Abstract
Background
An outbreak was reported from a large military station located in South India in 2013. In spite of instituting the preventive measures early, it took more than 2 months to bring the outbreak under control. This paper brings out lessons learnt and suggests strategy for controlling similar outbreak in future.
Method
The Military station comprises of 6 large Regimental Centres and many smaller units. The approximate strength of the serving personnel and their families is 25,000. Besides the unit Regimental Medical Officers, a large tertiary care hospital and a Station Health Organization is available to provide health care.
Result
A total of 266 patients including 192 serving personnel and 74 of their dependents were hospitalized for dengue between 15 May 2013 and 28 Jul 2013. Many dependents not having severe symptoms, were not hospitalized and treated on outpatient basis.
Health advisories and instructions for constituting Dengue Task Force (DTF) were issued well in advance. Preventive measures were instituted early. But the outbreak was controlled only after intervention from higher administrative authorities.
Lessons learnt included correct and timely perception of threat is essential; behavioural change of individuals is desired; availability of adequate health functionaries is mandatory; and complete dataset helps correct perception.
Conclusion
Future strategy for control of dengue outbreak should include repeated and timely survey of entire area for correct risk perception, assessment of behavioural change among individuals; operational research to assess the impact of ongoing public health campaign.
Keywords: Control measures, Dengue outbreak, Future strategy, Lessons learnt, Military station
Introduction
Dengue is the fastest spreading mosquito borne viral disease and is now endemic in over 100 countries.1 In India, number of reported dengue cases have increased by 6 – folds and deaths due to dengue by 2-fold from 2008 to 2013. The most affected states in 2013 were Kerala, Orissa, Karnataka, Gujarat and Tamil Nadu in that order.2 During the year, an outbreak also occurred in a large military station located in South India when more than 200 cases of dengue were reported in a span of 3 months from Jun to Aug 2013. In spite of instituting the preventive measures early, it took more than 2 months to bring the outbreak under control. This paper is an effort to share the challenges we faced in controlling the outbreak, to bring out the lessons learnt during our endeavour and suggest strategy for controlling, if not preventing, a similar outbreak in future.
Material and methods
The Military station located in the heart of the city, is in contiguity with the civil areas on all sides. It is at an altitude of 3092 ft from mean sea level. During rainy season the mean atmospheric temperature varies from 20 °C to 35 °C and relative humidity from 60% to 80%.
The Military Station comprises of 6 large Regimental Training Centres and many smaller units. The approximate strength of the serving personnel and their families is 25,000. Unit Regimental Medical Officers and a large tertiary care hospital located in the station look after the health care needs of the garrison. Station Health Organization (SHO), commanded by a specialist in Community Medicine is also located in the vicinity for monitoring the health activities and rendering technical advice to Commanders regarding prevention of diseases.
Cases of dengue fever have been reported from the station in past also. In the year 2010, 2011 and 2012, only 13, 19 and 36 cases were reported respectively. In 2013, 266 cases of dengue fever were hospitalized between 02 Jun and 06 Oct 2013. This was clearly more than the expected number and hence, was considered an outbreak.
Results
A probable case of dengue was defined as an individual reporting with fever associated with two or more of symptoms like nausea and/or vomiting; rash; aches and pains; positive tourniquet test; leucopenia; and any warning sign including abdominal pain, restlessness, lethargy, bleeding tendencies and hepatomegaly. A confirmed case was defined as a probable case found positive for NS1 Antigen ELISA Test reactive.3
During the outbreak a total of 266 patients including 192 serving personnel and 74 of their dependents were hospitalized. Age wise distribution of these cases is shown in Table 1. Many dependents even found positive on serology but not having severe symptoms, were not hospitalized and treated on outpatient basis. The possibility that some of them did not report to service hospital and went to private practitioner could not be ruled out.
Table 1.
Age wise distribution of dengue fever cases.
| Age group | No. of cases |
Total (%) | |||
|---|---|---|---|---|---|
| Serving pers (%) | Dependents |
||||
| Male | Female | Total (%) | |||
| <5 years | – | 1 | 1 | 2 (02.6) | 2 (00.8) |
| 6–10 years | – | 2 | 5 | 7 (09.5) | 7 (02.6) |
| 11–15 years | – | 6 | 8 | 14 (18.8) | 14 (05.3) |
| 16–20 years | 36 (18.8) | 5 | 7 | 12 (16.2) | 48 (18.0) |
| 21–25 years | 60 (31.3) | 3 | 4 | 7 (09.5) | 67 (25.2) |
| 26–30 years | 19 (09.8) | – | 3 | 3 (04.1) | 22 (08.3) |
| 31–35 years | 27 (14.1) | – | 4 | 4 (05.4) | 31 (11.7) |
| 36–40 years | 24 (12.5) | – | 4 | 4 (05.4) | 28 (10.5) |
| 41–45 years | 20 (10.4) | – | 3 | 3 (04.1) | 23 (08.6) |
| 46–50 years | 4 (02.1) | – | 1 | 1 (01.4) | 5 (01.9) |
| >50 years | 2 (01.0) | 2 | 15 | 17 (23.0) | 19 (07.1) |
| Tota | 192 (100) | 19 | 55 | 74 (100) | 266 (100) |
Fever was present in all cases (100%). Body-ache (69.9%) was the next most common symptom followed by joint pains (51.5%) and headache (49.2%). Retro orbital pain was present in 10.9% and skin rashes in 5.3% cases.
First case of dengue fever was reported on 15 May 2013 which was considered to be a sporadic case and not the cause of current outbreak. Subsequently 4 cases reported from four different locations on 09 Jun 2013, indicating a multi-focal origin, sparked off the outbreak. By 30 Jun 2013, 10 cases of dengue fever were hospitalized which necessitated the need for instituting preventive measures. Number of cases kept on rising till 28 Jul 2013 and thereafter the decline started. Epidemic curve drawn on the basis of date of admission of serving personnel to hospital due to dengue fever is shown in Fig. 1.
Fig. 1.
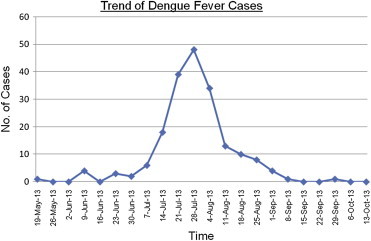
Trend of dengue fever cases.
Health advisories for prevention of dengue were issued well in advance. Dengue Task Force (DTF) teams were constituted at unit levels and members were trained by local SHO in carrying out survey, anti larval activity, elimination of breeding places, focal residual spraying and small scale fogging. Importance of use of mosquito repellants and mosquito nets; and sanitation in peri-domestic area was also explained. In spite of this, occurrence of dengue fever cases continued to be reported from almost all the units. Following death of 3 serving persons, panic was set in and the units resorted to indiscriminate fogging without much result.
Intermittent rain, collection of water in bamboo shoots, roof gutters of older buildings and laxity in garbage clearance due to weather conditions marred the control measures. Ornamental ponds and flower pots with a plate below it, perceived by unit commanders as essential for office and unit area, further compounded the problem.
A high level team including a specialist in Community Medicine and Senior Administrative Authorities visited the station which added impetus to control activity. Working uniform was changed to full sleeve camouflaged dress with immediate effect. Concerted indoor and outdoor fogging was started in the entire station on twice weekly basis. A specialist in Community Medicine, mobilized from another station, was stationed at the unit which reported maximum number of cases. The effort started showing results and a decline in the trend was observed within a week. The outbreak was controlled in about a month's time.
Discussion
From our experience, following lessons can be drawn:-
-
(a)
Correct and timely perception of the threat is essential: In the present case health advisory on prevention of dengue was issued and capsule course for training of DTF was conducted well before the onset of the outbreak. Apparently it was not taken seriously as unit commanders were found wanting in ensuring control measures. Hence, it is essential that likelihood of an outbreak, its perceived severity and availability of resources to control it is communicated and discussed with the administrative authorities well in advance. It is their perception of the situation which will be translated into action subsequently.
-
(b)
Behavioural change of individuals is desired: Adoption of protective behaviour is linked to risk perception. Over the ages, humans have become so used to the presence of mosquitoes in their surrounding that they perceive them as harmless. As a result when cases of mosquito borne diseases like dengue or malaria are reported, the perceived risk is translated in personal protection only. It alone may not be adequate in an outbreak situation. Elimination of all breeding places by maintaining hygienic condition in peri-domestic area and correct garbage disposal is essential for checking the spread of the disease. This is possible only when change in human behaviour is brought out. It can be achieved if the risk perception is correctly communicated to the individuals, health authorities are available to impart correct knowledge and administrative authorities are there to ensure it.
-
(c)
Availability of adequate health functionaries is mandatory: In spite of the commitment of administrative authorities, the present outbreak was controlled only when it was directly supervised by a Specialist in Community Medicine who was mobilized from another station, and health staff of SHO. The health functionaries kept visiting all units round the clock to ensure that control measures were correctly implemented. Hence adequate number of health functionaries in terms of Station Health Officer and his full complement of health staff is a mandatory requirement to tide over such a situation.
-
(d)
Complete dataset helps correct perception: In the present outbreak complete data in respect of serving persons was available which helped in perceiving the threat. However complete data in respect of dependents was not available as many of them were treated on outpatient basis and their record was not maintained. Had it been available, the number of reported dengue fever cases would have been higher and real time threat could have been perceived earlier. Early onslaught could have controlled the outbreak earlier.
Conclusion
In India dengue outbreak gets worse with each passing year. It being a non-notifiable disease, the government continues to rely on data provided by government hospitals because the private sector which caters for almost 80% of healthcare, does not share their data with the government.4 In such a situation, outbreaks similar to the present one will keep occurring.
Various mathematical models for forecasting the outbreaks5 and controlling the outbreaks6 have been developed; vector mapping,7 lethal ovitraps8 and flightless Aedes mosquitoes9 have been tried. But till the time a vaccine is available, the control strategy will continue to focus on curbing the transmission of virus by using combination of chemical and biological targeting of Aedes mosquito and managing the breeding sites.
The future strategy, therefore, for control of dengue outbreak should rely on a public health response beyond routine larviciding or focal spraying.10 It, in our opinion, should include (a) repeated and timely survey of the entire area for correct risk perception; (b) assessment of behavioural change among individuals; (c) operational research to assess the impact of ongoing public health campaign; (d) close interaction between communities and municipal vector control services; and (e) newer research into development of vaccine for dengue.
Conflicts of interest
All authors have none to declare.
References
- 1.WHO. Dengue. Available at: www.who.int/denguecontrol/en/Accessed 1.07.14.
- 2.GOI . National Vector Borne Disease Control Programme, MOHFW; 2014. Dengue Cases and Deaths in the Country Since 2008.www.mohfw.com Available at: cited on 03 Jul 2014. [Google Scholar]
- 3.WHO . New ed. WHO Publications; Geneva: 2009. Dengue: Guidelines for Diagnosis, Treatment, Prevention and Control. [PubMed] [Google Scholar]
- 4.Chaudhuri M. What can India do about dengue fever? BMJ. 2013;346:643. doi: 10.1136/bmj.f643. [DOI] [PubMed] [Google Scholar]
- 5.Descloux E., Mangeas M., Menkes C.E. Climate-based models for understanding and forecasting dengue epidemics. Negl Trop Dis. 2012;6:e147. doi: 10.1371/journal.pntd.0001470. www.plosntds.org Available at: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barmak D.H., Dorso C.O., Otero M., Solari H.G. Modelling interventions during a dengue outbreak. Epidemiol Infect. 2014;142:545–561. doi: 10.1017/S0950268813001301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tilak R., Dutta Gupta K.K., Verma A.K. Vector databank in the Indian armed forces. MJAFI. 2008;64:36–39. doi: 10.1016/S0377-1237(08)80143-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tilak R., Gupta V., Suryam V., Yadav J.D., Dutta Gupta K.K. A laboratory investigation into oviposition responses of Aedes aegypti to some common household substances and water from conspecific larvae. MJAFI. 2005;61:227–229. doi: 10.1016/S0377-1237(05)80159-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mustafa M.S., Bansal A.S., Rastogi V. Flightless Aedes mosquitoes in dengue control. MJAFI. 2011;67:192–193. doi: 10.1016/S0377-1237(11)60035-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arunachalam N., Tana S., Espino F. Eco-bio-social determinants of dengue vector breeding: a multicountry study in urban and periurban Asia. Bull World Health Organ. 2010;88:173–184. doi: 10.2471/BLT.09.067892. [DOI] [PMC free article] [PubMed] [Google Scholar]


