Abstract
Although lipomas are common soft tissue tumors, few cases of lipoma or its variants have been reported in the oral cavity. We here described the clinical, histological, and immunohistochemical features of 24 cases of oral lipoma obtained from medical records at Nagasaki University Hospital between 1977 and 2010, and also retrospectively reviewed 603 cases of oral lipoma reported in the English literatures. The patients examined comprised 11 men and 13 women with a mean age of 59 years, ranging from 31 to 90 years. The main sites involved were the buccal mucosa (n = 9), followed by the tongue (n = 4), lip and retromolar area (n = 3), floor of the mouth (n = 2), and gingiva (n = 1). The mean tumor size was 2.0 cm, ranging from 0.2 to 5 cm. Histological analysis revealed 20 cases of lipoma, 2 cases of fibrolipoma, and one case each of intramuscular lipoma and spindle cell lipoma. Twenty-three cases were treated surgically while one case underwent biopsy and follow-up. Recurrence was not observed in any case. We reviewed the English literatures, and similar results were obtained. In immunohistochemical analysis, PCNA and ki-67 expression indices were higher in intramuscular lipoma cases than in its variants. Especially, it showed that a long time follow-up may be necessary in ki-67 positive cases.
Keywords: Lipoma, Oral cavity, ki-67, PCNA
Introduction
Lipoma is a benign tumor of fat. It represents by far the most common mesenchymal neoplasm, and most cases occur on the trunk and proximal portions of the extremities; however, lipomas of the oral and maxillofacial region are rare [1]. Their overall incidence in the oral cavity is thought to be less than 4.4 % of all benign oral mesenchymal neoplasms [2–4, 7, 13], and was higher in previous study [5]. Oral lipomas may occur in various anatomical sites including the major salivary glands, buccal mucosa, lip, tongue, palate, and floor of the mouth. Of these, the buccal mucosa and buccal vestibule are the most common intraoral sites and account for approximately 50 % of all cases [4]. Histologically, lipomas can be classified as classic lipomas or its variants, such as fibrolipomas, spindle lipomas, intramuscular lipomas, angiolipomas, salivary gland lipomas, pleomorphic lipomas, myxoid lipomas, and atypical lipomas [4, 16].
We here analyzed the clinicopathological features and proliferative activities of 24 cases of oral lipomas in our department, and compared the results with 603 cases reported in the literature in English [4–15].
Materials and Methods
Medical records were reviewed at the Department of Oral and Maxillofacial Surgery, Nagasaki University Graduate School of Biomedical Sciences Nagasaki, Japan between 1977 and 2010. All cases diagnosed with benign oral mesenchymal tumors including lipomas of the oral cavity were retrieved according to the classification adopted by the World Health Organization (WHO). Information regarding the gender and age of the patients, the site, size, and duration before the lesions were treated, as well as the treatments performed and the length of the follow-up were carefully examined from the patient records. In addition, we reviewed the literature in English where possible using PubMed to search for studies. No tumor involving the skin, subcutaneous tissues, the bone, or parotid gland was included in the analysis.
The proliferative activities of all lipomas were assessed immunohistochemically using antibodies against the proliferating cell nuclear antigen and ki-67 antigen (Dako, A/S, Denmark), auto-crave antigen retrieval, and the Envision system (EnVision+, DAKO). PCNA and ki-67 slides were analyzed histochemically by calculating the average percentage of positive cells in ten high-power fields for each marker in all cases.
Results
Clinical Data
The clinicopathologic features of this study are summarized in Table 1. Males accounted for 45.8 % and females 54.2 % of 24 patients during the 33-year period between 1977 and 2010. The mean age of the patients was 59 years, ranging from 31 to 90 years. The mean duration between the first awareness of symptoms and treatment was 1 year, ranging from 4 days to 37 years. This was unclear in 2 cases. Most patients were asymptomatic, noting only increased swelling. However, one patient with lipoma in the lip had prior trauma, one patient with lipoma in the tongue had swelling with pain, and one patient with lipoma in the tongue had dysmotility and dysarthria. The lipoma size ranged from 0.2 to 5 cm, with a mean of 2.0 cm. Most cases had overlying mucosa that was normal in color, while it was yellow in 5 cases and unknown in 1 case.
Table 1.
Clinical and pathological findings in oral lipomas
| Case | Age/sex | Size (cm) | Duration (months) | Symptom | Color | Site | Histological type | Treatment | Follow-up (months) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 72/M | 2.4 | 60 | Asymptom | Yellow | Palate | Lipoma | Excision | Unclear |
| 2 | 31/F | 1.5 | 36 | Asymptom | Normal ~ yellow | Lip | Lipoma | Excision | Unclear |
| 3 | 45/F | 1.5 | 18 | Asymptom | Unclear | Buccal | Lipoma | Excision | Unclear |
| 4 | 46/M | Unclear | 60 | Asymptom | Normal | Retromolar area | Lipoma | Excision | Unclear |
| 5 | 55/F | 3.0 | 3 | Asymptom | Yellow | Buccal | Lipoma | Excision | Unclear |
| 6 | 64/M | 2.5 | 1 | Pain | Unclear | Tongue | Lipoma | Excision | Unclear |
| 7 | 64/M | 4.5 | 60 | Asymptom | Unclear | Buccal | Lipoma | Excision | Unclear |
| 8 | 50/F | 0.5 | 4 days | Asymptom | Normal | Floor of the mouth | Lipoma | Excision | 1 |
| 9 | 44/F | 2.0 | 444 | Asymptom | Normal | Palate | Lipoma | Excision | Unclear |
| 10 | 55/F | 0.7 | Several years | Asymptom | Normal | Retromolar area | Lipoma | Excision | Unclear |
| 11 | 66/F | 1.1 | 6 | Asymptom | Normal | Lip | Lipoma | Excision | Unclear |
| 12 | 70/M | 1.5 | 120 | Trauma | Normal | Lip | Lipoma | Excision | Unclear |
| 13 | 47/F | 2.5 | Unclear | Unclear | Unclear | Buccal | Lipoma | Excision | Unclear |
| 14 | 83/M | 1.2 | Unclear | Asymptom | Unclear | Gingiva | Lipoma | Excision | Unclear |
| 15 | 55/M | .10 | 12 | Asymptom | Unclear | Buccal | Lipoma | Excision | Unclear |
| 16 | 62/F | 2.5 | 3 | Asymptom | Normal | Tongue | Lipoma | Excision | 3 |
| 17 | 69/F | 2.0 | 120 | Asymptom | Normal | Buccal | Lipoma | Excision | 41 |
| 18 | 90/M | 3.0 | 6 | Asymptom | Yellow | Buccal | Lipoma | Excision | 0 |
| 19 | 59/M | 0.8 | 3 | Asymptom | Normal | Buccal | Lipoma | Excision | 1 day |
| 20 | 71/M | 2.5 | 1 | Asymptom | Normal ~ yellow | Tongue | Lipoma | Excision | 2 weeks |
| 21 | 76/F | 3.0 | 72 | Asymptom | Normal | Floor of the mouth | Fibrolipoma | Excision | Unclear |
| 22 | 70/M | 1.5 | 12 | Asymptom | Normal | Palate | Fibrolipoma | Biopsy | NA |
| 23 | 42/F | 5.0 | 12 | Asymptom | Normal | Buccal | Spindle cell lipoma | Excision | 12 |
| 24 | 58/F | 3.5 | 6 | Dysmotility and dysarthria | Normal | Tongue | Intramuscular lipoma | Excision | 6 |
The most common site was the buccal mucosa (37.5 %), followed by the tongue (16.6 %), palate and lip (12.5 %), floor of the mouth (8.3 %), retromolar area (8.3 %), and gingiva (4.15 %). Histologically, there were 20 cases of classic lipoma (83.3 %), followed by 2 cases of fibrolipoma (8.3 %), one case of intramuscular lipoma (4.15 %), and one case of spindle cell lipoma (4.15 %). Classic lipomas had well demarcated adipose nodules and a small amount of fibrous connective tissue intermingled in the tumor. Cytologic atypia was absent and no central cartilaginous or osseous metaplasia was observed. Fibrolipomas were characterized by significant fibrous components intermixed with lobules of fat cells. Intramuscular lipomas were covered with an unclear capsule partially containing skeletal muscle fibers. The stroma was composed of mature adipose cells surrounding and separating irregular bundles of skeletal muscle fibers. Spindle cell lipomas were composed of spindle cells and fat cells distributed in a myxoid matrix (Table 2).
Table 2.
Summary of the 603 cases of oral lipoma reported in the literatures
| [4] | [5] | [6] | [7] | [8] | [9] | [10] | [11] | [12] | [13] | [14] | [15] | Total | Our study | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. cases | 46 | 13 | 26 | 10 | 41 | 26 | 57 | 145 | 16 | 19 | 146 | 58 | 603 | 24 |
| Study period (year) | 31 | 14 | 4 | 10 | 38 | 25 | NA | 21 | 5 | 19 | NA | 20 | NA | 33 |
| Sex | ||||||||||||||
| Male/female | 20:26 | 5:08 | 6:20 | 4:06 | 12:29 | 10:14 | 31/26 | 68/57 | 2:14 | 10:09 | 77/69 | 29/29 | 274/329 | 11/13 |
| Ratio | 1:1,1 | 1:1,6 | 1:3,3 | 1:1,5 | 1:2,4 | 1;1,4 | 1,2:1 | 1,2:1 | 1;7 | 10;9 | 1,1:1 | 1:01 | 1:1.2 | 1:1.18 |
| Age | ||||||||||||||
| Range | 8–80 | 40–73 | 29–91 | 8–92 | 18–75 | 28–63 | 20–70 | 2–87 | 27–70 | 11–75 | NA | NA | NA | 31–90 |
| Peak incidence | 6th | 7th | 6th | 6th | 7th | NA | 6th | 5th | NA | 4th | NA | NA | NA | 6th |
| Mean size (cm) | 2 | 0.8 | 1.19 | 1.66 | 2.1 | NA | NA | 2.6 | NA | 1.6 | NA | 1.68 | NA | 2.0 |
| Range size (cm) | 0.3–5 | 0.2–1.5 | 0.5–2.8 | 0.2–1.0 | 0.5–10 | NA | NA | 0.5–10 | 0.3–2.5 | 0.5–3.0 | 0.3–2.2 | 0.2–10 | NA | 0.2–5 |
| Localization | ||||||||||||||
| Buccal mucosa | 21 | 4 | 9 | 5 | 22 | 11 | 24 | 46 | 8 | 3 | 49 | 31 | 233 | 9 |
| Vestibule | 4 | 0 | 1 | 3 | 6 | 4 | 1 | 18 | 0 | 6 | 14 | 5 | 62 | 0 |
| Gingiva | 0 | 0 | 0 | 1 | 0 | 0 | 3 | 8 | 0 | 0 | 0 | 0 | 12 | 2 |
| Retromolar area | 2 | 0 | 2 | 1 | 3 | 4 | 0 | 0 | 5 | 1 | 9 | 0 | 27 | 2 |
| Tongue | 6 | 2 | 7 | 0 | 4 | 0 | 11 | 28 | 0 | 3 | 21 | 10 | 92 | 4 |
| Lip | 6 | 1 | 4 | 0 | 1 | 2 | 6 | 9 | 0 | 5 | 31 | 6 | 71 | 1 |
| Oral floor | 5 | 3 | 3 | 0 | 3 | 2 | 8 | 21 | 2 | 1 | 8 | 6 | 62 | 3 |
| Palate | 0 | 1 | 0 | 0 | 1 | 3 | 1 | 13 | 0 | 0 | 8 | 0 | 27 | 3 |
| Other | 2 | 2 | 0 | 0 | 1 | 0 | 3 | 2 | 1 | 0 | 6 | 0 | 17 | 0 |
| Histologic subtype | ||||||||||||||
| Lipoma | 21 | 9 | 15 | 4 | 18 | 24 | 7 | 71 | 8 | 11 | 83 | 28 | 299 | 20 |
| Fibrolipoma | 18 | 2 | 7 | 4 | 14 | 2 | 5 | 48 | 8 | 8 | 50 | 19 | 185 | 2 |
| Myxoid lipoma | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 8 | 0 | 9 | 0 |
| Angiolipoma | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 2 | 6 | 0 |
| Intramuscular lipoma | 4 | 2 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 12 | 1 |
| Spindle cell lipoma | 1 | 0 | 0 | 0 | 4 | 0 | 0 | 0 | 0 | 0 | 2 | 3 | 10 | 1 |
| Minor salivary gland lipoma | 2 | 0 | 1 | 0 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 9 | 0 |
| Unknown | 0 | 0 | 0 | 0 | 0 | 0 | 45 | 26 | 0 | 0 | 0 | 0 | 73 | 0 |
| Duration of awareness (months) | 75.8 | NA | NA | 30.4 | 48 | NA | NA | NA | NA | 53 | NA | 31.2 | NA | 12 |
| Follow up period (months) | 26.5 | NA | 6–12 | 34.5 | 45 | NA | NA | NA | NA | NA | 12–96 | 31.5 | NA | 3 |
Twenty-three cases were treated surgically and 1 case underwent biopsy and follow-up. Follow-up information after surgery was only available for 8 cases (33.3 %). The mean follow-up period was 3 months, ranging from 1 day to 41 months, and no records of recurrence were found in any case.
Immunohistochemical Data
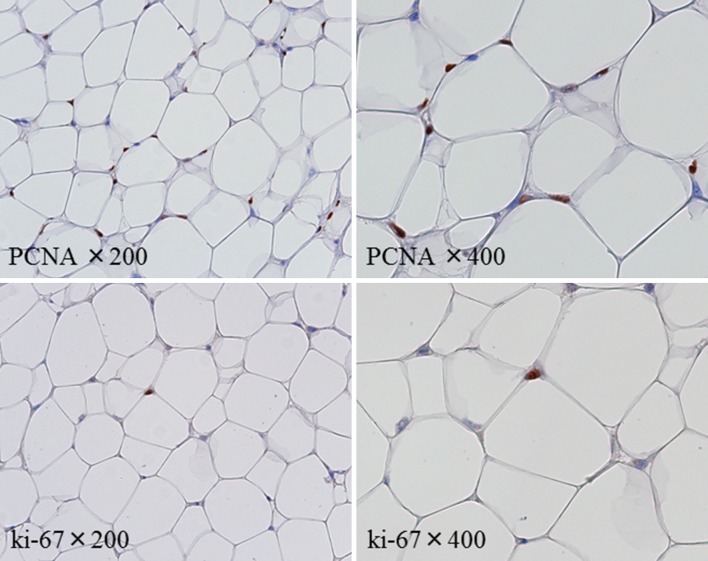
The mean percentage of immunohistochemical PCNA expression in all the cases studied was 14.4 % (ranging from <1 to 42.8 %) and for ki-67 was less than 1 % (ranging from <1 to 18.3 %). Immunohistochemical staining for both PCNA and ki-67 was detected in the nuclei of mature fat cells (Fig. 1). The distribution of PCNA and ki-67 expression by different histological groups was shown in Table 3. Although statistical analysis could not be performed due to the small number of cases, both PCNA and ki-67 labeling indices tended to be higher in intramuscular lipoma cases than in those of other lipomas.
Fig. 1.
Representative immunohistochemical staining for PCNA and Ki-67 in the nuclei of mature fat cells
Table 3.
Distribution of oral lipomas according to the site of occurrence and histological variants
| Site | Lipoma | Fibrolipoma | Intramuscular lipoma | Spindle cell lipoma | Total |
|---|---|---|---|---|---|
| Tongue | 3 | ― | 1 | ― | 4 (16.6 %) |
| Buccal mucosa | 8 | ― | ― | 1 | 9 (37.5%) |
| Lip | 3 | ― | ― | ― | 3 (12.5 %) |
| Floor of mouth | 1 | 1 | ― | ― | 2 (8.3 %) |
| Palate | 2 | ― | ― | ― | 2 (8.3 %) |
| Retromolar area | 2 | 1 | ― | ― | 3 (12.5 %) |
| Gingiva | 1 | ― | ― | ― | 1 (4.15 %) |
| Total | 20 (83.3 %) | 2 (8.3 %) | 1 (4.15 %) | 1 (4.15 %) | 24 (100 %) |
Literature Review
Twelve literature searches between 1966 and 2011 identified 603 cases of oral lipomas. The study period ranged from 4 to 38 years and 45.4 % of all cases were reported in males, with a male to female ratio of 1:1.2. Some literatures were reported that the peak incidence of tumors was observed in the sixth decade of life. Tumor size ranged from 0.2 to 10 cm, and mean size ranged 0.8–2.6 cm. The most frequent site was the buccal mucosa (38.6 %), followed by the tongue (15.2 %), lip (11.8 %), floor of the mouth and buccal vestibule (10.3 %), palate and retromolar area (4.5 %), gingiva (2.0 %), and others (2.8 %). Histological patterns according to the subtypes classified in the present study [1] revealed that lipomas were the most common (49.6 %), followed by fibrolipomas (30.7 %), intramuscular lipomas (2.0 %), spindle cell lipomas (1.66 %), minor salivary gland lipomas and myxoid lipomas (1.5 %), angiolipomas (1.0 %), and unknown (12.1 %). These results were shown in Table 2.
Discussion
Lipomas of the oral cavity are relatively rare adipose mesenchymal neoplasms. Their overall incidence accounted for less than 4.4 % of all tumors diagnosed as benign oral mesenchymal neoplasms, and was reportedly 7.5 % in one previous study [2–4, 7, 13]. As recently reported, the causes of lipoma include heredity, fatty degeneration, hormonal abnormalities, injuries, infection, infarction, muscle cell metaplasia, residual embryonic fat cells, and chronic irritation [6, 7, 10]. In our study, one patient had a history of a traumatic episode. None of the patients had systemic diseases, a family history of lipomas, or a specific predisposing event.
Our study revealed that Oral lipomas are slightly more common in female, and the male to female ratios is equal in classic lipomas and fibrolipomas. It has been reported that there is a male preponderance for classic lipomas (1.5:1), whereas there is a female preponderance for fibrolipomas (1:1.3) [13]. In 299 classic lipomas and 185 fibrolipomas (Table 2), 114 classic lipomas and 64 fibrolipomas was possible to examine the male to female ratios in details [5–7, 11, 13]. There is a male preponderance for classic lipomas (1.19:1), whereas there is a female preponderance for fibrolipomas (1:1.6), and similar results were obtained.
Most cases of lipoma occur at 60 years of age or older, and are rare in children [4–15]. In our study, the mean age of the patients was 59 years, with only one case being less than 40 years old. To the best of our knowledge, only 4 cases of oral lipoma in children were reported in English literatures [17–20].
The most common site of oral lipomas has been reported as the buccal mucosa, comprising 38.6 % of all cases, followed by the tongue, lip, floor of the mouth and buccal vestibule, palate and retromolar area, gingiva, and others [4–15]. Our study also revealed that the most common site was the buccal mucosa, followed by the tongue, lip, and oral floor, and obtained similar results. This site predilection may be related to the availability of adipose tissue, which is high in the buccal mucosa because of the proximity of the buccal fat pad and very low in the palate.
The mean duration between the first awareness of symptoms and treatment was reported to be ranged 31.2–75.8 months [4, 7, 8, 13, 15], and our study showed 12 months. The mean tumor size was previously reported to be ranged from 0.8 to 2.6 cm, and our study showed 2.0 cm. The clinical course of oral lipomas is generally asymptomatic until they reach a large size, and large oral lipomas sometimes cause severe oral dysfunction. A previous study reported that a case of giant lipoma arising in the tongue that measured 10.0 × 9.0 × 6.0 cm, weighed 200 g, and caused severe functional impairment [21]. Among our cases, an intramuscular lipoma in the tongue measured 3.5 × 3.0 × 2.0 cm, and caused dysmotility and dysarthria.
Regarding histopathological findings, lipomas and fibrolipomas are the most frequently reported histological variants in the oral cavity [1]. Previous studies demonstrated that the incidence of lipomas and fibrolipomas accounted for approximately 80 % of all cases, followed by intramuscular lipomas and spindle cell lipomas. In the present study, they accounted for more than 90 % of all cases, which was consistent with the findings of previous studies.
Lipoma of the oral cavity is treated by conservative local excision and local recurrence is extremely rare [4, 7, 8]. No significant differences have been reported in prognoses between the major histopathological variants of lipomas [8]. One important exception is intramuscular lipomas. We previously demonstrated that the reason for recurrence was related to difficulties in achieving radical surgical excision because intramuscular lipomas are often more deeply situated, not encapsulated, and have an infiltrative growth pattern [22]. The findings of this case revealed that some parts of the lesion were firmly attached to the muscles. Only two cases of lipoma in the oral cavity have been reported to date [23, 24]. Therefore, it is necessary to excise tumor and the surrounding tissue attaching it to the muscles.
Regarding the proliferative activities of lipomas, we performed an immunohistochemical analysis of the expression of PCNA and ki-67 in different histological groups. In a related report, the expression in fibrolipomas and intramuscular lipomas were found to be higher than classic lipomas, whereas no significant difference was observed in clinical behavior following surgery. The mean labeling indices of PCNA and ki-67 showed 13.2 and 2.8 %, respectively [3]. Our study obtained similar results. On the other hand, other authors have reported that the average labeling index of ki-67 in lipoma and liposarcoma showed 0 and 2.43 %, respectively [25]. It has been reported that ki-67 immunoreactivity appeared to be more selective for the S + G2M phases of the cell cycle than PCNA, and was associated with the mitotic rate, histological grade of malignancy, and biological behavior [26]. In the ki-67 immunoreactivity, our study showed that it was positive in a few cases of classic lipomas and intramuscular lipoma. Although no records of recurrence were found our study, these results showed that ki-67 expression may indicate recurrence or malignant transformation, and a long-term follow-up is necessary (Table 4).
Table 4.
Expression of PCNA and Ki-67 according to the histological classification of oral lipomas
| Histological classification | Total | ||||
|---|---|---|---|---|---|
| Lipoma | Fibrolipoma | Intramuscular lipoma | Spindle cell lipoma | ||
| PCNA (%) (median and range) | 13.4 % (<1 ~ 42.8 %) | 11.25 % (<1 ~ 22.5 %) | 32.2 % | 17.2 % | 14.1 % (<1 ~ 42.8 %) |
| Ki-67 (%) (median and range) | 2.6 % (<1 ~ 18.3 %) | <1 % | 14.4 % | <1 % | 2.77 % (<1 ~ 18.3 %) |
Acknowledgments
Conflict of interest
None declared.
Abbreviations
- F
Female
- M
Male
- cm
Centimeters
- NA
Not available
References
- 1.Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and maxillofacial pathology. 3. Elsevier: Saunders; 2009. pp. 523–524. [Google Scholar]
- 2.Bertelli AP. Uncommon tumors of the tongue (lipoma and leiomyofibroma); report of two cases. Oral Surg Oral Med Oral Pathol. 1965;19:771–775. doi: 10.1016/0030-4220(65)90349-X. [DOI] [PubMed] [Google Scholar]
- 3.Lombardi T, Odell EW. Spindle cell lipoma of the oral cavity: report of a case. J Oral Pathol Med. 1994;23:237–239. doi: 10.1111/j.1600-0714.1994.tb01120.x. [DOI] [PubMed] [Google Scholar]
- 4.Fregnami ER, Pires FR, Falzoni R, Lopes MA, Vargas PA. Lipomas of the oral cavity: clinical findings, histological classification and proliferative activity of 46 cases. Int J Oral Maxillofac Surg. 2002;32:49–53. doi: 10.1054/ijom.2002.0317. [DOI] [PubMed] [Google Scholar]
- 5.Epivatianos A, Markopoulos AK, Papanayotou P. Benign tumors of adipose tissue of the oral cavity: a clinicopathologic study of 13 cases. J Oral Macillofac Surg. 2000;58:1113–1117. doi: 10.1053/joms.2000.9568. [DOI] [PubMed] [Google Scholar]
- 6.De Freitas MA, Freitas VS, de lima AA, Pereira FB Jr, dos Santos JN (2009) Intraoral lipomas; a study of 26 cases in a Brazilian population. Quintessence Int 40:79–85 [PubMed]
- 7.Studart-Soares EC, Costa FW, Sousa FB, Alves AP, Osterne RL. Oral lipomas in a Brazilian population: a 10-year study and analysis of 450 cases reported in the literature. Med Oral Patol Oral Cir Bucal. 2010;15(5):e691–e696. doi: 10.4317/medoral.15.e691. [DOI] [PubMed] [Google Scholar]
- 8.Juliasse LE, Nonaka CF, Pinto LP, Freitas Rde A, Miguel MC. Lipomas of the oral cavity: clinical and histopathologic study of 41 cases in a Brazilian population. Eur Arch Otorhinolaryngol. 2010;267(3):459–465. doi: 10.1007/s00405-009-1010-z. [DOI] [PubMed] [Google Scholar]
- 9.Seldin HM, Seldin SD, Rakower W, Jarrett WJ. Lipomas of oral cavity: report of 26 cases. J Oral Surg. 1967;25(3):270–274. [PubMed] [Google Scholar]
- 10.MacGregor AJ, Dyson DP. Oral lipoma. A review of the literature and report of twelve new cases. Oral Surg Oral Med Oral Pathol. 1966;21(6):770–777. doi: 10.1016/0030-4220(66)90100-9. [DOI] [PubMed] [Google Scholar]
- 11.Hatziotis JC. Lipoma of the oral cavity. Oral Surg Oral Med Oral Pathol. 1971;31(4):511–524. doi: 10.1016/0030-4220(71)90348-3. [DOI] [PubMed] [Google Scholar]
- 12.Greer RO, Richardson JF. The nature of lipomas and their significance in the oral cavity. Oral Surg Oral Med Oral Pathol. 1973;36(4):551–557. doi: 10.1016/0030-4220(73)90313-7. [DOI] [PubMed] [Google Scholar]
- 13.de Visscher JG. Lipomas and fibrolipomas of the oral cavity. J Maxillofac Surg. 1982;10(3):177–181. doi: 10.1016/S0301-0503(82)80036-2. [DOI] [PubMed] [Google Scholar]
- 14.Said-Al-Naief N, Zahurullah FR, Sciubba JJ. Oral spindle cell lipoma. Ann Diagn Pathol. 2001;5(4):207–215. doi: 10.1053/adpa.2001.26973. [DOI] [PubMed] [Google Scholar]
- 15.Manor E, Sion-Vardy N, Joshua BZ, Bodner L. Oral lipoma: analysis of 58 new cases and review of the literature. Ann Diagn Pathol. 2011;15(4):257–261. doi: 10.1016/j.anndiagpath.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 16.Furlong MA, Fanburg-Smith JC, Childers EL. Lipomas of the oral and maxillofacial region: site and subclassification of 125 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:441–450. doi: 10.1016/j.tripleo.2004.02.071. [DOI] [PubMed] [Google Scholar]
- 17.Kim JW, Kang SJ. Pediatric lipoma of the buccal fat pad. J Craniofac Surg. 2012;23(6):1934–1935. doi: 10.1097/SCS.0b013e3182653f60. [DOI] [PubMed] [Google Scholar]
- 18.Sato H, Gotoh C, Uchida H, Kawashima H, Yoshida M, Kitano Y, Kishimoto H. Sialolipoma of the submandibular gland in a child. J Pediatr Surg. 2011;46(2):408–410. doi: 10.1016/j.jpedsurg.2010.09.097. [DOI] [PubMed] [Google Scholar]
- 19.Gokul S, Ranjini KV, Kirankumar K, Hallikeri K. Congenital osteolipoma associated with cleft palate: a case report. Int J Oral Maxillofac Surg. 2009;38(1):91–93. doi: 10.1016/j.ijom.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 20.Lerosey Y, Choussy O, Gruyer X, Francois A, Marie JP, Dehesdin D, et al. Infiltrating lipoma of the head and neck: a report of one pediatric case. Int J Pediatr Otorhinolaryngol. 1999;47(1):91–95. doi: 10.1016/S0165-5876(98)00173-6. [DOI] [PubMed] [Google Scholar]
- 21.Dattilo DJ, Iqe JT, Nwana EJ. Intraoral lipoma of the tongue and submandibular space: report of a case. J Oral Maxillofac Surg. 1996;54(7):915–917. doi: 10.1016/S0278-2391(96)90549-2. [DOI] [PubMed] [Google Scholar]
- 22.Naruse T, Yanamoto S, Kawano T, Yoshitomi I, Yamada S, Kawasaki G, et al. Intramuscular lipoma of the tongue: report of a case complicated with diffuse lipomatosis. J Oral Maxillofac Surg Med Pathol. 2012;24:237–240. doi: 10.1016/j.ajoms.2012.03.010. [DOI] [Google Scholar]
- 23.Scherl MP, Som PM, Biller HF, Shah K. Recurrent infiltrating lipoma of the head and neck: case report and literature review. Arch Otolaryngol Head Neck Surg. 1986;112:1210–1212. doi: 10.1001/archotol.1986.03780110086014. [DOI] [PubMed] [Google Scholar]
- 24.Lacey MS, Craig I. Infiltrating lipoma of the face. Ann Plast Surg. 1995;35:307–309. doi: 10.1097/00000637-199509000-00015. [DOI] [PubMed] [Google Scholar]
- 25.Hatano H, Morita T, Ogose A, Hotta T, Kobayashi H, Honma K. Well-differentiated liposarcoma associated with benign lipoma. Anticancer Res. 2004;24(2C):1039–1044. [PubMed] [Google Scholar]
- 26.Kindblom LG, Meis-Kindblom JM. Chondroid lipoma: an ultrastructural and immunohistochemical analysis with further observations regarding its differentiation. Hum Pathol. 1995;26(7):706–715. doi: 10.1016/0046-8177(95)90217-1. [DOI] [PubMed] [Google Scholar]