Abstract
Cavernous sinus thrombosis is a rare presentation. Early diagnosis and aggressive treatment are required to prevent morbidity and mortality. Nasal infections can give rise to serious intracranial complications. Presented here is a case series of cavernous sinus thrombosis of nasal septic origin. The purpose of this article is to report our experience in pediatric patients with this illness to ascertain a clinical course and outcomes for further clinical application. Eight (08) cases of nasalseptic origin of cavernous sinus thrombosis ata tertiary care teaching hospital in the north India region of India were included in the study. Cases presented with various symptoms like headache, proptosis, ophthalmoplegia and fever. The patients were investigated by doing High Resolution Computed Tomography of nose & PNS and brain with intravenous contrast. The cases were treated with intravenous broad spectrum antibiotics. Eight patients less than 16 years of age (mean age of 11.2 years)diagnosed with cavernous sinus thrombophlebitis due to nasal septic focus over the period of 05 years were reviewed retrospectively. The predisposing infections and causative microorganisms were similar to previous reports in children. A conservative management strategy with antibiotics gave a good prognosis in these cases. There were no deaths. Early recognition of this condition, the appropriate selection of empirical antibiotic therapy, and the awareness of associated complication were the key factors leading to excellent outcome.
Keywords: Cavernous sinus thrombosis, Nasal, Proptosis, Ophthalmoplegia
Introduction
Cavernous sinus thrombosis (CST) was initially described by Bright in 1831 as a complication of epidural and subdural infections. CST is a very rare, life-threatening condition that can affect adults and children. CST is usually a late complication of an infection of the central face or paranasal sinuses. Other causes include bacteremia, trauma, and infections of the ear or maxillary teeth. Occurrence of CST has always been low, with only a few hundred case reports in the medical literature. One review of the English-language literature found only 88 cases from 1940–1988 [1].In the pre antibiotic era, CST was a well known complication. Septic cavernous sinus thrombosis is now a rare disease as the incidence of CST has been decreased greatly with the advent of effective antimicrobial agents [2].
CST is not often reported in the pediatric literature. Its incidence is evaluated to be 0.67 case per 100,000 children per year. The causes of CST are numerous, but can be classified, according to Virchow, into 3 main groups. The first group consists of all hyper-congealable states. The second group consists of conditions causing blood flow disturbance. The third group comprises all causes of inflammation, infection, or damage to the sinus wall [3].The classic presentation of CST is severe illness associated with typically high and swinging fever. As the clot proliferates along the sinus, it is accompanied by peri-venous inflammation, tenderness, and jugular lymphadenopathy. The increased intracranial pressure is usually suggested by papilledema and visual loss. Septic emboli dissemination to the lungs, large joints, and subcutaneous tissues usually follows [4].
Prior to the advent of effective antimicrobial agents, the mortality rate from CST was effectively 100 %. Typically, death is due to sepsis or central nervous system (CNS) infection. With aggressive management, the mortality rate is now less than 30 %. Morbidity, however, remains high, and complete recovery is rare. Roughly one sixth of patients are left with some degree of visual impairment, and one half have cranial nerve deficits. [5]
Staphylococcus aureus accounts for approximately 70 % of all infections. Streptococcus pneumoniae, gram-negative bacilli, and anaerobes can also be seen. Fungi are a less common pathogen and may include Aspergillus and Rhizopus species [2].Many times, the cultures yield a mixed flora [6].
Blindness as a result of cavernous sinus thrombosis is uncommon, occurring in less than 10 % of cases. Several mechanisms may be implicated. Corneal ulceration may occur from failure of lid closure. Occlusion of the central retinal artery may develop from pressure at the orbital apex or as the result of embolium. Focal arteritis leading to occlusion of the internal carotid artery may cause ophthalmic artery ischaemia. Toxic neuritis of the optic nerve has been suggested as a possible cause of blindness, secondary to ‘adjacent purulent inflammation’ [5].
Anatomy
Cavernous sinus is an irregular shaped, endothelium lined venous space, on either side of sella turcica at the base of the skull, just lateral and superior to the sphenoid sinus and are immediately posterior to the optic chiasm. Each cavernous sinus is formed between layers of the dura mater, and multiple connections exist between the 2 sinuses.
Structures passing through the wall of cavernous sinus are internal carotid artery, abducens, oculomotor, trochlear nerve and divisions of trigeminal nerve. The intimate juxtaposition of veins, arteries, nerves, meninges, and paranasal sinuses accounts for the characteristic etiology and presentation of CST.
The cavernous sinuses receive venous blood from the facial veins (via the superior and inferior ophthalmic veins) as well as the sphenoid and middle cerebral veins. They, in turn, empty into the inferior petrosal sinuses, then into the internal jugular veins and the sigmoid sinuses via the superior petrosal sinuses. This complex web of veins contains no valves; blood can flow in any direction depending on the prevailing pressure gradients. Thrombosis of the cavernous sinus may be due to extension of retrograde thrombosis from various sources. Because of the communications of the cavernous sinus with other venous channels, infection may occur via the orbital veins (as in septic lesions of the face, mouth, pharynx, ear, nose and paranasal sinuses), or as a metastasis in infectious diseases or septic conditions [7].
The “danger triangle of the face” consists of the area from the corners of the mouth to the bridge of the nose, including the nose and maxilla. The relationship between this area and a risk of cavernous sinus thrombosis was described as early as 1852. In 1937 a study found that 61 % of the cases of cavernous sinus thrombosis were the result of furuncles on the upper part of the face [8].Due to the special nature of the blood supply to the human nose and surrounding area, it is possible (although very rare) for retrograde infections from the nasal area to spread to the brain causing cavernous sinus thrombosis, meningitis or brain abscess. This is possible because of venous communication (via the ophthalmic veins) between the facial vein and the cavernous sinus [9, 10].
If the cavernous sinus is infected, it can cause the blood within the sinus to clot resulting in a cavernous sinus thrombosis. This affects the structures that are going through it or surround it. Inside cavernous sinus, constriction of the following nerves can be found: CN III (oculomotor nerve), CN IV (trochlear nerve), CN VI (abducens nerve), CN V (trigeminal nerve), specifically V1 (ophthalmic nerve) and V2 (maxillary nerve) branches. Failure of each of the nerves listed above will manifest in loss of function of the specific muscle, gland or a parasympathetic innervations (from CN III). In addition, it is possible that inflammation of the cavernous sinus will result in compression of the optic chiasm (resulting in vision problems) and/or the pituitary gland. Failure of CN III will result in loss of function of the following muscles: medial rectus, superior rectus, inferior rectus, as well as muscles that are responsible for opening the eyelid:levator palpebrae superioris muscle and the superior tarsal muscle (Muller’s muscle). CN III damage also results in loss of parasympathetic innervation of the eye (loss of pupillary constriction and lens accommodation).
| Symptoms of cavernous sinus thrombosis: [11] |
|---|
| Severe headache |
| Swelling, redness, or irritation around one or both eyes (Periorbital edema) |
| Drooping eyelids |
| Inability to move the eye |
| High fever |
| Pain or numbness around the face or eyes |
| Fatigue |
| Vision loss or double vision |
| Seizures |
The clinical symptoms at presentation may not be of the classical type, but they may be masked or changed due to a previous antibiotic therapy which was received by the patient.
Materials and Methods
The present study comprising of 08 patients of CST was carried out from 2007 to 2012. On admission, a thorough clinical history was taken and a clinical examination was done for all the patients. A haemogram, all routine investigations and the culture and sensitivity (c/s) of the discharge was done in all the cases, Blood culture was done in 02 cases and CSF culture in 01 case. The patients were subjected to high resolution computed tomography of nose and PNS with brain plain and contrast study. All patients had radiographic evidence of cavernous sinus thrombosis. An ophthalmological opinion was taken in all the cases to rule out papill-oedema. The pediatrician opinion was taken in all the cases.
The patients were started on an intravenous antibiotic combination which consisted of ceftrioxone, metronidazole and amikacin, on admission. This combination of antibiotics was chosen to cover the mixed flora which was found in these cases and a change in the antibiotics was made, based on the c/s results.
Observations
Ten patients were identified, but only 08 patients’ records were available for review.
Age and sex
Six male and two female patients were included in this study. The age of the patients ranged from 06 to 16 years, with mean of 11.2 years. Six patients (75 %) were from rural areas and of poor socioeconomic status. The time interval between the onset of the symptoms and the seeking of medical advice ranged between 04 to 10 days (average 6.5 days). Surgical intervention of the primary source of infection was done. The antibiotics were continued for 14 to 21 days (average 16.5 days). The mean follow-up was 07 months (range 03–12 months).
Symptoms/Signs
The clinical symptoms and signs have been detailed in (Table 1).
Table 1.
Symptoms & Signs
| S. No | Symptom/Signs | No. of patients | % |
|---|---|---|---|
| 1 | Nasal discharge/Septic focus | 08 | 100.0 |
| 2 | Nasal pain | 07 | 100.0 |
| 3 | Fever | 08 | 100.0 |
| 4 | Severe headache | 06 | 75.0 |
| 5 | Vomiting | 04 | 50.0 |
| 6 | Periorbital puffiness | 06 | 75.0 |
| 7 | Lid edema | 06 | 75.0 |
| 8 | Drooping eyelids (Ptosis) | 06 | 75.0 |
| 9 | Proptosis | 05 | 62.5 |
| 10 | Inability to move the eye (Ophthalmoplegia) | 05 | 62.5 |
| 11 | Pain or numbness around the face or eyes | 05 | 62.5 |
| 12 | Papilledema | 05 | 62.5 |
| 13 | Vision loss or double vision | 04 | 50.0 |
| 14 | Altered sensorium | 03 | 37.5 |
Nasal discharge, pain and fever were the most common symptoms which were present in all 08 patients.
Discussion
Cavernous sinus thrombosis is a serious life threatening condition with a high mortality. It has been improved markedly because of an early awareness of the condition and prompt initiation of parenteral antibiotics. Usually it is unilateral but due to inter-cavernous communication the other side is also affected [12].
In 1925 Eagleton suggested six often quoted, points as guides to the diagnosis of cavernous sinus thrombosis: (1) Known site of infection, (2) Septicemia, (3) Early signs of venous congestion such as full retinal veins (4) Ocular nerve, ophthalmic or maxillary nerve deficits, (5) Abscess or Phlebitis contiguous to the cavernous sinus and (6) Signs of an intracranial infection (e.g. headache, stiff neck, obtundation). [13] Whereas not all of these points must be present to initiate expectant management, they should be sought.
Septic cavernous sinus thrombosis has rarely been reported in children with variable outcome. Allergic rhinitis, a neglected untreated nasal furuncle and paranasal sinusitis can lead to cavernous sinus thrombosis. [14, 15] CST is usually a complication of a facial infection. Patients with CST present with hyperthermia, headache, vomiting, proptosis and involvement of the 3rd, 4th and 6th cranial nerves. Headache is the most common symptom, usually preceding fevers, periorbital edema, and cranial nerve signs [16]. The precise mechanism of headache in such patients who have no intracranial involvement remains unknown. It might be due to the irritation or stretching of nerve fibers in the walls of the affected sinus [17]. The diagnosis of CST has become increasingly difficult because of the previous antibiotic therapy and the vague non specific symptoms. In our study, the patients were from rural areas where the services of qualified ENT surgeons were not available and the patients had already been treated with antibiotics for a variable period by the local doctors. The Computerized Tomography (CT) scan and MRI are the mainstay of the investigations in CST. Precise orientation of thin cuts, concentrated contrast medium, multiplanar reconstruction, and special window settings are all needed. In the last decade, Magnetic Resonance Angiography (MRA) and Magnetic Resonance Venography (MRV) had been used to differentiate the slow venous flow from the occlusive thrombus.MR angiography is quite sensitive to blood flow and differentiates thrombosis from slow flow. It has several advantages; it is a non-invasive technique and does not require the use of intravenous contrast agent, it can be performed rapidly and does not use ionizing radiation [18]. In our series, all the patients underwent High resolution Contrast enhanced CT scan of the nose, PNS and brain with fine cuts (Figs 1, 2, 3, 4; Table 2).
Fig. 1.

Proptosis of Left eye with bilateral lid edema, with septic focus nasal dorsum and columella
Fig. 2.
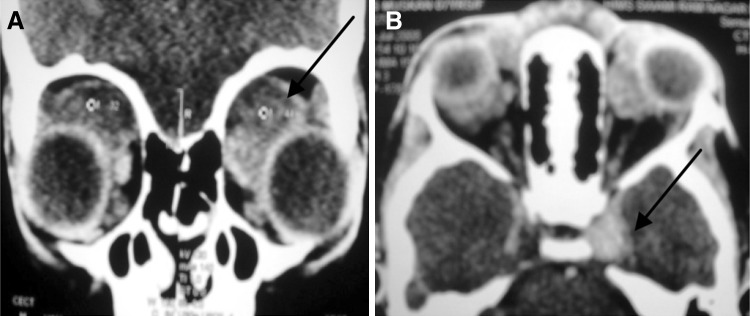
CT scan revealing. a Bilateral orbital abscess. b Radio-opacity right side cavernous sinus (Cavernous sinus thrombosis) and increase in diameter and enhancement of left cavernous sinus
Fig. 3.

Bilateral lid edema, with septic focus nasal dorsum— a At presentation, b Post treatment (07th day)
Fig. 4.

Bilateral lid edema, with septic focus nasal cavity and ethmoids
Table 2.
Site of nasal septic focus, microbial organism and antibiotic used
| Pt. | Age/Sex | Septic focus | Duration to onset (days) | Pus (Culture- organism) | Treatment given (I.V.) | Duration of treatment (days) | Outcome |
|---|---|---|---|---|---|---|---|
| 1 | 7/M | Lt nasal vestibule | 05 days | No growth for bacterial culture | Ceftriaxone, metronidazole and amikacin | 16 | Complete recovery |
| 2 | 11/F | Nasal dorsum | 04 days | S. aureus | Ampicillin, metronidazole and vancomycin | 14 | Complete recovery |
| 3 | 16/M | Lt Nasal cavity/Ethmoid sinus | 06 days | S. aureus Streptococcus sp | Piperacillin + tazobactam and vancomycin, + dexamethasone | 18 | Ocular weakness |
| 4 | 15/M | Nasal dorsum | 07 days | S. aureus | Ceftriaxone, metronidazole and amikacin | 14 | Complete recovery |
| 5 | 12/M | Lt nasal cavity/Ethmoid sinus | 10 days | S. aureus | Piperacillin + tazobactam and vancomycin, | 21 | Complete recovery |
| 6 | 11/F | Rt nasal vestibule | 05 days | S. aureus | Ceftriaxone, metronidazole and amikacin | 14 | Complete recovery |
| 7 | 6/M | Bilateral nasal cavity/Ethmoid sinus | 06 days | Streptococcus sp | Amoxycillin + clavulanic acid, metronidazole, amikacin + dexamethasone | 21 | Ocular weakness Vision Loss (Partial) |
| 8 | 12/M | Lt nasal vestibule and columella | 09 days | No growth for bacterial culture | Amoxycillin + clavulanic acid, metronidazole and amikacin | 14 | Complete recovery |
+ Analgesics & Local decongestants given in all
Features that distinguish CST from orbital cellulitis include cranial nerve dysfunction, bilateral eye involvement, and mental status changes. The diagnosis of septic cavernous sinus thrombosis requires a high index of suspicion and confirmation by imaging; early diagnosis and surgical drainage of the underlying primary source of infection in conjunction with long-term intravenous antibiotic therapy are critical for an optimal clinical outcome [11].
Immediate empiric antibiotic coverage must include gram-positive, gram-negative, and anaerobic bacteria coverage and can be narrowed as cultures and sensitivities become available. There is no agreement about the best antibiotic to use. Surgical intervention of the primary source of infection, including the nasal septum, nasal sinus, and face, is the primary treatment modality. Empirical antimicrobial therapy usually depends on the antecedent clinical condition and must include coverage for MRSA. An empirical combination, such as parenteral metronidazole, vancomycin, and ceftriaxone, will achieve reasonable CSF and brain penetration and is likely to be active against S. aureus (including CAMRSA strains) as well as the usual pathogens. After the initial empirical antibiotics it is important to deescalate antibiotic. Antimicrobial selection can be based on positive cultures. Duration of parenteral antimicrobial therapy should be at least 3–4 weeks [19].
The role of anticoagulation as an adjuvant to antibiotic therapy remains controversial. Administration of low-molecular-weight heparin was demonstrated to be effective in improving outcomes of venous thrombosis. However, there is no information regarding its usefulness in secondary thrombosis from infective process [20].
Conclusion
Cavernous sinus thrombosis, although it is a rare complication, with the advent of antibiotics, It can still be seen in populations with access to poor medical facilities and in poor socioeconomic groups. An awareness of this complication is necessary for an early diagnosis and a prompt treatment. High index of suspicion is important. The favorable outcome depends upon prompt diagnosis and early institution of antibiotics [21].
References
- 1.Shaw RE. Cavernous sinus thrombophlebitis. A review. Br J Surg. 1952;40:40–48. doi: 10.1002/bjs.18004015908. [DOI] [PubMed] [Google Scholar]
- 2.Gupta MC, Ahuja OP, Kumar S. Cavernous sinus thrombosis. Indian J Med Sci. 1970;24:748–753. [PubMed] [Google Scholar]
- 3.De Veber G, Andrew M, Adams C, Bjornson B, Booth F, Buckley DJ, et al. Cerebral sinovenous thrombosis in children. N Engl J Med. 2001;345:417–423. doi: 10.1056/NEJM200108093450604. [DOI] [PubMed] [Google Scholar]
- 4.Jose J, Coatesworth AP, Anthony R, Reilly PG. Life threatening complications after partially treated mastoiditis. BMJ. 2003;327:41–42. doi: 10.1136/bmj.327.7405.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ahmad R, Salman R, Islam S, Rehman A (2009) Cavernous sinus thrombosis as a complication of sphenoid sinusitis: a case report and review of literature. Internet J Otorhinolaryngol 12(1)
- 6.Tveteras K, Kristensen S, Dommerby H. Septic cavernous and lateral sinus thrombosis: the modern diagnostic and therapeutic principles. J Laryngol Otol. 1988;2:877–892. doi: 10.1017/S0022215100106711. [DOI] [PubMed] [Google Scholar]
- 7.Bassey OO, Elebute EA. Septic thrombosis of the cavernous sinus. West Afr Med J. 1968;17:39–41. [PubMed] [Google Scholar]
- 8.Maes U (1937) Infections of the dangerous areas of the face. Annals Surg 106 (1): 1–10 [DOI] [PMC free article] [PubMed]
- 9.Osborn AG (1981). Craniofacial venous plexuses: angiographic study. AJR 136: 139–143 [DOI] [PubMed]
- 10.Zhang J, Stringer MD (2010). Ophthalmic and facial veins are not valveless. Clin Exp Ophthalmol 38 (5): 502–510 [DOI] [PubMed]
- 11.Deshmukh V, Lakhkar B, Wagha J (2008) Cavernous sinus thrombosis. Pediatr Oncall J 5(5)
- 12.Sofferman RA. Cavernous sinus thrombophlebitis secondary to sphenoid sinusitis. Laryngoscope. 1983;93:797–800. doi: 10.1288/00005537-198306000-00017. [DOI] [PubMed] [Google Scholar]
- 13.Chandra K, Varshney S, Alam J, Nawab Z (1995) Traumatic-lateral sinus thrombosis. Bihar J Otolarygol 15:5–8
- 14.Canon ML, Antonio BL, McCloskey JJ, Hines MH, Tobin JR, Shetty AK. Cavernous sinus thrombosis complicating sinusitis. PediatrCrit Care Med. 2004;5:86–88. doi: 10.1097/01.PCC.0000102385.95708.3B. [DOI] [PubMed] [Google Scholar]
- 15.Holzmann D, Willi U, Nadal D. Allergic rhinitis as a risk factor for orbital complication of acute rhinosinusitis in children. Am J Rhinol. 2001;15(6):387–390. [PubMed] [Google Scholar]
- 16.DiNubile MJ. Septic thrombosis of the cavernous sinuses. Arch Neurol. 1988;45(5):567–572. doi: 10.1001/archneur.1988.00520290103022. [DOI] [PubMed] [Google Scholar]
- 17.Boukobza M, Crassard I, Bousser MG. When the ‘dense triangle’ in dural sinus thrombosis is round. Neurology. 2007;69:808. doi: 10.1212/01.wnl.0000275548.60964.bf. [DOI] [PubMed] [Google Scholar]
- 18.Daniels DL, Czervionke LF, BonnerilleJF, Cattin F, Mark LP, PechP, et al (1988) MR of the cavernous sinus: valve of spin echo and gradient recalled echo images. AJR Am J Roentgenol 151:1009–14.30 [DOI] [PubMed]
- 19.Swaminath D, Narayanan R, Orellana-Barrios MA, Temple B. Necrotizing fasciitis of the nose complicated with cavernous sinus thrombosis. Case Rep Infect Dis. 2014;2014:914042. doi: 10.1155/2014/914042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Samaha M, Prudencio JA, Tewfik TL, Schloss MD. Bilateral lateral sinus thrombosis associated with otitis media and mastoiditis. J Otolaryngol. 2001;30:250–253. doi: 10.2310/7070.2001.20187. [DOI] [PubMed] [Google Scholar]
- 21.Verma R, Junewar V, Singh RK, Ram H, Pal US. Bilateral cavernous sinus thrombosis and facial palsy as complications of dental abscess. Natl J Maxillofac Surg. 2013;4:252–255. doi: 10.4103/0975-5950.127664. [DOI] [PMC free article] [PubMed] [Google Scholar]


