Abstract
Background
Smart home technologies provide a valuable resource to unobtrusively monitor health and wellness within an older adult population. However, the breadth and density of data available along with aging associated decreases in working memory, prospective memory, spatial cognition, and processing speed can make it challenging to comprehend for older adults. We developed visualizations of smart home health data integrated into a framework of wellness. We evaluated the visualizations through focus groups with older adults and identified recommendations to guide the future development of visualizations.
Materials and Methods
We conducted four focus groups with older adult participants (n=31) at an independent retirement community. Participants were presented with three different visualizations from a wellness pilot study. A qualitative descriptive analysis was conducted to identify thematic content.
Results
We identified three themes related to processing and application of visualizations: (1) values of visualizations for wellness assessment, (2) cognitive processing approaches to visualizations, and (3) integration of health data for visualization. In addition, the focus groups highlighted key design considerations of visualizations important towards supporting decision-making and evaluation assessments within integrated health displays.
Conclusions
Participants found inherent value in having visualizations available to proactively engage with their healthcare provider. Integrating the visualizations into a wellness framework helped reduce the complexity of raw smart home data. There has been limited work on health visualizations from a consumer perspective, in particular for an older adult population. Creating appropriately designed visualizations is valuable towards promoting consumer involvement within the shared decision-making process of care.
Key words: : data display, aged, holistic health, consumer health information
Introduction
Health Visualizations for Older Adults
Older adults (65 years of age or above) face a broad range of health-related issues while striving to maintain healthy independence. Wellness assessment tools can be an effective means towards supporting successful aging.1,2 However, both breadth and density of data are challenges toward creating meaningful representations of complex constructs such as quality of life or wellness. Normal age-associated changes such as reduced visual acuity and slower information processing speeds present unique challenges for the design of older adult-specific visualizations.3–5 In addition, the health information needs of older adults differ from those of healthcare providers (HCPs).6 Representing data to an older adult stakeholder group through appropriately designed visualizations can improve the utility of wellness assessment tools while promoting involvement of older adults as full members of the care team. We addressed the lack of existing consumer-centric visualization approaches for older adults through the design and evaluation of novel representations of wellness from smart home health data.
Dunn's Model of Wellness as a Conceptual Framework
Dunn7 defined wellness as an integrated balance of social, physical, cognitive, and spiritual health. This is consistent with older adults' multidimensional perceptions of successful aging.8 We applied Dunn's conceptual model of wellness to categorize health monitoring data into the four domains of physiological, social, spiritual, and cognitive health. These represent the units of analyses for our visualizations. The aim of this research was not to test the conceptual model for wellness, which has been previously validated, but instead to evaluate and compare data visualization approaches.9,10
Cognitive Processing of Visualizations
To inform the design of visualizations, we examined the existing literature on cognitive design principles. Cognitive theories provide guidelines for developing appropriate visualizations with abstractions that help reduce the cognitive load of extracting information from data. As summarized by Carpenter and Shah,11 there are three primary steps involved in comprehending a visualization: (1) encoding the visual information, (2) relating visual features to concepts, and (3) associating concepts with existing knowledge.
Visual characteristics of the display can influence how effective a viewer can encode graphical information. Cleveland and McGill12 identified six elementary perceptual tasks of visualizations and provided a ranking of these tasks based on accuracy of performance. The tasks ranked from most accurate to least accurate were as follows: position along a common scale, position along a nonaligned scale, length and angle, area, volume, and shading.
Once encoded, the visualization is mapped into conceptual relations such as differences in size, changes in trend, and differences in spatial location.13,14 Pinker15 proposed a set of cognitive operations that are executed when processing a graph to create a mapping (graph schema) that relates visual features to conceptual relations found in the display. Errors in interpretation occur when visual characteristics do not effectively get translated into concepts or relationships.14–16
Existing knowledge impacts the interpretation of visualizations by providing context for conceptual elements.17 Health visualizations designed for older adults are challenging because there is often a gap in domain knowledge. Concepts of spiritual, cognitive, social, and physical health may differ across participants. From a design perspective, this informs the need to articulate the underlying structure of the visualizations and to relate it to familiar existing experiences of participants.
Purpose
We evaluated comprehensive visualization approaches of well-being for older adults. Health monitoring systems can collect an overwhelming amount of data. Visualizing this information provides a meaningful overview of long-term health progress for older adults to use and share for decision-making about their health. We evaluated our visualization designs through focus groups with older adults. The results of our evaluation are part of an iterative design process to guide future visualizations within wellness assessment.
Materials and Methods
Health Monitoring Data
Data for our visualizations came from an 8-week pilot study where commercially available health monitoring technologies were implemented within a community room at a retirement facility in the Seattle, WA, area. The data came from three commercially available sources: (1) a telehealth kiosk system, (2) cognitive assessment software, and (3) a survey collection tool.16,17 Types of data collected included physiological measures such as heart rate and blood pressure, self-reported survey responses of social and spiritual health, and cognitive software assessments. We categorized the data into the four domains of health as defined by Dunn's model of wellness and calculated a normalized score for each domain (ranging from 0 to 100). Data processing is explained in full detail in Thompson et al.18 We extrapolated a hypothetical dataset over 12 months based on these data to serve as the source for our visualizations of longitudinal health.
Design of Health Visualizations
Prior to prototyping, we brainstormed concepts about the features, content, and the look and feel of the visualizations. We created hand sketches of several ideas for each concept and conducted an evaluation session with researchers in gerontological care. Based on our initial sketches, the researchers' feedback, and preferences expressed by community-dwelling older adults in earlier sessions,18,19 we created four design goals for guiding our preliminary data visualization wireframes:
1. Display comparison. From previous research, older adult participants were eager to understand how well they were doing in terms of overall wellness, in comparison with their peers in the community.20,21 The visualization should then provide a juxtaposition of multiple datasets of well-being information to illustrate differences.
2. Display trend. Older adults expressed a need for a view of longitudinal data to detect health trends.22 The visualization should provide a diagram with one parameter of the data represented over time to indicate a trend. Change over time is the most important aspect of these diagrams.
3. Keep it simple. It should only show the data that are necessary and meaningful, so users can absorb the information more easily. The user is not necessarily analytical or scientific, nor are they trained to analyze clinical data. However, if the data appear too simple, they might feel the visualization has been manipulated, or that it is no longer substantial. Maintaining credibility while also maintaining simplicity and clarity is a design challenge.23,24
4. Provide focus. The visualization should provide data points and highlight areas that may require attention. The aim is to prevent the user from dismissing information that is most critical. The system should aid users in processing the information quickly and effectively.
These recommendations provided a common frame of reference for our initial design choices. In addition, we applied cognitive design principles found in the data visualization literature to further guide the visualization development. Empirical studies vary on the overall superiority of one graphical method as opposed to another. Instead, the value of the visualization is impacted by the match between structure and function16; therefore, we included both considerations in the development of early prototype visualizations.
Visual Displays
Based on our initial design recommendations and design principles, we developed three visualization prototypes: (1) the bar graph diagram (Fig. 1), (2) the radial plot (Fig. 2), and (3) the light ball metaphor (Fig. 3).
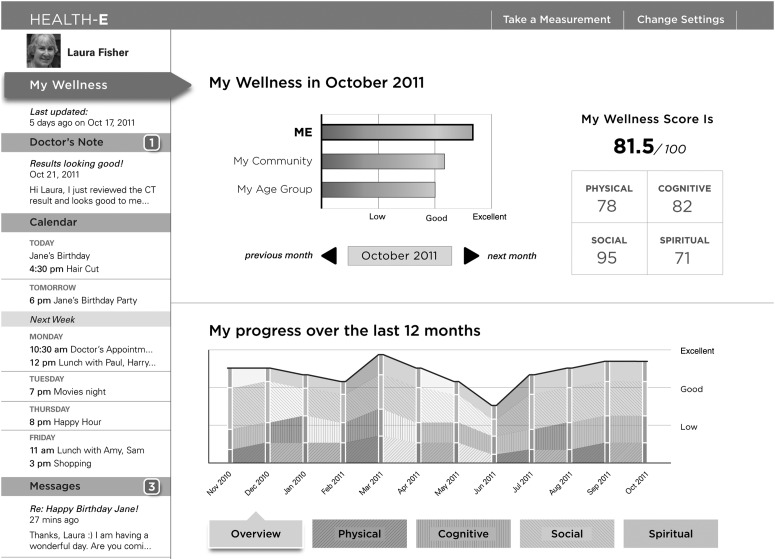
Fig. 1.
Bar graph representation of holistic wellness. Each bar contains components for social, physical, cognitive, and spiritual health while providing both longitudinal views and comparisons with the population.
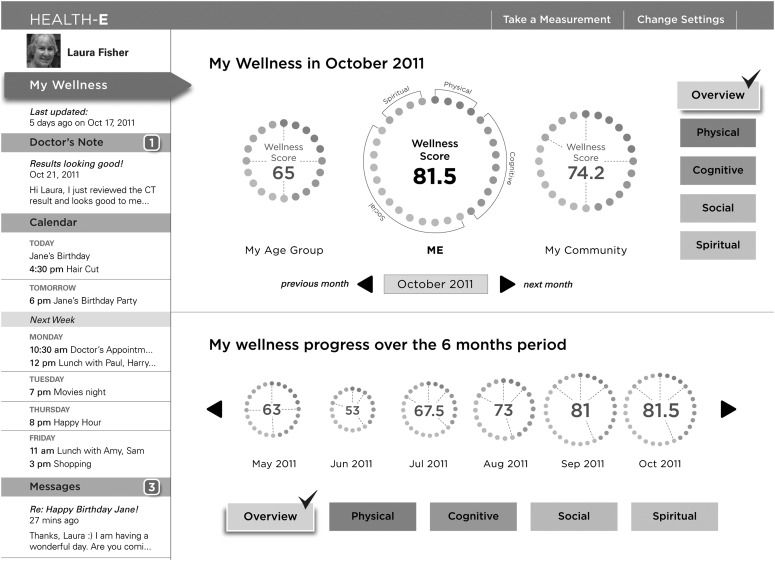
Fig. 2.
Radial plot representation of holistic wellness. Overall radius of the plot represents wellness score. Social, physical, cognitive, and spiritual components of wellness are modeled as colored dots composing the radial plot.
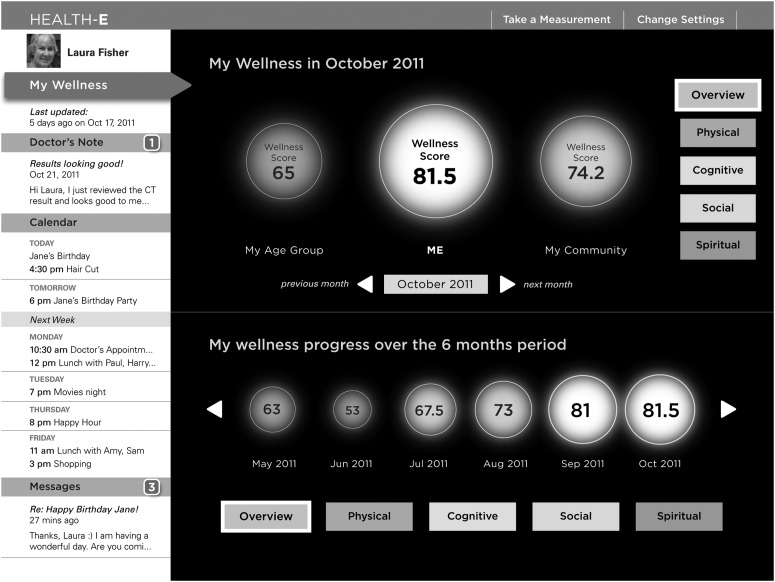
Fig. 3.
A light ball metaphor to represent wellness. Shading and size of the light ball are correlated with overall wellness, whereas individual components are viewed by selecting labeled panes for social, physical, cognitive, and spiritual health as appropriate.
In the bar graph (Fig. 1), each component of health is plotted as part of a stacked bar extended over 12 months for longitudinal trends. Within the stacks are differences in shading to reinforce changes in health components from the prior month. Darker shades represent increased values, whereas lighter shades represent a decline in score.
For the radial plot (Fig. 2), the visualization is composed of individual dots earned as scores for physiological, social, cognitive, and spiritual health. The overall size of the radial visualization reinforces holistic wellness as an aggregate wellness score, whereas individual colored dots emphasize the composition of the wellness score. An individual evenly balanced in wellness would have a radial plot split into equal quadrants for the four components of health.
The light ball metaphor (Fig. 3) reflects changes in brightness with differences in score. For a given wellness score, the metaphor changes in both size and brightness as scores increase. We selected this visualization as a metaphoric display of accomplishment with a positive glow for high scores, reinforced with size of the ball as a visual cue.
Focus Group Setting and Participants
We conducted four 60-min focus groups of between seven and nine participants each (22 females, 8 males) at an independent retirement community in Seattle. Focus groups are a valuable qualitative method for eliciting feedback during the early design process through moderated discussion. The retirement community consists of older adults at least 62 years old residing in both private apartments and assisted living homes. We restricted participants to older adult members of the retirement community who were independent in activities of daily living, fluent in English, and willing to participate through informed consent. The University of Washington Institutional Review Board approved all study procedures.
Data Collection
The research team developed and pilot-tested a protocol script to guide the facilitation of the focus groups. The focus groups examined questions related to interpretability of the visualizations and cognitive processes involved in evaluating them. We placed a focus on the processes involved with visualization as opposed to a quantification of the data. For example, the protocol addressed how the use of gradients, colors, or metaphors may impact a participant's ability to interpret the data. We also asked participants questions related to the application of different visualizations as support for wellness assessment. These included questions such as: How might participants apply these visualizations? How do participants use visualizations to identify longitudinal trends? How might visualizations support sharing of health information? What components of the visualization supported understanding of information?
Qualitative Analysis
We transcribed the focus groups verbatim. Analysis involved an initial review of the focus group transcripts and consensus development of a preliminary codebook. Two researchers independently coded content within the focus groups using the codebook. The researchers then compared and reconciled coded content while refining the codebook as necessary before being applied to the next transcript.25–27 This double coding helped ensure inter-rater reliability and the iterative development of a codebook allowed for flexibility in analyzing content. We conducted a content analysis from the coded focus groups, extracting themes related to information needs and design recommendations of the visualizations.25 The findings were presented as qualitative description of the themes.28,29
Results
Visualization Evaluation
From our qualitative descriptive analysis, we identified three themes related to the processing and application of visualizations:
1. Values of visualizations for wellness assessment. Older adults highlighted the potential applications of the visualizations, both for wellness assessment and for the promotion of shared decision-making between patient and provider. As one older adult described, this could serve as a “graphic diary” to track health information. Older adults also recognized the limited availability of HCPs to remain informed about a patient's health status:
Six months or sometimes I go often, sometimes I don't go for quite a while. In between, anything can happen and he [physician] wouldn't know about it. And sometimes you can't verbalize these problems, raise them.
Due to the interval between visits with a HCP, there exists a gap in knowledge and older adults are challenged with recalling and summarizing their perception of their wellness trajectory during that time. Integrated health visualizations help bridge this gap by providing a common frame of reference for discussions with HCPs. Although visualizations allowed the individual to track health, participants did have caveats. Longitudinal health tracking was valued if participants could identify interventions to impact the trajectories identified within the display:
If we could have some effect on it ourselves, like if it indicated that something you were doing or not doing was causing a drop or rise, we could act appropriately or we could consult a health care provider who takes care of that.
2. Cognitive evaluation of visualizations. Older adults applied a high-level approach toward processing visual information by focusing on holistic scores of wellness first and then, if necessary, examining components of wellness: “I look at the highs and lows. I actually look at the high, when it was, March. And then I look at the lows, it's June. I'm trying to figure out in my own mind why there is a difference.” In contrast, HCPs are often more concerned with fine-grained data for diagnostic purposes.6,30
Older adults highlighted the challenge of representing complex information within the focus groups. Participants felt that too much information was presented within the visualization and were uncertain on what what elements of the visualization to focus. Abstractions of data led to further confusion for participants. This applied primarily to the radial plot (Fig. 2) and light ball metaphor (Fig. 3). For example, one participant stated:
It's hard to imagine what the dots really represent in terms of what was your base? Why do I have four physical dots in the center and eight of the cognitive? What went into that? It seems arbitrary. Of course it represents some measurement, but I think it's hard to feel specific about it. [The radial plot] is sort of a looser, quicker, look at your condition.
Both brightness and size of the visualizations were visual cues intended to reinforce wellness score; however, they either created confusion or were ignored completely. Even within the traditional bar plot visualization (Fig. 1), participants found the subtle shading of the bars, a visual cue for slope, difficult to discern: “So now I have to worry about colors and shades of colors…I prefer something much simpler.”
3. Integration of health data for visualization. Participants identified with the conceptual framework of wellness consisting of different domains of health. They emphasized the importance of this segregation of wellness components within their personal experiences, noting that combining different components of health into an average score was an incongruent comparison: “putting together apples and oranges,” “it doesn't make sense,” and “each category has to stand on its own.” In particular, the weights of each component of wellness may not be equal; some participants had limited interest in spiritual wellness or had greater interest in social wellness. Allowing consumers to customize weights of these components would improve value of the visualizations.
Design Recommendations
We provide a summary of design recommendations (Table 1). The bar plot (Fig. 1) was well received by participants. Older adults were quick to comprehend the data presented, partially becasue of the familiarity with the display method: “We've all had a lot more experience or exposure to bar graphs and line graphs. They do immediately tell us something.” The aligned scale along the x-axis made it easier to compare overall wellness in time, while the slopes allowed for detection of changes in wellness. However, participants found the shaded gradient within the displays confusing, creating an additional dimension of analysis that was too subtle and ineffective.
Table 1.
Summary of Specific Feedback and Design Recommendations for Each of the Three Health Visualizations
| POSITIVE FEEDBACK | NEGATIVE FEEDBACK | RECOMMENDATIONS | |
|---|---|---|---|
| Bar plot (Fig. 1) | • Familiar self-contained visualization • Provides for quick longitudinal comparisons • Allows for component comparisons |
• Low, good, excellent ratings have no context. • Color gradient for group comparisons creates confusion. • Shadings for longitudinal display are too subtle. |
• Remove color gradient from low to excellent • Separate holistic wellness graphs into components • Use solid color as opposed to shades |
| Radial plot (Fig. 2) | • Explicit colors as opposed to gradual shadings • Numbered wellness scores allow for direct comparisons |
• Dots are difficult to count. • Colors are difficult to contrast. • Shapes are perceived as distracting. |
• Individual wellness components • Connect dots for a solid ring |
| Light ball metaphor (Fig. 3) | • Brightness difference amplifies large changes. • Simplification of information • Accommodates color blindness |
• Can only view one wellness component at a time • Dark background creates an ominous tone. |
• Use an alternative colored background • Increase sharpness for comparisons |
Older adults found that the colored dots of the radial plot (Fig. 2) lacked clarity for comparisons: “…these various size circles and very small dots are too numerous for us to want to bother with. I mean I can only think of coinage and one is for Japan and one is for Germany and one is for Great Britain. It doesn't make sense for personal use.” The visualization was also difficult to compare longitudinally, requiring an added cognitive load to count the dots, reference the key, and compare from one radial plot to the next. Instead, one participant described his process of analysis as: “I would ignore it [size and composition] and look for the numbers because the two middle buttons are the same and yeah they're a little bit bigger but I wouldn't use them as a difference between the two.”
The light ball metaphor (Fig. 3) had mixed responses throughout the focus groups. Older adults found the display simple, while also contrasting sharply against the dark background. However, participants often disregarded differences in size and shading of the light ball. These differences were too difficult to distinguish unless drastic changes in score occurred. An unanticipated consequence of this visualization was its negative association with mood due to its ominous background. Participants suggested keeping the existing light ball metaphor concept, however, with brighter colors similar to the bar and radial visualizations.
Limitations
Participants may interact with paper interfaces differently than an on-screen display; this was commented on by those who noted the contrast between the static display and presence of icons within the visualization. We also conducted focus group evaluations at a single retirement community; greater generalizability of results may apply if we had participants in a broader spectrum of health literacy. We did not explicitly ask participants demographic information such as age, education, or socioeconomic status. The construct of wellness was integrated into a single score as an average of the four components of social, spiritual, cognitive, and physiological health. Participants expressed some reservations about this approach; an alternative for the design would be to allow for customizable weights for each component of wellness.
Discussion
Visualization Needs of Older Adults
Our evaluation of early visualization prototypes highlight key needs expressed by older adults. The visual representation of complex multidimensional constructs like quality of life or wellness should be clear and easy to understand; this component is often lost when designing visualizations for wellness assessments with a clinical focus. We found that visual cues should be used in moderation. Having multiple cues to reinforce a visual trend detracts from, rather than reinforces, cognitive efficiency. Participants expressed confusion with multiple visual cues and in some instances chose to ignore them completely.
Carpenter and Shah11 proposed a mixed interaction of both bottom-up processing and top-down processing involved in graph comprehension. Bottom-up processing involves integrating visual chunks from a graph for comprehension, whereas top-down processing involves existing experiential knowledge for interpretation.11 Both elements were observed during our focus group evaluations. A top-down approach contributed to preferences for the bar plot display (Fig. 1), as participants cited familiarity and experience with the visualization. Bottom-up processes were described by participants who used the visual displays to quickly identify longitudinal trends such as drops in holistic wellness. Understanding theoretical principles behind graph comprehension allows us to design better visualizations as part of further iterations. It can also highlight where errors occur from cognition to comprehension.
Conceptually, older adults found the visualizations valuable as a resource to stimulate discussion with HCPs. There was personal interest in using the visualizations to monitor long-term health trends, in particular, identifying changes that were gradual and not otherwise observable day-to-day. The framework of wellness was favorably received as older adults agreed that wellness is a multidimensional concept. However, a personal level of customization was also requested given that individuals place different weights on social, spiritual, cognitive, and physiological wellness.
Conclusions
Older adults are often faced with difficult decisions without full access to all relevant information.31,32 According to Prahalad and Ramaswamy,33 providing clinical information in an accessible manner allows patients to have a personalized understanding of risk-benefits to support decision-making. Our evaluation of three different approaches to synthesize and display wellness identified specific visualization needs of older adults and provides recommendations to inform the design of consumer-centric visualizations.
Acknowledgments
This work was supported in part by National Library of Medicine training grant T15LM007442 and National Institute of Nursing Research training grant T32NR007106.
Disclosure Statement
No competing financial interests exist.
References
- 1.Mynatt ED, Melenhorst AS, Fisk AD, Rogers WA. Aware technologies for aging in place: understanding user needs and attitudes. IEEE Pervas Comput 2004;3:36–41 [Google Scholar]
- 2.Hendriks MRC, et al. Cost-effectiveness of a multidisciplinary fall prevention program in community-dwelling elderly people: A randomized controlled trial (ISRCTN 64716113). Int J Technol Assess Health Care 2008;24:193–202 [DOI] [PubMed] [Google Scholar]
- 3.Salthouse TA, Hancock HE, Meinz EJ, Hambrick DZ. Interrelations of age, visual acuity, and cognitive functioning. J Gerontol B Psychol Sci Soc Sci 1996;51:317–330 [DOI] [PubMed] [Google Scholar]
- 4.Strayer DL, Wickens CD, Braune R. Adult age differences in the speed and capacity of information processing: 2. An electrophysiological approach. Psychol Aging 1997;2:99–110 [DOI] [PubMed] [Google Scholar]
- 5.John DR, Cole CA. Age differences in information processing: Understanding deficits in young and elderly consumers. J Consumer Res 1986;13:297–315 [Google Scholar]
- 6.Reeder B, Le T, Thompson HJ, Demiris G. Comparing information needs of health care providers and older adults: Findings from a wellness study. Stud Health Technol Inform 2013;192:18–22 [PMC free article] [PubMed] [Google Scholar]
- 7.Dunn HL. High-level wellness for man and society. Am J Public Health Nations Health 1959;49:786–792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Phelan EA, Anderson LA, Lacroix AZ, Larson EB. Older adults' views of ‘successful aging’—How do they compare with researchers' definitions? J Am Geriatr Soc 2004;52:211–216 [DOI] [PubMed] [Google Scholar]
- 9.Greenberg JS. Health and wellness: A conceptual differentiation. J School Health 1985;55:403–406 [DOI] [PubMed] [Google Scholar]
- 10.Walker SN, Sechrist KR, Pender NJ. The Health-Promoting Lifestyle Profile: Development and psychometric characteristics. Nurs Res 1987;36:76–81 [PubMed] [Google Scholar]
- 11.Carpenter PA, Shah P. A model of the perceptual and conceptual processes in graph comprehension. J Exp Psychol Appl 1998;4:75–100 [Google Scholar]
- 12.Cleveland WS, McGill R. Graphical perception: Theory, experimentation, and application to the development of graphical methods. J Am Stat Assoc 1984;79:531–554 [Google Scholar]
- 13.Bertin J. Graphics and graphic information-processing. Berlin: Walter de Gruyter, 1981 [Google Scholar]
- 14.Kosslyn SM. Understanding charts and graphs. Appl Cogn Psychol 1989;3:185–225 [Google Scholar]
- 15.Pinker S. Artificial intelligence and the future of testing. Mahwah, NJ; Lawrence Erlbaum Associates, 1990 [Google Scholar]
- 16.Larkin JH, Simon HA. Why a diagram is (sometimes) worth ten thousand words. Cogn Sci 1987;11:65–100 [Google Scholar]
- 17.Bertin J. Semiology of graphics: Diagrams, networks, maps. Redlands, CA: ESRI Press, 2010 [Google Scholar]
- 18.Thompson HJ, Demiris G, Rue T, Shatil E, Wilamowska K, Zaslavsky O, Reeder B. A holistic approach to assess older adults' wellness using e-health technologies. Telemed J E Health 2011;17:794–800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Demiris G, Thompson HJ, Reeder B, Wilamowska K, Zaslavsky O. Using informatics to capture older adults' wellness. Int J Med Inform 2013;82:e232–e241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Black K, Dobbs D, Young TL. Aging in community mobilizing a new paradigm of older adults as a core social resource. J Appl Gerontol 2012. November 20 [Epub before print]. doi: 10.1177/0733464812463984 [DOI] [PubMed] [Google Scholar]
- 21.Johnson RJ, Wolinsky FD. The structure of health status among older adults: Disease, disability, functional limitation, and perceived health. J Health Soc Behav 1993;34:105–121 [PubMed] [Google Scholar]
- 22.Demiris G, Thompson HJ, Boquet J, Le T, Chung J. Older adults' acceptance of a community-based telehealth wellness system. Inform Health Soc Care 2013;38;27–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Friedman B. Value-sensitive design. Interactions 1996;3:16–23 [Google Scholar]
- 24.Van der Hoven J, Manders-Huits N. A companion to the philosophy of technology. Malden, MA: Wiley-Blackwell, 2009 [Google Scholar]
- 25.Boyatzis RE. Transforming qualitative information: Thematic analysis and code development. Thousand Oaks, CA: Sage Publications, 1998 [Google Scholar]
- 26.Miles MB, Huberman AM. Qualitative data analysis: An expanded sourcebook. Thousand Oaks, CA: Sage Publications, 1994 [Google Scholar]
- 27.Krippendorff K. Content analysis: An introduction to its methodology. Thousand Oaks, CA: Sage Publications, 2003 [Google Scholar]
- 28.Sandelowski M. What's in a name? Qualitative description revisited. Res Nurs Health 2010;33:77–84 [DOI] [PubMed] [Google Scholar]
- 29.Sandelowski M. Whatever happened to qualitative description? Res Nurs Health 2000;23:334–340 [DOI] [PubMed] [Google Scholar]
- 30.Le T, Reeder B, Thompson HJ, Demiris G. Health providers' perceptions of novel approaches to visualizing integrated health information. Methods Inf Med 2013;52:250–258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Selwyn N, Gorard S, Furlong J, Madden L. Older adults' use of information and communications technology in everyday life. Ageing Soc 2003;23:561–582 [Google Scholar]
- 32.Reference Point Foundation A national assessment of consumer health information demand and delivery. 1995. Available at http://odphp.dhhs.gov/harris.htm (last accessed November7, 2014)
- 33.Prahalad CK, Ramaswamy V. Co-creation experiences: The next practice in value creation. J Interact Market 2004;18:5–14 [Google Scholar]