Abstract
To compare the functional results between posterior cordotomy, cordoplasty and external procedure in managing bilateral vocal cord paralysis in one of the largest published study group. Retrospective and comparative study. 54 patients with bilateral vocal cord paralysis who underwent posterior cordotomy (Group-I), cordoplasty (Group-II) and external procedure (Group-III) from 2001 to 2013 were compared for functional outcomes. Successful decannulation was achieved more in Group-I and II than in Group-III. Voice outcome was better in Group-II patients compared to other groups. Outcomes of cordoplasty was better than posterior cordotomy and external procedures, with acceptable airway and good quality of voice. Posterior cordotomy is preferred in patients without tracheostomy and in pediatric patients. In patients with tracheostomy or who accept temporary tracheostomy, a cordoplasty is preferred for favorable voice. External procedure is preferred for patients not fit for general anesthesia.
Electronic supplementary material
The online version of this article (doi:10.1007/s12070-014-0740-4) contains supplementary material, which is available to authorized users.
Keywords: Bilateral vocal cord paralysis, Laser surgery, Cordotomy, Voice quality
Introduction
Most cases of the bilateral vocal cord paralysis (BVCP) are a consequence of thyroid operation [1]. Other causes are neurologic, viral infection, idiopathic and intubation trauma [1], oesophageal, thyroid and gastric malignancy [2], Wegener’s granulomatosis, congenital and rheumatologic diseases [1, 3, 4].
Patients with BVCP present with snoring and dyspnea. Onset and severity of dyspnea depends upon extent of damage to laryngeal nerves. In most cases voice is serviceable [5] as both the vocal cords are either in median or paramedian position.
Various options available for surgical treatment of BVCP are tracheostomy, extra laryngeal, endoscopic and laryngofissure arytenoidectomy, lateral fixation of vocal cord, arytenoidectomy with ventriculo-cordotomy, arytenoidopexy and laser transverse cordotomy [1, 2, 5, 6]. Laryngeal re-innervation by nerve muscle pedicle and laryngeal pacing via crico-arytenoid muscle are still under research [7]. None of these are currently effective in completely restoring three main functions of larynx viz respiration, voice production and protection of airway.
Various approaches to arytenoidectomy and resection of ventricles can preserve the vocal cord but protection to airway is lost, causing aspiration [8]. Moreover, laser arytenoidectomy can cause granulation tissue formation necessitating revision surgery [9]. Similarly, if vocal cords are removed as in cordectomy or cordotomy, voice outcome is compromised [10]. So, there is a need for a new technique.
Currently, laser posterior cordotomy is preferred option as it permits voice production with the anterior part of the vocal cord and an adequate airway through the posterior glottis [3, 4, 11–14]. On the other hand, our technique of cordoplasty preserves vocal cord mucosa completely. Superior and lateral shifting of the posterior third of the vocal cord produces a two dimensionally enlarged glottis with good quality voice in cordoplasty.
The purpose of this study is to compare the functional outcomes of posterior cordotomy, cordoplasty and external procedure in managing BVCP. This is one of the largest comparative study involving the two common treatment modalities and our new technique of cordoplasty for BVCP.
Materials and Methods
Design of Study
This is a retrospective and comparative study of 54 patients aged 4–67 years, who underwent surgery from 2001 to 2013 for BVCP at MCV Memorial ENT Trust Hospital, an Otolaryngology and head and neck surgery referral and teaching hospital. The most common etiology for BVCP in our series was thyroidectomy (Table 1).
Table 1.
Etiology of BVCP in our series (54 cases)
| Etiology | No. of cases | Percentage (%) |
|---|---|---|
| Thyroidectomy | 32 | 59.3 |
| Idiopathic | 13 | 24.1 |
| Congenital | 3 | 5.6 |
| Parkinsonism | 2 | 3.7 |
| External traumatic | 2 | 3.7 |
| Post-intubation trauma | 1 | 1.8 |
| Wegener’s granulomatosis | 1 | 1.8 |
Management
Patients were endoscoped in office for assessing the airway, and to decide the side of surgery. The cord which is placed more medially and with minimal movement is preferred for surgery. When both the vocal cords are the same, left side is preferred (for right handed surgeon). In patients with acute onset BVCP, laryngeal electromyography (EMG) was done, which helps in assessing the likelihood of recovery [15], exclude vocal cord fixation [9] and facilitate treatment plan. As there is a chance of recovery of BVCP within 6 months of onset, acute airway obstruction was managed with tracheostomy and irreversible procedure to widen the glottis was deferred for 6 months as the chances of recovery is unlikely after this period [15].
Chest X-ray, ECG, laboratory investigations and neurologic evaluation were done to exclude systemic disorders. MRI of head and neck to delineate the course of vagus and recurrent laryngeal nerves and CT chest to rule out pulmonary pathology and multilevel airway obstruction was done in post traumatic and long term tracheostomized patient.
Adult patients without tracheostomy were taken in Group-I (posterior cordotomy). As cordoplasty requires enough space within the larynx to operate, patients with tracheostomy or willing for temporary tracheostomy were included in Group-II. Patients contraindicated for general anesthesia underwent external procedure under local anesthesia (Group-III). Procedures done in individual groups are given in Tables 2 and 3. All patients were explained about the choice and outcomes of the procedures and consent was taken for the same. All these groups were compared for post-operative functional outcomes and complications.
Table 2.
Procedures done in Group-I and II
| Groups | Group-I (posterior cordotomy) | Group-II (cordoplasty) |
|---|---|---|
| Primary cases | 27 | 10 |
| Revision cases | 4 | – |
Table 3.
Procedures done in Group-III
| Group-III: procedures | No. of cases |
|---|---|
| External arytenoidectomy and vocal cord lateralization (primary) | 10 |
| External arytenoidectomy and vocal cord lateralization (revision) | 2 |
| External arytenoidectomy and vocal cord lateralization with additional type-I thyroplasty after 3 months | 1 |
Anesthesia
Details of anesthesia techniques used are detailed in Table 4.
Table 4.
Anesthesia techniques used in individual groups
| Anesthesia techniques | Group-I (total no. = 31) | Group-II (total no. = 10) | Group-III (total no. = 13) |
|---|---|---|---|
| Existing tracheostomy | 8 (25.8 %) | 10 (100 %) | – |
| Jet ventilation | 22 (71 %) | – | – |
| Endotracheal intubation | 1 (3.2 %) | – | 1 (7.7 %) |
| Local anesthesia with pre-operative tracheostomy | – | – | 12 (92.3 %) |
Surgery
Posterior Cordotomy
Bupivacaine (0.5 %) with dexamethasone (4 mg/ml) and adrenaline (1:80,000) is injected at the surgical site to minimize bleeding, post-operative edema and pain. CO2 laser with continuous mode at 10–15 watts was used to create a ‘C’ shaped wedge in posterior third of membranous vocal cord, anterior to vocal process of arytenoids (Fig. 1). Laterally, laserising the perichondrium or cartilage is avoided by palpation to identify the cricoid cartilage.
Fig. 1.
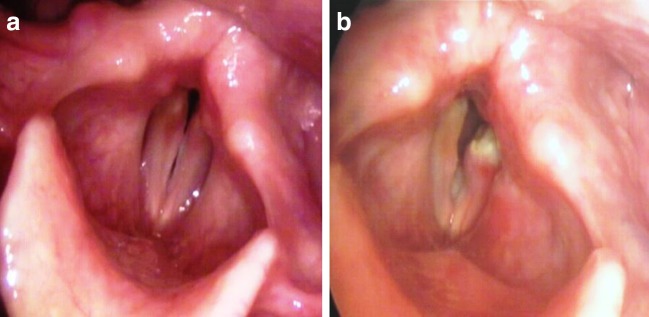
Pre (a) and Post (b) operative 90° endoscopic view of glottis in left posterior cordotomy patient
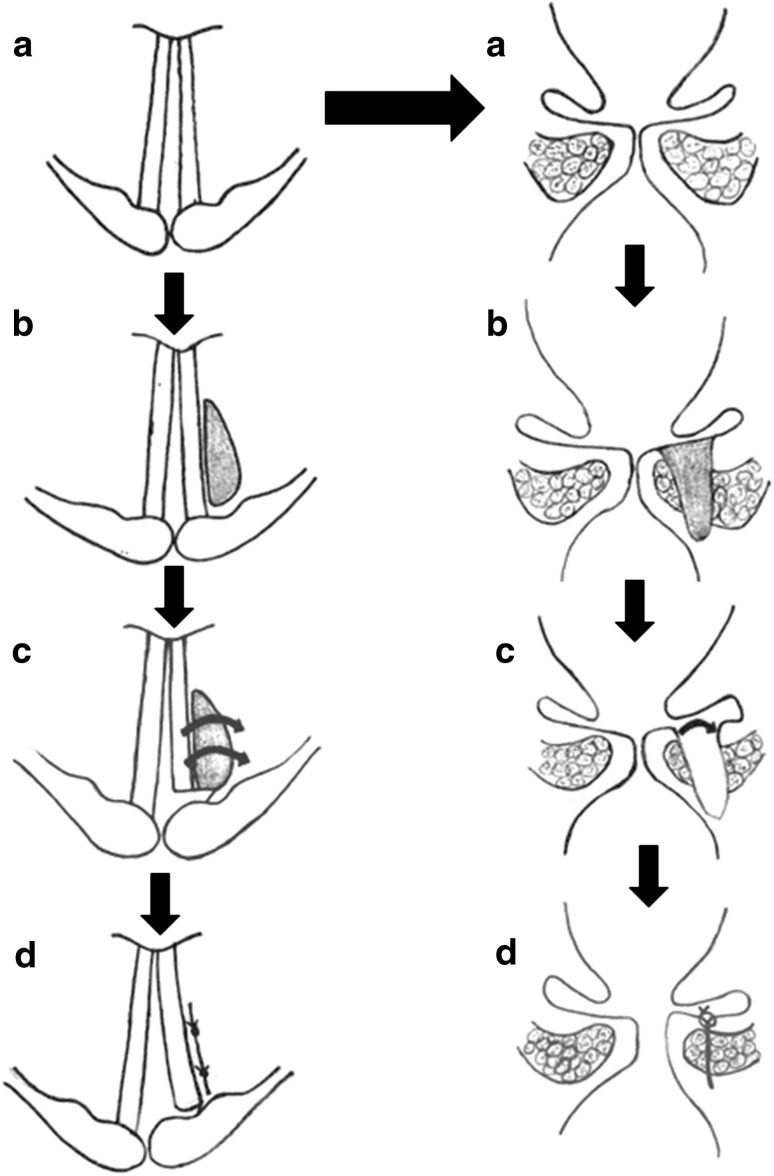
Cordoplasty
In cordoplasty, linear vaporization of ventricular floor adjacent to posterior one-third of membranous vocal cord is done with CO2 laser after application of false vocal cord retractor without damaging true vocal cord. Laser defect (Fig. 2) is made approximately 1.5 × 1 × 1 cm size, anteroposterior length being 1.5 cm. The vaporization proceeds until the subglottic mucosa is reached and the mucosa and vocal process is carefully preserved. Then using a scissors, the posterior end of membranous cord is divided completely from vocal process. This creates a flap of viable vocal cord tissue pedicled anteriorly and inferiorly which is pulled laterally and superiorly to obliterate the dead space of the laser defect. 5-0 vicryl rapide (polyglactin 910) sutures keep the flap in place (Fig. 3).
Fig. 2.
Steps of laser cordoplasty in endoscopic (left) and coronal view (right). a Both vocal cords (VC) in para-median position. b Laser vaporization of right ventricular floor with preservation of VC mucosa. c Posterior end of membranous VC divided completely and VC flap created. d Flap pulled laterally and superiorly with 5-0 vicryl rapide suture
Fig. 3.
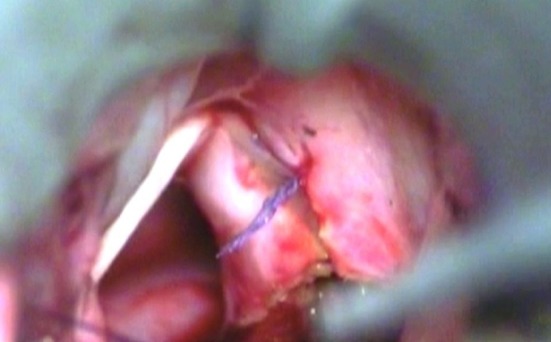
Picture showing laterally sutured right cordoplasty flap with vocal cord retractor in place
External Procedure
Under local anesthesia a horizontal skin crease incision is made just above lower border of thyroid ala on the side of surgery. The dissection carried out posteriorly between sternocleidomastoid and strap muscles to identify posterior border of thyroid cartilage. The cricothyroid joint is dislocated and larynx is rotated with hooks placed on posterior border of thyroid cartilage. The constrictor muscles are incised and Marago’s window is cut. Then pyriform sinus mucosa is carefully elevated from undersurface of the cartilage. The posterior crico-arytenoid (PCA) muscle is identified and tendon is followed to the muscular process of arytenoid and 3-0 prolene suture is placed through vocal process of arytenoid and rest of the arytenoid removed. The suture is tied to the inferior horn of thyroid cartilage, thus pulling the vocal process laterally and inferiorly. The adequacy of airway checked through an indwelling system of fiber optic scope.
Post-operative Management
All patients received broad spectrum antibiotics for 7 days, nebulized steroids, oral prednisolone in tapering dose and anti reflux medications.
Follow up
All 54 patients were followed until present. Duration of follow up ranged from 10 months to 12 years. The mean duration of follow up was 5 years and 5 months.
Results
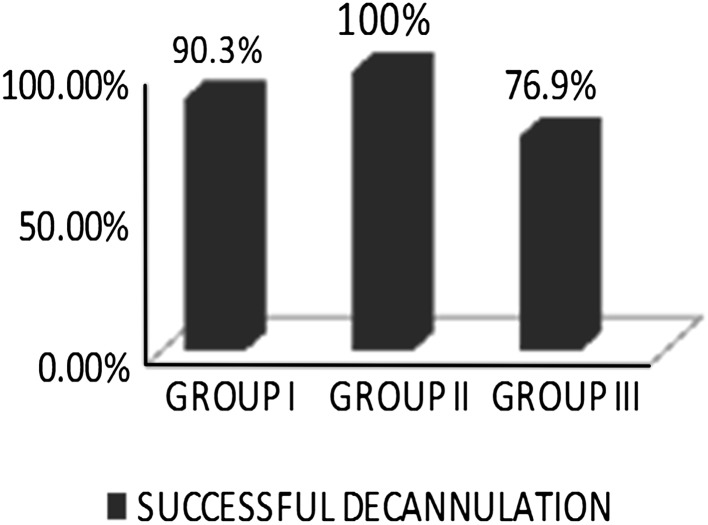
Tracheostomy Decannulation
In Group-I (n = 31), 28 patients (90.3 %) were successfully decannulated. 2 (6.5 %) patients were tracheostomy dependent due to psychological reasons and in one patient (3.2 %) decannulation was not possible due to Wegener’s granulomatosis involving the subglottic region.
In Group-II (n = 10) all patients were successfully decannulated (100 %). In Group-III (n = 13), 10 patients (76.9 %) were successfully decannulated (Fig. 4). Decannulation was not possible in three patients (23.1 %), one due to brain damage following head injury and two other due to coexistent advanced Parkinsonism causing airway collapse.
Fig. 4.
Comparison of successful tracheostomy decannulation in individual group
Adequacy of Airway
Adequacy of airway was assessed with 90° rigid laryngoscopy and Medical Research Council (MRC) Breathlessness scale [16, 17] and the results are shown in Table 5. Patients with good airway did not have snoring and vice versa.
Table 5.
| MRC dyspnea grading | Group-I (total no. = 31) | Group-II (total no. = 10) | Group-III (total no. = 13) | |||
|---|---|---|---|---|---|---|
| I | 2 | 87.1 % | – | 100 % | 1 | 69.2 % |
| II | 16 | 6 | 3 | |||
| III | 9 | 4 | 5 | |||
| IV | 1 | 3.2 % | – | – | 1 | 7.7 % |
| V | 3 | 9.7 % | – | – | 3 | 23.1 % |
Aspiration
No significant aspiration symptoms observed in all the groups. Three patients in Group-I had mild symptoms of aspiration (cough on supine position) immediately after the surgery which settled in a month. There were no symptoms of aspiration in Group-II and III patients.
Voice
Voice outcomes were assessed by experienced speech pathologist as per Maurizi et al. [18]. It was assessed only in decannulated patients. The results are shown in Table 6.
Table 6.
Comparison of voice outcome in individual groups
| Voice outcome | Group-I (total no. = 28) | Group-II (total no. = 10) | Group-III (total no. = 10) |
|---|---|---|---|
| Normal | 1 (3.6 %) | – | – |
| Near normal | 14 (50 %) | 8 (80 %) | 2 (20 %) |
| Fair | 13 (46.4 %) | 2 (20 %) | 8 (80 %) |
Discussion
Tracheostomy was once the only option available to treat BVCP. Chevalier Jackson in 1922 was the first person to perform ventriculocordectomy with an aim of preserving the voice. Even though this gave an excellent airway, voice quality was poor [19]. Other procedures like extra laryngeal, endoscopic and laryngofissure arytenoidectomy and lateralization of vocal cord with stainless steel suture were also developed. All of them had inconsistent voice outcomes [19].
Kelly in 1941 modified King’s technique by excising the arytenoid through a window in the thyroid cartilage and by placing a suture to lateralize the vocal cord. In 1946, Woodman described a method of partial arytenoidectomy with lateralization of vocal cord by suturing vocal process to inferior cornu of thyroid cartilage without creating a thyroid window. This procedure remained popular for almost 50 years [1].
Strong et al. in 1976, was the first to use the CO2 laser for endoscopic arytenoidectomy. Dennis and Kashima introduced a modification in this technique by using CO2 laser for posterior cordotomy. This posterior cordotomy has the advantage of shorter operating time, good phonatory anterior vocal cord, and a wide posterior airway [19].
The hallmark of CO2 laser is precision and haemostasis. This results in coagulum covered surgical field minimizing infection and post-operative morbidity [19]. However it is not advisable to apply laser to arytenoid cartilage and inner perichondrium of cricoid.
Suture lateralization by lateral fixation of vocal cord to the neck skin with non absorbable suture is described as a method to preserve vocal cord mucosa [20, 21]. This technique can be used only as a temporary means as suture can cause granulation tissue over the vocal cord, around the suture site. Long term results are not stable with this method.
In our technique of cordoplasty, a two dimensionally enlarged glottis is produced with minimal change in position of anterior vibrating vocal cord as the arc of rotation of vocal cord flap is centered posterior to the anterior commisure. Loss of tissue from posterior glottis compromises voice quality and swallowing function [10], so in cordoplasty, scissors are used to cut vocal cords attachment to vocal process and no vocal cord mucosa is sacrificed as in posterior cordotomy [5], which resulted in better voice outcome (80 %). Moreover, “5-0 vicryl rapide” suture material used gets absorbed rapidly preventing granulation [22].
In our series, cordoplasty had 100 % successful decannulation compared to 90.3 % in posterior cordotomy and 76.9 % in external group. Microlaryngeal approach provides adequate anatomical exposure of the field and facilitates precisely controlled widening of glottis.
On assessing the adequacy of airway with MRC dyspnea grading, Group-I and II patients fared better, especially cordoplasty group. The inadequate airway achieved in external group may be due to our learning curve, as these patients were done earlier in our series.
Even though 6 (19.4 %) patients in Group-I had pre-existing tracheostomy, posterior cordotomy was performed because cordoplasty technique was not developed at that time. Remaining patients underwent surgery without tracheostomy. All patients in the external procedure group needed tracheostomy before the definitive procedure, except in one patient. It is possible to do a posterior cordotomy without tracheostomy due to the short operating time. Laser application also contributes to this as it seals of the microcirculation at the margins resulting in minimal oedema [5]. In patients who were referred to us with tracheostomy and who insist on an optimal voice, we preferred cordoplasty. This requires longer operating time and more space within larynx to operate necessitating temporary tracheostomy.
In our series, we have done 4 revision posterior cordotomies, owing to undercorrection of airway at first attempt and unfavourable fibrosis. In our experience, we found, it’s better to undercorrect the airway initially and perform a revision later if airway was found to be inadequate, as overcorrecting the airway initially will leave the patient with poor voice and reversal of overcorrection is difficult even under best circumstances [15]. The revision rate in our series of posterior cordotomy is less (12.9 %) compared to other series [4, 8, 23]. This is due to our technique of posterior cordotomy which extends laterally up to inner lamina of cricoid cartilage so we could achieve a wide airway while preserving integrity of opposite vocal cord. Compared to bilateral posterior cordotomy in our series (two cases), unilateral posterior cordotomy patients had good quality voice. We prefer doing bilateral cordotomy only as a revision, as it can cause aspiration [24].
Most revisions are due to fibrosis. This can be minimized by preserving interarytenoid mucosa [19] and by cordoplasty method. We use a laser deflection mirror (5 mm Storz 8596) for achieving a deep cut at posterior end of vocal cord up to cricoid lamina without damaging the false vocal cord or arytenoids. Only problem we encountered using this instrument was heating the opposite vocal cord which was in contact with the back of the mirror.
A wide glottic airway can be achieved by external procedure. Experience gathered from arytenoid adduction has improved the result of external procedure for BVCP. In our series, a female BVCP patient underwent three normal deliveries after an external procedure done 10 years ago without the need for tracheostomy. Type-I thyroplasty was done as an additional procedure for one patient in this group to overcome breathy voice due to wide glottis. Other main disadvantages of this procedure are its poor voice outcome and the need for neck incision.
In the literature, posterior cordotomy is found to be a more effective tool to widen the glottis for patients with BVCP, but its main complication cited is aspiration [5, 25]. However, no persistent swallowing difficulty or severe symptoms of aspiration occurred in our patients. This is likely due to sparing of false cord and arytenoids [8].
Advantages of posterior cordotomy are achieving a wide posterior airway with reasonably good quality of voice, short operative time and relative ease of the procedure, minimal bleeding and edema. The main limitations is that it is inappropriate for patients with a short neck in whom it is difficult to identify the vocal cords and in patients with fixation of the cervical spine in whom it is impossible to extend the neck [1].
All the failed decannulations in our series were either due to psychological dependence on tracheostomy tube or due to co-existent systemic disease. In posterior cordotomy group, we had one case of Wegener’s granulomatosis involving subglottic region. This patient underwent posterior cordotomy with biopsy of subglottic granulation and histopathological examination showed non-specific granulation tissue. Subsequently, cANCA was found to be positive and patient was started on steroids, but she failed to respond favorably. Another patient in the same group had been on tracheostomy tube for more than 10 years and in spite of having sufficiently wide glottic chink following posterior cordotomy decannulation was not possible, reason for failure was her psychological dependence on tracheostomy. Yet another patient in posterior cordotomy group had suprastomal granulation due to long term metallic tracheostomy tube and that was addressed during the revision surgery and subsequent decannulation was achieved. Patients on long term tracheostomy tube have a tendency to develop psychological dependence on tube and suprastomal granulation. This should be kept in mind when operating on long term tracheostomized patients.
Conclusion
We recommend posterior cordotomy or cordoplasty for patients with BVCP to achieve adequate airway and good quality of voice. Posterior cordotomy procedure can be performed safely with gratifying results without the need for tracheostomy. As this procedure is quick, it is preferred for elderly patients for whom anesthesia has to be short [18] and also in patients who do not have or want a tracheostomy. Cordoplasty has an added advantage that vocal cord mucosa is preserved and is preferred for patients who already have a tracheostomy or accept temporary tracheostomy for a better vocal outcome. External procedure under local anesthesia will be preferred in cases with restricted neck movements and in patients contraindicated for general anesthesia.
Summary
Various currently available surgical treatment for BVCP are not effective in completely restoring the three main functions of larynx viz respiration, voice production and protection of airway.
This study elaborates new technique of endolaryngeal suturing of vocal cord flap laterally (cordoplasty) to achieve adequate airway, without aspiration and with minimal compromise in voice quality.
Patients who underwent cordoplasty had adequate airway with good voice quality compared to posterior cordotomy and external procedure.
Posterior cordotomy is done for patients who prefer not to have temporary tracheostomy and in elderly patients for whom anesthesia has to be short.
External procedure is preferred in patients with restricted neck movements and in patients contraindicated for general anesthesia.
Electronic supplementary material
Acknowledgments
All financial and material support by MCV Memorial ENT Trust Hospital.
Conflict of interest
None.
References
- 1.Joshua B, Feinmesser R, Zohar L, Shvero J. Endoscopic laser assisted posterior ventriculocordectomy without tracheostomy for bilateral vocal cord immobility. Isr Med Assoc J. 2004;6(6):336–338. [PubMed] [Google Scholar]
- 2.Benninger MS, Gillen JB, Altman JS. Changing aetiology of vocal fold immobility. Laryngoscope. 1998;108(9):1346–1350. doi: 10.1097/00005537-199809000-00016. [DOI] [PubMed] [Google Scholar]
- 3.Shvero J, Koren R, Stern Y, Segal K, Feinmesser R, Hadar T. Laser posterior ventriculocordectomy with partial arytenoidectomy for the treatment of bilateral vocal fold immobility. J Laryngol Otol. 2003;117(7):540–543. doi: 10.1258/002221503322112969. [DOI] [PubMed] [Google Scholar]
- 4.Laccourreye O, Paz Escovar MI, Gerhardt J, Hans S, Bicabe B, Brasnu D. CO2 laser endoscopic posterior partial transverse cordotomy for bilateral paralysis of the vocal fold. Laryngoscope. 1999;109(3):415–418. doi: 10.1097/00005537-199903000-00014. [DOI] [PubMed] [Google Scholar]
- 5.Ahmed B, Hydri AS, Malik KZ. Laser arytenoidectomy and vocal cord lateralization for bilateral abductor vocal cord paralysis. Pak J Otolaryngol. 2003;19:19–21. [Google Scholar]
- 6.Gupta AK, Mann SB, Nagarkar N. Surgical management of bilateral immobile vocal folds and long term followup. J Laryngol Otol. 1997;111(5):474–477. doi: 10.1017/s0022215100137685. [DOI] [PubMed] [Google Scholar]
- 7.Tucker HM. Human laryngeal reinnervation. Laryngoscope. 1976;86:769–779. doi: 10.1288/00005537-197606000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Riffat F, Palme CE, Veivers D. Endoscopic treatment of glottis stenosis: a report on the safety and efficacy of CO2 laser. J Laryngol Otol. 2012;126(5):503–505. doi: 10.1017/S002221511100301X. [DOI] [PubMed] [Google Scholar]
- 9.Pinto JA, Godoy LB, Marquis VW, Sonego TB, Leal Cde F. Bilateral vocal fold immobility: diagnosis and treatment. Braz J Otorhinolaryngol. 2011;77(5):594–599. doi: 10.1590/S1808-86942011000500010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bajaj Y, Sethi N, Shayah A, Harris AT, Henshaw P, Coatesworth AP, Nicolaides AR. Vocal fold paralysis: role of bilateral transverse cordotomy. J Laryngol Otol. 2009;123(12):1348–1351. doi: 10.1017/S0022215109990983. [DOI] [PubMed] [Google Scholar]
- 11.Dennis DP, Kashima H. Carbon dioxide laser posterior cordectomy for treatment of bilateral vocal cord paralysis. Ann Otol Rhinol Laryngol. 1989;98(12 Pt 1):930–934. doi: 10.1177/000348948909801203. [DOI] [PubMed] [Google Scholar]
- 12.Eckel HE, Thumfart M, Wassermann K, Vossing M, Thumfart WF. Cordectomy versus arytenoidectomy in the management of bilateral vocal cord paralysis. Ann Otol Rhinol Laryngol. 1994;103(11):852–857. doi: 10.1177/000348949410301105. [DOI] [PubMed] [Google Scholar]
- 13.Remacle M, Lawson G, Mayne A, Jamart J. Subtotal carbon dioxide laser arytenoidectomy by endoscopic approach for treatment of bilateral cord immobility in adduction. Ann Otol Rhinol Laryngol. 1996;105(6):438–445. doi: 10.1177/000348949610500604. [DOI] [PubMed] [Google Scholar]
- 14.Ossoff RH, Sisson GA, Duncavage JA, Moselle HI, Andrews PE, McMillan WG. Endoscopic laser arytenoidectomy for the treatment of bilateral vocal cord paralysis. Laryngoscope. 1984;94(10):1293–1297. doi: 10.1288/00005537-198410000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Benninger MS, Bhattacharyya N, Fried MP. Surgical management of bilateral vocal fold paralysis. Oper Tech Otolaryngol. 1998;9(4):224–229. doi: 10.1016/S1043-1810(98)80008-0. [DOI] [Google Scholar]
- 16.Bestall JC, Paul EA, Garrod R, et al. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999;54(7):581–586. doi: 10.1136/thx.54.7.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stenton C. The MRC breathlessness scale. Occup Med. 2008;58(3):226–227. doi: 10.1093/occmed/kqm162. [DOI] [PubMed] [Google Scholar]
- 18.Maurizi M, Paludetti G, Galli J, Cosenza A, Di Girolamo S, Ottaviani F. CO2 laser subtotal arytenoidectomy and posterior true and false cordotomy in the treatment of post-thyroidectomy bilateral laryngeal fixation in adduction. Eur Arch Otorhinolaryngol. 1999;256(6):291–295. doi: 10.1007/s004050050248. [DOI] [PubMed] [Google Scholar]
- 19.Oswal VH, Gandhi SS. Endoscopic laser management of bilateral abductor palsy. Indian J Otolaryngol Head Neck Surg. 2009;61(Suppl 1):47–51. doi: 10.1007/s12070-009-0017-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Werner JA, Lippert BM. Lateral fixation of the vocal cord instead of tracheotomy in acute bilateral vocal cord paralysis. Dtsch Med Wochenschr. 2002;127(17):917–922. doi: 10.1055/s-2002-25381. [DOI] [PubMed] [Google Scholar]
- 21.Pérouse R, Coulombeau B, Arias C, Casanova C. Lateral fixation of the vocal fold (Lichtenberger’s technique): interest in the bilateral laryngeal immobilities. Rev Laryngol Otol Rhinol. 2006;127(5):353–355. [PubMed] [Google Scholar]
- 22.Aderriotis D, Sàndor GK. Outcomes of irradiated polyglactin 910 Vicryl Rapide fast-absorbing suture in oral and scalp wounds. J Can Dent Assoc. 1999;65(6):345–347. [PubMed] [Google Scholar]
- 23.Kashima HK. Bilateral vocal fold motion impairment: patho-physiology and management by transverse cordotomy. Ann Otol Rhinol Laryngol. 1991;100(9 Pt 1):717–721. doi: 10.1177/000348949110000905. [DOI] [PubMed] [Google Scholar]
- 24.Mohamad I, Jihan WS, Mohamad H, Abdullah B. Laser posterior cordotomy for bilateral abductor vocal cord palsy: a case report. Malays J Med Sci. 2008;15(1):42–43. [PMC free article] [PubMed] [Google Scholar]
- 25.Harnisch W, Brosch S, Schmidt M, Hagen R. Breathing and voice quality after surgical treatment for bilateral vocal cord paralysis. Arch Otolaryngol Head Neck Surg. 2008;134(3):278–284. doi: 10.1001/archoto.2007.44. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.