Abstract
The aim of the study was to examine and analyze the epidemiology and outcome of treatment for paediatric acquired subglottic stenosis treated with endoscopic bougie dilatation and topical mitomycin C. There were 15 patients identified from 2008 until 2013. All of them had acquired subglottic stenosis due to history of intubation. Majority of the patients had grade III stenosis, with the total of seven. Three patients had grade IV; three were grade II and two were grade I. All of the patients with severe stenosis (grade III and IV) needed tracheostomy while only one in mild stenosis group (grade I and II) required it for prolonged ventilation rather than obstruction due to subglottic stenosis. All of them underwent direct laryngoscopy under general anesthesia followed by endoscopic dilatation with bougie and topical mitomycin C 0.4 mg/ml for 5 min. Aim of success in our study was decannulation of tracheostomy or absence of symptoms at exertion. We achieved 6 (60 %) successful decannulation out of 10 patients with tracheostomy (excluded the patient with tracheostomy in grade I stenosis due to prolonged ventilation). As for those without tracheostomy, 3 (75 %) out of 4 patients were asymptomatic even at exertion. Average number of dilatation was 3.1 times, with mean duration of 28 min. No complications were reported in our series. One patient with grade I stenosis passed away due to severe pneumonia unrelated to the stenosis or dilatation, and she did not have any dilatation before she passed away. Multiple related risk factors were identified such as intubation, prematurity, movement of endotracheal tube, respiratory infection, traumatic intubation and gastroesophageal reflux disease. Experience of open surgical method was very limited in our centre in Sabah in East Malaysia. Endoscopic technique plays an important role in treatment of subglottic stenosis with adjunct like mitomycin C possibly booster the successful rate.
Keywords: Subglottic stenosis, Endoscopic, Bougie, Dilatation, Mitomycin C
Introduction
Subglottic stenosis (SGS) is the narrowing of the subglottic lumen. It can be divided into congenital and acquired type. Congenital type is the third most common congenital abnormality and consists of abnormal shape and size. Most common acquired cause is endotracheal intubation [1]. Other important risk factors are low birth weight (<1500 gm), reintubation [2], respiratory tract infection [3], movement of endotracheal tube (ETT) [4], inappropriate size of ETT, and gastroesophageal reflux disease [5].
Since the advent of prolonged ventilation in mid 1960 s by MacDonald and Stock, the incidence of SGS was about 8 % in intubated infants [6]. With better care and appropriate use of endotracheal tube, the incidence decreased to less than 2 % in 2001 as reviewed by Warner et al. [7].
Queen Elizabeth Hospital Sabah is a major tertiary referral centre for paediatric otolaryngological problems and largest hospital in Sabah, Malaysia. Even though it is biggest hospital in Sabah, it is considered a district hospital with limited expertise and experience. Therefore, our facilities and expertise for open surgical procedures for SGS are still limited. Endoscopic dilation with topical application of mitomycin C is the main treatment option in our centre. Patients who failed endoscopic treatment will be referred to major mainland hospitals in Malaysia which are thousands miles away separated by South China Sea. Aim of our study is to examine the outcome of endoscopic dilatation and application of topical mitomycin C in Hospital Queen Elizabeth Sabah from January 2008 till June 2013.
Methods
All infants and children who were diagnosed with SGS from January 2008 till june 2013 were identified. All the cases were retrospectively reviewed and followed up, in particular for age, sex, race, classification and grade of stenosis, risk factors (history of intubation, reintubation, movement of ETT, respiratory tract infection, gastroesophageal reflux disease, size of ETT), number of endoscopic dilation and mitomycin C usage, and eventual outcome. All these patients underwent endoscopic dilation under general anaesthesia via existing tracheostomy or jet ventilation. Direct laryngoscopy was performed by Parson direct laryngoscope. Then, the scope was stabilised with suspension apparatus. Under direct vision with HOPKIN telescopy, severity of stenosis was graded according to Myer-cotton grading system 8. Shapshay radial incision was made and stenotic area was dilated with bougie with topical application of mitomycin C 0.4 mg/ml for 5 min. Dilatation was done till maximum size that fitted the stenotic lumen with scar already cut. Granulation tissues were also removed with cold method if present. Patients were then discharged the following day after strict observation in ward. We defined our success as decannulation of tracheostomy or absent of dyspnoea at exertion.
Results
A total of 15 patients were identified during the study period. There were 9 males and 6 females. The mean age at diagnosis of SGS was 21.6 months. There were 5 Bajau, 3 Kadazan, 2 Dusun. The rest were non-citizen from Philippine. Four patients were born premature with mean gestational age of 29.3 weeks (from 27–31 weeks).
Majority of patients (7/15, 47 %) had grade III SGS followed by three (20 %) with grade II, two (13 %) with grade I and three (20 %) with grade IV stenosis (Fig. 1). All patients presented with stridor and dyspnoea from 5 to 21 days after extubation.
Fig. 1.
Severity of subglottic stenosis among patients
The aetiology of SGS was all acquired in our study, which was related to endotracheal intubation. Most of patients (6/15) were ventilated due to respiratory disease included bronchopneumonia and lung empyema. Three patients (13 %) required ventilatory support for severe meningitis and respiratory distress syndrome due to prematurity respectively. Other reasons for ventilation are shown in Fig. 2. Some patients had more than one pathologies simultaneously and therefore, the total number of cases in Fig. 2 exceeds 15 patients. The average duration of intubation was 21 days (range from 6 to 81 days). 11 out of 15 patients needed tracheostomy for the relief of airway obstruction.
Fig. 2.
Various causes of ventilation. RDS = respiratory distress syndrome; others include acute tubular necrosis, idiopathic pulmonary hypertension, and meliodosis
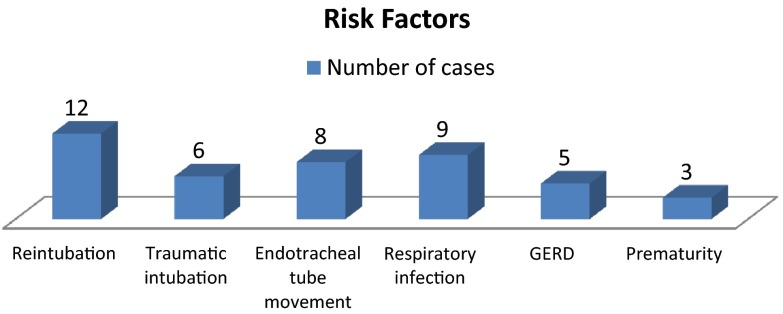
Regarding the risk factors, 12 patients (80 %) had history of reintubation; 8 (53.3 %) had (ETT) movement; 9 (60 %) had evidence of airway infection with positive tracheal aspirate culture; 6 (40 %) had traumatic intubation, and 5 (33.3 %) had gastroesophageal reflux disease diagnosed by either pH prove study or ultrasound (Fig. 3). ETT movement included tube dislodgement, self-extubation, and readjustment of tube due to inappropriate size. Mean reintubation rate in our series was 2.8 times.
Fig. 3.
Risk factors for subglottic stenosis. GERD = gastroesophageal reflux disease
Respiratory tract infection is believed to potentiate injury to subglottic area that leads to formation of scar. This recorded second highest number of patients as compared to other risk factors. These group of patients had proven signs of respiratory infection such as increased oxygen requirement, fever, raised total white cell count, chest X ray changes and positive tracheal aspirate culture. Pseudomonas aeruginosa and Klebsiella species were frequently cultured organisms (Fig. 4).
Fig. 4.
Spectrum of cultured microorganisms MRSA = Methicillin resistant staphylococcus aurues
All patients underwent endoscopic bougie dilation with topical mitomycin C application (concentration of 0.4 mg/ml for 5 min). Our aim was to achieve decannulation of tracheostomy or absence of dyspnoea at rest. Table 1 shows patients’ data on the characteristics of stenotic airway, number of dilatations and the outcome. All of the patients with severe stenosis (grade III and IV) needed tracheostomy to bypass the airway obstruction. One patient in grade I group was tracheostomised for prolonged ventilation rather than airway obstruction. None in grade II needed tracheostomy.
Table 1.
Patients data on the severity of subglottic stenosis, need for tracheostomy, characteristics of stenotic airway, number of dilatations and outcome
| Patient | Grading of stenosis | Tracheostomy | Features of stenosis | Number of dilatations | Outcome |
|---|---|---|---|---|---|
| 1 | I | No | 30 % posterior subglottic, 5 mm thickness | No, conservative | asymptomatic |
| 2 | I | Yes | 20 % posterior subglottic, 5 mm thickness | No | Passed away due to severe pneumonia |
| 3 | III | Yes | Soft circumferential, 12 mm thickness | 4 | Decannulated |
| 4 | II | No | Soft circumferential | 1 | asymptomatic |
| 5 | III | Yes | Anterior soft scar, with suprastomal granulation tissue, 5 mm thickness | 5 | Ongoing follow up |
| 6 | III | Yes | Soft circumferential, 8 mm thickness | 3 | Decannulated |
| 7 | III | Yes | Elliptical scar | 5 | Decannulated |
| 8 | IV | Yes | Soft scar, 5 mm thickness, 8 mm from vocal cords, mobile cords | 6 | Decannulated |
| 9 | II | No | Soft posterior subglottic | 2 | Dyspnoea at exertion |
| 10 | III | Yes | Matured scar, circumferential, 5 mm thickness | 4 | Awaiting for open surgery |
| 11 | IV | Yes | Matured scar | 4 | Underwent cricotracheal resection and primary anastomosis, decannulated |
| 12 | IV | Yes | Matured scar, 7 mm from vocal cords | 4 | Underwent cricotracheal resection and primary anastomosis, decannulated |
| 13 | III | Yes | Elliptical soft, 5 mm thickness | 4 | Decannulated |
| 14 | II | No | Soft posterior subglottic | 3 | asymptomatic |
| 15 | III | Yes | Soft circumferential scar, vocal process granuloma | 3 | Decannulated |
There was average of 3.1 dilations done for each patient (range from 1 to 6). Out of 10 patients with tracheostomy for the sole purpose to bypass obstruction due to subglottic stenosis, 6 patients (60 %) were successfully decannulated from endoscopic method per se. Four patients has thus far failed endoscopic dilatation with two already underwent cricotracheal resection and primary anastomosis. Both of them were successfully decannulated after the surgery done in mainland hospitals in Malaysia. One patient is still waiting for open surgery while the remaining one is still keen to try further on endoscopic dilatation rather than the invasive open surgery. In our series, it was pleased to achieve decannulation in a grade IV stenosis. It was in fact, a very soft scar which during probing at endoscopic examination scar was perforated. He needed up to 6 endoscopic dilatations to achieve an adequate airway.
As for mild stenosis (grade I and II), 1 out of 5 patients was still symptomatic with dyspnoea in exertion. The patient had grade II stenosis with only 2 endoscopic dilatations performed. We believed further dilatation with mitomycin C will help in relieving the symptoms. One passed away due to causes unrelated to subglottic stenosis. The rest were well and led normal daily activities. Excluding the patient whom passed away, our successful rate to achieve an asymptomatic airway among mild stenosis was 75 %.
For each procedure of endoscopic dilation and topical mitomycin application, the average of time consumed was 28 min. The more severe the stenosis, the higher number of dilatations needed (Fig. 5).
Fig. 5.
Number of endoscopic dilatation decannulation rate among different severity of stenosis
There were no complication or mortality recorded from use of mitomycin C in our studies.
There were numerous literatures showing wide range of success rate for endoscopic dilatation because of difference in definition of their success (decannulation, asymptomatic after surgery, duration of follow up). We achieved 6 (60 %) successful decannulation in 6 out of 10 patients with tracheostomy (excluded the patient with tracheostomy in grade I stenosis due to prolonged ventilation). As for those without tracheostomy, 3 (75 %) out of 4 patients were asymptomatic even at exertion.
Discussion
Management of SGS continues to challenge otorhinolaryngologists despite advances in surgical technique and understanding of the wound healing process. There were many surgical methods proposed but no single therapy was proven satisfactory for all cases. Currently, no consensus exists with regards to specific indication for endoscopic versus open surgical management for SGS in children. As for general rules, low grade stenosis (Grade I, II) usually do well and managed expediently with ‘wait and watch’ policy or endoscopic management if failed observation whereas more severe stenosis (Grade III, IV) will need open surgical intervention. Endoscopic advances have been great for the past two decades. Multiple techniques had been described such as CO2 laser excision by Strong and Jako, and radial incision and dilation by Shapshay et al., just to name a few. Review of literatures revealed wide range of success rate, Strong et al. [8], 50 %; Shapshay et al. [9], 44 %; Ossoff et al., 57 % [10]. Restenosis and scar formation remains primary cause of failure. Modulation of wound healing response in preventing scar formation plays a major role in increasing the success. In our study, all patients were subjected to endoscopic dilation and topical mitomycin C application.
As for mechanism of subglottic stenosis, this happens after the trauma to the subglottic mucosa. The placement of ETT causes oedema and hyperemia of the mucosa. It then progresses to pressure necrosis of the mucosa and exposure of the perichondrium of the cricoid cartilage. Scarring of the subglottic area is the end result of the infected perichondrium [11, 12].
Because the fibroblast population and collagen formation is increased during inflammation and the healing process, inhibiting this process should be useful in preventing scar formation. Mitomycin-C acts as an antiproliferative agent that would inhibit fibroblastic activity and scarring. It has been successfully used as an adjunct in glaucoma surgery, dacryocystorhinostomy, optic nerve sheath fenestration, and pterygium recurrence [13–15].
Mitomycin is an antineoplastic antibiotic produced by Streptomyces caespitosus. It is also referred to as mitomycin-C to differentiate it from mitomycin-A and -B, which under certain conditions are also produced. Mitomycin’s mechanism of antineoplastic activity is similar to that of the alkylating agents. Its enzymatic reduction within the susceptible cells is necessary for its antineoplastic activity. It causes cross-linking of DNA and in high concentration can inhibit RNA and protein synthesis. Numerous studies have shown that mitomycin inhibits fibroblast and scar formation in vitro as well as in vivo [16].
Our result has demonstrated that topical application of mitomycin C was beneficial in the modulation of wound healing in decreasing the scarring of our airway stenosis.
In previous published literatures, there were various methods of endoscopic dilatation, be it bougie, balloon, CO2 with or without use of adjunct therapy. There were heterogenous results due to differences in definition of success as mentioned. To date, there are still no comparative studies that evaluate balloon versus rigid dilatation method. Most authors believe balloon dilatation technique provides better result.
Conclusion
With limited facilities in Hospital Queen Elizabeth Sabah, endoscopic bougie dilatation and topical mitomycin C plays a major role in the treatment of subglottic stenosis. Our study demonstrated that mitomycin C is beneficial in improving SGS without any complication and such a procedure can be done in relatively short time. Proper and meticulous intensive care is of utmost importance such as adequate sedation of patients, properly secured ETT to prevent movement, appropriate size use during intubation, intubation by experienced personnel. This will definitely help to reduce the incidence of acquired subglottic stenosis.
References
- 1.Cotton RT, Evans JN. Laryngotracheal reconstruction in children. 5 year follow up. Ann Otol Rhinol Laryngol. 1981;90:516–520. doi: 10.1177/000348948109000522. [DOI] [PubMed] [Google Scholar]
- 2.Holinger PH, Kutnick SL, Schild JA, Holinger LD. Subglottic stenosis in infants and children. Ann Otol Rhinol Laryngol. 1976;85:591–599. doi: 10.1177/000348947608500505. [DOI] [PubMed] [Google Scholar]
- 3.Sasaki CT, Horiuchi M, Koss N. Tracheostomy related subglottic stenosis: bacteriologic pathogenesis. Laryngoscope. 1979;89:857. doi: 10.1288/00005537-197906000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Noyek AM. Xeroradiography in the assessment of the pediatric larynx and trachea. J Otolaryngol. 1976;5:468–474. [PubMed] [Google Scholar]
- 5.Koufman JA. The otolaryngologic manifestation of gastroesophageal reflux disease: a clinical investigation of 225 patients using ambulatory 24 hour pH monitoring and an experimental investigation of the role of acid and pepsin in the development of laryngeal injury. Larungoscope. 1991;101(suppl 53):1. doi: 10.1002/lary.1991.101.s53.1. [DOI] [PubMed] [Google Scholar]
- 6.McDonald IH, Stocks JG. Prolonged nasotracheal intubation. Br J Anaesth. 1965;37:161. doi: 10.1093/bja/37.3.161. [DOI] [PubMed] [Google Scholar]
- 7.Walner DI, Loewen MS, Kimura RE. Neonatal subglottic stenosis—incidence and trends. Laryngoscope. 2001;111(1):48–51. doi: 10.1097/00005537-200101000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Strong MS, Vaughan CW, Polanyi T, Wallace R. Bronchoscopic carbon dioxide laser surgery. Ann Otol Rhinol Laryngol. 1974;83:769–776. doi: 10.1177/000348947408300612. [DOI] [Google Scholar]
- 9.Shapshay SM, Beamis JF, Hybels RL, Bohigian RK. Endoscopic treatment of subglottic and tracheal stenosis by radial laser incision and dilation. Ann Otol Rhinol Laryngol. 1987;96:661–664. doi: 10.1177/000348948709600609. [DOI] [PubMed] [Google Scholar]
- 10.Ossolf RH, Tucker GF, Duncavage JA, Toohill RJ. Efficacy of bronchoscopic carbon dioxide laser surgery for benign strictures of the trachea. Laryngoscope. 1985;95:1220–1223. doi: 10.1288/00005537-198510000-00015. [DOI] [PubMed] [Google Scholar]
- 11.Courey MS. Airway obstruction: the problem and its causes. Otolaryngol Clin N Am. 1995;28(4):673–684. [PubMed] [Google Scholar]
- 12.Eliashar R, Eliachar I, Esclamado R, Gramlich T, Strome M. Can topical mitomycin prevent laryngotracheal stenosis? Laryngoscope. 1999;109(10):1594–1600. doi: 10.1097/00005537-199910000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Doolin EJ, Strande LF, Tsuno K, Santos MC. Pharmacologic inhibition of collagen in an experimental model of subglottic stenosis. Ann Otol Rhinol Laryngol. 1998;107:275–279. doi: 10.1177/000348949810700402. [DOI] [PubMed] [Google Scholar]
- 14.Ingrams DR, Sukin SW, Ashton P, et al. Does Slow-release 5 flurouracil and nolone reduce subglottic stenosis. Otolaryngol Head Neck Surg. 1998;118:174–177. doi: 10.1016/S0194-5998(98)80006-5. [DOI] [PubMed] [Google Scholar]
- 15.Palmer SS. Mitomycin as adjunct chemotherapy with trabeculectomy. Ophthalmology. 1991;98:317–321. doi: 10.1016/S0161-6420(91)32293-0. [DOI] [PubMed] [Google Scholar]
- 16.Jang CH, Song CH, Pak SC. Effect of exposure to mitomycin C on cultured tympanic membrane fibroblasts. Int J Pediatr Otorhinolaryngol. 2003;67:173–176. doi: 10.1016/S0165-5876(02)00367-1. [DOI] [PubMed] [Google Scholar]