIDS Behav. 2011;15(4):842–852. doi: 10.1007/s10461-010-9747-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moshabela M, Schneider H, Silal SP, Cleary SM. Factors associated with patterns of plural healthcare utilization among patients taking antiretroviral therapy in rural and urban South Africa: a cross-sectional study. BMC Health Serv Res. 2012;12:182. doi: 10.1186/1472-6963-12-182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peltzer K, Preez NF, Ramlagan S, Fomundam H. Use of traditional complementary and alternative medicine for HIV patients in KwaZulu-Natal, South Africa. BMC Public Health. 2008;8(255) doi: 10.1186/1471-2458-8-255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Muhamadi L, Mbona TN, Kadobera D, Gaetano M, Wabwire-mangen F. Lack of pre-antiretroviral care and competition from traditional healers, crucial risk factors for very late initiation of antiretroviral therapy for HIV - A case-control study from eastern Uganda. PanAfrican Med J. 2011;8(40):1–10. doi: 10.4314/pamj.v8i1.71155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Horwitz RH, Tsai AC, Maling S, et al. No Association Found Between Traditional Healer Use and Delayed Antiretroviral Initiation in Rural Uganda. AIDS Behav. 2013;17(1):260–265. doi: 10.1007/s10461-011-0132-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chi P, Li X. Impact of Parental HIV/AIDS on Children’s Psychological Well-Being: A Systematic Review of Global Literature. AIDS Behav. 2012 doi: 10.1007/s10461-012-0290-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cluver L, Operario D, Lane T, Kganakga M. “I Can’t Go to School and Leave Her in So Much Pain”: Educational Shortfalls Among Adolescent “Young Carers” in the South African AIDS Epidemic. J Adolesc Res. 2011;27(5):581–605. [Google Scholar]
- 19.Cluver L, Orkin M, Moshabela M, Kuo C, Boyes M. The hidden harm of home-based care: pulmonary tuberculosis symptoms among children providing home medical care to HIV/AIDS-affected adults in South Africa. AIDS Care Psychol Socio-medical Asp AIDS/HIV. 2013;25(6):748–755. doi: 10.1080/09540121.2013.772281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brislin RW. Back-translation for cross-cultural research. J Cross Cult Psychol. 1970;1(3):185–216. [Google Scholar]
- 21.Hosegood V, Vanneste A, Timæus IM. Levels and causes of adult mortality in rural South Africa: the impact of AIDS. AIDS. 2004;18:663–671. doi: 10.1097/00002030-200403050-00011. [DOI] [PubMed] [Google Scholar]
- 22.Lopman B, Barnabas RV, Boerma JT, et al. Creating and validating an algorithm to measure AIDS mortality in the adult population using verbal autopsy. PLoS Med. 2006;3(8):e312. doi: 10.1371/journal.pmed.0030312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Doctor HV, Weinreb Aa. Estimation of AIDS adult mortality by verbal autopsy in rural Malawi. AIDS. 2003;17(17):2509–2513. doi: 10.1097/00002030-200311210-00014. [DOI] [PubMed] [Google Scholar]
- 24.Nyamukapa Ca, Gregson S, Lopman B, et al. HIV-associated orphanhood and children’s psychosocial distress: theoretical framework tested with data from Zimbabwe. Am J Public Health. 2008;98(1):133–141. doi: 10.2105/AJPH.2007.116038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lopman B, Cook A, Smith J, et al. Verbal autopsy can consistently measure AIDS mortality: a validation study in Tanzania and Zimbabwe. J Epidemiol Community Health. 2010;64(4):330–334. doi: 10.1136/jech.2008.081554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.The South African Antiretroviral Treatment Guidelines. Republic of South Africa. 2010 Available at: http://www.uj.ac.za/EN/CorporateServices/ioha/Documentation/Documents/ARTGuideline.pdf.
- 27.Steinberg J, et al. Three Letter Plague: A Young Man’s Journey Through a Great Epidemic. London: Vintage; 2008. [Google Scholar]
- 28.Sorsdahl K, Stein DJ, Grimsrud A, et al. Traditional Healers in the Treatment of Common Mental Disorders in South Africa. J Nerv Ment Dis. 2009;197(6):434–441. doi: 10.1097/NMD.0b013e3181a61dbc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Peltzer K, Phaswana-Mafuya N. The symptom experience of people living with HIV and AIDS in the Eastern Cape, South Africa. BMC Health Serv Res. 2008;8:271. doi: 10.1186/1472-6963-8-271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Posse M, Meheus F, van Asten H, van der Ven A, Baltussen R. Barriers to access to antiretroviral treatment in developing countries: a review. Trop Med Int Heal. 2008;13(7):904–913. doi: 10.1111/j.1365-3156.2008.02091.x. [DOI] [PubMed] [Google Scholar]
- 31.Muula AS, Ngulube TJ, Siziya S, et al. Gender distribution of adult patients on highly active antiretroviral therapy (HAART) in Southern Africa: a systematic review. BMC Public Health. 2007;7(63) doi: 10.1186/1471-2458-7-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Turan JM, Nyblade L. HIV-related Stigma as a Barrier to Achievement of Global PMTCT and Maternal Health Goals: A Review of the Evidence. AIDS Behav. 2013:2528–2539. doi: 10.1007/s10461-013-0446-8. [DOI] [PubMed] [Google Scholar]
- 33.Unge C, Ragnarsson A, Ekström AM, et al. AIDS Care: Psychological and Socio-medical Aspects of AIDS / HIV The influence of traditional medicine and religion on discontinuation of ART in an urban informal settlement in Nairobi, Kenya. AIDS Care. 2011;23(7):37–41. doi: 10.1080/09540121.2010.534432. [DOI] [PubMed] [Google Scholar]
- 34.Nachega J, Knowlton A, Deluca A, et al. Treatment Supporter to Improve Adherence to Antiretroviral Therapy in HIV-Infected South African Adults. J Acquir Immune Defic Syndr. 2006;43:127–133. doi: 10.1097/01.qai.0000248349.25630.3d. [DOI] [PubMed] [Google Scholar]
- 35.Leclerc-Madlala S. “We will eat when I get the grant”: negotiating AIDS , poverty and antiretroviral treatment in South Africa. African J AIDS Res. 2006;5(3):249–256. doi: 10.2989/16085900609490386. [DOI] [PubMed] [Google Scholar]
- 36.Simchowitz B. Assessing "Disability” in the Context of ARV Treatment. Cape Town: Republic of South Africa; 2004. [Google Scholar]
- 37.SSA. Census in Brief. Pretoria: 2001. [Google Scholar]
- 38.May J, Carter M, Haddad L, Maluccio J. KwaZulu-Natal income dynamics study (KIDS) 1993-1998: A longitudinal household data set for South African policy analysis. 1999:1993–1998. [Google Scholar]
- 39.Booysen F. Using demographic and health surveys to measure poverty-an application to South Africa. J Stud Econ Econom. 2002;26(3):53–70. [Google Scholar]
- 40.Filmer D, Pritchett LH. Estimating Wealth Effects Without Expenditure Data - Or Tears: An Application to Educational Enrollments in States of India. Demography. 2001;38(1):115–132. doi: 10.1353/dem.2001.0003. [DOI] [PubMed] [Google Scholar]
- 41.Montgomery MR, Gragnolati M, Burke K, Paredes E. Measuring Living Standards with Proxy Variables. Demography. 2000;37(2):155–174. [PubMed] [Google Scholar]
- 42.Myer L, Smit J, Roux L Le, Parker S, Stein DJ, Seedat S. Common mental disorders among HIV-infected individuals in South Africa: prevalence, predictors, and validation of brief psychiatric rating scales. AIDS Patient Care STDS. 2008;22(2):147–158. doi: 10.1089/apc.2007.0102. [DOI] [PubMed] [Google Scholar]
- 43.Hamad R, Fernald LCH, Karlan DS, Zinman J. Social and economic correlates of depressive symptoms and perceived stress in South African adults. J Epidemiol Community Health. 2008;62(6):538–544. doi: 10.1136/jech.2007.066191. [DOI] [PubMed] [Google Scholar]
- 44.Steele GI, Edwards DJA. The development and validation of the Xhosa translations of the Beck Depression Inventory, the Beck Anxiety Inventory, and the Beck Hopelessness Scale. J Psychol Africa. 2008;18(2):217. [Google Scholar]
- 45.Sherbourne CD, Stewart AL, Corporation TR, Street M, Monica S. Ca USA. The MOS Social Support Survey. Soc Sci Med. 1991;32(6):705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 46.Nyblade L, MacQuarrie K. Can we measure HIV/AIDS-related stigma and discrimination? Current knowledge about quantifying stigma in developing countries. 2006 [Google Scholar]
- 47.Tabachnick BG, Fidell LS, Osterlind SJ. Using multivariate statistics. Allyn and Bacon Boston; 2001. [Google Scholar]
- 48.Johnson LF. Access to Antiretroviral Treatment in South Africa: 2004 – 2011. South Afr J HIV Med. 2012 Mar;:22–27. [Google Scholar]
- 49.Lehohla P. Use of health facilities and levels of selected health conditions in South Africa: Findings from the General Household Survey, 2011. Pretoria: 2011. [Google Scholar]
- 50.Abbo C, Ekblad S, Waako P, Okello E, Muhwezi W, Musisi S. Psychological distress and associated factors among the attendees of traditional healing practices in Jinja and Iganga districts, Eastern Uganda: a cross-sectional study. Int J Ment Health Syst. 2008;2(1):16. doi: 10.1186/1752-4458-2-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Susan LR, Janet R, Senica G, et al. Depressive Symptoms and Their Impact on Health-seeking Behaviors in Newly-diagnosed HIV-infected Patients in Durban , South Africa. AIDS Behav. 2012;16:2226–2235. doi: 10.1007/s10461-012-0160-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Judd FK, Cockram AM, Komiti A, Mijch AM, Hoy J, Bell R. Depressive symptoms reduced in individuals with HIV/AIDS treated with highly active antiretroviral therapy: a longitudinal study. Aust N Z J Psychiatry. 2000;34(6):1015–1021. doi: 10.1080/000486700278. [DOI] [PubMed] [Google Scholar]
- 53.Cooke GS, Tanser FC, Bärnighausen TW, Newell M-L. Population uptake of antiretroviral treatment through primary care in rural South Africa. BMC Public Health. 2010;10(585) doi: 10.1186/1471-2458-10-585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kaggwa E, Hindin M. XIX International AIDS Conference: Positive health, dignity, psychological well being, mentalhealth and prevention. Washington DC: 2011. Psychological well being and sexual behaviour among HIV-positive young people: a case study from Uganda; p. 2012. [Google Scholar]
- 55.Tripp G, Tan S, Milne J. Risk Perception and Anxiety. NZ J Psychol. 1995;24(2):37–43. [Google Scholar]
- 56.Campos LN, Guimaraes MDC, Reimen RH. Anxiety and depression symptoms as risk factors for non-adherence to antretroviral therapy in Brazil. AIDS Behav. 2010;14(2):289–299. doi: 10.1007/s10461-008-9435-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fraser MW, Richman JM, Galinsky MJ, Day SH. Intervention Research: Developing Social Programs. New York, New York: Oxford University Press, Inc; 2009. [Google Scholar]
- 58.Kazooba P, Kasamba I, Baisley K, Mayanja BN, Maher D. Access to, uptake of, antiretroviral therapy in a developing country with high HIV prevalence: a population-based cohort study in rural Uganda: 2004–2008. Trop Med Int Heal. 2012;17(8):E49–E57. doi: 10.1111/j.1365-3156.2012.02942.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Schneider H, Govender V, Harris B, Cleary S, Moshabela M, Birch S. Gender differences in experiences of ART services in South Africa: a mixed methods study. Trop Med Int Heal. 2012;17(7):820–826. doi: 10.1111/j.1365-3156.2012.03009.x. [DOI] [PubMed] [Google Scholar]
- 60.Ostrom R, Serovich JM, Lim JY, Mason TL. The role of stigma in reasons for HIV disclosure and nondisclosure to children. AIDS Care. 2006;18(1):60–65. doi: 10.1080/09540120500161769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.RSA. Operational Plan for Comprehensive HIV and AIDS Care, Management and Treatment for South Africa. 2003 [Google Scholar]