Abstract
Eustachian tube dysfunction (ETD) has a role in chronic otitis media (COM) is a well known fact and number of modalities have come up for its assessment—slow motion dynamic videoendoscopy (SMDV) being the latest. (i) To find prevalence of ETD in COM and (ii) to check the efficacy of SMDV in detecting dysfunction as compared to gold standard tympaometry (TYM). It’s a prospective analytical study with total of 100 patients of chronic otitis media, hence 200 ears were tested for ETD by TYM and SMDV. Prevalence of ETD was noted as 35.5 % in COM whereas the two testing modalities TYM versus SMDV showed agreement in 161 cases out of the 200 ears giving a moderate agreement of statistical significance (Kappa test) suggesting SMDV to be included in standard of protocol when assessing ETD along with TYM.
Keywords: Slow motion dynamic videoendoscopy, Eustachian tube, Tympanometry, Chronic otitis media, Adenoid hypertrophy
Introduction
Eustachian tube being necessary for a healthy and functioning tympanum is a known fact and precise evaluation of the tube function helps to predict success of the surgical practices is also a well studied fact.
More than 600 articles were published on otitis media between April 2004 and April 2005. Of these articles, several focused on the role of the eustachian tube in the pathogenesis of otitis media.The tubal muscles must actively dilate the tubal valve to open Eustachian tube for adequate ventilation of the middle ear to occur. Failure of the valve to open adequately is likely responsible for a significant percentage of otitis media with effusion (OME) cases. Inflammation of the tubal lumen is probably a major contributor to tubal dysfunction [1, 2].
In some tests we are checking the eustachian tube through the middle ear route in which impedance audiometry is still the gold standard. But till what extent is the anatomical assessment of tube from pharyngeal end helpful in predicting dysfunction is the ongoing research. Dynamic video endoscopy and assessment of the tubal movement are to a greater extent important tool for assessment of dysfunctions associated with anatomical abnormalities, muscular dysfunction and patulous Eustachian tube. Among the most common dysfunctions are obstruction occurring as a result of an anatomic abnormality, local mucosal changes created by otitis media or allergies, patulous Eustachian tubes, or palatal myoclonus [2, 3].
In year 2001, Poe DS studied the analysis of ET dysfunction by video endoscopy and concluded that slow-motion endoscopic video analysis is a potentially useful technique in classifying types of pathologic changes in the ET. Video endoscopy of Eustachian tube is a promising, efficient and effective newer modality as it gives us, direct real time visualization of the ET and direct assessment of ET functioning [4].
The currently available data on the epidemiology of otitis media are important to review because the Eustachian tube is involved in the pathogenesis of this disease and its complications and sequelae and therefore affects the prevalence, incidence, and natural history in specific age groups and differing populations. Hence Eustachian tube dysfunction and its pathogenesis in chronic otitis media being an unsolved argument since era of evolution of otolaryngology, finding in the new techniques of assessment of Eustachian tube functioning—dynamic video endoscopy can be of great assistance for future application. Hence we decided to study the new modality of dynamic slow motion video endoscopy of Eustachian tube and compared it with the gold standard—tympanometry results in all cases of chronic middle ear diseases—a study which is not ventured much till date and research on same might open new horizons.
The aim and objective of study were to:
Find the prevalence of Eustachian tube dysfunction in middle ear pathologies.
Find the efficacy of the slow motion dynamic video endoscopic modality and correlate it with tympanometric findings (Agreement).
Methodology
The study was conducted after approval from HREC (Human Resource and Ethics Committee) of our institute. This was an Analytical prospective study carried out at Department of ENT & HNS, Pramukhswami Medical College and Shree Krishna Hospital, Karamsad, Anand, Gujarat, India from October 2011 to June 2013.
Inclusion Criteria
All patients of age >15 years clinically diagnosed with following conditions were included in the study.
Chronic otitis media—attico antral disease—retraction of pars flaccida or tensa which has retained squamous epitheial debris with inflammation of adjacent mucosa or has propensity to develop cholesteatoma, and Tubo tympanic disease—permanaent perforation of pars tensa with or without inflamed middle ear mucosa [5].
Secretory otitis media and its sequelae. (Atelectasis and Adhesive otitis media)—chronic accumulation of mucus in the middle ear and mastoid air cells for more than 12 weeks with on tympanometry showing type B or C curves [6].
Exclusion Criteria
All patients with acute upper respiratory infections and acute middle ear pathologies-acute phase of secretory otitis media, acute otitis media.
All chronic middle ear pathology patients were assessed for ET dysfunction by performing tympanometry (machine configuration are as follows amplaid middle ear analzer A766 with manual and automatic pressure changes and reflex recording). Tympanogram of the patients with intact tympanic membrane was obtained by performing the Wilson Test and with perforation recordings obtained on Toynbee Test by pressure equilibration (Inflation–Deflation) test.
Operational definitions considered in study are as below:
In Intact Tympanic membrane—type B curve (flat tympanogram) is considered ETD in secretory otitis media cases.
In Sequelae of OME—Adhesive and atelectasis—inability to get peak of tympanogram shifted to negative side of graph on swallowing is considered as Eustachian tube dysfunction present.
In perforated tympanic membrane—Any residual pressure of 50 daPa or more after 3 swallows is considered abnormal hence ETD present.
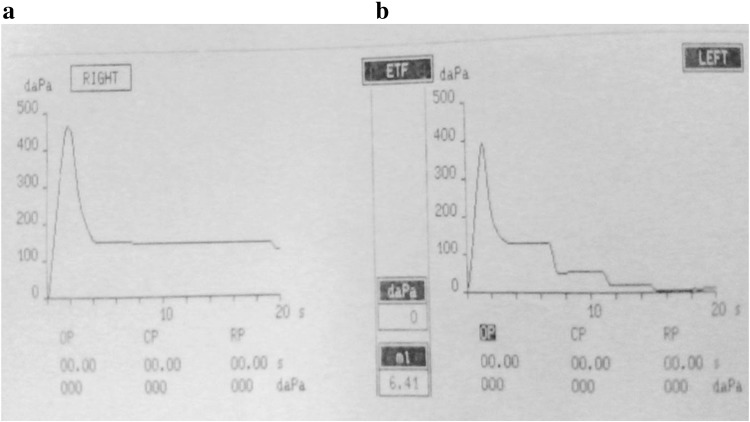
For Example in Fig. 1 which shows the recording of a patient with bilateral chronic otitis media tubotympanic type with moderate central perforation dry ear- toynbee’s test is performed. We can see that in the right ear (Fig. 1a) after the initial pressure rise there is a fall of >100 daP hence Eustachian tube does open to inflation but on swallowing action no further drop of the residual pressure occurred hence it was considered dysfunctional recording. In the left ear (Fig. 1b) on inflation same quantitative i.e. 100 daPa drop was seen but which further equilibrated with atmospheric pressure with each of the 3 swallows and finally the residual pressure is 0 daPa hence Eustachian tube was considered functioning on left side in a perforated tympanic membrane.
Fig. 1.
a Right ear recording (ETD present). b Left ear recording (ETD absent)
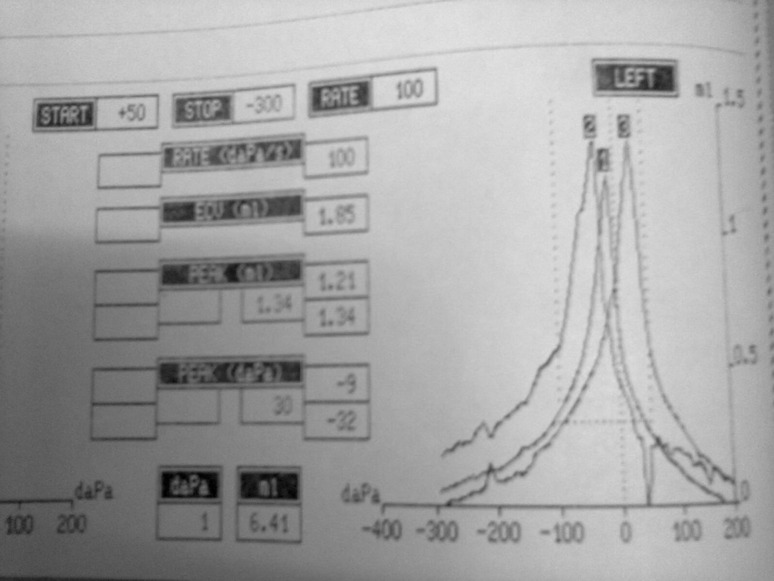
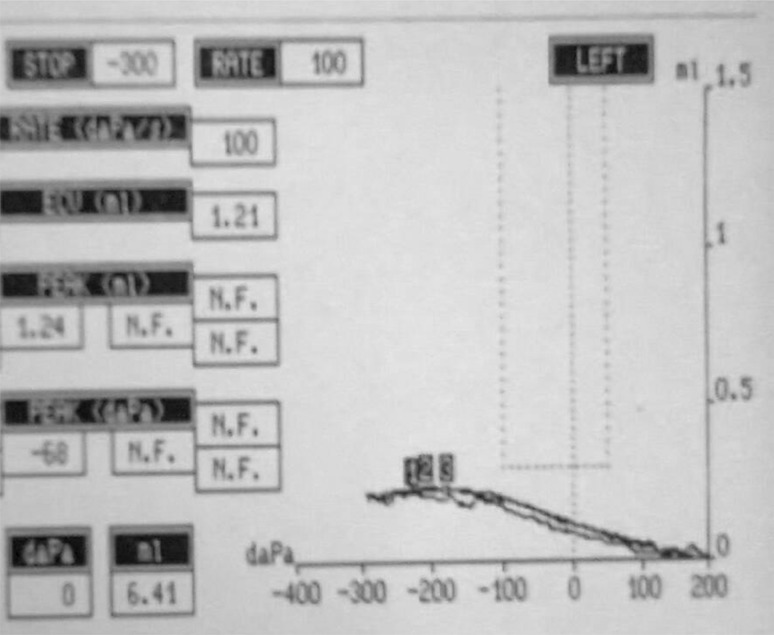
Another example to quote the findings in a patient with intact tympanic membrane tested by wilson’s test is shown in Fig. 2.
Fig. 2.
ETD absent
This Fig. 2 shows Eustachian tube tested in Intact Tympanic Membrane with wave 1 as primary baseline, wave 2 on swallowing i.e. negative pressure and hence the shift to left (negative), and lastly wave 3 on trial of valsalva which only few patient could perform which is positive pressure and hence shift to right side (positive) and hence the above are the finding of normal tympanic membrane. Any deviation from the above finding was considered dysfunctional as for example Fig. 3 where in secretory otitis media on well formed peak is seen instead a type B curve is seen which is not affected by the 3 swallow manuevre.
Fig. 3.
Left ear finding in case of secretory otitis media (ETD present)
In this study, nasal endoscopy was done with rigid Hopkin’s 30 degree 4 mm nasal endoscope. All subjects were examined in ENT outpatient department (OPD). Two cotton wick soaked in 2 % lignocaine were kept into each nasal cavity for 5–10 min. Once anesthetized, the nasal endoscope was introduced along the floor of the nasal cavity until it faced the nasopharyngeal orifice of the Eustachian tube. Nasal endoscopy was then viewed in EndoVue monitor with camera source of tricam SL and with xenon nova 300 as the light source in the OPD and the recordings were saved and viewed in VLC player software in slow motion 0.2× to 0.4× speed setting for observing the function. The patient was asked to swallow three times their own saliva and recording of the same was taken in nasal endoscopy. The process was performed for both Eustachian tube and Eustachian tube function was tested by studying the slow motion frame by frame recording of the videos of nasal endoscopies for the actions at rest and swallowing and the movements of medial cartilaginous lamina, lateral excursion, and dilatory wave of the lateral pharyngeal wall and tubal lumen opening were inspected.
Eustachian tubes were carefully inspected for evidence of anatomical obstruction, mucosal disease, opening and closing action of the tube, and observed for any other pathologic changes.
Examples of above are mentioned—Fig. 4 Normal left sided Eustachian tube.
Fig. 4.
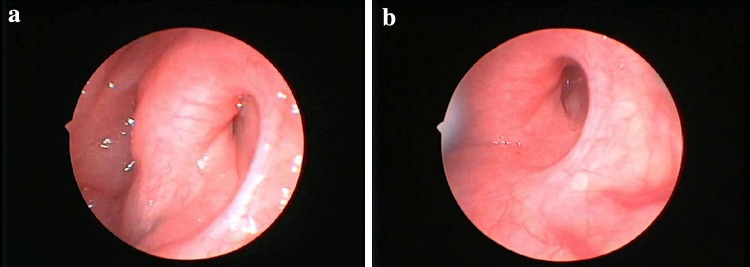
a Closed stage. b Open stage
Observation/Results
A Total of 100 cases were considered under the study and later each ear considered separately under the recordings hence we have 200 ear findings.
*Abreviations for further reference
Eustachian Tube Dysfunction—Tympanometry (ETD-T).
Eustachian Tube Dysfunction—Endoscopy (ETD-E).
Age and Sex Wise Distribution of Data
In the assessed data out of the 100 patients ETD was found in 37 % cases were from age range of 15–25 years and least were from 76 to 85 years.
Median age was 30 year i.e. 50 % of patients are above 30 year and 50 % below 30 year.
The Data showed Eustachian tube dysfunction (ETD) in which 36 were females and 23 males of which 16 females and 25 males had Eustachian tube dysfunction on tympanometry with a total of 41 cases with ETD-T out of 100.
The prevalence of Eustachian tube dysfunction in chronic otitis media cases in this study was 71 out of 200 ears (35.5 %) on tympanometry, however on nasal endoscopy the prevalence was 124 out of 200 ears (62 %).
For the further analysis of the Table 1, kappa analysis was applied to find an agreement between two testing modalities i.e. Eustachian tube function on tympanometry and dynamic slow motion video endoscopy. The Kappa value for the Table 1 is 0.553 which according to the interpretation of the value suggests that the data falls under Moderate Agreement.
Table 1.
ETD-T versus ETD-E 2 × 2 tabulation format (cross tabulation for kappa statistical analysis)
| ETD-T | ETD-E | ||
|---|---|---|---|
| Absent | Present | Total | |
| Absent | 117 | 12 | 129 |
| Present | 27 | 44 | 71 |
| Total | 144 | 56 | 200 |
N = 200
Disease Wise Correlation (Agreement) of ETD Done by Both Modalities
In cases of atticoantral disease out of the total 17 ears 11 showed agreement in terms that both nasal endoscopy and tympanometry showed dysfunction. Similarly in tubotympanic cases out of the 66 ears 58 showed agreement and 8 disagreement.
Secretory otitis media due to limited cases cannot be assessed for a definitive conclusion. There were total 8 cases of which 4 cases showed agreement and 4 disagreement among the testing modalities.
Lastly all ears with normal tympanic membrane with no obvious pathology showed disagreement in 18 ears rest all cases of the total 100 ears showed synchrony i.e. agreement.
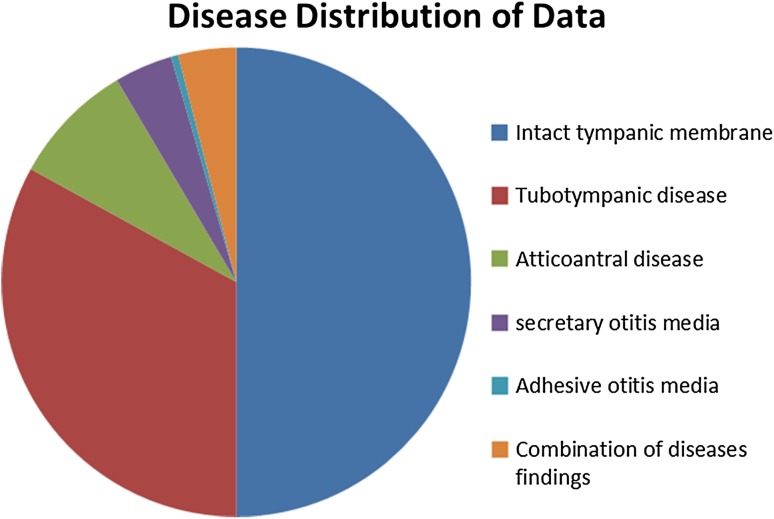
Following chart (Fig. 5) summarizes disease distribution in all patients included in our study.
Fig. 5.
PPie diagram summarizing disease distribution
Table 2.
Abnormalities seen on eustachian tube endoscopy findings (N=200)
| Tubal opening on swallowing | Medial lamina movement | Lateral lamina movement | Anatomical obstruction | Mucosal oedema | |
|---|---|---|---|---|---|
| Present | 175 | 177 | 178 | 16 | 38 |
| Absent | 25 | 23 | 22 | 184 | 162 |
| Total | 200 | 200 | 200 | 200 | 200 |
Total 16 cases showed anatomical obstruction as cause of dysfunction of which 14 had adenoid hypertrophy and 2 patients one a 30 year old female and another 35 year old male with nasopharyngeal mass, both of whom were not willing for further workup for the nasal mass hence the true diagnosis of mass is not known.
Out of the total dysfunction 124 ears of 200 ears on nasal endoscopy, 70 were attributed by dysfunction on tubal opening and closing and other muscular weakness whereas the mucosal edema amounted to 38 ears and adenoid hypertrophy to 16 ears.
Discussion
Its been known since the time of the very first description of Eustachian tube—its structure and function, that it plays an important role in the pathophysiology of chronic middle ear pathologies and if not solely but has significant contribution to this multifactorial disease. In this time of developing and newer technology this is our effort to test the modality of slow motion dynamic videoendoscopy for assessing the Eustachian tube dysfunction in chronic middle ear diseases.
By doing so the value of outpatient nasal endoscopy too gets upgraded as we not only assess the nose but also the ear by means of Eustachian tube assessment. Video endoscopic examination can be done with either a rigid or a flexible nasal endoscope. The Hopkins rod telescopes yield the best images with superior resolution, compared with the fiberoptic images. It is easier to pass the flexible scopes, but we preferred the 4-mm rigid scopes because of their high quality resolution [7].
The basis of our study was a study by Mathew [8] in 2006 where the author has tried to classify the video endoscopy findings in patients coming to ENT department. They have made an effort to make a grading system for the dysfunctions noted on endoscopy which is as follows.
Eustachian tube movements were graded endoscopically based on severity of tubal pathology observed, as follows:
Grade 0. Normal ET with no mucosal edema or congestion. Medial cartilaginous lamina and lateral wall motions are normal. Tubal lumen opens well on swallowing.
Grade 1. Edema and congestion of mucosa limited to pharyngeal orifice of ET. Normal lateral wall motion and tubal lumen opens with swallowing.
Grade 2A. Reduced lateral wall motion secondary to edema and congestion involving lumen. Tubal lumen opens partly with swallowing.
Grade 2B. Reduced lateral wall motion secondary to abnormal tubal muscle contraction. Tubal lumen opens partly with swallowing.
Grade 3A. Tubal lumen fails to open with swallowing secondary to gross edema.
Grade 3B. Tubal lumen fails to open with swallowing secondary to abnormal tubal muscle contraction.
Patulous (P). Patulous tubes showed noticeable concavity in the superior portion of the lateral wall of ET lumen, with persistent patency of the lumen, extending toward the isthmus, with medial and lateral cartilaginous lamina remaining separate even at rest [8].
In their case group, failure of tubal dilatation was most commonly caused by mucosal edema (56 %) followed by reduced, uncoordinated, or absent lateral wall movement (54 %). Further in a study of 58 dysfunctional ETs based on slow motion video endoscopy, Poe et al. noted mucosal edema with reduced lateral wall motion as the most common causes of tubal dysfunction. Edema of ET mucosa could affect tubal motion either from bulk effect, mechanical thickening, and stiffening of the walls or from secretory proteins with increased fluid viscosity. This could be secondary to primary mucosal disease, inflammatory conditions, infection, or allergy and could result in functional closure of the ET lumen [9].
In our study we have assessed the Eustachian tube dysfunction based on presence or absence of dysfunction by subjective characters of mucosal edema causing reduced tubal opening and closing or not opening at all,or it maybe due to muscular weakness and anatomical abnormality. Secondly these tests where done on all diagnosed cases of chronic middle ear disease with anticipated if not always, tubal dysfunction. We noted out of the 200 ears of which the tubal status was assessed on endoscopy, 19 % had mucosal edema, 12.5 % had edema alongwith muscular weakness and 8 % cases had anatomical obstruction in terms of adenoid hypertrophy or nasopharyngeal mass. Hence the findings did come in accordance to the previous studies in this area. Regarding the comparison and agreement among the tests we know that although there have been several manometric tests to assess tubal function indirectly, such as tympanometry, forced opening test, inflation-deflation. A single test of ET function is of low prognostic value. All direct tests such as mucociliary clearance tests, computed tomographic studies, and radiographic studies are time consuming, cumbersome, or expensive [10].
Tympanometry had lead otorhinolaryngologists to work upon the skills in middle ear reconstruction and tympanoplasties whereas endoscopy lead then to work on tubal opening by performing the tuboplasty and medical management for causes of persistent mucosal inflammation at the pharyngeal end. Because good ET function may enhance middle ear aeration, postoperative tympanic membrane mobility can be optimized to permit hearing improvement using the normal amplification mechanism of the middle ear. In a study at Korea using preoperative and postoperative tympanometry testing on inflation and deflation test, the patients were categorized into four groups according to preoperative ET function measurements using a modified pressure inflation-deflation equilibration test. Group I patients had residual pressures less than 10 daPa, and Group IV patients showed no pressure change (poor results). Groups II and III were intermediate. Hearing levels were determined using pure tone averages at four frequencies. Postoperative tympanometry performed to determine middle ear aeration observed a mean hearing improvement of 11–14 dB regardless of ET functional status, eventhough the worst postoperative hearing level was seen in Group IV patients. They concluded that ET function measured with a modified pressure equilibration test using an inflation-deflation manometric method is a good indicator of an aerated middle ear and is predictive of improved postoperative hearing [11, 12].
Our study has proved a moderate agreement among testing modalities so we can now apply the slow motion dynamic videoendoscopy alongwith tympanometry as a rountine protocol in preoperative assessment of tubal function in patient posted for ear surgeries to reduce the fallacies missed on tympanometry either because of technical issues or patient factor (pain, discharge) and over diagnosis on nasal endoscopies.
The Data at our center was assessed on gross grounds of slow motion dynamic videoendoscopy findings to reduce the subjectivity of results, as grading and its application was not possible in this point prevalence study. We also found a greater agreement in testing modality in cases of tubotympanic disease as compared to atticoantral disease which is not a negative point but a point requiring revision in tympanometry technical issues to reduce exclusion of atticoantral cases. On grounds of agreement and disagreement eventhough secretory otitis media did not give us satisfying results, the slow motion dynamic videoendoscopy did show mucosal edema in maximum cases of dysfunction leading us to the answer for chronicity of disease and its probable etiology of allergy and acid reflux diseases which resulted in tubal edema.
From this study, we would like to conclude that slow motion videoendoscopy is useful in studying the anatomy of pharyngeal end of ET orifice and lumen and inspecting its mucosa and helps us to better understand its dilatory movements and normal and abnormal patterns. Furthermore, the significant agreement between dynamic ET endoscopic findings with tympanometry studies in chronic middle ear disease suggests that, ears with a normal tympanic membrane (TM) finding with normal slow motion videoendoscopy and tympanometry results are most likely to have normal ET function. On the other hand, an abnormal TM finding with abnormal slow motion videoendosscopy and tympanometry studies point to a dysfunctional ET.
Further study is needed to assess the impact and effort of this new modality with tympanometry on tympanoplasty results.
Conclusion
By means of slow motion videoendoscopy, patency and dynamics of Eustachian tube are well understood and when this same knowledge is combined with the near gold standard test of tympanometry in chronic middle ear diseases we have a better output in identifying the dysfunctional tubes. Applying this modality agreement as a standard protocol in chronic middle ear disease patients, can help us get improved results in terms of medical and surgical management of patients. Hence on a concluding note agreement among tests can yield a better patient care in chronic middle ear pathologies. Slow motion videoendoscopic assessment of Eustachian tube is an office based testing modality ready to be explored in greater details.
Summary
Eustachian tube dysfunction is a major etiological contributor to chronic otitis media.
Prevalence of Eustachian tube dysfunction in chronic otitis media cases in this study was noted to be 35.5 %
The two tests—slow motion videoendoscopy and tympanometry showed moderate agreement as per analysis. Out of the 200 ears of patients with chronic otitis media included, 161 ears showed agreement of two tests and 39 showed disagreement. On kappa statistical analysis, a significant result of 0.553, which is Moderate Agreement, was noted.
Of all cases tubotympanic disease 88 % showed agreement and in atticoantral disease 35 % showed agreement. The results for secretory otitis media were not much encouraging and conclusive.
Of All dysfunction noted in slow motion dynamic videoendoscopy i.e. 62 %, 35 % (70 ears) showed dysfunction in tubal opening and closing and muscular weakness, 19 % (38 ears) showed mucosal edema, and 8 % (16 ears) showed anatomical obstruction (adenoid hypertrophy).
References
- 1.Bluestone CD, Rood SR, Douglas Swart J (2005) Anatomy and physiology of the eustachian tube. Chapter 142:2–6
- 2.Bluestone CD. Eustachian tube: structure, function, and role in otitis. Media. 2005;2:4. [Google Scholar]
- 3.Lindeman P, Holmquist J. Mastoid volume and Eustachian tube function in ears with cholesteatoma. Am J Otol. 1987;8:5–7. [PubMed] [Google Scholar]
- 4.Poe DS, Pyykko I, Valtonen H, Silvola J (2000) Analysis of eustachian tube function by video endoscopy. Am J Otol 21(5):602–607 [PubMed]
- 5.Chi M, Tong F, Andrew C, Hasselt V Otitis media with effusion in adults. 7th edn. Scott Brown, vol 3; chapter 237b, p 388
- 6.Browning G, Merchant S, Kelly G, Swan L, Canter R, Mckerrow W Chronic otitis media; 7th edition Scott Brown vol 3, chapter 237c, p 396
- 7.Linstrom CJ, Silverman CA, Rosen A. Eustachian tube endoscopy in patients with chronic ear disease. Laryngoscope. 2000;110:1884–1889. doi: 10.1097/00005537-200011000-00022. [DOI] [PubMed] [Google Scholar]
- 8.Mathew GA, Kuruvilla G, Job A. Dynamic slow motion video endoscopy in Eustachian tube assessment. Am J Otolaryngol Head Neck Med Surg. 2007;28:91–97. doi: 10.1016/j.amjoto.2006.06.019. [DOI] [PubMed] [Google Scholar]
- 9.Poe DS, Abou-Halawa A, Abdel-Razek O. Analysis of dysfunctional eustachian tube by video endoscopy. Otol Neurotol. 2001;22:590–595. doi: 10.1097/00129492-200109000-00005. [DOI] [PubMed] [Google Scholar]
- 10.El-Guindy A. A correlative manometric and endoscopic study of tubal function in chronic otitis media with effusion. Acta Otolaryngol (Stockh) 1998;118:692–696. doi: 10.1080/00016489850183197. [DOI] [PubMed] [Google Scholar]
- 11.Choi SH, Han JH, Chong WJ. Pre-operative evaluation of eustachian tube function using a modified pressure equilibration test is predictive of good postoperative hearing and middle ear aeration in type 1 tympanoplasty patients. Clin Exp Otorhinolaryngol. 2009;2(2):61–65. doi: 10.3342/ceo.2009.2.2.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miller GF, Jr, Bilodeau R. Preoperative evaluation of Eustachian tube function in tympanoplasty. South Med J. 1967;60:868–871. doi: 10.1097/00007611-196708000-00016. [DOI] [PubMed] [Google Scholar]