Abstract
Neurocognitive dysfunction is a major clinical consequence in patients with obstructive sleep apnea syndrome (OSAS). The effects of continuous positive airway pressure (CPAP) treatment, as the gold standard of treatment in OSAS, on this major complication are controversial. The duration and compliance of CPAP are thought to be important factors but evidence is lacking. This study is designed to evaluate the effects of immediate (one night), long-term (3 months) influence and the compliances of CPAP treatment on the neurocognitive function in OSAS patients. We enrolled newly diagnosed severe OSAS patients. Neurocognitive function test battery, CANTAB (Cambridge Neuropsychological Test Automated Battery), was performed before, one night and 3 months of CPAP treatment. Patients with CPAP compliance rate ≥ 70 % and < 50 % were grouped into good and poor adherence subjects, respectively. Fourteen patients were enrolled in final analyses. Six of them were in poor compliant group. Improvements in attention domain were found in all subjects after one-night treatment and maintained till three-month follow-up. Additional improvements in some attention performances and visual memory performances were gained only after three-month treatment. Significant changes of decision-making and response control function were found between good and poor compliance groups after three-month treatment. CPAP can improve some neurocognitive function at the very first day used. Longer treatment of CPAP can additionally improve some other neurocognitive functions. Compliance of CPAP has influence on the recovery of neurocognitive functions in patients with severe OSAS.
Electronic supplementary material
The online version of this article (doi:10.1007/s12070-014-0777-4) contains supplementary material, which is available to authorized users.
Keywords: Compliance, Continuous positive airway pressure, Neurocognitive function, Obstructive sleep apnea syndrome, Outcome
Background
Obstructive sleep apnea syndrome (OSAS) is a common clinical sleep disorder that affects about 2–4 % of middle-aged adults [1]. OSAS has been recognized as a significant problem associated with a wide range of physical and psychological consequences, including hypertension, increased risk of vascular disease and accident, depression, poor quality of life, attention deficit, poor alertness and cognitive problems [2–6]. The most common cognitive problems reported in OSAS patients are deficit on attention, memory and learning abilities, motor performance, constructional abilities and executive functions [2, 4].
Continuous positive airway pressure (CPAP) therapy is the first-line treatment for OSAS [6]. Adequate CPAP treatment can ameliorate the cardiovascular morbidity and mortality in OSAS patients [5–7]. Patients do experience improvement on spirit at the very first day after CPAP usage but no report had ever focused on this. Compliance is the major concerned when chose CPAP as the treatment in patients with OSAS. However, the compliance of CPAP treatment in most sleep center is as low as 30–60 % [8]. The effects of CPAP treatment on the cognitive function are controversial with various results [2, 4, 9–11]. Various CPAP compliances, different measurement tools and condition are factors confounding these results [9]. However, the evidence about the duration of CPAP and the compliance with the changes of neurocognitive function is little.
This study is to evaluate the immediate (one night) and longer (3 months) period of CPAP treatment on the neurocognitive function in patients with OSAS. And we also compare the improvement of neurocognitive function between patients of different compliance.
Methods
Clinical Patients
The Research and Ethics Committee of the Chang Gung Medical Foundation approved the study protocol in advance (number: 98-3945B), and each patient provided informed written consent before participating. We prospectively included patients presenting to the Sleep Clinic for overnight polysomnography (PSG) between January 2010 and December 2010 who were more than 20 years old and had a chief complaint of habitual snoring. Because neurocognitive test battery use touch panel, participants who were left-handed dominated and had abnormal or not corrected-to-normal visual acuity were excluded. We excluded patients who had apnea-hypopnea index less than 30/h and who ever received oral appliance, surgical and CPAP treatment for OSAS. We also excluded subjects who had major medical disease because of these patients may have cognitive impairment, such as heart failure, chronic renal failure, liver cirrhosis, chronic obstructive pulmonary disease, hematological disease, autoimmune disease and cancer [12–18]. Patients with sleep disorder other than OSAS such as restless legs syndrome and periodic limb movements, neurological disorder, dementia, major psychiatric disorder, handicap, psychomotor retardation and had current use of any psychoactive or hypnotic medications were also excluded.
Polysomnography
Conventional overnight PSG (Embla N7000; Medcare, Reykjavik, Iceland) was performed in a sleep laboratory between the hours of 2200 and 0600–0700 to document sleep parameters and architecture. OSAS was diagnosed according to the recommendations of the American Academy of Sleep Medicine 2005 which apnea was defined as a cessation of airflow for at least 10 s and hypopnea was defined as an abnormal respiratory event with at least 30 % reduction in airflow compared to the baseline value and lasting at least 10 s and with equal or more than a 4 % oxygen desaturation or an arousal [19].
Assessment of Daytime Sleepiness
The subject’s daytime sleepiness was assessed by Epworth Sleepiness Scale (ESS). The eight-item ESS evaluated daytime somnolence in eight specific situations and generated a total score ranging from zero (best) to 24 (worst). A Mandarin Chinese version of the ESS was used with permission in this study [20].
Neurocognitive Task Battery
Cambridge Neuropsychological Test Automated Battery (CANTAB), a widely used tool for assessment of patterns of cognitive function [21–24], was performed in our study. CANTAB included 4 major domains: attention domain, visual memory domain, decision-making and response control domain and executive function, working memory and planning domain. Each domain includes 2–5 subtests. According to prior empirical study, we excluded some of the tests in the CANTAB battery show significant improvements in performance with practice, and significant influenced by cultural difference [25]. Meanwhile, considering empirical data from OSAS associated neurocognitive function performance, we selected nine subtests from CANTAB included reaction time and rapid visual information processing from attention domain, delayed matching to sample from visual memory domain, information sampling task and stop signal task from decision-making and response control domain and intra/extradimensional set shift and spatial span from executive function, working memory and planning domain.
All participants took CANTAB three times: the first test took before any treatment, then the second test at the very first day after CPAP treatment, and 3 months after CPAP treatment. Each time, the task was performed by our subjects during 9:00–12:00 a.m. Six healthy subjects without sleep apnea were invited to repeat this CANTAB for two consecutive days to evaluate the learning effect.
Continuous Positive Airway Pressure Therapy
Optimal therapeutic pressure levels were obtained from all subjects in advance. All participants were educated and applied whole night CPAP in sleep laboratory at first night. C-Flex™ (Respironic) was used at home for 3 months. The compliance rate of CPAP was downloaded from the record chip of CPAP machine every month.
Definition of Poor and Good Compliant Group
Compliance at home was objectively reported by software. The compliance rate is calculated as the days of use more than 4 h divided by total record days. Patients with compliance rate equal to or more than 70 % were grouped into good compliant subjects [26]. In order to clearly show the difference between groups, only patients with compliance rate less than 50 % were selected as poor adherent group.
Statistical Analysis
Data collected from CANTAB were continuous variables. Nonparametric two independent samples test, Mann–Whitney U test, was used to compare the variables between poor and good compliant groups. For excluding practicing effects, repeat measures ANOVA test was used for pre-treatment and post treatment as well as between study and control groups comparison and observed power (using alpha = 0.05) estimation. All about tests were two-tailed, and a p value less than 0.05 was considered statistically significant. Statistical analyses were performed using Statistical Package for Social Sciences 15.0 for Windows (SPSS Inc., Chicago, IL, USA).
Results
Totally, 14 patients completed the study and were enrolled in final analyses. Six of them were in poor compliant group. Table 1 shows the characteristics in overall subjects with poor and good adherent groups. No difference in baseline characteristic was found between poor and good compliant groups, except CPAP compliance rate.
Table 1.
Characteristics in overall subjects and in different CPAP compliant groups
| Overall (n = 14) | Poor adherence (n = 6) | Good adherence (n = 8) | p value | |
|---|---|---|---|---|
| Age (years) | 48.9 ± 7.2 | 47.8 ± 8.4 | 49.7 ± 6.7 | 0.70 |
| Male (%) | 93 | 83 | 100 | 0.25 |
| BMI (kg/m2) | 31.0 ± 5.1 | 33.3 ± 4.6 | 29.2 ± 5.1 | 0.09 |
| ESS score | 11.1 ± 6.6 | 14 ± 6.2 | 8.9 ± 6.3 | 0.15 |
| AHI (/h) | 63.6 ± 16.7 | 60.9 ± 16.3 | 65.7 ± 17.8 | 0.65 |
| Minimum O2Sat (%) | 68.1 ± 9.7 | 70.2 ± 7.1 | 66.6 ± 11.5 | 0.65 |
| Compliance rate (%)* | 62.1 ± 25.4 | 35.4 ± 8.6 | 82.2 ± 8.5 | <0.01 |
| Range of compliance rate (%) | − | 24.0–43.7 | 71.7–94.3 | − |
* comparing good compliant group with poor compliant group
CPAP continuous positive airway pressure; BMI body mass index; ESS Epworth sleepiness scale; O 2 Sat oxygen saturation
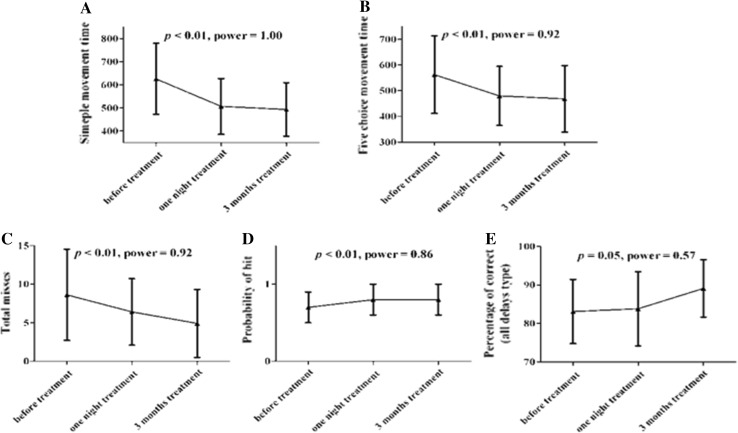
In the data after one night of CPAP treatment, we found significant improvements in parameters of attention domain (simple movement time and five-choice movement time of reaction time, total and probability of hits, total miss, and total correct rejections of rapid visual information process) and decision-making and response control domain (Mean color decision latency and mean box opening latency) (Fig. 1a–d and Table S1 in the online supporting information). Most of these parameters remain significantly improved after 3 months of CPAP treatment except the mean box open latency which has the trend of improvement but not significant (Fig. 1a–d and Table S1 in the online supporting information). Some parameters show significant changes after 3 months of CPAP treatment only, such as the total and percentage of correction in visual memory domain, sampling errors, total and percentage of correction, number of box open in decision-making and response control domain (Fig. 1e and Table S1 in the online supporting information).
Fig. 1.
Changes of neurocognitive function before and after continuous positive airway pressure treatment in all subjects. Improvements in parameters in reaction time of attention domain were found after one-night treatment and were maintained till 3 months treatment (a and b). Improvements in parameters in rapid visual information process of attention domain (c and d) and in delayed matching to sample of visual memory domain (e) were gained after three-month treatment, but not one-night treatment
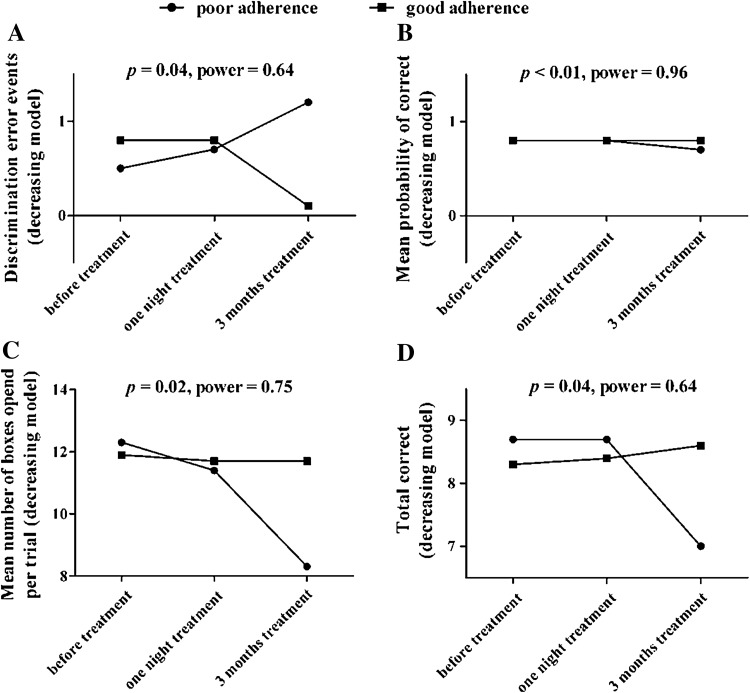
After 3 months of CPAP treatment, we found some neurocognitive functions are different between good and poor compliant groups in decision making and response control domain, such as discrimination error, mean percent and number of correction and mean number of box opened (Fig. 2, all data at Table S2 in the online supporting information). No significant difference was found in the changes of other neurocognitive functions between poor and good compliant groups.
Fig. 2.
Changes of information sampling task (decreasing model) in decision-making and response control tests domain after CPAP treatment in different compliant groups. After three-month CPAP treatment, improvements in discrimination error (a) and mean probability of correct (b) were found in good compliant group, while worsening or just maintenance in poor compliant group. Maintenance in mean number of boxes opened per trial (c) and total correct (d) were found in good compliant group after three-month CPAP treatment while worsening of these neurocognitive test results were gotten in poor compliant group
The improving score on the decision making domain is related to the latency of test performance which could be related to the improvement from reaction time; whereas the total and percentage of correct decision is not improved on these trials. But when we divided these score into good and poor complaint groups, we also noted that the correction and the decreasing of error improved on good complaint patients. In poor compliant group, these functions were getting worse (Fig. 2).
Discussion
Our study found that just one day of CPAP usage do improve the neurocognitive function in patients with OSAS especially on the reaction time and most of these effects persist till 3 months of treatment. Some changes on visual memory and decision making and response control were only noted after 3 months of CPAP treatment. The compliance rate of CPAP had influence on decision making and response control.
There is no report regarding the one-night effect of CPAP treatment on the neurocognitive function. Most of neurocognitive studies evaluate at least 4 weeks after CPAP treatment [9]. Orth et al. report improvement of reaction time in 2 and 42 days of CPAP treatment on their study for good compliant patients [27]. Our data confirm this observation and prove even one night of treatment can improve on the reaction time. Yang et al. report a longer reaction time noted at the first and 7th days after CPAP withdrawal from stable CPAP user and regain the reaction time at the first day after CPAP use [28]. However, due to data variability, his result did not get statistical significance.
Most studies found improvement in attention and vigilance after CPAP treatment, while improvement in executive function was less reported [9]. Similar to these findings, improvement in attention domain with no change in executive, working memory and planning domain were also found in our poor and good compliant groups, both after one-night and three-month treatment. Thus, our population is fitted to general clinical findings and our results are more reliable in general practice. Antic et al. showed improvement on verbal memory and executive function but not vigilance after 3 months of treatment [29]. Our study as well as Monasterio et al. reaches similar results that visual memory and attention function were improved after 3 months of CPAP treatment [30]. Lojander et al. showed that longer CPAP treatment (12 months) was not associated with greater improvement in neurocognitive function [10].
When examining the scores on the Information Sampling Task that differed significantly between the groups, poor compliant group showed decrease in the number of boxes opened per trial and decreased percentage of correction as well as increase in discrimination and sampling errors. This profile indicates premature decision making before obtaining enough information, and therefore may reflect an increase in impulsivity. The increase of direction errors on the Stop Signal Task in poor compliant group further supports this possibility.
Compliance of CPAP influences on the effect of treatment in OSAS patients. Engleman et al. showed benefit in mental flexibility, attention, and speed of information processing in patients treated by CPAP 3.5 h per night whereas no improvement was noted if treated by 2.8 h per night [31–34]. In our study, the correction and the decreasing of error in decision making and response control domains improved 3 months after CPAP treatment on good compliant patients. Whereas in poor compliant group, these functions were getting worse. Weaver et al. showed a dose response on day time function on CPAP duration after 3 months of treatment by MSLT and questionnaire [35]. Aloie et al. showed baseline neuropsychologic function have influence on the compliant rate and additional improvements in psychomotor speed and nonverbal learning was noted in compliant patients [36, 37]. Active intervention could improve the compliance rate in their study. This is not our cases because our baseline neurocognitive function is the same in both groups and no intervention was conducted in our patients.
Our study is subject to some limitations. Although the power of difference in changes of decision-making and response control domain were 0.64–0.96, relative small sample size may be criticized to statistically exclude the difference in changes of other domains. The small sample also excluded the possibility of changes in the other domains. A further study include more subjects is mandatory.
Our study shows that one night of CPAP treatment improves the neurocognitive function and the effect persists for 3 months. Different CPAP compliance can really influence the results of neurocognitive function test only in decision-making and response control domain in severe OSAS patients. Studies using other neurocognitive measures or randomizing subjects in different CPAP compliance should be done before explaining the lack of improvement in other domain of neurocognitive function is caused by inadequate CPAP compliance.
Electronic supplementary material
Acknowledgments
This study is supported by the Chang Gung Medical Foundation, Grant number CMRPG 360501.
Conflict of Interest
The authors declare that they have no conflict of interest.
Contributor Information
Shih-Wei Lin, Email: ec108146@cgmh.org.tw.
Yu-Ting Chou, Email: eaton6666@yahoo.com.tw.
Kuo-Chin Kao, Email: kck0502@cgmh.org.tw.
Li-Pang Chuang, Email: lpchuang1678@yahoo.com.tw.
Chien-Ming Yang, Email: yangcm@nccu.edu.tw.
Han-Chung Hu, Email: h3226@cgmh.org.tw.
Chung-Chi Huang, Email: cch4848@cgmh.org.tw.
Cheng-Ta Yang, Email: yang1946@cgmh.org.tw.
Ning-Hung Chen, Phone: +886 3 3281200, Email: ninghung@yahoo.com.tw.
References
- 1.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. New Engl J Med. 1993;328(17):1230–1235. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 2.Saunamaki T, Jehkonen M. A review of executive functions in obstructive sleep apnea syndrome. Acta Neurol Scand. 2007;115(1):1–11. doi: 10.1111/j.1600-0404.2006.00744.x. [DOI] [PubMed] [Google Scholar]
- 3.Sassani A, Findley LJ, Kryger M, Goldlust E, George C, Davidson TM. Reducing motor-vehicle collisions, costs, and fatalities by treating obstructive sleep apnea syndrome. Sleep. 2004;27(3):453–458. doi: 10.1093/sleep/27.3.453. [DOI] [PubMed] [Google Scholar]
- 4.Engleman HM, Douglas NJ. Sleep. 4: sleepiness, cognitive function, and quality of life in obstructive sleep apnoea/hypopnoea syndrome. Thorax. 2004;59(7):618–622. doi: 10.1136/thx.2003.015867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bradley TD, Floras JS. Obstructive sleep apnoea and its cardiovascular consequences. Lancet. 2009;373(9657):82–93. doi: 10.1016/S0140-6736(08)61622-0. [DOI] [PubMed] [Google Scholar]
- 6.Phillips B, Kryger MH. Management of obstructive sleep apnea syndrome: overview. In: Kryger MH, Roth T, Dement WC, editors. Principles and practice of sleep medicine. Philadelphia: Elsevier Saunders; 2005. pp. 1109–1121. [Google Scholar]
- 7.Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365(9464):1046–1053. doi: 10.1016/S0140-6736(05)71141-7. [DOI] [PubMed] [Google Scholar]
- 8.Weaver TE, Sawyer AM. Adherence to continuous positive airway pressure treatment for obstructive sleep apnoea: implications for future interventions. Indian J Med Res. 2010;131:245–258. [PMC free article] [PubMed] [Google Scholar]
- 9.Sanchez AI, Martinez P, Miro E, Bardwell WA, Buela-Casal G. CPAP and behavioral therapies in patients with obstructive sleep apnea: effects on daytime sleepiness, mood, and cognitive function. Sleep Med Rev. 2009;13(3):223–233. doi: 10.1016/j.smrv.2008.07.002. [DOI] [PubMed] [Google Scholar]
- 10.Lojander J, Kajaste S, Maasilta P, Partinen M. Cognitive function and treatment of obstructive sleep apnea syndrome. J Sleep Res. 1999;8(1):71–76. doi: 10.1046/j.1365-2869.1999.00141.x. [DOI] [PubMed] [Google Scholar]
- 11.Henke KG, Grady JJ, Kuna ST. Effect of nasal continuous positive airway pressure on neuropsychological function in sleep apnea-hypopnea syndrome. A randomized, placebo-controlled trial. Am J Respir Crit Care Med. 2001;163(4):911–917. doi: 10.1164/ajrccm.163.4.9910025. [DOI] [PubMed] [Google Scholar]
- 12.Biegler KA, Chaoul MA, Cohen L. Cancer, cognitive impairment, and meditation. Acta Oncol. 2009;48(1):18–26. doi: 10.1080/02841860802415535. [DOI] [PubMed] [Google Scholar]
- 13.Zuccala G, Cattel C, Manes-Gravina E, Di Niro MG, Cocchi A, Bernabei R. Left ventricular dysfunction: a clue to cognitive impairment in older patients with heart failure. J Neurol Neurosurg Psychiatry. 1997;63(4):509–512. doi: 10.1136/jnnp.63.4.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koushik NS, McArthur SF, Baird AD. Adult chronic kidney disease: neurocognition in chronic renal failure. Neuropsychol Rev. 2010;20(1):33–51. doi: 10.1007/s11065-009-9110-5. [DOI] [PubMed] [Google Scholar]
- 15.McAndrews MP, Farcnik K, Carlen P, Damyanovich A, Mrkonjic M, Jones S, Heathcote EJ. Prevalence and significance of neurocognitive dysfunction in hepatitis C in the absence of correlated risk factors. Hepatology. 2005;41(4):801–808. doi: 10.1002/hep.20635. [DOI] [PubMed] [Google Scholar]
- 16.Crews WD, Jefferson AL, Bolduc T, Elliott JB, Ferro NM, Broshek DK, Barth JT, Robbins MK. Neuropsychological dysfunction in patients suffering from end-stage chronic obstructive pulmonary disease. Arch Clin Neuropsychol (the official journal of the National Academy of Neuropsychologists) 2001;16(7):643–652. doi: 10.1093/arclin/16.7.643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kadan-Lottick NS, Zeltzer LK, Liu Q, Yasui Y, Ellenberg L, Gioia G, Robison LL, Krull KR. Neurocognitive functioning in adult survivors of childhood non-central nervous system cancers. J Nat Cancer Inst. 2010;102(12):881–893. doi: 10.1093/jnci/djq156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Conti F, Alessandri C, Perricone C, Scrivo R, Rezai S, Ceccarelli F, Spinelli FR, Ortona E, Marianetti M, Mina C, Valesini G. Neurocognitive dysfunction in systemic lupus erythematosus: association with antiphospholipid antibodies, disease activity and chronic damage. PLoS ONE. 2012;7(3):e33824. doi: 10.1371/journal.pone.0033824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kushida CA, Littner MR, Morgenthaler T, Alessi CA, Bailey D, Coleman J, Jr, Friedman L, Hirshkowitz M, Kapen S, Kramer M, Lee-Chiong T, Loube DL, Owens J, Pancer JP, Wise M. Practice parameters for the indications for polysomnography and related procedures: an update for 2005. Sleep. 2005;28(4):499–521. doi: 10.1093/sleep/28.4.499. [DOI] [PubMed] [Google Scholar]
- 20.Chen NH, Johns MW, Li HY, Chu CC, Liang SC, Shu YH, Chuang ML, Wang PC. Validation of a Chinese version of the Epworth sleepiness scale. Qual Life Res (an international journal of quality of life aspects of treatment, care and rehabilitation) 2002;11(8):817–821. doi: 10.1023/A:1020818417949. [DOI] [PubMed] [Google Scholar]
- 21.De Luca CR, Wood SJ, Anderson V, Buchanan JA, Proffitt TM, Mahony K, Pantelis C. Normative data from the CANTAB. I: development of executive function over the lifespan. J Clin Exp Neuropsychol. 2003;25(2):242–254. doi: 10.1076/jcen.25.2.242.13639. [DOI] [PubMed] [Google Scholar]
- 22.Lange KW, Robbins TW, Marsden CD, James M, Owen AM, Paul GM. L-dopa withdrawal in Parkinson’s disease selectively impairs cognitive performance in tests sensitive to frontal lobe dysfunction. Psychopharmacology. 1992;107(2–3):394–404. doi: 10.1007/BF02245167. [DOI] [PubMed] [Google Scholar]
- 23.Sahakian BJ, Owen AM, Morant NJ, Eagger SA, Boddington S, Crayton L, Crockford HA, Crooks M, Hill K, Levy R. Further analysis of the cognitive effects of tetrahydroaminoacridine (THA) in Alzheimer’s disease: assessment of attentional and mnemonic function using CANTAB. Psychopharmacology. 1993;110(4):395–401. doi: 10.1007/BF02244644. [DOI] [PubMed] [Google Scholar]
- 24.Owen AM, Roberts AC, Polkey CE, Sahakian BJ, Robbins TW. Extra-dimensional versus intra-dimensional set shifting performance following frontal lobe excisions, temporal lobe excisions or amygdalo-hippocampectomy in man. Neuropsychologia. 1991;29(10):993–1006. doi: 10.1016/0028-3932(91)90063-E. [DOI] [PubMed] [Google Scholar]
- 25.Lowe C, Rabbitt P. Test/re-test reliability of the CANTAB and ISPOCD neuropsychological batteries: theoretical and practical issues. Cambridge neuropsychological test automated battery. International study of post-operative cognitive dysfunction. Neuropsychologia. 1998;36(9):915–923. doi: 10.1016/S0028-3932(98)00036-0. [DOI] [PubMed] [Google Scholar]
- 26.Kribbs NB, Pack AI, Kline LR, Smith PL, Schwartz AR, Schubert NM, Redline S, Henry JN, Getsy JE, Dinges DF. Objective measurement of patterns of nasal CPAP use by patients with obstructive sleep apnea. Am Rev Respir Dis. 1993;147(4):887–895. doi: 10.1164/ajrccm/147.4.887. [DOI] [PubMed] [Google Scholar]
- 27.Orth M, Duchna HW, Leidag M, Widdig W, Rasche K, Bauer TT, Walther JW, de Zeeuw J, Malin JP, Schultze-Werninghaus G, Kotterba S. Driving simulator and neuropsychological [corrected] testing in OSAS before and under CPAP therapy. Eur Respir J. 2005;26(5):898–903. doi: 10.1183/09031936.05.00054704. [DOI] [PubMed] [Google Scholar]
- 28.Yang Q, Phillips CL, Melehan KL, Rogers NL, Seale JP, Grunstein RR. Effects of short-term CPAP withdrawal on neurobehavioral performance in patients with obstructive sleep apnea. Sleep. 2006;29(4):545–552. doi: 10.1093/sleep/29.4.545. [DOI] [PubMed] [Google Scholar]
- 29.Antic NA, Catcheside P, Buchan C, Hensley M, Naughton MT, Rowland S, Williamson B, Windler S, McEvoy RD. The effect of CPAP in normalizing daytime sleepiness, quality of life, and neurocognitive function in patients with moderate to severe OSA. Sleep. 2011;34(1):111–119. doi: 10.1093/sleep/34.1.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Monasterio C, Vidal S, Duran J, Ferrer M, Carmona C, Barbe F, Mayos M, Gonzalez-Mangado N, Juncadella M, Navarro A, Barreira R, Capote F, Mayoralas LR, Peces-Barba G, Alonso J, Montserrat JM. Effectiveness of continuous positive airway pressure in mild sleep apnea-hypopnea syndrome. Am J Respir Crit Care Med. 2001;164(6):939–943. doi: 10.1164/ajrccm.164.6.2008010. [DOI] [PubMed] [Google Scholar]
- 31.Engleman HM, Martin SE, Deary IJ, Douglas NJ. Effect of CPAP therapy on daytime function in patients with mild sleep apnoea/hypopnoea syndrome. Thorax. 1997;52(2):114–119. doi: 10.1136/thx.52.2.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Engleman HM, Kingshott RN, Wraith PK, Mackay TW, Deary IJ, Douglas NJ. Randomized placebo-controlled crossover trial of continuous positive airway pressure for mild sleep apnea/hypopnea syndrome. Am J Respir Crit Care Med. 1999;159(2):461–467. doi: 10.1164/ajrccm.159.2.9803121. [DOI] [PubMed] [Google Scholar]
- 33.Engleman HM, Martin SE, Deary IJ, Douglas NJ. Effect of continuous positive airway pressure treatment on daytime function in sleep apnoea/hypopnoea syndrome. Lancet. 1994;343(8897):572–575. doi: 10.1016/S0140-6736(94)91522-9. [DOI] [PubMed] [Google Scholar]
- 34.Engleman HM, Martin SE, Kingshott RN, Mackay TW, Deary IJ, Douglas NJ. Randomised placebo controlled trial of daytime function after continuous positive airway pressure (CPAP) therapy for the sleep apnoea/hypopnoea syndrome. Thorax. 1998;53(5):341–345. doi: 10.1136/thx.53.5.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Weaver TE, Maislin G, Dinges DF, Bloxham T, George CF, Greenberg H, Kader G, Mahowald M, Younger J, Pack AI. Relationship between hours of CPAP use and achieving normal levels of sleepiness and daily functioning. Sleep. 2007;30(6):711–719. doi: 10.1093/sleep/30.6.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Aloia MS, Ilniczky N, Di Dio P, Perlis ML, Greenblatt DW, Giles DE. Neuropsychological changes and treatment compliance in older adults with sleep apnea. J Psychosom Res. 2003;54(1):71–76. doi: 10.1016/S0022-3999(02)00548-2. [DOI] [PubMed] [Google Scholar]
- 37.Aloia MS, Di Dio L, Ilniczky N, Perlis ML, Greenblatt DW, Giles DE. Improving compliance with nasal CPAP and vigilance in older adults with OAHS. Sleep Breath. 2001;5(1):13–21. doi: 10.1055/s-2001-12789. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.