1. Disease characteristics
1.1 Name of the disease (synonyms)
Angelman Syndrome (AS).
1.2 OMIM# of the disease
105830.
1.3 Name of the analysed genes or DNA/chromosome segments
UBE3A/#15q11-q13.
1.4 OMIM# of the gene(s)
601623.
1.5 Mutational spectrum
75% Maternal deletion 15q11–q13.
1–2% Paternal uniparental disomy (upd(15)pat).
3% Imprinting defect.
5–10% Variants in the UBE3A gene.
10–15% Unknown (It is important to exclude differential diagnoses in these cases as there is phenotypic overlap with several other genetic disorders).
Data on this disease (gene variants/phenotype) can be found in the public database Decipher (https://decipher.sanger.ac.uk).
1.6 Analytical methods
The most sensitive approach in diagnosing AS is to study the DNA methylation pattern within the imprinted region 15q11–q13, in particular at the differentially methylated SNURF-SNRPN exon1/promoter region. Normal individuals have an unmethylated paternal allele and a methylated maternal allele. In patients with AS who have a de novo maternal deletion of 15q11–q13, upd(15)pat or an imprinting defect only a paternal unmethylated allele can be detected. Patients with a UBE3A variant have a normal methylation pattern. The most widely adopted methods for methylation analysis are the methylation-specific (MS)-PCR and the MS-MLPA (Multiplex Ligation Dependent Probe Amplification).
MS-PCR can detect methylation changes due to a 15q11–q13 deletion, upd(15)pat and an imprinting defect, but cannot distinguish between these underlying causes. Determination of the underlying cause is not possible. The same is true for other methylation analyses, including PCR following restriction digestion with a methylation-sensitive enzyme, melt-curve analysis and pyrosequencing, but these are rarely used. A follow-up testing that specifically interrogates each of the different types of molecular defects is necessary. This can be done by FISH or DNA microarray analysis to detect 15q11–q13 deletions, or by microsatellite analysis which can distinguish between deletions, upd(15)pat (uniparental inheritance of chromosomes 15) and imprinting defects (biparental inheritance of chromosomes 15).
MS-MLPA has the advantage that it can simultaneously detect changes in copy number and DNA methylation in a semiquantitative manner. Therefore, MS-MLPA can not only detect the presence of a methylation defect due to a 15q11–q13 deletion, a upd(15)pat or an imprinting defect, but it can also distinguish 15q11–q13 and imprinting centre (IC) deletions. Thus, MS-MLPA can determine the molecular defect directly in more than 75% of patients. As the MS-MLPA cannot distinguish between upd(15)pat and a non-IC deletion imprinting defect, further testing by microsatellite analysis is needed.
In patients who have a normal methylation pattern, but clinical features suggestive of AS, a UBE3A screening for variants should be performed.
A more detailed and expanded overview about molecular testing strategies in AS is given in the ‘Best Practice guidelines for the molecular analysis of Prader–Willi and Angelman Syndromes'.1
1.7 Analytical validation
Parallel analysis of positive and negative controls.
1.8 Estimated frequency of the disease (Incidence at birth (‘birth prevalence') or population prevalence. If known to be variable between ethnic groups, please report):
Prevalence at birth: approximately 1:12 000 to 1:20 000.2
1.9 Diagnostic setting

Comment: In AS cases with a 15q11–q13 de novo deletion or upd(15)pat, the recurrence risk is very low if parental chromosomes are normal. In rare cases with a de novo deletion (<1%), a balanced translocation in the mother involving chromosome 15 confers a high recurrence risk and should be excluded by FISH. In rare cases with a upd(15)pat, a Robertsonian translocation in one of the parents could increase the recurrence risk and should be ruled out by cytogenetic analysis. Patients with an imprinting defect have a maternal and a paternal chromosome 15, but the maternal chromosome 15 carries a paternal imprint. The majority of patients with AS and an imprinting defect are sporadic cases without any detectable variants at the DNA sequence level. Imprinting defects of this type usually do not show familial recurrence, and therefore, appear to be associated with a low recurrence risk. However, approximately 10–15% of patients with an imprinting defect have a microdeletion of the chromosome 15 IC. In the majority of these cases, the IC deletion is found to be a familial variant associated with a 50% recurrence risk. If the underlying cause is a maternally inherited UBE3A variant, the recurrence risk is 50% if the mother is a carrier of the variant. In other cases, the IC deletion or the UBE3A variant arises de novo (low recurrence risk) or is a consequence of a germline mosaicism in the mother (increased recurrence risk).3
2. Test characteristics

2.1 Analytical sensitivity (proportion of positive tests if the genotype is present)
Maternal deletion 15q11–q13: nearly 100%.
Paternal uniparental disomy 15: nearly 100%.
Imprinting defect: nearly 100% (low levels of mosaicism might not be detected).
UBE3A variants: nearly 100%.
Chromosomal aberrations: depends on the method used.
2.2 Analytical specificity (proportion of negative tests if the genotype is not present)
Nearly 100%.
2.3 Clinical sensitivity (proportion of positive tests if the disease is present)
The clinical sensitivity can be dependent on variable factors such as age or family history. In such cases a general statement should be given, even if a quantification can only be made case by case.
Nearly 85–90%. In 10–15% of patients with a clinical diagnosis of AS, no deletion, uniparental disomy, an imprinting defect or an UBE3A variant is detected and therefore the molecular defect is unknown.
2.4 Clinical specificity (proportion of negative tests if the disease is not present)
The clinical specificity can be dependent on variable factors such as age or family history. In such cases a general statement should be given, even if a quantification can only be made case by case. Nearly 100%.
2.5 Positive clinical predictive value (life time risk to develop the disease if the test is positive)
The risk to develop the disease if the test is positive is 100%, because all known molecular defects lead to the phenotype.
2.6 Negative clinical predictive value (probability not to develop the disease if the test is negative)
Assume an increased risk based on family history for a non-affected person. Allelic and locus heterogeneity may need to be considered.
Index case in that family had been tested:
If the index case had been tested negative the probability for the non-affected individual not to develop the disease is nearly 100%.
Index case in that family had not been tested:
Can only be clarified through analysis of the non-affected individual.
3. Clinical utility
3.1 (Differential) diagnostics: The tested person is clinically affected
(To be answered if in 1.9 ‘A' was marked)
3.1.1 Can a diagnosis be made other than through a genetic test?
Though the clinical phenotype is characteristic, the significant clinical overlap with the disorders mentioned below means that diagnosis can only be secure when confirmed molecularly.4
Conditions most likely to mimic AS
Pitt–Hopkins syndrome (TCF4)
Christianson syndrome (SLC9A6)
Mowat–Wilson syndrome (ZEB2)
Typical Rett syndrome (MECP2)
Other conditions that can also mimic AS
Prader–Willi syndrome (at <2 years of age)
22q13.3 deletion, Phelan–McDermid syndrome
2q23.1 deletion, MBD5 haploinsufficiency syndrome
17q21.31 deletion, KANSL1 haploinsufficiency (Koolen–de Vries) syndrome
Kleefstra syndrome (9q34.3 deletion, EHMT1 haploinsufficiency)
HERC2 deficiency syndrome
Adenylosuccinase deficiency
FOXG1 haploinsufficiency syndrome
STXBP1 haploinsufficiency syndrome
MECP2 duplication
MEF2C haploinsufficiency syndrome
Alpha-thalassemia/intellectual disability syndrome (ATRX)
3.1.2 Describe the burden of alternative diagnostic methods to the patient
Not applicable.
3.1.3 How is the cost effectiveness of alternative diagnostic methods to be judged?
Not applicable.
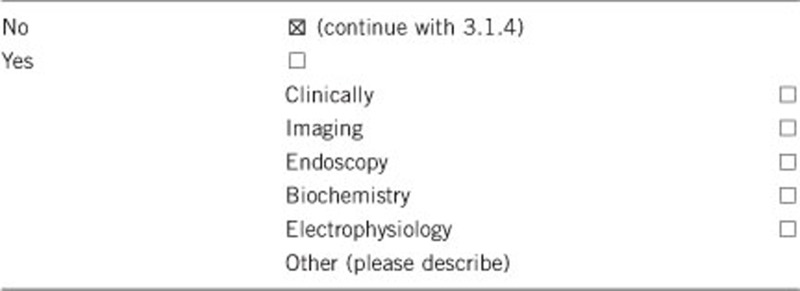
3.1.4 Will disease management be influenced by the result of a genetic test?

3.2 Predictive setting: the tested person is clinically unaffected but carries an increased risk based on family history
(To be answered if in 1.9 ‘B' was marked)
3.2.1 Will the result of a genetic test influence lifestyle and prevention?
If the test result is positive (please describe).
If the test result is negative (please describe).
3.2.2 Which options in view of lifestyle and prevention does a person at-risk have if no genetic test has been done (please describe)?
Not applicable.
3.3 Genetic risk assessment in family members of a diseased person
(To be answered if in 1.9 ‘C' was marked)
3.3.1 Does the result of a genetic test resolve the genetic situation in that family?
Yes. Identification of the precise molecular mechanism underlying AS in an individual case will enable accurate identification of at-risk individuals within the family and facilitate accurate genetic counselling. If a UBE3A variant, an imprinting centre deletion or a translocation involving 15q11–13 is identified, then the mother of the affected case and other family members at risk can be tested to determine the carrier status, although because Angelman Syndrome is an imprinted disorder, these individuals will not be at risk of developing symptoms.
3.3.2 Can a genetic test in the index patient save genetic or other tests in family members?
No.
3.3.3 Does a positive genetic test result in the index patient enable a predictive test in a family member?
Not applicable.
3.4 Prenatal diagnosis
(To be answered if in 1.9 ‘D' was marked)
3.4.1 Does a positive genetic test result in the index patient enable a prenatal diagnosis?
Yes. Testing for a known familial variant can be performed on fetal DNA.
4. If applicable, further consequences of testing
Please assume that the result of a genetic test has no immediate medical consequences. Is there any evidence that a genetic test is nevertheless useful for the patient or his/her relatives? (Please describe).
Parents will finally know the cause of the disease. No need for further diagnostic investigations, particularly those to exclude the syndromes mentioned above. A positive molecular diagnosis may confer eligibility for participation in clinical trials and research studies. Moreover, the testing is important for other family members regarding the recurrence of the disease.
Acknowledgments
This work was supported by EuroGentest2 (Unit 2: ‘Genetic testing as part of health care'), a Coordination Action under FP7 (Grant Agreement Number 261469) and the European Society of Human Genetics. KB, GG-K and BH are supported by the German Ministry of education and sciences BMBF (Network ‘Imprinting Diseases', 01GM1114), GG-K and BH are members of the COST Action BM1208. JC-S's work on diagnostic testing in AS and related disorders is supported by Action Medical Research SP4555.
The authors declare no conflict of interest.
References
- Ramsden SC, Clayton-Smith J, Birch R, Buiting K. Practice guidelines for the molecular analysis of Prader-Willi and Angelman Syndromes. BMC Med Genet. 2010;11:11–70. doi: 10.1186/1471-2350-11-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dagli A, Buiting K, Williams CA. Molecular and clinical aspects of Angelman syndrome. Mol Syndromol. 2012;2:100–112. doi: 10.1159/000328837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buiting K. Prader-Willi syndrome and Angelman syndrome. Am J Med Genet Part C. 2010;154C:365–376. doi: 10.1002/ajmg.c.30273. [DOI] [PubMed] [Google Scholar]
- Tan W-H, Bird LM, Thibert RL, Williams CA. If not Angelman, what is it? A review of Angelman-like syndromes. Am J Med Genet Part A. 2013;9999:1–18. doi: 10.1002/ajmg.a.36416. [DOI] [PubMed] [Google Scholar]


