Abstract
In perforator flap reconstruction, vascular mapping using preoperative computed tomography (CT) angiography is widely used to confirm the existence and location of an appropriate perforator. This study proposes a rapid, accurate, and convenient method for marking the perforator location on the skin surface. For 12 patients who underwent perforator flap reconstruction between November 2011 and November 2013, metal clips were fixed on the skin surface at the anticipated perforator locations, which were decided using a handheld Doppler. CT angiography was used to compare the location between the metal clip and the actual perforator. The metal clip was moved and repositioned, if needed, on the basis of the CT images. The locations of the appropriate perforator and the metal clip, which were observed during the surgery, were then compared. In CT angiography, the mean distance between the metal clip and the perforator was 3±3.9 mm, and the mean distance that was measured during surgery was 0.8±0.8 mm. In conclusion, we report a simple, rapid, and precise technique to indicate the accurate location of the appropriate perforator on the skin surface.
Keywords: Ultrasonography, Doppler; Multidetector computed tomography; Perforator flap
INTRODUCTION
For the past 20 years, various studies on flap design have been conducted, and interest in perforator-based flaps has increased [1]. The use of a perforator flap allows the preservation of the originating artery and the underlying muscles with good cosmetic results because the flap thickness and color are similar to those of the recipient site. However, appropriate selection and careful dissection are needed for the procedure. Further, it is difficult to harvest the flap, and consequently, the procedure requires a long operation time. To overcome these disadvantages, the precise location of the perforator and its anatomy should be investigated before surgery [2].
Various methods have been used to investigate the location and anatomy of the perforator. The handheld Doppler is convenient and does not cause radiation exposure or side effects that are introduced by the administration of contrast agents; however, this method has been associated with a high false-positive ratio. Computed tomography (CT) angiography is highly accurate and can be used to confirm the preoperative perforator location [1]. However, the location of the perforator on the skin surface is difficult to confirm with CT angiography alone. Thus, accurately identify the perforator's accurate location on the skin surface, clinicians use specific structures such as the umbilicus and coordinates [3,4,5,6]. Other methods which were used by clinicians are the calculation of the distance between the fibula head and the lateral malleolus [7] and the use of CT stereotaxy [8]. These methods require collaboration with radiologists, or a specialized program, which necessitates additional time and effort [3,4,5,6,7,8].
In this study, the anticipated location of the appropriate perforator was investigated using a handheld Doppler. A metal clip was attached to the site before CT angiography was performed to confirm that the perforator was appropriate and determine its location accurately on the skin surface.
IDEA
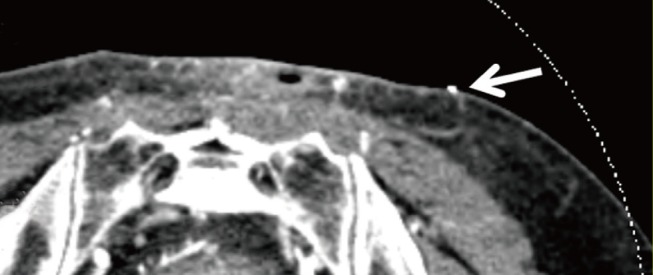
A total of 12 patients who underwent perforator flap reconstruction for soft tissue defects that had occurred between November 2011 and November 2013 were targeted for this study. Two to three points on an anticipated donor site that had the loudest signal using a handheld Doppler were found using a handheld Doppler. If pressing the Doppler probe caused the signal to fade, the location was marked as an anticipated perforator location [6]. Next, 0.5-cm-long metal clips were attached to the marked areas using adhesive film (Fig. 1) before CT angiography.
Fig. 1.

Metal clip marking on anticipated perforator location
SOMATOM Definition 128 ch (Siemens Medical Solutions, Erlangen, Germany) was used for CT angiography under dual source mode conditions, and with the following parameters CARE dose 4D, 80 kV, and 140 kV, 230 effective mAs, rotation time of 0.33, pitch of 0.7, and slice thickness of 5.0 mm. As a contrast agent, 150 mL of iopamidol (Iomeron 400, Braco Imaging Korea, Seoul, Korea) was instilled at a speed of 4 mL/sec, and 100 mL of normal saline was injected before the arterial phase test. The 3-dimensional images were restructured during monitoring with 300 Hounsfield units.
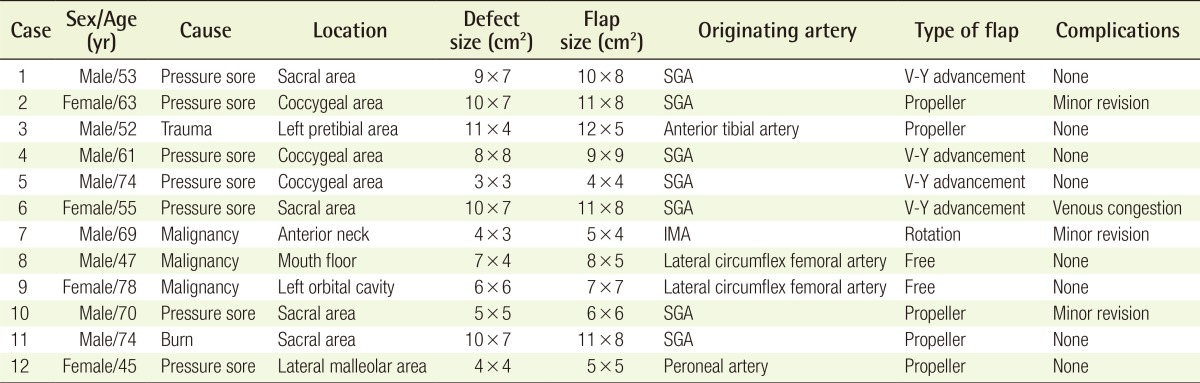
The proper perforator locations were confirmed, and the distance to the nearest metal clip was measured. When the perforator location was not clearly determined because the artifacts caused by the metal clip or other issues were problematic, a commercial software program (Aquarius, TeraRecon Inc., Foster City, CA, USA) was used for clear image of CT scan (Fig. 2). When the distance between the metal clip and the perforator was less than 5 mm, surgery was performed without an additional procedure. However, when the distance was 5 mm or longer, the metal clip was moved and repositioned at the perforator location that had been confirmed through CT angiography before the surgery.
Fig. 2.
Location of the metal clip and the perforator
White arrow indicates the location of the perforator.
The flap was designed and elevated on the basis of the location of the metal clip attached to the surface of the perforator. Dissection proceeded after an incision was made on one side of the flap and was carefully performed to minimize any possible perforator damage. When the perforator location was confirmed in the operative field, at the point of fascial penetration or intermuscular septum, an imaginary vertical line was made on the skin surface. The distance between the metal clip and the imaginary vertical line on the skin surface was compared with the distance between the metal clip and the perforator measured via CT angiography.
The 12 patients ranged from 47 to 78 years of age, with a mean age of 63 years. Reconstruction sites included the sacral area, coccygeal area, pretibial area, and mouth floor. The size of the soft tissue defects ranged from 3×3 cm to 10×7 cm. The perforators used in the reconstruction originated from the superior gluteal artery, anterior tibial artery, or lateral circumflex femoral artery. CT angiography was conducted the day after the metal clip was attached, and no allergic reactions or complications caused by the contrast agent were observed (Table 1).
Table 1.
Patient demographics and clinical results
SGA, superior gluteal artery; IMA, internal mammary artery.
The distance between the metal clip and the proper perforator, which was measured through CT angiography, ranged from 0 to 12 mm, with a mean of 3±3.9 mm. In four cases, a 5 mm or greater distance was observed, and the location of the metal clip was adjusted to the confirmed perforator location before the surgery. The confirmed distance between the perforator and the metal clip in the operative field ranged from 0 to 2 mm, with a mean of 0.8±0.8 mm (Table 2). In all the cases, reliable perforators were confirmed under the metal clips, and consequently, all the flaps were successfully moved. In three cases, minor revisions were performed, and in one case, venous congestion was observed but was relieved by applying leeches. No complications including total flap loss were observed, and the donor site was completely healed.
Table 2.
Distance between the metal clip and the perforator
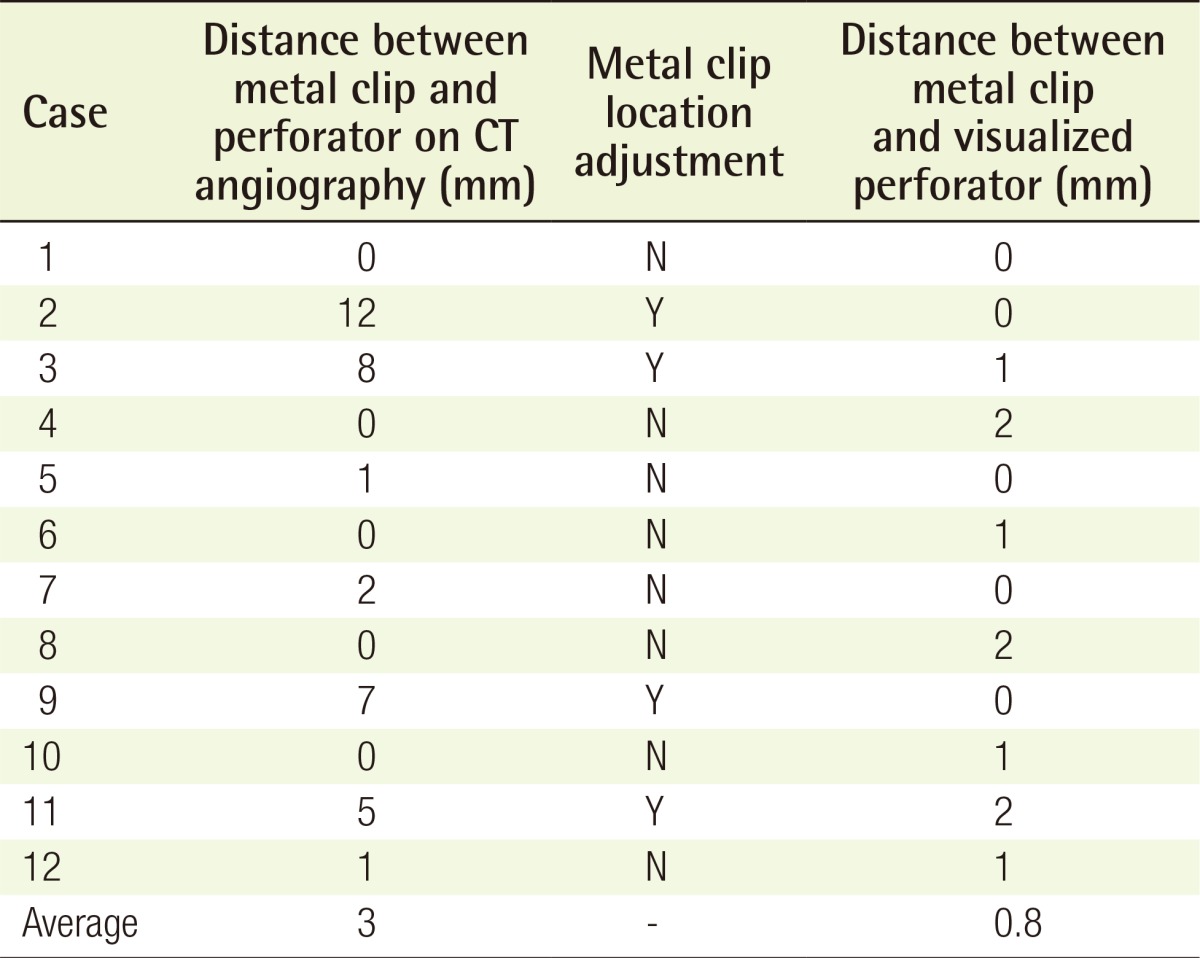
CT, computed tomography.
Case 1
A 74-year-old male patient visited the authors' hospital due to a third-degree burn in his sacral area, which developed while he was sleeping on an electric blanket. Debridement was performed, and as a result, a 10×7 cm defect developed. In the three areas around the defect, the anticipated perforator locations were confirmed using a handheld Doppler, and metal clips were attached before CT angiography. The perforator of the left superior gluteal artery was confirmed at 1 mm medial to the metal clip that was attached to the upper left area. The perforator location that was observed during the surgery completely coincided with the location of the metal clip. Next, a superior-gluteal-artery perforator-based propeller flap was performed. The donor site was primarily closed, and both the flap and the donor sites healed without significant complications (Fig. 3).
Fig. 3.

Case 1: defect on sacral area
(A) The three anticipated sites of the left superior gluteal artery perforators were marked with metal clips by using handheld Doppler. The black arrow indicates the location of the perforator with the loudest handheld Doppler signal. (B) Through the axial view of the three-dimensional computed tomography angiography of the lower extremity, we observed that the metal clip showed concordance with the perforator. The white arrow indicates the location of the perforator with the loudest handheld Doppler signal, which was denoted by black arrow in Fig. 3A. (C) During the surgery, the location of the perforator, which was denoted by the black arrow, was confirmed; it matched the location of the metal clip marking.
Case 2
A 45-year-old female patient visited the authors' hospital due to a pressure sore on her right lateral malleolar area. Metal clips were attached to the three anticipated perforator locations around the defect by using a handheld Doppler a day before the CT angiography. The appropriate perforator location was confirmed at 1 mm inferior to the metal clip by using the CT images. The final defect was as large as 4×4 cm, and a peroneal-artery perforator-based propeller flap reconstruction was performed. The perforator was confirmed during the surgery at a distance of 1 mm from the metal clip. A split-thickness skin graft was performed on the donor site, and both the donor site and the flap healed without significant complications.
Case 3
A 52-year-old male patient visited the authors' hospital due to an 11×4 cm defect in his left pretibial area, which developed after a car accident. Using CT angiography, we found that the appropriate perforator was located 8 mm inferior to the metal clip; therefore, the metal clip was repositioned 8 mm inferiorly before the surgery. The distance between the perforator and the repositioned metal clip was measured as 1 mm during the surgery, and anterior-tibial-artery perforator-based propeller flap reconstruction was performed. A split-thickness skin graft was performed for the donor site, and both the flap and the donor site healed without significant complications (Fig. 4).
Fig. 4.
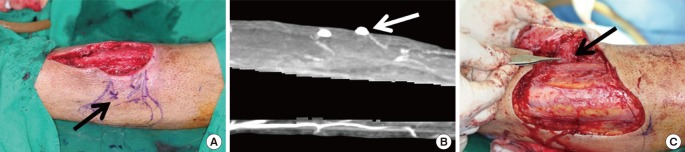
Case 3: defect on pre-tibia
(A) The anticipated sites of the perforator were marked with metal clips by using a handheld Doppler. The black arrow indicates the location of the perforator with the loudest handheld Doppler signal. (B) Three-dimensional computed tomography angiography of the lower extremity showed that the metal clip, which was denoted by a white arrow, was placed 8 mm superior to the perforator location. (C) After the metal clip was adjusted, the perforator location was confirmed to be beneath the metal clip. The black arrow indicates the location of the visualized perforator.
DISCUSSION
This study proposed and confirmed a rapid and accurate method to identify the appropriate perforator location on any skin surface of the body that does not require assistance from radiologists. Accurately locating and quantifying the perforator vessel in perforator flap reconstruction enhances the survival rate of the flap, decreases the development of postoperative complications, shortens the operative time, and reduces preoperative tension [5]. When the perforator location is not confirmed before surgery, the range of flap dissection may increase, which can lengthen the operative time. Moreover, vascular spasm or excessive tension on the perforator may occur during the procedure, and it is difficult to identify the best perforator for the operation [9].
Various tools such as handheld Doppler [1,6,9,10], CT angiography [1,4,5,7,11], magnetic resonance angiography [12], and color duplex ultrasound [13] have been used to understand the preoperative perforator location and structure. Color duplex ultrasound can provide information such as the perforator location and the flow velocity in the vessels. However, it requires a long administration time, and only experienced examiners with knowledge of perforator flap surgery can use this technique. In addition, it is difficult to reproduce due to its real-time dynamics [14]. Magnetic resonance angiography allows less exposure to radiation than CT angiography, but it is expensive, cannot be used for patients with ferrous metal implants, and is less accurate than CT angiography for identifying small perforators [1]. In comparison, the handheld Doppler is mobile, low cost, convenient, and safe from the side effects caused by radiation exposure or the use of contrast agents. However, it detects perforators that may have diameters that are too small for flap reconstruction, and has a high false-positive reaction rate. Frequently used Dop pler probes (8 MHz) are unable to identify vessels that are 20 mm beneath the skin surface or deeper [1,6,15]. CT angiography is non-invasive and highly accurate; it shows the vessel caliber and course in visual detail in addition to structural relationships with the surrounding structures. Therefore, although it exposes the patient to radiation, CT angiography is the most widely used technique, with the handheld Doppler, used to confirm the preoperative perforator [1,2,5,10]. Masia et al. [3] and Clavero et al. [4] suggested the use of the umbilicus as a reference point when marking CT angiography-confirmed perforator locations on the skin surface in breast reconstruction using the deep inferior epigastric perforator flap. A study on fibular osteocutaneous free-flap reconstruction conducted by Chang et al. [7], reported that serial axial images based on the fibular condyle and the lateral malleolus were used to mark the perforator location and were confirmed through CT angiography. In anterolateral thigh-perforator flap reconstruction, Rozen et al. [8] used CT angiography and CT-guided stereotactic navigation to mark the perforator location on the skin surface. In chimeric anterolateral thigh-flap reconstruction, Chiu et al. [11] performed CT angiography and attached four metal clips on both sides of the anterior superior iliac spine and both sides of the superior lateral border of the patella to mount a plastic tube between the clips of each thigh. The tubes were used as guidance markers for the perforator location on the skin surface. All these methods require preoperative collaboration with radiologists or specialized programs, which also necessitates additional time and effort.
In this study, a handheld Doppler and CT angiography were used complementarily. The method suggested in this study allows for marking the perforator location in any part of the body and does not require coordination with radiologists or a specific landmark such as the umbilicus. Moreover, no significant time and effort were needed to determine the perforator location with a handheld Doppler and to attach the metal clip before the CT angiography. In four cases, a discrepancy between the location of the metal clip and the perforator location that was confirmed with CT angiography was observed, but the metal clip was moved and repositioned on the skin surface area on the basis of the CT images. As a result, the perforator was visually confirmed to be positioned just beneath the metal clip in the operative field.
Complementary use of the handheld Doppler and CT angiography allow rapid and convenient perforator identification on the skin surface. The patients underwent the procedure and were very compliant due to the simple, non-invasive, and rapid test features. The perforator flaps were quickly and safely elevated, and the perforators that were not planned preoperatively to be preserved and used were quickly processed through ligation or electrocauterization. This study proposes a convenient method that can be used to rapidly and accurately determine the appropriate perforator location in perforator flap reconstructive surgery.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Smit JM, Klein S, Werker PM. An overview of methods for vascular mapping in the planning of free flaps. J Plast Reconstr Aesthet Surg. 2010;63:e674–e682. doi: 10.1016/j.bjps.2010.06.013. [DOI] [PubMed] [Google Scholar]
- 2.Higueras Sune MC, Lopez Ojeda A, Narvaez Garcia JA, et al. Use of angioscanning in the surgical planning of perforator flaps in the lower extremities. J Plast Reconstr Aesthet Surg. 2011;64:1207–1213. doi: 10.1016/j.bjps.2011.03.015. [DOI] [PubMed] [Google Scholar]
- 3.Masia J, Clavero JA, Larranaga JR, et al. Multidetector-row computed tomography in the planning of abdominal perforator flaps. J Plast Reconstr Aesthet Surg. 2006;59:594–599. doi: 10.1016/j.bjps.2005.10.024. [DOI] [PubMed] [Google Scholar]
- 4.Clavero JA, Masia J, Larranaga J, et al. MDCT in the preoperative planning of abdominal perforator surgery for postmastectomy breast reconstruction. AJR Am J Roentgenol. 2008;191:670–676. doi: 10.2214/AJR.07.2515. [DOI] [PubMed] [Google Scholar]
- 5.Heo CY, Hong KY, Yoon CJ, et al. The value of preoperative multidetector computed tomography for deep inferior epigastric artery perforator free flap. J Korean Soc Plast Reconstr Surg. 2009;36:140–146. [Google Scholar]
- 6.Giunta RE, Geisweid A, Feller AM. The value of preoperative Doppler sonography for planning free perforator flaps. Plast Reconstr Surg. 2000;105:2381–2386. doi: 10.1097/00006534-200006000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Chang TJ, Kim EK, Choi JW. Preoperative identification of perforator using CT angiography in fibular osteocutaneous free flap head and neck reconstruction. Arch Craniofac Surg. 2012;13:41–45. [Google Scholar]
- 8.Rozen WM, Ashton MW, Stella DL, et al. Developments in perforator imaging for the anterolateral thigh flap: CT angiography and CT-guided stereotaxy. Microsurgery. 2008;28:227–232. doi: 10.1002/micr.20485. [DOI] [PubMed] [Google Scholar]
- 9.Blondeel PN, Beyens G, Verhaeghe R, et al. Doppler flowmetry in the planning of perforator flaps. Br J Plast Surg. 1998;51:202–209. doi: 10.1016/s0007-1226(98)80010-6. [DOI] [PubMed] [Google Scholar]
- 10.Little SA, Bruce AS. Osmotic determinants of postlens tear film morphology and hydrogel lens movement. Ophthalmic Physiol Opt. 1995;15:117–124. [PubMed] [Google Scholar]
- 11.Chiu WK, Lin WC, Chen SY, et al. Computed tomography angiography imaging for the chimeric anterolateral thigh flap in reconstruction of full thickness buccal defect. ANZ J Surg. 2011;81:142–147. doi: 10.1111/j.1445-2197.2010.05483.x. [DOI] [PubMed] [Google Scholar]
- 12.Greenspun D, Vasile J, Levine JL, et al. Anatomic imaging of abdominal perforator flaps without ionizing radiation: seeing is believing with magnetic resonance imaging angiography. J Reconstr Microsurg. 2010;26:37–44. doi: 10.1055/s-0029-1220862. [DOI] [PubMed] [Google Scholar]
- 13.Ulatowski L. Colour Doppler assessment of the perforators of anterolateral thigh flap and its usefulness in preoperative planning. Pol Przegl Chir. 2012;84:119–125. doi: 10.2478/v10035-012-0020-5. [DOI] [PubMed] [Google Scholar]
- 14.Smit JM, Dimopoulou A, Liss AG, et al. Preoperative CT angiography reduces surgery time in perforator flap reconstruction. J Plast Reconstr Aesthet Surg. 2009;62:1112–1117. doi: 10.1016/j.bjps.2007.12.090. [DOI] [PubMed] [Google Scholar]
- 15.Alonso-Burgos A, Garcia-Tutor E, Bastarrika G, et al. Preoperative planning of deep inferior epigastric artery perforator flap reconstruction with multislice-CT angiography: imaging findings and initial experience. J Plast Reconstr Aesthet Surg. 2006;59:585–593. doi: 10.1016/j.bjps.2005.12.011. [DOI] [PubMed] [Google Scholar]


