Abstract
Objective
To conduct a systematic review to assess the effectiveness of patient education interventions delivered or directed by health professionals for people with musculoskeletal conditions who also have lower levels of literacy.
Methods
Electronic databases were searched from 1946 to May 2012. Randomized controlled trials with primary interventions designed specifically for individuals with musculoskeletal conditions and lower levels of literacy were eligible for inclusion. The quality of the study was determined by assessing method of randomization, allocation concealment, creation and maintenance of comparable groups, blinding of patients and providers, control of confounding, and the validity and reliability of outcome measures.
Results
Of the 2,440 studies located using the search strategy, 6 studies met the inclusion criteria. Three public health community studies and 3 rheumatology clinic-based studies delivered educational programs to people with musculoskeletal conditions who also had lower levels of literacy. Three moderate quality studies suggest that musculoskeletal educational interventions had a small short-term effect on knowledge and 2 moderate quality studies suggest musculoskeletal interventions had a small effect on self-efficacy (although results on self-efficacy were conflicting in 1 of these studies). Only 1 moderate quality study showed a small effect on anxiety and 1 on self-perceived health and well-being in people with lower literacy.
Conclusion
High quality evidence is lacking on the effectiveness of musculoskeletal education interventions for people with lower literacy levels. Research programs that test the effectiveness of patient education interventions for arthritis must recruit and engage people with lower levels of literacy.
INTRODUCTION
Musculoskeletal conditions are a major cause of ill health and disability throughout the world (1). Indicators of such ill health and disability include pain related to the musculoskeletal system (bones and joints) and limitations related to mobility, activities of daily living, and participation in society because of musculoskeletal complaints (1). These indicators can all be addressed through patient education within the health care system. For example, patient education forms an integral part of the management of osteoarthritis (2) and rheumatoid arthritis (RA) (3), two of the most prevalent musculoskeletal conditions (1).
Patient education for musculoskeletal conditions tends to be disease specific (2–5). There is an information deficit underpinning a lack of awareness and understanding of musculoskeletal conditions in general (1). Organizing patient education around musculoskeletal conditions as a whole may lead to transference of knowledge and skills between different health care disciplines and across different chronic disease diagnostic categories, including musculoskeletal conditions. Such transference may lead to a greater understanding of the patient self-management required as part of chronic disease patient education.
Chronic disease management requires active involvement on the part of the patient and health professional (6,7). It is especially important that people with musculoskeletal conditions and other chronic conditions develop effective relationships with their health care providers because of the ongoing nature of their condition. Effective chronic disease management strategies draw on a number of techniques, such as goal setting and problem solving, as well as a fundamental transformation of the patient–health provider relationship (4). However, such techniques, strategies, and engagement require a high level of literacy, self-management skills, and participation on the part of the patient (8–10). This paper focuses on literacy in terms of the ability to read and write, as well as numeracy.
Literacy in a health context is known as health literacy (11,12). The significant and rising prevalence of low literacy is considered a public health crisis (13). A low level of literacy impacts the patient’s ability to access and navigate their way around the health care system, as well as the ability to read information leaflets and sign consent forms (11,12). Health literacy includes these aspects of health care and goes beyond to consider the social skills required to establish a relationship with health care providers. Establishing a relationship requires acknowledgment of tensions underlying the patient–provider relationship in the understanding, enactment, and teaching/learning of chronic disease self-management (14). Patient education is a public health concern as well as a clinical chronic disease self-management and health promotion issue (15). Low literacy and low health literacy are important considerations for each of these different forms of patient education.
In general, individuals with chronic diseases who also have lower levels of literacy experience worse health outcomes and difficulty in understanding and following medical practitioners’ advice (16–19). The risks associated with low literacy have only relatively recently been understood and acknowledged. As a consequence, there has been limited evaluation of patient education interventions for people with musculoskeletal conditions who also have lower levels of literacy. While some evidence exists for a link between low literacy and the impact on health outcomes for musculoskeletal conditions (20–25), the research and review findings are limited by issues concerned with methodologic rigor. Likewise, there is limited evidence-based understanding of the mechanisms underlying the impact of low literacy on health outcomes for people with musculoskeletal conditions.
On a general level it is believed that patient factors implicated in the health literacy causal pathway include a level of knowledge, self-efficacy, beliefs, problem solving, navigation skills, participation in decision making, and motivation, which affect patients’ access and utilization of health care, provider–patient interaction, and self-care (16,26). Provider communication, teaching ability, time management, and patient-centered care are also implicated (16,26). On a system level, the complexity and organization of care is thought to impact on health outcomes through health literacy (16,26).
Moreover, the assumptions underlying health professional practice and research have received little attention. For example, the assumption that provision of information about a chronic disease will assist in self-management has not been fully explored or analyzed for people who have lower levels of literacy (8,27,28). The lack of information on effective patient education interventions for people with lower levels of literacy may increase the poor health outcomes experienced by disadvantaged populations.
This paper reports on the results of a systematic review that explores the effectiveness of patient education interventions (15,29) designed to address patient needs for musculoskeletal conditions in individuals with lower levels of literacy. The research asks the following question: “What are effective patient education interventions for people with musculoskeletal conditions who also have lower levels of literacy?”
Significance & Innovations.
Effects of musculoskeletal patient education interventions are not equal for people with different levels of literacy.
Trials of musculoskeletal patient education interventions do not tend to include a large proportion of people with lower levels of literacy.
Strategies are required to recruit and engage people with lower levels of literacy into musculoskeletal patient education programs.
The internal validity of randomized controlled trials for musculoskeletal patient education is questioned when people with lower literacy levels are not included.
MATERIALS AND METHODS
A standard protocol was developed for the systematic review according to Cochrane review guidelines (30). The study aim and key objectives were specified in order to structure the collection and analysis of data.
Study aim and objectives
The aim of the study was to assess the effectiveness of educational health interventions delivered or directed by health professionals for people with musculoskeletal conditions who also have lower literacy levels. The study objectives were to 1) assess the effectiveness of patient education interventions for people with musculoskeletal conditions who also have lower levels of literacy, 2) review the extent to which literacy levels have been considered in patient education interventions by health professionals or peers, and 3) review the extent to which literacy levels have been considered in self-management interventions.
Data sources and selection
This systematic review was conducted and reported using Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement guidelines (31,32). The sources searched included the Cochrane Central Register of Controlled Trials, OVID Medline, CINAHL (Cumulative Index to Nursing and Allied Health Literature), PsychINFO, ERIC (Educational Resources Information Centre), and EMBase. Grey literature was searched using databases such as MedNar, MAGiC, and ETHOS. Web sites searched included government departments, charitable bodies, professional associations, and some universities. The MeSH headings were developed by a technical expert panel (WL, CB, LF, CE, and JA) with expertise in musculoskeletal conditions, patient education, health literacy, and systematic reviews (see Supplementary Appendix A, available in the online version of this article at http://onlinelibrary.wiley.com/doi/10.1002/acr.22085/abstract). The inclusion and exclusion criteria were developed using the Population Intervention Comparison Outcome Time Setting system (16,30) (see Supplementary Appendix B, available in the online version of this article at http://onlinelibrary.wiley.com/doi/10.1002/acr.22085/abstract).
A systematic review marking (in/out) grid was developed (see Supplementary Appendix C, available in the online version of this article at http://onlinelibrary.wiley.com/doi/10.1002/acr.22085/abstract) and 2 independent reviewers (WL and JA) identified research that met the inclusion criteria. A third reviewer (CB) was available for arbitration on unclear inclusion/exclusion decisions. The reference lists of included papers were scanned for any additional relevant sources of information such as companion papers. Authors were contacted in order to provide further information about their study.
Data extraction and quality assessment
Two independent reviewers (WL and JA) agreed on the data extraction process by consensus. Data were extracted using a form specifically developed for this systematic review given the impact of methodologic issues on the results (12,16,30,31). This process was informed by a number of different sources. However, only the section on risk of bias (internal validity) is reported here (16,30) (see Supplementary Appendix D, available in the online version of this article at http://onlinelibrary.wiley.com/doi/10.1002/acr.22085/abstract). The quality of the study was determined by assessing method of randomization, allocation concealment, creation and maintenance of comparable groups, blinding of patients and providers, control of confounding, and the validity and reliability of outcome measures. This risk of bias tool provided a rating of high, moderate, and low measure of internal validity, which corresponded to a “high level of confidence in the conclusions being correct given the amount of bias”; a “moderate level of confidence: the conclusions are probably correct given the amount of bias”; and “low confidence: the conclusions are not certain because the bias is too large” (16). These ratings followed the Agency for Healthcare Research and Quality Evidence-Based Practice Centers guidelines (16), which were compatible with the criteria for judging risk of bias tool from the Cochrane Collaboration Handbook (30). Two independent reviewers (WL and JA) were responsible for the ratings.
Data synthesis and analysis
The results were synthesized as a narrative. The study effect sizes (ES) were extracted where relevant data were presented so that the influence of each patient education intervention on study outcomes for people with low literacy could be reported. The ES was calculated using the following equation (32):
 |
where = posttest mean − baseline mean (intervention),
= posttest mean − baseline mean (intervention), = posttest mean − baseline mean (control), and Spooled is the pooled SD (pre- or posttest) calculated as
= posttest mean − baseline mean (control), and Spooled is the pooled SD (pre- or posttest) calculated as
 |
A correction factor was calculated to allow for small sample sizes. However, the difference between the unadjusted ES and the corrected ES was found to be negligible. The correction factor for small sample size
 |
RESULTS
Study selection
The study flow diagram according to PRISMA guidelines (33) is shown in Figure 1, which reports the processes of identification, screening, eligibility, and inclusion (34–51). The full 2,444 citations identified from the search processes were reviewed by their titles and abstracts using the marking grid developed for the project (see Supplementary Appendix C, available in the online version of this article at http://onlinelibrary.wiley.com/doi/10.1002/acr.22085/abstract). Of these, 14 were deemed eligible for full text review to discern whether they met the inclusion and exclusion criteria. One article could not be obtained in spite of extensive attempts (47) and 2 were written in languages other than English (48,49). The remaining 2 articles were in abstract form only from conference proceedings (38,45). Eight studies (11 citations) were subjected to the data extraction process. Following this, 2 studies were excluded because (although literacy levels were measured) the study intervention did not primarily address lower levels of literacy (50,51). Six studies (9 citations) were in the final review (38–46). The vast majority of excluded studies did not include any measure of health literacy or literacy. These were randomized controlled trials (RCTs) on different patient education interventions, including self-management for people with musculoskeletal conditions.
Figure 1.
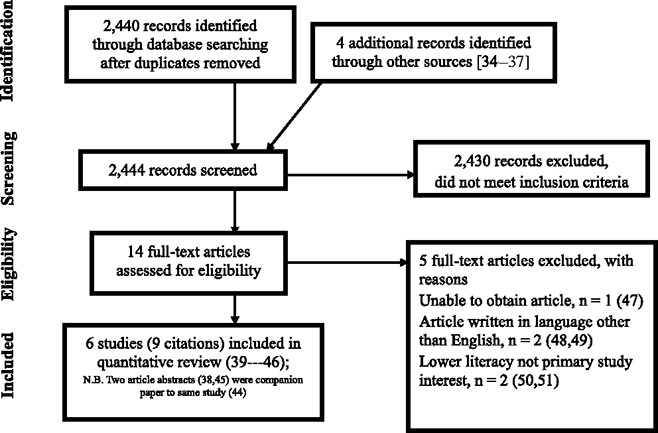
Study flow diagram.
Study characteristics
The study characteristics of each research study are presented in Table1. Research on people with lower literacy levels who also had musculoskeletal conditions was conducted across 4 different countries, i.e., UK, US, Indonesia, and India.
Table 1.
Summary of characteristics of patient education interventions for people with musculoskeletal conditions who also have lower levels of literacy∗
| Source | Design (sample size) | Population | Literacy/health literacy levels | Control | Intervention | Outcomes |
|---|---|---|---|---|---|---|
| Hill and Bird, 2003 (41) | RCT (n = 100) | UK rheumatology clinic patients | Reading ability (Holborn Scale) 12% of sample had reading age <13 years | Drug information leaflet only | Drug information leaflet and verbal explanation | DPA questionnaire |
| Rudd et al, 2009 (44) | RCT (n = 127) | US rheumatology clinic patients | 18% < high school on A-REALM | Standard care; Arthritis Foundation notebook with rheumatology clinic visit only | Plain English notebook with access to educator for 2 visits over 12 months, guides to navigating health system, individualized approach | SF-36 mental subscale satisfaction, HAQ score, self-efficacy, medication adherence, appointment keeping |
| Walker et al, 2007 (46) | RCT (n = 363) | Patients in 3 UK rheumatology clinics | REALM <60 = 15% of sample, <45 = 4%; i.e., 19% of sample were poor readers (<60) | ARC booklet only | ARC booklet and mind map | HAQ, REALM, PKQ |
| Darmawan et al, 1992 (39) | RCT (n = 844) | Randomly selected people positively identifying as having MSK pain in rural Indonesia | Illiteracy/literacy according to school attendance | No intervention | ACE puppet play of popular Hindu epic, which included simple instructions for coping with neck and back pain, and deformed, stiff, swollen, or painful joints; posture, positioning, joint protection, exercises, functional level improvement | Dichotomous pictoquestionnaire, pre/posttest (1 and 6 months) |
| Goeppinger et al, 2007 (40) | RCT (n = 499) | Community participants with self-reported physician diagnosis of any type of arthritis or persistent chronic joint pain as defined by CDC; held in US | Proxy measure of literacy/level of education | Comparison between different self-management programs (ASHC and CDSMP), participants randomly assigned to either intervention | ASHC, CDSMP, group workshops, 6 weeks, 2–25 hours each week | Health care use, health-related quality of life, self-management behaviors, self-efficacy for arthritis self-management |
| Rana et al, 2010 (42) | Quasi-experimental study of 8 randomly selected villages in rural Bangladesh (n = 839) | Community participants with self-reported arthritis-related illness; all forms of arthritis, back and joint pain, biting sensation, joint swelling and inflammation | Educational status categorized as literate or illiterate; literate group comprised those reporting ability to read/write local language (Bangla) | No intervention | Health advice, home-based physical activities, aspects of health care management; individual and group sessions, distribution of leaflets, video documentaries, and theatre performances to increase likelihood of participation | Self-rated health, self-rated arthritis, self-reported compliance in intervention group |
RCT = randomized controlled trial; DPA = D-penicillamine; A-REALM = Arthritis Rapid Estimate of Adult Literacy in Medicine; SF-36 = Short Form 36 health survey; HAQ = Health Assessment Questionnaire; ARC = Arthritis Research Campaign; PKQ = Patient Knowledge Questionnaire; MSK = musculoskeletal; ACE = Arthritis Community Education; CDC = Centers for Disease Control and Prevention; ASHC = Arthritis Self-Help Course; CDSMP = Chronic Disease Self-Management Program.
Two studies were conducted in the UK (41,46), 2 were conducted in the US (40,44), and 1 was conducted in each of India (42) and Indonesia (39). Sample sizes ranged from 100 to 844 participants with larger sample sizes for the community-oriented education interventions (India, Indonesia, and US). The mean ± SD age range was 58.5 ± 13.8 years (44) to 70.6 ± 7.3 years (42) giving an overall mean ± SD age of 63.09 ± 11.55 years for all the studies. Musculoskeletal conditions included RA and arthritis. Only 1 study reported the presence of comorbidities (mean ± SD 4.2 ± 1.88 additional symptoms, including most commonly hypertension, overweight, and diabetes mellitus) (40). Literacy levels were measured using the Arthritis Rapid Estimate of Adult Literacy in Medicine (A-REALM) (44), the Rapid Estimate of Adult Literacy in Medicine (REALM) (46), the Holborn test of reading ability (41), the ability to read and write the local dialect (39,42), and a through proxy measure of educational level (40). Although the studies were reported as RCTs, the processes of randomization and blinding were limited. Three clinical rheumatology studies (41,44,46) provide comparison and contrast to 3 community-based studies (39,40,42). All had limitations with their methodologic rigor.
The 3 clinical rheumatology studies focused on reducing the literacy burden of patient education leaflets (41) and Arthritis Research Campaign (ARC) booklets (44,46) with 1 study providing additional strategies, such as guides to navigating the health care system, an individualized approach, and access to an educator over 12 months (44). One study provided an additional verbal explanation of a drug information leaflet (41). The 3 community-based studies included a range of strategies such as information on correct positioning, performance of activities of daily living (39), and comprehensive chronic disease management programs (40), as well as individual and group strategies on physical activity and health care management (42), often through innovative means such as theatre and puppetry (39,42).
Methodologic quality
All studies were described as RCTs. All studies reported information about attrition rates, which were generally low (all <26%) except for 1 with high attrition rates at 12 months (40). Only 1 study described the attrition rate due to medication side effects (41). All 6 studies provided a thorough description of the intervention, although less information was forthcoming about a theoretical framework or a model of teaching and learning. The risk of bias tool (17,31) used in the data extraction provided information about the strength of evidence.
Strength of evidence
The evidence reported from each study was assessed for internal validity using a risk of bias tool (17,31). Generally, the 6 studies performed moderately with the biggest challenges provided by the processes of randomization, blinding, and whether confounding factors were taken into account or discussed. The processes of randomization, blinding, and the presence of potential confounding factors affected the internal validity (see Supplementary Appendix D, available in the online version of this article at http://onlinelibrary.wiley.com/doi/10.1002/acr.22085/abstract).
Issues of concern for the clinically based studies included study participants having a high level of literacy and, therefore, the intervention was not tested on the target population with lower levels of literacy (41,42); that taking medication both increased knowledge gained (46) and accounted for the attrition rate by withdrawal due to medication side effects (41); difficulty recruiting meant that the study design had to be changed (44); patients tended to rely on health professionals as the source of information, not the intervention (i.e., information booklet) (46); and limited stratification due to small sample sizes so that the results did not take into account ethnicity, socioeconomic status, disease severity and duration, or comorbidity (41,44,46).
In contrast, community-based studies of lower levels of literacy reached the target population with samples, including greater proportions of people with lower levels of literacy. The larger sample sizes could have reduced the effect of some of the methodologic issues across all studies. Issues of concern included that measurement of literacy tended to be by a proxy, such as education level or classification into literate or illiterate based on the participants’ ability to read and write the local language (39,42,43). The community-based interventions were tailored to people with lower levels of literacy by drawing on a range of modalities for engaging people and disseminating information, whereas the clinical studies tended to rely on written information alone (46) or with the addition of verbal support (41,42).
In order to maximize the learning opportunity provided, this systematic review is inclusive of a range of approaches to patient education for arthritis. The 6 studies that were included in the systematic review ranged across the public health (39,42), clinical (41,44,46), and social science/education disciplines (40). While theoretical frameworks demonstrated disciplinary differences, there was some overlap in the outcomes.
Intervention methods
Interventions ranged from distribution of simple leaflets about medication with additional verbal explanation (41), the ARC booklet and mind map (46), to the distribution of Arthritis Foundation and plain language notebook with access to an educator for 2 visits over 6 months (44) in the clinical model.
In contrast, the community-based interventions for people with lower levels of literacy were multiple. Based on 2 self-management programs (Arthritis Self-Help Course [ASHC] and Chronic Disease Self-Management Program [CDSMP]) with cultural adaptations through participatory action research, 1 study recruited African American people for 6-week programs on diet, exercise, and lifestyle advice for arthritis (40). Likewise, Rana et al (42) and Darmawan et al (39) drew on a range of interventions to reach community members that were not just based around reading and writing. Rana et al provided a prolonged 15-month period of interventions based on lifestyle advice such as lifting, diet, and exercise, and through modalities such as leaflets, videos, and theatre performances to focus on arthritis-related illness and self-rated health (42). Darmawan et al used theatre puppetry to integrate the arthritis self-care messages into the local culture to increase knowledge and comprehension (39).
Proportion of sample with lower levels of literacy
The percentage of people with lower literacy in the study sample ranged from 15% (REALM score <60; cutoff point for literacy level necessary to function in a health context) (46) to 12% having a reading age of ≤13 years (41), with 21% (control) and 16% (intervention) having an A-REALM score that was less than high school–level education, although the exact measure is not clear (44). The actual attendance for high school or less was 52% (control) and 48% (intervention group) (44).
The proportion of participants who had levels of literacy equivalent to high school was high in the study by Goeppinger et al (40). The mean ± SD number of years of education was 11.7 ± 3.14 for all participants and 11.7 ± 3.18 for African American people; therefore, most people completed high school. The actual percentages of people with lower levels of literacy were not stated.
The study by Darmawan et al showed a large percentage of people who were classified as illiterate: 76% (control group) and 75% (intervention group) (39). The study by Rana et al reported that 37.8% of study participants were literate; therefore, 62.2% of study participants were categorized as illiterate (42).
Patient outcomes
Knowledge
Three studies showed an increase in knowledge as a result of the intervention (39,41,46), although there was evidence that the knowledge gained was not equal across all groups (46). Participants with higher levels of literacy tended to gain more knowledge (46). Results from 1 study demonstrated that at 6 months, illiteracy was positively correlated with a loss of knowledge, which was also associated with being older (39). Table2 presents the percentage of correct responses for the patient education intervention across different literacy groups (39) and Table3 presents the percentage change in self-efficacy (40). Studies that provided raw data, including SDs, from which effect sizes were calculated, are included in Table4.
Table 2.
Percentage correct responses for patient education intervention∗
| Before ACE | 1 month postintervention | 6 months postintervention | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Author | Literacy/education level | Intervention (no.) | Control (no.) | Intervention | Control | Intervention | Control | Intervention | Control |
| Darmawan et al, 1992 (39) (n = 844) Knowledge | Illiterate | 302 | 289 | 52.2 | 52.3 | 82.0 | 52.4 | 57.6 | 50.0 |
| Primary school | 61 | 58 | 60.1 | 69.1 | 91.0 | 71.1 | 77.1 | 72.2 | |
| Junior high school | 21 | 20 | 67.1 | 78.1 | 86.7 | 80.0 | 78.6 | 76.3 | |
| Senior high school | 15 | 13 | 77.1 | 80.0 | 91.7 | 87.5 | 80.0 | 77.8 | |
| Academy/university | 2 | 2 | 100.0 | 84.6 | 100.0 | 98.2 | 100.0 | 96.4 | |
ACE = Arthritis Community Education.
Table 3.
Percentage increase of self-efficacy∗
| 4-month outcomes | 12-month outcomes | |||||
|---|---|---|---|---|---|---|
| Author | Intervention (no.) | Control (no.) | ASHC | CDSMP | ASHC | CDSMP |
| Goeppinger et al, 2007 (40) | ||||||
| Self-efficacy, all participants | 231 | 185 | ↑12.9%; P = 0.004 | ↑14.1%; P = 0.038 | No statistically significant changes | No statistically significant changes |
| Self-efficacy, African American participants | 208 | 157 | ↑12.5%; P = 0.005 | ↑11.2%; P = 0.102 | No statistically significant changes | No statistically significant changes |
ASHC = Arthritis Self-Help Course; CDSMP = Chronic Disease Self-Management Program.
Table 4.
Effect size (ES) and summary data of outcomes where presented for 4 included studies∗
| Author | Outcome | Participants, no. | Intervention, mean ± SD | Control, mean ± SD | ES (95% CI) |
|---|---|---|---|---|---|
| Hill and Bird, 2003 (41) | Knowledge | nI = 51 | Pretest 2.8 ± 3.5 | Pretest 2.57 ± 2.54 | 0.22 (−0.19, 0.62) |
| nC = 49 | Posttest 10.8 ± 2.03 | Posttest 9.90 ± 2.46 | |||
| Walker et al, 2007 (46) | Knowledge | nI = 175 | PKQ 62.26 ± 9.12 | PKQ 63.28 ± 7.96 | −0.013 (−0.22, 0.19) |
| nC = 188 | Increase in knowledge 6.45 (95% CI 3.78, 10) | Increase in knowledge 6.56 (95% CI 3.36, 8.75) | |||
| Rudd et al, 2009 (44) | Self-efficacy, 6 months | nI = 49 | Pretest 2.78 ± 0.49 | Pretest 2.87 ± 0.48 | 0.39 (0.009, 0.775) |
| nC = 57 | Posttest 2.83 ± 0.54 | Posttest 2.73 ± 0.59 | |||
| Self-efficacy, 12 months | nI = 48 | Pretest 2.78 ± 0.49 | Pretest 2.87 ± 0.48 | 0.454 (0.069, 0.839) | |
| nC = 57 | Posttest 2.91 ± 0.63 | Posttest 2.78 ± 0.59 | |||
| SF-36, 6 months | nI = 49 | Pretest 74.8 ± 12.6 | Pretest 75.0 ± 18.4 | 0.413 (−0.554, 1.38) | |
| nC = 57 | Posttest 77.7 ± 14.1 | Posttest 71.3 ± 23.9 | |||
| SF-36, 12 months | nI = 48 | Pretest 74.8 ± 12.6 | Pretest 75.0 ± 18.4 | 0.362 (−0.511, 1.236) | |
| nC = 57 | Posttest 78.6 ± 15.3 | Posttest 73.0 ± 19.2 | |||
| Rana et al, 2010 (42) | Arthritis-related illness | nI = 425 | Dichotomous variables | OR 1.9 (1.3–2.8) | |
| Self-reported health | nC = 414 | Dichotomous variables | OR 1.4 (1.0–1.9) |
95% CI = 95% confidence interval; nI = intervention; nC = control; PKQ = Patient Knowledge Questionnaire; SF-36 = Short Form 36 health survey; OR = odds ratio.
The increase in knowledge was significant for people who were illiterate and those who attended primary school (P < 0.05 at 1 month) (38). At 6 months, illiteracy in the intervention group was associated with a significant loss of knowledge gained at 1 month after Arthritis Community Education, reported as a correlation coefficient of 0.874, P > 0.05 (39). People who were illiterate were predominantly middle-aged and elderly, while primary school attendees were mainly younger people (39).
The SDs and effect sizes were not reported. The increase in knowledge 1 month after the intervention for those who were illiterate was significant (P < 0.05) at a 95% confidence interval (95% CI) for difference of means (−31.90, −27.70). This effect became insignificant (P > 0.05) 6 months after intervention (95% CI −8.05, 2.75). For those that attended primary school the effect was again most significant at 1 month (P < 0.05; 95% CI for difference of means −31.60, −30.20). This knowledge was retained at 6 months after intervention (P < 0.05; 95% CI −18.30, 15.70).
In terms of the content, isometric exercises were the least understood. Only approximately two-thirds of responses were correct for isotonic exercises. Approximately 75% of responses were correct for positioning painful joints (39).
One study demonstrated no difference in knowledge gained between intervention and control (41). Eighty-four patients had a reading age of 13 years and 9 months (the rest were below that score). The increase in knowledge was statistically significant at P < 0.0001. However, there were no differences between groups; therefore, the additional verbal explanation made no difference (P = 0.109).
Self-efficacy
All participants in the ASHC showed improvements in self-efficacy, which were maintained at 4 and 12 months (P = 0.036) (39). For a subgroup analysis of African American participants, the modest improvement in self-efficacy was not statistically significant (40).
Among all ASHC participants (n = 83), only the 4-month improvement in arthritis self-efficacy was maintained for 12 months (14.9%; P = 0.036). Among African American ASHC participants (n = 76), there was modest, although not statistically significant, maintenance in self-efficacy improvements from baseline (P = 0.069) (40).
None of the CDSMP participants (n = 84) had statistically significant changes at 12 months. An increase in practice of cognitive stress management emerged as statistically significant (81%; P = 0.031). The improvement in stretching and strengthening approached statistical significance (83.3%; P = 0.055) (40).
The study by Rudd et al (44) showed that the intervention had a significant effect (P = 0.05 at 6 months and P = 0.04 at 12 months) on self-efficacy in the univariate analysis. This effect was not sustained in the multivariate analysis (P = 0.12) when covariates such as age, work status, literacy level, annual family income, and baseline values of outcome measures were taken into consideration.
Anxiety
Rudd et al (44) showed a slight lessening of anxiety experienced by participants at 6 months in the intervention group (P = 0.04). In another study, although the change in anxiety was not measured, poorer readers and less knowledgeable participants were significantly more anxious (P = 0.01) and more depressed (P = 0.006) than better readers (46).
Arthritis-related illness and self-rated health
Arthritis-related illness decreased and self-rated health improved in the group compliant with arthritis education advice (42). Literate and nonpoor participants were more likely to report positive health, and participants with advancing age were less likely to report positive health. For all other outcomes, the differences between the intervention and the control group were not statistically significant.
Summary of evidence
Table4 reports the ES for the increase in knowledge for the studies by Hill and Bird (41) and Walker et al (46) and for self-efficacy in the study by Rudd et al (44), as well as the study by Rana et al (42). The interventions provided a small effect for knowledge and self-efficacy (31,52,53).
DISCUSSION
In this systematic review of interventions designed specifically for people with musculoskeletal conditions who also have lower levels of literacy, a number of different approaches to patient education were explored. These approaches included changing leaflet design, providing additional verbal back-up in a clinical model of musculoskeletal conditions intervention, comprehensive culturally tailored self-management programs designed specifically for people in the African American community, and, finally, a range of information and advice-giving formats, such as face-to-face counseling, video, theatre, and puppetry.
Evidence for the effects of these interventions on health outcomes was small, especially for people with lower literacy levels who were underrepresented in clinical intervention trial populations. An increase in knowledge was recorded by 3 studies (39,41,46), although this was not equal across all literacy groups (46). For one study, an increase in self-efficacy was demonstrated at 4 and 12 months, although not for all ethnic groups (40). Another study demonstrated an increase in self-efficacy, although this effect was not sustained once contextual factors were taken into account in the analysis (44). The effect sizes for knowledge and self-efficacy were small, although of the same magnitude as those reported elsewhere (54,55). One area for future work is to establish expected effect sizes for musculoskeletal patient education interventions for people with lower levels of literacy. The methodologic quality of these quantitative studies in support of patient education interventions meant that the strength of evidence could only be described as moderate (17,31). This could be due to a number of factors that affect internal validity and include risk of bias, potential confounding (medication, disease severity, comorbidity), small sample sizes and lack of a priori power calculations (41,44,46), relatively high level of literacy of participants (41,44,46), difficulty recruiting people with lower levels of literacy, and limited use of theoretical frameworks to underpin educational interventions (56).
The limited theoretical frameworks can also influence the analysis of the effect of interventions due to a limited understanding of the mediators and moderators of an intervention. The heterogeneity of studies and associated confounding factors provides a case for strong analytical frameworks that can help researchers to design studies addressing lower levels of literacy that show strong, consistent associations between patient education interventions and health outcomes for people with musculoskeletal conditions (56,57). Therefore, the effectiveness of patient education interventions for people with musculoskeletal conditions who also have lower levels of literacy can only be inferred at this stage due to the very small number of studies that address this issue and the small number of participants with lower literacy levels included. At present, the impact of lower literacy on patient education interventions for people with musculoskeletal conditions tends to manifest as a lack of recruitment and engagement with people with lower levels of literacy. Strategies are required to engage people with lower levels of literacy in the design and development of trials testing patient education interventions.
Part of the reason that the interventions may not have been as effective as they could be was because they did not reach the intended population. Although the percentages reflect the significant minority of people in the community who have lower levels of literacy (for example, 22% of adults in the US are disadvantaged by their literacy skills, which are at National Adult Literacy Survey Level 1 [12]; in Australia, the prevalence of inadequate health literacy ranges from 7% to 21% depending on the measure [57]), the interventions cannot claim to focus solely on people with lower levels of literacy. In some cases the proportion of people with lower levels of literacy was not stated as there was a reliance on proxy measures of literacy (40). Using educational levels as a proxy measure for literacy has been criticized as they do not always reflect literacy levels (56).
The extent to which health literacy has been considered in patient education interventions, including self-management, is limited (58). The limited consideration of health literacy and of literacy requirements of patient education interventions could be part of the reason for the persistence of health inequalities. Inequities in health outcomes may be introduced at many points during the planning and delivery of interventions, particularly if these interventions have an educational component, are one-size-fits-all, rely on voluntary behavior change, and incur costs to the patient (59).The translation of patient education research results across different chronic diseases has been limited.
The limitations of this systematic review reflect the nature of the field. The small number of studies, heterogeneity in settings and outcome measures, and limited theoretical frameworks and measurement tools meant that the studies could not be combined in a meta-analysis. However, exploring the current state of patient education interventions for people with musculoskeletal conditions who also have lower literacy levels has meant that areas for improvement in study design can now be explored in depth in order to provide meaningful changes for patients, health care providers, and systems. The risk of publication bias means that a more positive effect for patient education interventions could be shown when this is not the case. However, this is unlikely in this systematic review since there was not strong evidence for the benefit of patient education interventions for people with musculoskeletal conditions and lower levels of literacy.
In conclusion, high quality evidence is lacking on the effectiveness of musculoskeletal education interventions for people with lower literacy levels. An urgent matter seems to be how to recruit and engage people with lower levels of literacy and musculoskeletal conditions into research programs that test the effectiveness of patient education interventions.
AUTHOR CONTRIBUTIONS
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be submitted for publication. Dr. Lowe had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design. Lowe, Ballinger, Protheroe, Lueddeke, Nutbeam, Armstrong, Falzon, Edwards, Russell, McCaffery, Adams.
Acquisition of data. Lowe, Ballinger, Falzon, Edwards, Adams.
Analysis and interpretation of data. Lowe, Adams.
Acknowledgments
We would like to acknowledge Helena Smartt, Katie McDonell, Dimoula Eracli, Dimitris Stavropoulos, Simona Dagyte, and Dr. Solange Correa Onel for their statistical advice. We would also like to thank the two anonymous reviewers for their helpful advice.
Supporting Information
Additional Supporting Information may be found in the online version of this article.
Supplementary Appendix A
Supplementary Appendix B
Supplementary Appendix C
Supplementary Appendix D
REFERENCES
- WHO Technical Report Series. The burden of musculoskeletal conditions at the start of the new millennium. Geneva: World Health Organization; 2003. [PubMed] [Google Scholar]
- Jordan KM, Arden NK, Doherty M, Bannwarth B, Bijlsma JW, Dieppe P, et al. EULAR recommendations 2003: an evidence based approach to the management of knee osteoarthritis. Report of a task force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT) Ann Rheum Dis. 2003;62:1145–55. doi: 10.1136/ard.2003.011742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brosseau L, Wells GA, Tugwell P, Egan M, Dubouloz CJ, Welch VA, et al. Ottawa panel evidence-based clinical practice guidelines for patient education in the management of rheumatoid arthritis (RA) Health Educ J. 2012 URL: http://hej.sagepub.com/content/71/4/397. [Google Scholar]
- Warsi A, LaValley MP, Wang PS, Avorn J, Solomon DH. Arthritis self-management education programs: a meta-analysis of the effect on pain and disability. Arthritis Rheum. 2003;48:2207–13. doi: 10.1002/art.11210. [DOI] [PubMed] [Google Scholar]
- Reisma R, Kirwan J, Taal E, Rasker J. Patient education for adults with rheumatoid arthritis. Cochrane Database Syst Rev. 2002;3 doi: 10.1002/14651858.CD003688. :CD003688. [DOI] [PubMed] [Google Scholar]
- De Silva D. Evidence: helping people help themselves. London: Health Foundation; 2011. [Google Scholar]
- National Institute for Clinical Excellence. 2012. . Patient experience in adult NHS services: improving the experience of care for people using adult NHS services. URL: http://guidance.nice.org.uk/CG138/NICEGuidance/pdf/english.
- Adams RJ. Improving health outcomes with better patient understanding and education. Risk Manag Healthc Policy. 2010;3:61–72. doi: 10.2147/RMHP.S7500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Audulv A, Asplund K, Norbergh KG. Who’s in charge? The role of responsibility attribution in self-management among people with chronic illness. Patient Educ Couns. 2010;81:94–100. doi: 10.1016/j.pec.2009.12.007. [DOI] [PubMed] [Google Scholar]
- Townsend A, Wyke S, Hunt K. Self-managing and managing self: practical and moral dilemmas in accounts of living with chronic illness. Chronic Illn. 2006;2:185–94. doi: 10.1177/17423953060020031301. [DOI] [PubMed] [Google Scholar]
- Nutbeam D. Health promotion glossary. Health Promot Int. 1998;13:349–64. [Google Scholar]
- Nielsen-Bohlman L, Panzer AM, Kindig D, editors. Committee on Health Literacy and Board of Neuroscience and Behavioural Health. Health literacy: a prescription to end confusion. Washington: National Academies Press; 2004. , editors, for the. [PubMed] [Google Scholar]
- Parker RM, Wolf MS, Kirsch I. Preparing for an epidemic of limited health literacy: weathering the perfect storm. J Gen Intern Med. 2008;23:1273–6. doi: 10.1007/s11606-008-0621-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holm S. Justifying patient self-management: evidence-based medicine or the primacy of the first person perspective. Med Health Care Philos. 2005;8:159–64. doi: 10.1007/s11019-005-2280-x. [DOI] [PubMed] [Google Scholar]
- Caraher M. Patient education and health promotion: clinical health promotion. The conceptual link. Patient Educ Couns. 1998;33:49–58. doi: 10.1016/s0738-3991(97)00055-4. [DOI] [PubMed] [Google Scholar]
- Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Viera A, Crotty K, et al. Health literacy interventions and outcomes: an updated systematic review. Evid Rep Technol Assess. 2011;199:1–941. [PMC free article] [PubMed] [Google Scholar]
- Loke YK, Hinz I, Wang X, Rowlands G, Scott D, Salter C. Impact of health literacy in patients with chronic musculoskeletal disease: systematic review. PLoS One. 2012;7:e40210. doi: 10.1371/journal.pone.0040210. . URL: http://www.plosone.org/article/info:doi/10.1371/journal.pone.0040210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheridan SL, Halpern DJ, Viera AJ, Berkman ND, Donahue KE, Crotty K. Interventions for individuals with low health literacy: a systematic review. J Health Commun. 2011;(Suppl 3):30–54. doi: 10.1080/10810730.2011.604391. [DOI] [PubMed] [Google Scholar]
- Berkman ND, Sheridan S, Donahue K, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155:97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- Gordon MM, Hampson R, Capell HA, Madhok R. Illiteracy in rheumatoid arthritis as determined by the Rapid Estimate of Adults Literacy in Medicine (REALM) score. Rheumatology (Oxford) 2002;41:750–4. doi: 10.1093/rheumatology/41.7.750. [DOI] [PubMed] [Google Scholar]
- Buchbinder R, Hall S, Youd JM. Functional health literacy of patients with rheumatoid arthritis attending a community-based rheumatology practice. J Rheumatol. 2006;33:879–86. [PubMed] [Google Scholar]
- Kim SH. Health literacy and functional health status in Korean older adults. J Clin Nurs. 2009;18:2337–43. doi: 10.1111/j.1365-2702.2008.02739.x. [DOI] [PubMed] [Google Scholar]
- Hirsh JM, Boyle DJ, Collier DH, Oxenfield AJ, Caplan L. Health literacy predicts the discrepancy between patient and provider global assessments of rheumatoid arthritis activity at a public urban rheumatology clinic. J Rheumatol. 2010;37:961–6. doi: 10.3899/jrheum.090964. [DOI] [PubMed] [Google Scholar]
- Swearingen CJ, McCollum L, Daltroy LH, Pincus T, DeWalt DA, Davis TC. Screening for low literacy in a rheumatology setting: more than 10% of patients cannot read “cartilage,” “diagnosis,” “rheumatologist,” or “symptom.”. J Clin Rheumatol. 2010;16:359–64. doi: 10.1097/RHU.0b013e3181fe8ab1. [DOI] [PubMed] [Google Scholar]
- Hirsh JM, Boyle DJ, Collier DH, Oxenfeld AJ, Nash A, Quinzanos I, et al. Limited health literacy is a common finding in a public health hospital’s rheumatology clinic and is predictive of disease severity. J Clin Rheumatol. 2011;17:236–41. doi: 10.1097/RHU.0b013e318226a01f. [DOI] [PubMed] [Google Scholar]
- Paasche-Orlow MK, Wolf M. The causal pathways linking health literacy to health outcomes. Am J Health Behav. 2007;(Suppl 1):19–26. doi: 10.5555/ajhb.2007.31.supp.S19. [DOI] [PubMed] [Google Scholar]
- Protheroe J, Rogers A, Kennedy AP, Macdonald W, Lee V. Promoting patient engagement with self-management support information: a qualitative meta-synthesis of processes influencing uptake. Implement Sci. 2008;8:44. doi: 10.1186/1748-5908-3-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borkhoff CM, Wieland ML, Myasoedova E, Ahmad Z, Welch V, Hawker GA, et al. Reaching those most in need: a scoping review of interventions to improve health care quality for disadvantaged populations with osteoarthritis. Arthritis Care Res (Hoboken) 2011;63:39–52. doi: 10.1002/acr.20349. [DOI] [PubMed] [Google Scholar]
- Lorig K. Patient education: treatment or nice extra. Br J Rheumatol. 1995;34:703–6. doi: 10.1093/rheumatology/34.8.703. [DOI] [PubMed] [Google Scholar]
- Higgins JP, editor; Green S, editor. editors. Cochrane handbook for systematic reviews of interventions: version 5.1.0. 2011. . URL: www.cochrane-handbook.org.
- Gough D, Oliver S, Thomas J. An introduction to systematic reviews. London: Sage; 2012. [Google Scholar]
- Wilson DB, Gottfredson DC, Najaka SS. School-based prevention of problem behaviours: a meta-analysis. J Quant Criminol. 2001;17:247–72. [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:7;1–6.e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhat AA. 2008. Literacy in arthritis [dissertation]. Chapel Hill (NC): University of North Carolina;
- Blanch D, Rudd R, Wright E, Gall V, Katz JN. Predictors of refusal during a multi-step recruitment process for a randomized controlled trial of arthritis education. Patient Educ Couns. 2008;73:280–5. doi: 10.1016/j.pec.2008.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinlan P. 2009. The relationship between health literacy, health knowledge and adherence to treatment in patients with rheumatoid arthritis [dissertation]. New York: Columbia University;
- Thorn BE, Day MA, Burns J, Kuhajda MC, Gaskins SW, Sweeney K, et al. Randomized trial of group cognitive behavioural therapy compared with pain education control for low literacy rural people with chronic pain. Pain. 2011;152:2710–20. doi: 10.1016/j.pain.2011.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanch D, Rudd R, Wright E, Gall V, Katz JN. Literacy-related strategies to enhance recruitment to a randomized controlled trial of arthritis education. Arthritis Rheum. 2005;52(Suppl):S667–8. [abstract]. [Google Scholar]
- Darmawan J, Muirden KD, Wigley RD, Valkenburg HA. Arthritis community education by leather puppet (wayang kulit) shadow play in rural Indonesia (Java) Rheumatol Int. 1992;12:97–101. doi: 10.1007/BF00290262. [DOI] [PubMed] [Google Scholar]
- Goeppinger J, Armstrong B, Schwartz T, Ensley D, Brady TJ. Self-management education for persons with arthritis: managing comorbidity and eliminating health disparities. Arthritis Rheum. 2007;57:1081–8. doi: 10.1002/art.22896. [DOI] [PubMed] [Google Scholar]
- Hill J, Bird H. The development and evaluation of a drug information leaflet for patients with rheumatoid arthritis. Rheumatology (Oxford) 2003;42:66–70. doi: 10.1093/rheumatology/keg032. [DOI] [PubMed] [Google Scholar]
- Rana AK, Kabir ZN, Lundborg CS, Wahlin A. Health education improves both arthritis-related illness and self-rated health: an intervention study among older people in rural Bangladesh. Public Health. 2010;124:705–12. doi: 10.1016/j.puhe.2010.07.005. [DOI] [PubMed] [Google Scholar]
- Rana AK, Lundborg CS, Wahlin A, Ahmed SM, Kabir ZN. The impact of health education in managing self-reported arthritis-related illness among elderly persons in rural Bangladesh. Health Educ Res. 2008;23:94–105. doi: 10.1093/her/cym002. [DOI] [PubMed] [Google Scholar]
- Rudd RE, Blanch DC, Gall V, Chibnik LB, Wright EA, Reichmann W, et al. A randomized controlled trial of an intervention to reduce low literacy level barriers in inflammatory arthritis management. Patient Educ Couns. 2009;75:334–9. doi: 10.1016/j.pec.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudd RE, Chibnik LB, Gall V, Wright E, Blanch D, Reichmann W, et al. Preliminary results of a randomized controlled trial (RCT) of a literacy based educational intervention in arthritis management. Arthritis Rheum. 2006;54(Suppl):S766. . [abstract]. [Google Scholar]
- Walker D, Adebajo A, Heslop P, Hill J, Firth J, Bishop P, et al. Patient education in rheumatoid arthritis: the effectiveness of the ARC booklet and the mind map. Rheumatology (Oxford) 2007;46:1593–6. doi: 10.1093/rheumatology/kem171. [DOI] [PubMed] [Google Scholar]
- Keshtkaran Z, Ghodsbin F, Solouki S, Razeghi M, Zare N. The impact of self-care education on quality of life of those clients suffering from osteoarthritis in rehabilitation centres of Shiraz University of Medical Science (Iran) LA Ara J Babol Univ Med Sci. 2010;12:8–15. [Google Scholar]
- Cardiel MH, Ruiz-Mercado R, Glave C, Abello M, Herrera-Lasso I, Mobarak L, et al. A randomized controlled trial to evaluate the effectiveness of two educational modalities in patients with rheumatoid arthritis (RA) Arthritis Rheum. 1992;35(Suppl):S123. [Google Scholar]
- Rodriguez LC, Bilbao A, Naranjo A, Ojeda S, Francisco F. Patient education in rheumatoid arthritis: its influence in the disease outcome. Revista Espanola De Reumatologia. 1996;23:40–8. . In Spanish. [Google Scholar]
- Ackerman IN, Buchbinder R, Osborne RH. Challenges in evaluating an arthritis self-management program for people with hip and knee osteoarthritis in real-world clinical settings. J Rheumatol. 2012;39:1047–55. doi: 10.3899/jrheum.111358. [DOI] [PubMed] [Google Scholar]
- Bhat AA, DeWalt DA, Zimmer CR, Fried BJ, Callahan LF. The role of helplessness, outcome expectation for exercise and literacy in predicting disability and symptoms in older adults with arthritis. Patient Educ Couns. 2010;81:73–8. doi: 10.1016/j.pec.2009.12.004. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioural sciences. 2nd ed. Englewood Cliffs (NJ): Lawrence Erlbaum Associates; 1988. [Google Scholar]
- Coe R . It’s the effect size, stupid: what effect size is and why it is important. Presented at the Annual Conference of the British Educational Research Association, University of Exeter, England, 12–14 September 2002. URL: http://www.leeds.ac.uk/educol/
- Superio-Cabuslay E, Ward MM, Lorig KR. Patient education interventions in osteoarthritis and rheumatoid arthritis: a meta-analytic comparison with nonsteroidal anti-inflammatory drug treatment. Rheumatology (Oxford) 1996;9:292–301. doi: 10.1002/1529-0131(199608)9:4<292::aid-anr1790090414>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- Riesma RP, Taal E, Kirwan JR, Rasker JJ. Systematic review of rheumatoid arthritis patient education. Arthritis Rheum. 2004;51:1045–59. doi: 10.1002/art.20823. [DOI] [PubMed] [Google Scholar]
- Buchbinder R, Batterham R, Ciciriello S, Newman S, Horgan B, Ueffing E, et al. Health literacy: what is it and why is it important to measure? J Rheumatol. 2011;38:1791–7. doi: 10.3899/jrheum.110406. [DOI] [PubMed] [Google Scholar]
- Jordan JE, Osborne RH, Buchbinder R. Critical appraisal of health literacy indices revealed variable underlying constructs, narrow content and psychometric weakness. J Clin Epidemiol. 2011;64:366–79. doi: 10.1016/j.jclinepi.2010.04.005. [DOI] [PubMed] [Google Scholar]
- Bauer C, Ostrove N. Testing rules of thumb and the science of health literacy. Ann Intern Med. 2011;155:129–30. doi: 10.7326/0003-4819-155-2-201107190-00010. [editorial]. [DOI] [PubMed] [Google Scholar]
- White M, Adams J, Heywood P. How and why do interventions that increase health overall widen inequalities within populations? In: Babones SJ, editor. Social inequality and public health. Bristol: Policy Press; 2009. pp. 65–81. In: editor. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Appendix A
Supplementary Appendix B
Supplementary Appendix C
Supplementary Appendix D


