Abstract
Jugular phlebectasia is fusiform dilatation of internal jugular vein seen in childrens. It usually occurs in children but can occur at any age. It usually presents as unilateral swelling in the neck found during coughing and shouting. It is usually asymptomatic, so it is often ignored or misdiagnosed. Differential diagnosis include laryngocele, cavernous hemangioma, cystic hygroma, branchial cyst. Treatment is usually conservative as complications like thrombosis and horners syndrome are very rare. Non invasive investigations like Doppler sonogram and are usually done to diagnose this condition. We report two cases of jugular phlebectasia, who presented to our out patient department with history of swelling in the right side of neck which increases on crying and shouting. Doppler sonogram and ultrasound was done to diagnose the condition. There seems be lack of knowledge among medical fraternity in various specialities. So a questionnaire was prepared to assess the knowledge among resident doctors, general practitioners, Otorhinolaryngologists, paediatricians. Questionnaire was posted in social networking sites and the feedback was obtained. Out of the 150 interns in our hospital, only one (0.66 %) was able to explain about the condition. In general practitioners group containing 369 respondents, only 4 (1.08 %) knew the condition and have seen patients. A pediatricians group containing 312 respondents only 23 (7.37 %) pediatricians knew the condition, 289 (92.62 %) persons had no idea about the treatment. Otorhinolaryngologists group containing 328 respondents. 21 (6.40 %) knew the condition, 293 (89.3 %) have no idea. The Chi square test shows that the specialty of the respondent like pediatrician and ENT practitioner have more knowledge than the other for jugular phlebectasia at p < 0.0001.
Keywords: Jugular phlebectasia, Jugular ectasia, Laryngocele, Cyst
Introduction
Phlebectasia is a term which denotes abnormal saccular or fusiform dilatation of veins [1]. Internal jugular phlebectasia is fusiform dilatation of the jugular vein which is thought to be of congenital in origin. It usually occurs in children, but can occur at any age and affects both genders. It usually presents as unilateral neck swelling which increases on valsalva manoeuvre. It is usually asymptomatic, so it is often ignored or misdiagnosed. Differential diagnosis include laryngocele, cavernous hemangioma, cystic hygroma, branchial cyst. Treatment is usually conservative as complications like thrombosis and horners syndrome are very rare. Non invasive investigations like Doppler sonogram and ultrasonogram are usually done to diagnose this condition.
Case 1
A 6 year old boy was accompanied by his mother with history of swelling in the right side of neck for 6 months, found during crying (Fig. 1a). There was no history of trauma. Physical examination was normal at rest but showed a soft, non tender compressible swelling of size 3 × 3 cm in anterior triangle of neck during valsalva manoeuvre. Swelling was not attached to any deeper structures. There was no murmur or bruae. We decided to do ultrasonogram and Doppler. Ultrasound showed a normal study on gray scale imaging when the patient is at rest, while during valsalva there was a fusiform dilatation of the internal jugular vein (IJV) on the right side when compared to the left side as shown in Fig. 1b. Colour Doppler study revealed complete filling of the dilated right IJV with intermittent aliasing suggesting mild turbulence (Fig. 2). Contrast enhanced computed tomography of the neck also revealed the dilated right IJV when compared to the left (Fig. 3).
Fig. 1.
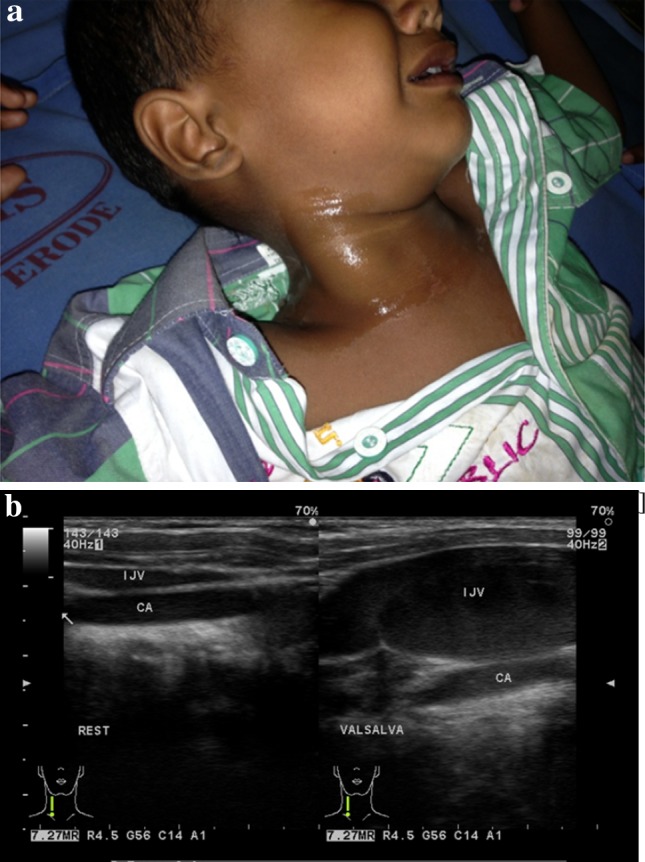
a Swelling on crying. b Ultrasound picture (B mode scan) of the internal jugular vein (IJV) at rest and valsalva
Fig. 2.

Colour doppler revealed a complete luminal filling of the vein
Fig. 3.

Post contrast computed tomography of the neck shows dilated internal jugular vein on the right side when compared to the left
Case 2
A 10 year old boy was referred from a pediatrician as a case of laryngocele. Patient presented with a history of swelling in the right side of neck which increases in size on crying, shouting and valsalva (Fig. 4) There is no history of trauma. On examination swelling appears in the neck during straining and coughing, but it is soft, non compressible, non tender. There was no venous hum or bruae. Patient was subjected to ultrasound and colour Doppler, which again confirmed it as jugular phlebectasia.
Fig. 4.

Child at rest and during valsalva
Though there are number of case reports in literature, there seems be lack of knowledge among medical fraternity in various specialities. It is often misdiagnosed or under reported as there is a tendency to report only operated cases. Lack of knowledge could be attributed to text books in various specialities ignoring to mention about the condition.
A questionnaire is prepared to assess the knowledge among resident doctors, general practitioners, otorhinolaryngologists, paediatricians. Questionnaire evaluated whether they know about the condition or not, number of cases seen, side of the lesion, unilateral or bilateral, operated or not, any complications seen, common investigations done. Questionnaire was posted in social networking sites and the feedback was obtained.
Questionnaire
What is jugular phlebectasia?
Have you ever seen a case of jugular phlebectasia?-yes or no. If yes
2a No of cases seen
(a)1–2 (b) 2–5 (c)more than 5
Have you ever seen a operated case?
Have you seen any complications associated with condition- yes or no. If yes,
(a) Rupture (b) Horners syndrome (c) Thrombosis
Results
We enquired 150 interns in our hospital, all of them participated in the study and the questionnaire was posted in a social networking site. General practitioners group containing 932 members were requested to participate in the study and questionnaire was presented to them. Of which, only 369 responded. A pediatricians group containing 654 members was selected, of which only 312 (47.7 %) responded. Otorhinolaryngologists group containing 721 was requested, of which 328 (52.8 %) responded. The Chi square test shows the specialty of the respondent is independent of response rate at p < 0.0001 (as represented in Table 1; Fig. 5).
Table 1.
Frequency and percentage distribution of medical practitioner who have participated in the study of knowledge of jugular phlebectasia
| Speciality | Response | Non response | Total | χ2 value | Significant |
|---|---|---|---|---|---|
| Interns | 150 (100 %) | 0 (0 %) | 150 | 193.14 | p < 0.0001 |
| General practitioners | 369 (39.6 %) | 563 (60.4 %) | 932 | ||
| Paediatricians | 312 (47.7 %) | 342 (52.3 %) | 654 | ||
| Otorhinolaryngologists | 328 (52.8 %) | 293 (47.2 %) | 621 | ||
| Total | 1,159 (49 %) | 1,198 (51 %) | 2,357 |
Fig. 5.
Response by various categories of doctors
We presented the questionnaire to the interns in our hospital, out of the 150 interns, only one (0.66 %) was able to explain about the condition. In General practitioners group containing 369 respondents only 4 (1.08 %) knew the condition and have seen patients. A pediatricians group containing 312 respondents only 23 (7.37 %) pediatricians knew the condition, 289 (92.62 %) persons had no idea about the treatment. Otorhinolaryngologists group containing 328 respondents. 21 (6.40 %) knew the condition, 293 (89.3 %) have no idea. The Chi square test shows that the specialty of the respondent like pediatrician and ENT practitioner have more knowledge than the other for jugular phlebectasia at p < 0.0001 as shown in Table 2.
Table 2.
Frequency and percentage distribution of medical practitioner having the knowledge regarding the jugular phlebectasia
| Specialty | Knowledge of the jugular phlebectasia yes | No knowledge of the jugular phlebectasia | Total | χ2 value | p value |
|---|---|---|---|---|---|
| Interns | 1 (0.66 %) | 149 (99.37 %) | 150 | 25.15 | p < 0.0001 |
| General practitioners | 4 (1.08 %) | 365 (98.92 %) | 369 | ||
| Paediatricians | 23 (7.37 %) | 289 (92.63 %) | 312 | ||
| Otorhinolaryngologists | 21 (6.40 %) | 307 (93.60 %) | 328 | ||
| 49 (4.23 %) | 1,110 (95.77 %) | 1,159 |
The Chi square test shows that the specialty of the respondent like pediatrician and ENT practitioner have seen jugular phlebectasia at p < 0.005 (Tables 3, 4).
Table 3.
Frequency and percentage distribution of medical practitioner who have seen jugular phlebectasia patients
| Specialty | Yes | No | Total | χ2 value | p value |
|---|---|---|---|---|---|
| Interns | 0 (0 %) | 150 (100.00 %) | 150 | 13.26 | p < 0.005 |
| General practitioners | 4 (1.1 %) | 365 (98.9 %) | 369 | ||
| Paediatricians | 9 (2.9 %) | 303 (97.1 %) | 312 | ||
| Otorhinolaryngologists | 15 (4.6 %) | 313 (95.4 %) | 328 |
Table 4.
Frequency and percentage distribution of medical practitioner who either follow up or do surgery for jugular phlebectasia patients
| Speciality | Follow up | Surgery | Total |
|---|---|---|---|
| General practitioners | 1 (0.27 %) | – | 1 (0.09 %) |
| Paediatricians | 7 (2.24) | 2 (0.64 %) | 9 (0.78 %) |
| Otorhinolaryngologists | 8 (2.43 %) | 7 (2.13 %) | 15 (1.29 %) |
| Total | 16 (1.38 %) | 9 (0.78 %) | 25 (2.16 %) |
Out of 1,159 medical practitioner of our study, total number of patients seen by them were 25 (2.16 %).which shows that prevalence of the disease was 2.16 %. Out of the 25 patients most of the patients by the Otorhinolaryngologists 15 (60 %) and Pediatricians 9 (36 %). The General Practitioner had a small number, only one (4 %).
Discussion
Internal jugular phlebectasia first described by Zukschwerdt [2]. Though the exact etiology is not known, a number of factors is proposed which include anomalous reduplication of IJV, mechanical compression of right or left brachiocephalic vein, idiopathic [3, 4]. The most common cause of a neck mass that becomes visible or increases in size with valsalva manoeuvre is laryngocele, followed by jugular ectasia and superior mediastinal tumour cysts. Other differential diagnoses include, pharyngeal pouch, external laryngeal diverticulum, cavernous haemangioma.
The IJV is the most commonly affected and in most cases it is unilateral and right side. Though there are reports of association with childhood asthma [5], both of our patients were non asthmatic. Diagnosis can be done by using ultrasonography with Doppler, CECT, CT Angiography and MR venography [6]. Though ultrasound gives a accurate extent of the lesion and its relationship to the underlying structures, Doppler ultrasonogram done during valsalva manouver gives a accurate diagnosis. CECT has obvious advantage of delineating the adjacent structures.
Surgical intervention was done in the past with significant mortality and morbility. Since it is a benign condition, conservative management with regular follow up is advised. Surgical management is planned only if it presents with complications like thrombosis, impending pulmonary embolism, horners syndrome. Congestive cardiac failure, spontaneous rupture which is very rare [7]. There is a rare chance that a thrombosed jugular phlebectasia can mimic a cervical adenitis and attempt to excise or draining it can lead to disaster.
Conclusion
Though jugular phlebectasia is a rare condition, it is not mentioned in any of the standard otolaryngology, pediatrics, pediatrics surgery textbooks. This makes the situation much worse, leading to misdiagnosis or wrong treatment. So it is highly recommended that this condition should be mentioned in undergraduate and postgraduate textbooks in relevant fields. This will translate into correct diagnosis and unnecessary mismanagement.
Contributor Information
Rajprakash Dharmapuri Yaadhavakrishnan, Email: dyrajprakash@gmail.com.
Nagendran Navaneethan, Email: naugendran@yahoo.com.
References
- 1.Gerwig WH., Jr Internal jugular phlebectasia. Ann Surg. 1952;135:130–133. doi: 10.1097/00000658-195201000-00021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zukschwerdt L. Seltene localisation einer venectasie. Dtsch Z Chir. 1929;216:283–285. doi: 10.1007/BF02797034. [DOI] [Google Scholar]
- 3.Paleri V, Gopalakrishman G. Jugular phlebectasia: theory of pathogenesis and review of literature. Int J Pediatr Otorhinolaryngol. 2001;57:155–159. doi: 10.1016/S0165-5876(00)00435-3. [DOI] [PubMed] [Google Scholar]
- 4.Yokomori K, Kubo K, Kanamori Y, Takemura T, Yamamoto T. Internal jugular phlebectasia in two siblings: manometric and histopathologic studies of the pathogenesis. J Pediatr Surg. 1990;25:762–765. doi: 10.1016/S0022-3468(05)80014-4. [DOI] [PubMed] [Google Scholar]
- 5.Kwok KL, Lam HS, Ng DKK. Unilateral right-sided internal jugular phlebectasia in asthmatic children. J Paediatr Child Health. 2000;36:517–519. doi: 10.1046/j.1440-1754.2000.00529.x. [DOI] [PubMed] [Google Scholar]
- 6.Desai SJ, Rajan S, Jain T. Anterior jugular vein aneurysm: diagnosis by CT angiography. Indian J Radiol Imaging. 2002;12:369–370. [Google Scholar]
- 7.Swami SLH, Nambiar S. Focal ectasia of internal jugular vein. Med J Armed Forces India. 2009;65:3. doi: 10.1016/S0377-1237(09)80029-4. [DOI] [PMC free article] [PubMed] [Google Scholar]



