Abstract
Lichen planus is an idiopathic inflammatory condition, which may involve mucosa of the oral cavity, gastrointestinal tract, larynx or the cutaneous surface either in isolation or in combinations. Mucosal lichen planus is more common than the cutaneous variant. Isolated lip involvement is very rare and should be differentiated from other similar leukoplakic lesions. We are reporting a rare case of oral lichen planus in an elderly male that was exclusively localised to the lower lip.
Keywords: Oral lichen planus (OLP), Lip, Plaque, Leukoplakia
Introduction
Lichen planus is a disease of the skin and mucous membrane with an unknown aetiology. It is usually seen in the sixth decade of life with a mean age of 52 years and a female preponderance [1]. It can involve oral mucosa, genital region, conjunctiva, esophageal, laryngeal and anal mucosa with oral mucosa being the commonest site. In oral cavity, commonly involved sites are posterior part of buccal mucosa, tongue, gingiva, retromolar trigone, vestibule, palate, floor of mouth and lip [2]. Literature review suggests that dental restorative agents, stress, drugs like angiotensin converting enzyme (ACE) inhibitors, non-steroidal anti-inflammatory drugs (NSAIDs), infectious agents like herpes simplex virus, Epstein barr virus, cytomegalovirus, hepatitis C virus and irritants like alcohol and smoking as the triggering factors for lichen planus or lichenoid lesions. We are presenting here a rare case of isolated plaque variant of lower lip lichen planus presenting as leukoplakia.
Case Report
A 52 years old male patient presented to our otolaryngology outpatient department with complaint of isolated whitish patch on his lower lip for last one year, which was insidious onset and was not progressing in its dimension. The lesion was painless and was present at the inner aspect of lower lip in the midline. Patient had no history of any local injury, tobacco chewing, smoking or alcohol intake. The patient was referred from another center, with a provisional diagnosis of leukoplakia.
On clinical examination there was a single 1.0 × 0.5 cm, painless whitish patch present over the mucosal surface at the centre of lower lip (Fig. 1). The lesion had slightly irregular margins with minimal elevated borders and the base was indurated. Based on these clinical findings a provisional diagnosis of leukoplakia was made. In view of limited size and extent of the lesion, with patients consent an excision biopsy was planned. Under all aseptic precautions, the lesion was excised completely under local anaesthesia using cold knife, followed by primary closure.
Fig. 1.

Clinical photograph showing whitish patch seen on the lower lip
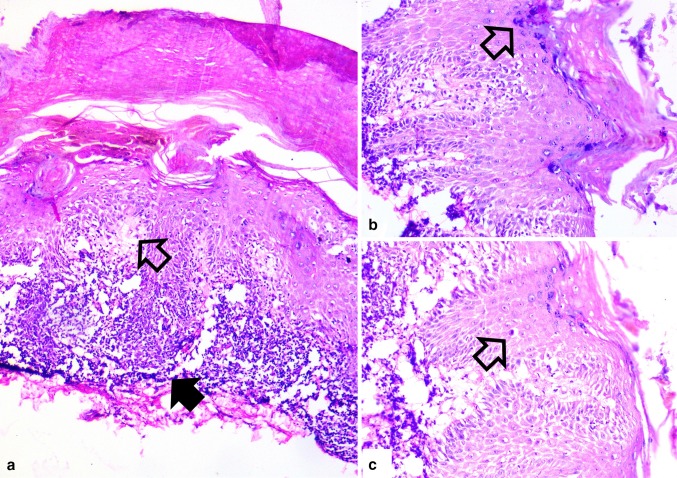
Histopathological examination of the excised tissue revealed hyperkeratosis, mild focal parakeratosis, wedge shaped hypergranulosis and focal irregular acanthosis. Marked basal vacuolar degeneration, edema and prominent band like lymphocytic infiltrate were noted (Fig. 2). Occasional colloid bodies representing necrotic keratinocytes were also seen. There was no evidence of dysplasia or malignancy. Overall histological findings were consistent with the diagnosis of lichen planus involving the lower lip.
Fig. 2.
a Photomicrograph showing hyperkeratosis, basal vacuolar degeneration (open arrow), edema and prominent band like lymphocytic infiltrate (solid arrow) [100X] b higher magnification of wedge shaped hypergranulosis (arrow) with basal vacuolar degeneration [200X] and c occasional colloid bodies representing degenerating necrotic keratinocytes (arrow) [200X]
Discussion
Although multifactorial, lichen planus is thought to have an autoimmune aetiology mediated by CD8 positive T cells [3]. Six clinical patterns of oral lichen planus (OLP) have been described in literature i.e.; reticular, erosive/ulcerative, papular, plaque like, atrophic and bullous with reticular being the most common variant [4]. In our case, it was a plaque like variant, presenting with a leukoplakic patch over the lower lip. Lichen planus may be associated with Hepatitis C Virus infection also [5]. Although asymptomatic, some cases of OLP may present with extensive erosion and pain over the local site. It should be differentiated from other mucosal lesions like pemphigus vulgaris, chronic ulcerative stomatitis, lupus erythematosus, oral leukoplakia and candidiasis. Commonly, it presents as bilateral whitish lesion in buccal mucosa or lingual mucosa. OLP can develop into squamous cell carcinoma in 0.3–3.0 % cases [4]. Mignogna et al. [6] found 3.7 % malignant transformation during his follow-up of five hundred two patients with OLP, which includes 28.5 % cases of in situ oral squamous cell carcinoma (OSCC), 38.0 % cases of microinvassive OSCC and 33.2 % cases of OSCC.
The absence of parakeratosis in lichen planus helps to differentiate the lesion from its close differentials like lichen planus-like keratosis or lichenoid drug eruptions. However, mild focal parakeratosis with minimal to absent hypergranulosis may be seen in OLP. Lichenoid lupus erythematosus or chronic graft versus host disease (GVHD) may also histologically mimic lichen planus, but the dermal infiltrate is predominantly perivascular and periadnexal in the latter two lesions. In addition, absence of atypia or dysplasia helps to rule out leukoplakia or other squamous intraepithelial lesions. Thus, a clinico-histological correlation with due emphasis to the constellation of characteristic histological findings, helps to confirm the diagnosis of lichen planus.
The initial management in symptomatic cases is aimed at alleviating the precipitating cause with maintenance of good oral hygiene. Topical steroids in the form of clobetasol propionate, triamcinolone acetonide, hydrocortisone, fluticasone propionate are the first line treatment. Immunomodulatory agents like cyclosporine, tacrolimus (calcineurin inhibitors) or retinoids can be used topically in patients not responding to topical steroids. Prednisone can be used systemically also in non-responders. Laser phototherapy can be used as an alternative modality of treatment of oral lichen planus; as suggested by Dillenburg CS et al. [7], who compared it with topical clobetasol and found it to be more effective.
In our case, the patient had a small, isolated lesion on the lower lip which had not responded to medical management. Excision biopsy in this particular situation has proved curative as well as diagnostic at the same time. Till last follow up there is no evidence of recurrence.
Conclusion
Isolated lip involvement is a very rare and atypical site of presentation of oral lichen planus. Tissue diagnosis either in form of diagnostic or excision biopsy (in small sub centric lesion) is warranted to differentiate plaque pattern of OLP from leukoplakia. As there is chance of recurrence and malignant transformation, OLP needs close follow-up for a prolonged period of time.
Acknowledgments
Conflict of interest
None, Authors declare that there are no conflicts of interest involved in this manuscript.
References
- 1.Silverman S, Jr, Gorsky M, Lozada-Nur F. A prospective follow-up study of 570 patients with oral lichen planus: persistence, remission, and malignant association. Oral Surg Oral Med Oral Pathol. 1985;60(1):30–34. doi: 10.1016/0030-4220(85)90210-5. [DOI] [PubMed] [Google Scholar]
- 2.Brown RS, Bottomley WK, Puente E, Lavigne GJ. A retrospective evaluation of 193 patients with oral lichen planus. J Oral Pathol Med. 1993;22(2):69–72. doi: 10.1111/j.1600-0714.1993.tb00046.x. [DOI] [PubMed] [Google Scholar]
- 3.Carrozzo M, Uboldi de Capei M, Dametto E, Fasano ME, Arduino P, Broccoletti R, Vezza D, Rendine S, Curtoni ES, Gandolfo S. Tumor necrosis factor-alpha and interferon-gamma polymorphisms contribute to susceptibility to oral lichen planus. J Invest Dermatol. 2004 Jan;122(1):87-94. Erratum in: J Invest Dermatol. 2004 Oct;123(4):805. [DOI] [PubMed]
- 4.Kaplan B, Barnes L. Oral lichen planus and squamous carcinoma. Case report and update of the literature. Arch Otolaryngol. 1985;111(8):543–547. doi: 10.1001/archotol.1985.00800100091015. [DOI] [PubMed] [Google Scholar]
- 5.Lodi G, Pellicano R, Carrozzo M. Hepatitis C virus infection and lichen planus: a systematic review with meta-analysis. Oral Dis. 2010;16:601–612. doi: 10.1111/j.1601-0825.2010.01670.x. [DOI] [PubMed] [Google Scholar]
- 6.Mignogna MD, Lo Muzio L, Lo Russo L, Fedele S, Ruoppo E, Bucci E. Clinical guidelines in early detection of oral squamous cell carcinoma arising in oral lichen planus: a 5-year experience. Oral Oncol. 2001;37(3):262–267. doi: 10.1016/S1368-8375(00)00096-8. [DOI] [PubMed] [Google Scholar]
- 7.Dillenburg CS, Martins MA, Munerato MC, Marques MM, Carrard VC, Filho MS, Castilho RM, Martins MD. Efficacy of laser phototherapy in comparison to topical clobetasol for the treatment of oral lichen planus: a randomized controlled trial. J Biomed Opt. 2014;19(6):68002. doi: 10.1117/1.JBO.19.6.068002. [DOI] [PubMed] [Google Scholar]