Abstract
This study examined the efficacy of an enhanced intervention to reduce sexual risk of HIV/STI and harmful alcohol use among female sex workers in Mongolia. Women (n = 166) were recruited and randomized to either (1) a relationship-based HIV sexual risk reduction intervention; (2) the same sexual risk reduction intervention plus motivational interviewing; or (3) a control condition focused on wellness promotion. At three and six month follow-up, both treatment interventions and the wellness promotion condition were effective in reducing the percentage and the number of unprotected acts of vaginal sex with paying partners in the past 90 days. All three conditions demonstrated efficacy in reducing harmful alcohol use. No significant differences in effects were observed between conditions. Findings suggest that even low impact behavioral interventions can achieve considerable reductions of HIV/STI risk and harmful alcohol use with a highly vulnerable population in a low resourced setting.
Keywords: HIV, Prevention, Sex work, Alcohol, Mongolia
Introduction
Mongolia is a country well-positioned to prevent an HIV epidemic by strategic and rapid implementation of effective prevention programs. Centrally located in Asia, the country has low reported HIV prevalence. However, Mongolia is bordered by Russia and China, two countries experiencing rapidly expanding HIV epidemics, and is experiencing a constellation of structural factors that, without rapid prevention program deployment, may fuel growth of a local epidemic [1]. These factors are a result of a slow and challenging economic transition since 1990, from a centrally planned (Soviet-supported) to a free market economy that has left over 32% of the population living below the poverty line [1, 2]. Factors include increased survival sex work among women, increased alcoholism among men and women, increased homelessness, increased migration of workers through the country, and a deteriorating health and social services system [2–4]. Increased sex work and migration of workers—particularly in the presence of high rates of sexually transmitted infections (STIs)—has been associated with growing HIV epidemics across geographic boundaries on other continents [5–8]. Concurrent with these escalating opportunities for risky heterosexual behaviors are increasing rates of STIs. As the most prevalent type of communicable disease in Mongolia [1], STI rates are as high in the general population [9], as they are among samples of sex workers and STI patients [3, 4, 10–12]. There is evidence that sexual risk for HIV and other STIs increases under the influence of alcohol [13, 14], and that unprotected sexual contact in the presence of STIs enhances the probability of HIV transmission [15]. Currently, the 62 reported HIV cases (of an estimated 376 cases) remain clustered within high-risk groups, with 50% of all reported female cases detected among female sex workers (FSWs), the male partners of whom are a key bridge population [1].
Women who engage in sex work are at especially high risk of HIV infection [16–18]. Studies highlight the multiple adverse social and environmental contexts contributing to HIV risk among sex workers, including poverty, violence, addiction [17, 19–25], multiple life traumas such as childhood abuse and partner violence, and severe physical and emotional health-related problems [21, 23, 26–29]. Sex workers face unique circumstances that exacerbate the challenge of negotiating protected sex such as receiving higher payment from clients to forgo condom use and establishing feelings of trust with regular paying partners [25, 30]. Moreover, economic, social, and gender inequalities make it difficult for all women, not just sex workers, to persuade partners to use male condoms [31–33].
Alcohol use is another factor associated with risky sexual behaviors, including inconsistent condom use and a greater number of partners [34–36]. Alcohol use in Mongolia is high among the general population. A 2009 study found 39% of men and 5% of women use alcohol at harmful levels [37]. There is limited research on alcohol use in the context of commercial sex. Some studies have found an association between higher HIV/STI rates and alcohol use among sex workers [21, 22, 36, 38, 39]. As many as 60% of Mongolian sex workers reported alcohol abuse as a primary reason for non-condom use with paying partners [2, 4].
The introduction, testing and implementation of behavioral, evidence-based programs to reduce sexual risk and alcohol use among female sex workers before HIV rates increase could be very effective in preventing a Mongolian HIV epidemic [31]. The purpose of this study was to examine the efficacy of a combined sexual risk reduction and motivational interviewing intervention on reducing sexual risk among alcohol dependent women who exchange sex for money or goods in Mongolia. Outcomes were examined at 2-week post test (PT), as well as three and six months post intervention. A secondary purpose was to examine and enhance the feasibility (recruitment, attendance, retention) for a future, larger clinical trial with a larger sample size and longer term follow-up.
Methods
Participants
This study was conducted between 2007 and 2009. Data for this sample were collected from women participating in services at the National AIDS Foundation (NAF) in Ulaanbaatar, Mongolia. Founded in 2000, NAF is the central distribution source for education and training in HIV/STI risk reduction information. NAF also provides limited HIV/AIDS prevention programming for high-risk groups, including sex workers. A total of 270 women were recruited and screened. Of those, 229 (85%) were considered eligible for the study. Women were eligible for the study if they (1) were at least 18 years of age; (2) were currently enrolled in the NAF program; (3) reported having engaged in vaginal or anal sexual intercourse in the 90 days prior to screening in exchange for money, alcohol, or other goods; (4) reported having engaged in unprotected vaginal or anal sexual intercourse in the 90 days prior to screening with a paying sexual partner; and (5) met criteria for harmful alcohol use in the past year [score of eight or above on the Alcohol Use Disorders Identification Test (AUDIT)] [40]. Participants would have been excluded if assessed to have a severe cognitive or psychiatric impairment that would interfere with the ability to provide informed consent or complete study instruments. No women were excluded.
Design
All participants completed a computer-based, interviewer-administered baseline assessment. Assessments were conducted in a private space in the study office at the NAF building. After completing the assessment, women were invited to attend the next group initiation session (held within two to four weeks of the baseline date). Intervention groups were closed groups, so if a woman missed the next group start date, she was then invited to the subsequent new group startup date. The average time from baseline to intervention was 14 days (range 1–45).
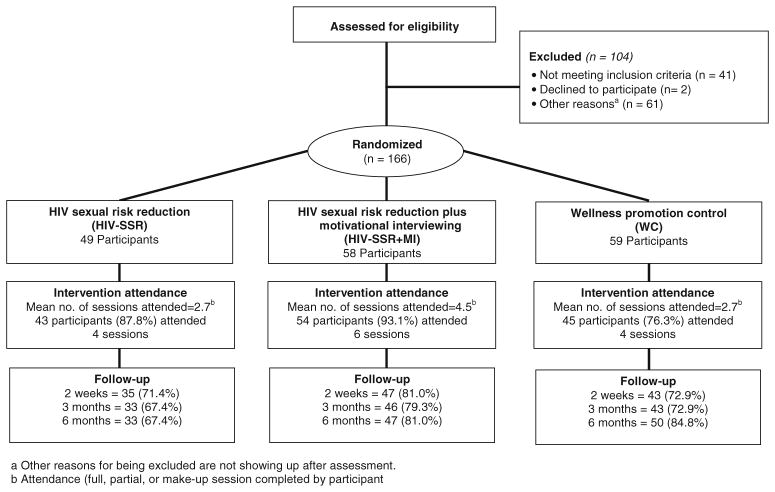
Randomizing by group was more efficient than attempting to accrue enough women in a short enough period of time to then randomize individually to three conditions at one time. For this reason, the study followed a cluster or group randomization schema. A random number generator was used to randomly assign a new group of participants to: (1) the treatment condition (HIV-SSR), four weekly relationship-based sessions on knowledge and skills related to HIV/STI risk reduction; (2) the enhanced treatment condition (HIV-SSR+MI), the same four weekly sessions as in the treatment condition plus two wrap-around sessions engaging motivational interviewing; or (3) the wellness promotion control condition (WP-C), four weekly sessions on overall health and wellness knowledge and skills (see Fig. 1). The generator sought to balance group assignments evenly across a total estimated number of groups needed to provide treatment to all participants.
Fig. 1.
Overview of Intervention Study
All women were considered randomized, and therefore (based on an intention to treat approach) were considered part of the study. For the first two groups, the PI disclosed the group condition to the study team so that they could prepare for the session ahead of time. As in many HIV prevention trials where time passes between randomization and the first session, this strategy yielded considerable attrition, which could have potentially biased the treatment effect estimates. For this reason, the team shifted the strategy to assigning the randomized condition to the participant at the time of participant’s arrival at their first session. The attrition that occurred for those two groups (25% from randomization to first group date) is consistent with attrition that occurs in other HIV prevention interventions studies, even with populations that are not as vulnerable [42, 46]. All women were asked to return for follow-up post test assessments, held at 2 weeks after the final session and then again at 3 and 6 months after their final session. All assessment staff was blinded to participant intervention assignment. Recruitment took place between March of 2008 and January 2009. Follow-up assessment was conducted from April 2008 until October of 2009.
Assessment
The assessment interview was designed to elicit self-reported data. Measures were translated into Mongolian from English and then back translated for accuracy. The baseline assessment was then pilot tested with seven NAF and research project staff, and determined to have adequate face validity. Trained interviewers administered the tool, which included sociodemographic characteristics, HIV/STI risk behaviors, and alcohol use variables.
Sociodemographic variables included: age, race/ethnicity, education, employment status, income, marital status, having a trust partner (defined as an intimate partner other than a paying partner, may include a spouse, boyfriend, lover), current housing situation, and whether exchanging sex for money was the primary source of income.
Using an adaptation of the Timeline Follow-back [41], participants provided self-reported data on the proportion and number of times they engaged in unprotected vaginal and anal sex with paying partners and with trust partners in the 90 days prior to three and six month post intervention assessments. The proportion of unprotected sex was calculated as the total number of sex acts minus the number of sex acts reported where a condom was used and then divided by the total number of sex acts. The number of times engaged in unprotected sex was a continuous variable. While sexual risk was collected at 2 week post test, the 2 week time frame was not consistent with baseline or 3 and 6 month follow-up (90 days) and therefore dropped from the analysis. Measures were assessed separately for paying partners and trust partners.
Harmful alcohol use was assessed using the AUDIT, which was implemented during screening and then again at three and six months post intervention. The AUDIT is a ten item scale that ranks a respondent’s self-reported alcohol use from 0 to 40, with 40 being the most harmful possible score [40]. The time frame for the AUDIT was ‘in the past year’, meaning that some overlap in reporting time frame.
A participant satisfaction survey was distributed and completed by participants at the end of the last intervention session for each cycle. Surveys were completed anonymously.
Intervention
The study included three conditions: an HIV sexual risk reduction intervention (HIV-SRR); an enhanced HIV-SRR intervention based on the original sessions, but adding two sessions of motivational interviewing; and a wellness promotion control condition. The HIV-SRR intervention was adapted from Project Connect [42] and based on social cognitive theory and a relationship-oriented ecological perspective. Understanding that risk behaviors occur in a dyadic context, and consistent with the conceptual framework of the original research, the intervention sessions are relationship-based, meaning that the unit of attention was the woman and her paying sexual partner. Findings from Project Connect support the efficacy of a relationship-based intervention regardless of whether provided to individual women or to women with their sexual partners [42, 43], but has not been tested with women engaged in sex work for risk reduction with paying partners. The four HIV-SSR sessions focused on building knowledge and skills such as identifying safety risks, negotiating safer sex, and avoiding unsafe situations. The enhanced intervention (HIV-SRR+MI) incorporated two additional motivational interviewing (MI) sessions to HIV-SRR by “wrapping” around them: that is, one session preceding HIV-SRR and one following. The two wrap-around MI sessions focused on motivation to change, with particular emphasis on alcohol use in the context of HIV risk. Women received education about the benefits of reducing alcohol intake and were encouraged to consider their current levels of alcohol use and the pros and cons of reducing their alcohol intake. The four-session wellness promotion condition was matched to HIV-SRR in duration, timing and structure. The wellness promotion sessions focused on relaxation, the importance of exercise, the harm of smoking and healthy diet and nutrition. All conditions were developed in English and then translated to Mongolian.
Adaptations specific to Mongolian culture and language were made following several focus groups with sex workers to identify potential issues related to both the content and implementation feasibility of sessions. Focus group participants were asked semi-structured questions to elicit: (1) phenomenological and contextual narratives of how episodes of unprotected HIV risk behavior and alcohol use evolve and play out with paying partners; (2) women’s reactions to and suggestions to refine the core components of the interventions; (3) women’s narratives on the barriers to study participation and ethical issues related to study involvement. Revisions based on focus group themes were made to the sessions in consultation with the investigative team and a local community advisory board.
During the adaptation process, women made several recommendations that we incorporated into the final intervention. First, the women suggested that a group-based intervention—as opposed to an individually-based intervention—would offer more social support, as well as provide more opportunities to discuss concerns and problem-solve safer options. Women indicated a preference for a single-gender group with other sex workers, but not to include paying partners. Rather than focus on risk reduction with both paying partners and with trust (intimate) partners, women indicated a preference for the program to focus on reducing risk behaviors with paying partners (based on the perception that these partners may put them at greater risk) and for more content related to reducing the likelihood of exposure to violence at the hands of paying partners. A videotape and discussion of ways to reduce exposure to violence were added to the risk reduction (HIV-SSR) and risk reduction plus motivational interviewing (HIV-SSR+MI) sessions. Finally, women indicated a preference for having female facilitators, due to the sensitive nature of the content. Intervention sessions were therefore conducted only with women—and not their paying partners—in groups of six to eight women per group. All intervention sessions were delivered in Mongol by female facilitators and met weekly for 90 minutes.
Quality Assurance
All relevant research staff completed a standardized training, used structured intervention and assessment protocols, met on a weekly basis with clinical and task supervisors and received routine monitoring and supervisory feedback. To ensure fidelity of the assessment and intervention delivery, all assessments and intervention sessions were audiotaped and a random sample of approximately 10% for each interviewer and facilitator was reviewed by research staff. Assessment quality assurance reviews focused on each interviewer’s (1) ability to reliably follow the structured interview script/questions, including appropriate probing for clarification and non-directive responses to participants’ questions about assessment items; and (2) accuracy in recording participants’ responses into the computer. All reviewed interviews passed the 80% criterion for acceptability.
Mongolian investigators conducted reviews of intervention quality assurance (adherence) using a checklist that identified any deviation of content (whether each activity for each session was addressed) or time (did the facilitator spend adequate or too much time delivering each element). A checklist was developed for each condition as activities varied across conditions. Adherence to 80% of activities and time frames constituted adequate fidelity to the intervention. Reviews found that in reviewed sessions at least 80% of the activities were adequately delivered (no deviation in content or time on most activities). In up to 15% of the reviews, the most common error made by session facilitators was exceeding the session time limit and either missing the last one or two exercises or extending the session for an additional 15–30 min.
The study design included a Data Safety and Monitoring Plan (DSMP) which guided the protections of human subjects and data safety. The principal investigator and two co-investigators, one in Mongolia and one in the U.S., held primary responsibility for complying with the reporting requirements of the institutional and local IRBs as well as the funding agency.
Data Analysis
Outcomes included the percentage and the number of unprotected vaginal intercourse acts with paying partners in 90 days prior to assessment. Although the original study aim was to examine acts of both vaginal and anal sex across all types of partners, reports of anal sex were low and only half of our sample of women reported having trust (intimate) partners. These low subsample sizes precluded meaningful analyses based on all partners across both vaginal and anal sexual acts. For the purposes of this paper we examine acts of vaginal sex with paying partners.
To model the percentage of unprotected vaginal sex with paying partners, we used a zero-inflated logistic multilevel model. This model accounts for cases where there were completely protected (or zero unprotected) vaginal sex acts and repeated measurements for the same women, and which better fits the over dispersed count data (excessive observed zeros) compared to a traditional logistic regression model [44]. This zero-inflated model assumes that the data are a mixture of two separate data generation processes: one process generating only zeros, and the other process being a binomial distribution (using a logistic model); a Bernoulli trial (a logistic model) is used to determine which of these two processes generates an observation.
To model the number of unprotected vaginal sex acts with paying partners, we used a zero-inflated multilevel Poisson model, with random effects for different women. Again, this zero-inflated model assumes that the data are a mixture of two separate data generation processes: one process generating only zeros and the other process being a Poisson distribution. A Bernoulli trial (a logistic model) is used to determine which of these two processes generates an observation. For both models, since four surveys were taken for the same woman at consecutive time points, a moving average model with lag one (MA) (1) is added to account for the temporal correlation and over dispersion.
Using an intent-to-treat approach, data collection at each time point included all women randomized. The missing data were imputed using data augmentation [45] implemented by WinBUGS (a Gibbs Sampling software for Bayesian modeling) and assuming the data are missing at random (MAR). Analysis of data from participants missing due to follow-up (approximately 25% at each time point), indicated that young, unmarried women and women with higher income were more likely to be missing in the surveys after intervention. To account for missing data, the pretreatment attributes of age, income, and marital status were included in the model. Other associated variables such as education, marital status, and years of sex work were also included to explore possible associations between the outcome and background characteristics. When a participant reported zero instances of sex acts with a paying partner, both the proportion and the number of unprotected sexual acts were assigned a value of zero [46].
We implemented a Poisson regression to analyze scores on the AUDIT. An error term was added in the log link function to account for any over dispersion. The logarithm of the AUDIT score at assessment was added into the regression as an offset, to account for the correlation between assessment and after intervention.
For each of the above models, treatment dummies for the three randomly assigned groups were added to test the difference between treatment group and control group after intervention, and the after intervention dummy variables were added to test the overall improvement over time.
Results
In Table 1 we summarize the sociodemographic and risk behavior characteristics from the sample by treatment condition. No characteristics vary significantly by group, except for ‘duration of sex work,’ suggesting that the randomization was successful. We controlled for the variable ‘duration of sex work’ in the analysis. No serious adverse events occurred during this study.
Table 1.
Sociodemographic and risk behavior characteristics at baseline
| Wellness | Risk reduction | Risk reduction and motivational interviewing | Non-randomized | |
|---|---|---|---|---|
| n = 59 | n = 49 | n = 58 | n = 56 | |
| Sociodemographic characteristics | ||||
| Aged <25 years, % (n) | 10.17 (2) | 14.29 (7) | 12.07 (7) | 14.29 (8) |
| ≥Secondary school, % (n) | 93.22 (55) | 87.76 (43) | 82.76 (48) | 87.50 (49) |
| Monthly income ≤ 100,000 tugriksa, % (n) | 52.54 (31) | 44.90 (22) | 37.93 (22) | 50.00 (28) |
| Divorced, widowed, or separated, % (n) | 57.63 (34) | 55.10 (27) | 67.24 (39) | 57.14 (32) |
| Has trust partner, % (n) | 44.07 (26) | 51.02 (25) | 43.10 (25) | 39.29 (22) |
| Duration of sex work in years, mean (n) | 4.43b (57) | 6.71b (45) | 6.58b (56) | 5.23b (53) |
| Risk behavior characteristics | ||||
| Number of paying partners during most recent working day, mean (n) | 2.93 (59) | 2.60 (48) | 2.95 (58) | 2.64 (56) |
| Proportion condom use during vaginal sex with paying partners in past 90 days, mean (n) | 0.65 (44) | 0.72 (34) | 0.73 (50) | 0.79 (54) |
| STI symptoms in the last 12 months,% (n) | 30.51 (18) | 28.57 (14) | 29.31 (17) | 25.00 (14) |
| HIV positive, % (n) | 0.00 (0) | 2.04 (1) | 1.72 (1) | 0.00 (0) |
| No. of unprotected vaginal sexual acts with paying partner in past 90 days, mean (n) | 32.09 (44) | 26.56 (34) | 34.12 (50) | 24.98 (54) |
| Audit scores at assessment, mean (n) | 30.98 (59) | 28.42 (49) | 32.64 (58) | n/a |
One U.S. dollar is approximately 1,250 tugriks; 100,000 tugriks is approximately $80 U.S.
Significant difference between conditions at the P ≤05 level, with t test
Table 2 provides the mean scores on each outcome variable at each assessment time point. Mean numbers and proportion of unprotected sex acts across groups were lower at follow-up compared to baseline figures in Table 1. Risk reduction participants demonstrate consistent decreases in risk behavior as follow-up time increases, however, wellness and risk reduction plus MI participants demonstrate some increases in risk behavior over time.
Table 2.
Description of sexual risk and alcohol outcomes at week 2 follow-up, month 3 follow-up, and month 6 follow-up for wellness, risk reduction, and risk reduction and motivational interviewing conditions
| No. of unprotected vaginal sexual acts with paying partners (SE) (n) |
Proportion of unprotected vaginal sexual acts with paying partners (SE) (n) |
Audit scorea (SE) (n) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||||
| Baseline | Week 2 |
Month 3 |
Month 6 |
Baseline | Week 2 |
Month 3 |
Month 6 |
Baseline | Month 3 |
Month 6 |
|
| Wellness | 32.09 (7.21) (44) | 4.77 (1.64) (39) | 3.07 (1.42) (42) | 7.14 (3.74) (44) | 0.35 (0.05) (44) | 0.10 (0.028) (39) | 0.070 (0.025) (42) | 0.96 (0.031) (44) | 30.98 (0.83) (59) | 18.52 (1.64) (35) | 18.30 (1.47) (50) |
| Risk reduction | 26.56 (6.10) (44) | 7.57 (2.39) (35) | 5.56 (2.37) (34) | 1.38 (0.53) (33) | 0.31 (0.06) (44) | 0.12 (0.035) (35) | 0.09 (0.029) (34) | 0.05 (0.021) (33) | 28.42 (1.14) (49) | 21.00 (1.93) (27) | 18.12 (1.70) (33) |
| Risk reduction and motivational interviewing | 34.12 (6.62) (50) | 6.30 (2.17) (47) | 10.17 (5.28) (46) | 9.49 (4.54) (45) | 0.28 (0.04) (44) | 0.11 (0.034) (47) | 0.09 (0.030) (46) | 0.09 (0.028) (45) | 32.64 (0.73) (58) | 22.88 (1.40) (43) | 21.72 (1.24) (47) |
No data were collected at week 2
In Table 3 we provide estimates modeling the percentage of unprotected acts of vaginal intercourse, with both odds ratios (OR) for the Bernoulli logistic model based on zero unprotected acts, adjusted relative risk ratio (RRR) for the binomial logistic model of the percentage of unprotected acts, odd ratios (OR) and adjusted incidence risk ratios (IRR) for numbers of unprotected acts for the zero-inflated Poisson model.
Table 3.
Estimates of percentage of unprotected vaginal acts and no of unprotected vaginal sex (n=166)
| Percentage of unprotected vaginal sex with paying partners
|
No. of unprotected vaginal sex with paying partners
|
|||
|---|---|---|---|---|
| Bernoulli logistic model OR (95% CI) | Binomial logistic model RRR (95% CI) | Bernoulli logistic model OR (95% CI) | Poisson model IRR (95% CI) | |
| Baseline dummy | 0.29** (0.15, 0.57) | 0.56** (0.36, 0.85) | 0.44** (0.25, 0.79) | 20.08** (19.29, 0.90) |
| Wellness group dummy | 0.59 | 0.04** | 2.13** | 3.67** |
| After intervention dummya | (0.22, 1.59) | (0.00, 0.22) | (2.00, 2.27) | (2.04, 6.60) |
| HIVSRR group dummy | 1.61 | 0.07** | 2.46** | 5.48** |
| After intervention dummya | (0.72, 3.60) | (0.01, 0.50) | (1.36, 4.43) | (3.05, 9.85) |
| HIVSRR+MI group dummy | 0.95 | 0.06** | 2.23** | 6.69** |
| After intervention dummya | (0.46, 1.96) | (0.01, 0.43) | (1.24, 4.02) | (3.71, 12.06) |
Both binomial and Poisson models also include marital status, education, age, income, and duration of work
P < 0.01
We define an after intervention dummy variable to be equal to one for the data points of IPT, month 3, and month 6 surveys, and equal to zero for the baseline. Separate dummy variables for different surveys were also fitted, and the estimated coefficients are not significantly different for different surveys, so the after intervention dummy variable is included in the final model
The estimated odds ratios for the interaction terms of HIV-SRR group and HIV-SRR+MI group dummy variables and after intervention dummy variable (OR = 1.16, 0.95) are significantly larger than the estimated odds ratio for the baseline dummy variable (OR = 0.29), which shows that for those two treatment groups, the proportions of completely protected acts are significantly higher than they were at baseline. The estimated odds ratio for the wellness group is also larger than that of the baseline data, although this improvement is not significant. For all groups there is a higher likelihood post-intervention that the women engage in zero unprotected vaginal sex acts with paying partners.
All of the relative risk estimates for the interaction terms of the three treatment group dummy variables and after intervention dummy variable (RRR = 0.04, 0.07, 0.06) are significantly smaller than that of the baseline dummy variable (RRR = 0.56), which shows the overall improvement over time. The RRRs for different treatment groups (0.04, 0.07, 0.06) are not significantly different, which shows that the difference between treatment groups and the control group is not statistically significant. For all groups, the women are less likely to engage in unprotected vaginal sex acts with paying partners post-intervention.
When modeling the number of unprotected vaginal sex with paying partners, similar results are obtained: the estimated odd ratios for after intervention dummy variables (OR = 2.01, 2.46, 2.22) are significantly larger than that of the baseline (OR = 0.45); the estimated incidence rate ratios (IRRs) for the after intervention dummy variables (IRR = 3.67, 5.48, 6.69) are all significantly smaller than that of the baseline (IRR = 20.8). All of these results suggest that the estimated number of times that women in each group engaged in unprotected sex is significantly smaller after intervention compared to the times at baseline. Again, we did not detect significant differences between different treatment groups.
In Table 4 we show that the AUDIT scores after intervention (at the third and sixth month) are 40% lower compared to baseline AUDIT scores for both treatment and control groups. Again, we did not find significant differences between treatment groups.
Table 4.
Estimates of reductions in Alcohol Use Disorders Identification Test (AUDIT) scores pre and post treatmenta
| Intervention Group | Reduction in AUDIT scores RRR (95% CI) |
|---|---|
| Wellness group dummy | 0.54** (0.45, 0.65) |
| HIVSRR group dummy | 0.60** (0.49, 0.73) |
| HIVSRR+MI group dummy | 0.60** (0.49, 0.73) |
P < 0.01
Post treatment data are month 3 and month 6 AUDIT measurements
Discussion
This study is the first behavioral clinical trial of either an HIV/STI prevention intervention or of an alcohol use risk reduction intervention in Mongolia. Study findings demonstrate sexual risk reduction and harmful alcohol use reduction among sex workers in Mongolia across study conditions. These reductions are statistically significant over time for each group, although the reduction differences we expected to see between groups are not significant. Harmful alcohol use was also reduced significantly across all groups, but not between groups, and sustained over six months.
These findings suggest that even low impact interventions, such as a wellness condition, can achieve considerable reductions of HIV and STI risk in such a low-resourced setting. With few social or supportive services available, and among such a vulnerable and underserved population, we observed that the women in the study responded very strongly to minimal intervention. These findings are important for Mongolia, where there is still a low HIV prevalence. Broad dissemination of effective interventions—even relatively low impact interventions or those that are not directly targeting HIV prevention—may mean successful risk reduction and prevention of an HIV epidemic.
In light of the positive findings across groups, we consider possible explanations outside the original model (47–51). Explanations may include the facilitator/participant contact, participant behaviors outside of therapy, and environmental events. For example, the facilitator/participant contact was a shared component of the intervention and control groups of this study. The women who participated represent a highly marginalized and stigmatized population. Prior to the intervention, they had minimal contact or support from social services. For this population of vulnerable women, the facilitator/participant contact, or the therapeutic alliance formed between the participant and the facilitator, may explain the positive results found across all groups. Similarly, the expanded social networks and mutual support exchanged between participants in the groups may also have been a shared contribution toward change leading to positive outcomes. Consistent with Social Cognitive Theory and an ecological perspective, a less stigmatizing environment which encourages social support (provided through group work) and promotes peer norms may have influenced positive behavior changes.
Another phenomenon which may explain improved outcomes in all study groups is participant reactivity to psychosocial research. A growing body of evidence in the alcohol dependency literature suggests that improvements in intervention participants’ alcohol dependency outcomes result from their involvement in the research process [47–50]. Even if participants are able to differentiate between the intervention and the assessment, the lengthy pre-treatment and follow-up assessments may have been the explanations for alcohol use and sexual risk reduction across all three study arms.
In addition to sexual risk and alcohol use reductions, the study demonstrated secondary outcomes related to feasibility. It generated important insights and successes on implementing an intervention with a highly stigmatized and vulnerable population in Mongolia. The research team was able to recruit 270 sex workers and enroll 166 of these women over ten months. The attrition rate of 25% between eligible participants and enrollment is comparable to that of other U.S.-based HIV prevention studies conducted with less vulnerable populations [42, 46]. We also found no significant differences between the demographics of enrolled versus non-enrolled women. Eighty-eight percent (n = 142) of women randomized to participate in the study attended all of the intervention sessions and completed six month follow-up assessment. In a satisfaction survey completed by all participants, 92% positively endorsed the program experience. Finally, there were no adverse events reported throughout the duration of the study.
Findings need to be interpreted in light of study limitations. The study had a relatively small sample size, data was collected through self-report and without biological outcomes on STIs, and the follow-up period was short-term. The ninety day recall period for sexual acts, while standard for HIV/STI clinical trials, may have challenged the accuracy of participant response. Finally, although we were able to measure significant reductions in alcohol use and severity at follow up, scores at follow-up were on average still substantially higher than ‘8’, the AUDIT threshold for harmful alcohol use, indicating a need for further efforts to reduce alcohol use severity. Also, the AUDIT timeframe was ‘in the past year,’ so that pre- and post-measures had some overlap, where ideally the assessment would only have accounted for time since the prior assessment with the same instrument.
With the scientific advances of this study also come additional questions that need to be addressed. Additional research is required, including structuring a follow-up study with more attention to an analysis of the ‘active ingredients’ of the study interventions that led to risk reduction as well as testing to what extent reactivity to measurement or study context may influence outcomes. Future studies may build on this work by examining differences in sex workers risk with intimate (trust) partners compared with paying partners, and identifying ways to reduce risk with trust partners. Future research should also focus on dissemination and implementation of these three tested interventions, as appropriate, in NGO settings to risk groups targeted for prevention of communicable as well as non-communicable disease in Mongolia.
Acknowledgments
We wish to thank the National Institute of Alcohol and Alcohol Abuse for their support of this study. We also thank the women who participated in this study for giving their time and for sharing their personal experiences so that we were able to complete this research. This study was supported by NIAAA grant no. R21AA016286 awarded to Dr. Witte.
Contributor Information
Susan S. Witte, Email: ssw12@columbia.edu, Social Intervention Group, Columbia University School of Social Work, Columbia University Social Intervention Group, 1255 Amsterdam Ave., #813, New York, NY 10027, USA
Batsukh Altantsetseg, Wellspring NGO, Ulaanbaatar, Mongolia.
Toivgoo Aira, Wellspring NGO, Ulaanbaatar, Mongolia.
Marion Riedel, Columbia University School of Social Work, New York, NY, USA.
Jiehua Chen, Columbia University School of Arts and Sciences, New York, NY, USA.
Katie Potocnik, Social Intervention Group, Columbia University School of Social Work, Columbia University Social Intervention Group, 1255 Amsterdam Ave., #813, New York, NY 10027, USA.
Nabila El-Bassel, Social Intervention Group, Columbia University School of Social Work, Columbia University Social Intervention Group, 1255 Amsterdam Ave., #813, New York, NY 10027, USA.
Elwin Wu, Social Intervention Group, Columbia University School of Social Work, Columbia University Social Intervention Group, 1255 Amsterdam Ave., #813, New York, NY 10027, USA.
Louisa Gilbert, Social Intervention Group, Columbia University School of Social Work, Columbia University Social Intervention Group, 1255 Amsterdam Ave., #813, New York, NY 10027, USA.
Catherine Carlson, Social Intervention Group, Columbia University School of Social Work, Columbia University Social Intervention Group, 1255 Amsterdam Ave., #813, New York, NY 10027, USA.
Hanfei Yao, Columbia University School of Arts and Sciences, New York, NY, USA.
References
- 1.SS UNGA. UNGASS country progress report: Mongolia. New York: United Nations General Assembly; 2010. [Google Scholar]
- 2.NAF. Summary of review and evaluation of STI/HIV/AIDS community projects implemented by NGOs/CBOs in 2003. Ulaanbaatar: National AIDS Foundation; 2003. [Google Scholar]
- 3.Purevdawa E, Moon T, Baigalmaa C, Davaajav K, Smith M, Vermund S. Rise in sexually transmitted diseases during democratization and economic crisis in Mongolia. Int J STD AIDS. 1997;8(6):398–401. doi: 10.1258/0956462971920190. [DOI] [PubMed] [Google Scholar]
- 4.NAF. HIV and drug use participatory situation assessment report. Ulaanbaatar, Mongolia: NAF/UNDCP/HIV Alliance; 2001. [Google Scholar]
- 5.Fages V. Migration and AIDS in South Africa: a public health issue. Pretoria: UNAIDS; 1999. [Google Scholar]
- 6.UNAIDS. Population mobility and AIDS–technical update. Geneva: United Nations; 2001. [Google Scholar]
- 7.UNAIDS. Sex work and HIV/AIDS–technical report. Geneva: United Nations; 2002. [Google Scholar]
- 8.Ghys PD, Jenkins C, Pisani E. HIV surveillance among female sex workers. AIDS. 2001;15(suppl 3):S33–40. doi: 10.1097/00002030-200104003-00005. [DOI] [PubMed] [Google Scholar]
- 9.Amindavaa O, Kristensen S, Pak CY, Khalzan D, Chultemsuren B, Randall AS, et al. Sexually transmitted infections among pregnant women attending antenatal clinics in Mongolia: potential impact on the Mongolian HIV epidemic. Int J STD AIDS. 2005;16:153–7. doi: 10.1258/0956462053057693. [DOI] [PubMed] [Google Scholar]
- 10.Garland S, Tabrizi S, Chen S, Byaamba C, Davaajav K. Prevalence of sexually transmitted infections (Neisseria gonorrhoeae, Chlamydia trachomatis, Trichomonas vaginalis and human papillomavirus) in female attendees of a sexually transmitted diseases clinic in Ulaanbaatar, Mongolia. Infect Dis Obstet Gynecol. 2001;9(3):143–6. doi: 10.1155/S1064744901000254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elbright J, Altantsetseg T, Oyungerel R. Emerging infectious diseases in Mongolia. Emerg Infect Dis. 2003;9(12):1509–15. doi: 10.3201/eid0912.020520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tellez I, Altankhuu M, Vermund SH, Gnann JW, Hook EH, Schwebke J. Hepatitis, syphilis, and HIV sentinel surveillance in Mongolia 1999–2000. Sex Transm Infect. 2002;78:223–4. doi: 10.1136/sti.78.3.223-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weinhardt LS, Carey MP. Does alcohol lead to sexual risk behavior? findings from event-level research. J Sex Res. 2000;11:125–57. [PMC free article] [PubMed] [Google Scholar]
- 14.Cook RL, Clark DB. Is there an association between alcohol consumption and sexually transmitted diseases? a systematic review. Sex Transm Dis. 2005;32:156–64. doi: 10.1097/01.olq.0000151418.03899.97. [DOI] [PubMed] [Google Scholar]
- 15.Fleming DT, Wasserheit JN. From epidemiological synergy to public health policy and practice: the contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sex Transm Infect. 1999;75:3–17. doi: 10.1136/sti.75.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Campbell C. Selling sex in the time of AIDS: The psychosocial context of condom use by sex workers on a Southern African mine. Soc Sci Med. 2000;50:479–94. doi: 10.1016/s0277-9536(99)00317-2. [DOI] [PubMed] [Google Scholar]
- 17.Cote A, Sobela F, Dzokoto A, Nzambi K, Asamoah-Adu C, Labbe A, et al. Transactional sex is the driving force in the dynamics of HIV in Accra, Ghana. AIDS. 2004;18(6):917–25. doi: 10.1097/00002030-200404090-00009. [DOI] [PubMed] [Google Scholar]
- 18.Wechsberg WM, Lam WK, Zule WA, Bobashev G. Efficacy of a woman-focused intervention to reduce HIV risk and increase self-sufficiency among African American crack abusers. Am J Public Health. 2004;94(7):1165–73. doi: 10.2105/ajph.94.7.1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ngugi E, Branigan E, Jackson D. Interventions for commercial sex workers and their clients. In: Gibney L, DiClemente RJ, editors. Preventing HIV in developing countries: biomedical and behavioral approaches. New York: Kluwer Academic/Plenum Publishers; 1999. [Google Scholar]
- 20.Witte SS, Campbell A, El-Bassel N, editors. Designing HIV prevention for drug-involved women exchanging street sex; Society for Social Work Research Conference; New Orleans. January 2004. [Google Scholar]
- 21.Wang B, Li X, Stanton B, Fang X, Yang H, Zhao R, et al. Sexual coercion, HIV-related risk, and mental health among female sex workers in China. Health Care Women Int. 2007;28(8):745–62. doi: 10.1080/07399330701465226. [DOI] [PubMed] [Google Scholar]
- 22.Markosyan KM, Babikian T, DiClemente RJ, Hirsch JS, Grigoryan S, del Rio C. Correlates of HIV risk and preventive behaviors in Armenian female sex workers. AIDS Behav. 2007;11(2):325–34. doi: 10.1007/s10461-006-9147-x. [DOI] [PubMed] [Google Scholar]
- 23.Chersich MF, Luchters SMF, Malonza IM, Mwarogo P, King’ola N, Temmerman M. Heavy episodic drinking among Kenyan female sex workers is associated with unsafe sex, sexual violence and sexually transmitted infections. Int J STD AIDS. 2007;18(11):764–9. doi: 10.1258/095646207782212342. [DOI] [PubMed] [Google Scholar]
- 24.Panchanadeswaran S, Johnson S, Sivram S, Krikrishnan AK, Latkin C, Bentley ME, et al. Intimate partner violence is as important as client violence in increasing street-based female sex workers’ vulnerability to HIV in India. Int J Drug Policy. 2008;19(2):106–12. doi: 10.1016/j.drugpo.2007.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Le M, D’Onofrio C, Rogers J. HIV risk behaviors among three classes of female sex workers in Vietnam. J Sex Res. 2010;47(1):38–48. doi: 10.1080/00224490902999278. [DOI] [PubMed] [Google Scholar]
- 26.Paone D, Cooper H, Alperen J, Shi Q, Des Jarlais D. HIV risk behaviours of current sex workers attending syringe exchange: the experiences of women in five US cities. AIDS Care. 1999;11(3):269–80. doi: 10.1080/09540129947910. [DOI] [PubMed] [Google Scholar]
- 27.Jung Y, Song J, Chong J, Seo H, Chae J. Symptoms of post-traumatic stress disorder and mental health in women who escaped prostitution and helping activists in shelters. Yonsei Med J. 2008;49(3):372–82. doi: 10.3349/ymj.2008.49.3.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shahmanesh MMM, Wayal SM, Cowan FMF, Mabey DDF, Copas A, Patel VPM. Suicidal behavior among female sex workers in Goa, India: the silent epidemic. Am J Public Health. 2009;99(7):1239. doi: 10.2105/AJPH.2008.149930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ulibarri M, Semple S, Rao S, Strathdee S, Fraga-Vallejo M, Bucardo J, et al. History of abuse and psychological distress symptoms among female sex workers in two Mexico—U.S. border cities. Violence Vict. 2009;24(3):399. doi: 10.1891/0886-6708.24.3.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Murray L, Moreno L, Rosario S, Ellen J, Sweat M, Kerrigan D. The role of relationship intimacy in consistent condom use among female sex workers and their regular paying partners in the Dominican Republic. AIDS Behav. 2007;11(3):463–70. doi: 10.1007/s10461-006-9184-5. [DOI] [PubMed] [Google Scholar]
- 31.Hagan J, Dulmaa N. Risk factors and prevalence of HIV and sexually transmitted infections among low-income female commercial sex workers in Mongolia. Sex Transm Infect. 2007;34(2):83–7. doi: 10.1097/01.olq.0000237670.59140.0f. [DOI] [PubMed] [Google Scholar]
- 32.Dworkin S, Ehrhardt A. Going beyond “ABC: to include “GEM”: critical reflections on progress in the HIV/AIDS epidemic. Am J Public Health. 2007;91(1):13–6. doi: 10.2105/AJPH.2005.074591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Exner T, Hoffman S, Dworkin S, Ehrhardt AA. Beyond the male condom: the evolution of gender-specific HIV interventions for women. Annu Rev Sex Res. 2003;14:113–46. [PubMed] [Google Scholar]
- 34.Kalichman SC, Simbayi LC, Jooste S, Cain D. Frequency, quantity, and contextual use of alcohol among sexually transmitted infection clinic patients in Cape Town, South Africa. Am J Drug Alcohol Abuse. 2007;33(5):687–98. doi: 10.1080/00952990701522716. [DOI] [PubMed] [Google Scholar]
- 35.Kalichman SC, Simbayi LC, Kaufman M, Cain D, Jooste S. Alcohol use and sexual risks for HIV/AIDS in sub-Saharan Africa: systematic review of empirical findings. Prev Sci. 2007;8(2):141–51. doi: 10.1007/s11121-006-0061-2. [DOI] [PubMed] [Google Scholar]
- 36.Li Q, Li X, Stanton B. Alcohol use among female sex workers and male clients: an integrative review of global literature. Alcohol Alcohol. 2010;45(2):188–99. doi: 10.1093/alcalc/agp095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.MoH, WHO, CMHN. Epidemiological study on prevalence of alcohol consumption, alcohol drinking patterns and alcohol related harms in Mongolia Ulaanbaatar, Mongolia. 2006. [Google Scholar]
- 38.Chiao C, Morisky DE, Rosenberg R, Ksobiech K, Malow R. The relationship between HIV/sexually transmitted infection risk and alcohol use during commercial sex episodes: results from the study of female commercial sex workers in the Philippines. Subst Use Misuse. 2006;41(10–12):1509–33. doi: 10.1080/10826080600846284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shuper PA, Neuman M, Kanteres F, Baliunas D, Joharchi N, Rehm J. Causal considerations on alcohol and HIV/AIDS—a systematic review. Alcohol Alcohol. 2010;45(2):159–66. doi: 10.1093/alcalc/agp091. [DOI] [PubMed] [Google Scholar]
- 40.Saunders JB, Aasland OG, Babor TF, DeLaFuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on early detection of persons with harmful alcohol consumption II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 41.Sobell LC, Sobell MB. Timeline follow-back: a technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen JP, editors. Measuring alcohol consumption: psychosocial and biochemical methods. Totowa: Humana Press; 1992. pp. 41–72. [Google Scholar]
- 42.El-Bassel N, Witte SS, Gilbert L, Wu E, Chang M, Hill J, et al. The efficacy of a relationship-based HIV/STD prevention program for heterosexual couples. Am J Public Health. 2003;93(6):963–9. doi: 10.2105/ajph.93.6.963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.El-Bassel N, Witte SS, Gilbert L, Wu E, Chang M, Hill J, et al. Long-term effects of an HIV/STI sexual risk reduction intervention for heterosexual couples. AIDS Behav. 2005;9(1):1–13. doi: 10.1007/s10461-005-1677-0. [DOI] [PubMed] [Google Scholar]
- 44.Hardin JWH, Joseph M. Generalized linear models and extensions. 2. College Station, Texas: Stata Press Publication, Stata Corp LP; 2007. [Google Scholar]
- 45.Schafer JL. Analysis of incomplete multivariate data. London: Chapman & Hall; 1997. [Google Scholar]
- 46.NIMH Multisite HIV Prevention Trial. Reducing sexual risk behavior. Science. 1998;280:1889–94. doi: 10.1126/science.280.5371.1889. [DOI] [PubMed] [Google Scholar]
- 47.Morgenstern J, Irwin TW, Wainberg ML, Parsons JT, Muench F, Bux JDA, et al. A randomized controlled trial of goal choice interventions for alcohol use disorders among men who have sex with men. J Consult Clin Psychol. 2007;75(1):72–84. doi: 10.1037/0022-006X.75.1.72. [DOI] [PubMed] [Google Scholar]
- 48.Epstein EE, Drapkin ML, Yusko DA. Is alcohol assessment therapeutic? pretreatment change in drinking among alcohol-dependent women. J Stud Alcohol Drugs. 2005;66(3):369–78. doi: 10.15288/jsa.2005.66.369. [DOI] [PubMed] [Google Scholar]
- 49.Clifford PR, Maisto SA, Davis CM. Alcohol treatment research assessment exposure subject reactivity effects: part 1. Alcohol use and related consequences. J Stud Alcohol Drugs. 2007;68(4):519–28. doi: 10.15288/jsad.2007.68.519. [DOI] [PubMed] [Google Scholar]
- 50.Anton R, O’Malley SS, Ciraulo DA, Cisler RA, Couper D, Donovan DM, et al. Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. JAMA. 2006;295(17):2003–17. doi: 10.1001/jama.295.17.2003. [DOI] [PubMed] [Google Scholar]