Abstract
BACKGROUND
Thrombocytopenia in patients with myelodysplastic syndrome (MDS) is associated with shortened survival and an increased risk of evolution to acute myeloid leukemia (AML). In this study, the authors evaluated the efficacy of romiplostim in patients who had thrombocytopenia with low-risk/intermediate-1–risk MDS.
METHODS
Patients who had thrombocytopenia with low-risk/intermediate-1–risk MDS (N = 250) were randomized 2:1 to receive romiplostim or placebo weekly for 58 weeks.
RESULTS
The primary endpoint— the number of clinically significant bleeding events (CSBEs) per patient—had a hazard ratio for romiplostim:placebo of 0.83 (95% confidence interval, 0.66-1.05; P = .13). CSBEs were reduced significantly in the romiplostim group for patients who had baseline platelet counts ≥20 × 109/L (P < .0001). For patients who had baseline platelet counts <20 × 109/L, there was no difference in the number of CSBEs, but the platelet transfusion rates were higher in the placebo group (P < .0001), which may have affected the overall CSBE results in this group with severe thrombocytopenia. The incidence of bleeding events was reduced significantly in the romiplostim group (relative risk, 0.92), as were protocol-defined platelet transfusions (relative risk, 0.77). Platelet response rates according to 2006 International Working Group criteria were higher for the group that received romiplostim (odds ratio, 15.6). On the basis of interim data, an independent data monitoring committee advised halting study drug because of concerns regarding excess blasts and AML rates with romiplostim (interim hazard ratio, 2.51). At 58 weeks, the AML rates were 6% in the romiplostim group and 4.9% in the placebo group (hazard ratio, 1.20; 95% confidence interval, 0.38-3.84), and the overall survival rates were similar.
CONCLUSIONS
Romiplostim treatment in patients with low-risk/intermediate-1–risk MDS increased platelet counts and decreased the number of bleeding events and platelet transfusions. Although study drug was discontinued because of an initial concern of AML risk, survival and AML rates were similar with romiplostim and placebo.
Keywords: romiplostim, myelodysplastic syndromes, drug therapy, thrombocytopenia, randomized controlled trial
INTRODUCTION
Thrombocytopenia, which is identified in approximately 50% of patients with low-risk/intermediate-1–risk myelodysplastic syndrome (MDS), is associated with shortened survival and an increased risk of evolution to acute myeloid leukemia (AML), which is part of the natural progression of MDS.1–5 In conjunction with abnormal platelet function, thrombocytopenia contributes to an increased risk of bleeding.6,7 Disease-modifying therapies, such as hypomethylating agents, can worsen thrombocytopenia and are not necessarily effective. Thus, platelet transfusions are the only treatment for thrombocytopenia in MDS.
Romiplostim (Nplate; Amgen, Inc., Thousand Oaks, Calif) is a peptibody approved for use in chronic immune thrombocytopenia.8,9 Results from trials in patients with lower risk MDS suggest that romiplostim, both as monotherapy and in combination with azacitidine, decitabine, or lenalidomide, improves thrombocytopenia in patients with MDS.10–15 Here, we describe the results of a 58-week, placebo-controlled study of romiplostim monotherapy in thrombocytopenic patients with low-risk/intermediate-1–risk MDS.
MATERIALS AND METHODS
Study Design and Patients
This phase 2, multicenter, randomized, double-blind study consisted of a 26-week placebo-controlled treatment period, a 4-week interim washout, followed by a bone marrow biopsy, a 24-week extended treatment period as randomized, and another 4-week washout, again followed by a bone marrow biopsy (Fig. 1), followed by an ongoing, 5-year survival long-term follow-up (LTFU) period (ClinicalTrials.gov identifier NCT00614523).
Figure 1.
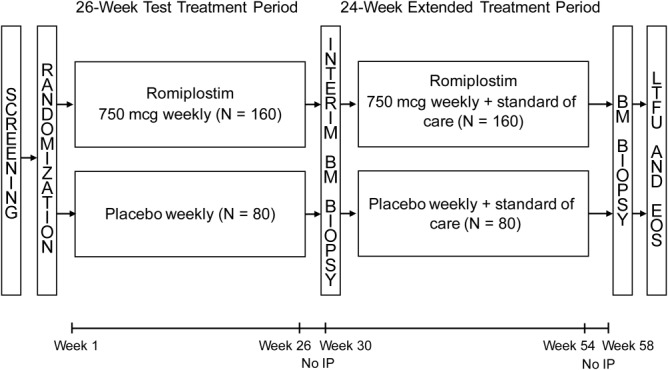
The study design is illustrated. BM indicates bone marrow; EOS, end of study; IP, investigational product; LTFU, long-term follow-up.
Eligible patients were adults diagnosed with MDS according to 2001 World Health Organization (WHO) criteria who had an International Prognostic Scoring System (IPSS) classification of low risk or intermediate-1 risk and platelet counts of <20 × 109/L or ≥20 × 109/L with a history of bleeding, as determined by the investigator. Patients underwent a bone marrow biopsy and aspirate within 3 months of starting the study. Exclusion criteria included receiving any MDS disease-modifying treatments or hematopoietic growth factors within 4 weeks of the study's start.
The study protocol and related documents were approved by study center institutional review boards. This study was conducted in accordance with US Food and Drug Administration and International Conference on Harmonization Good Clinical Practice regulations/guidelines. All patients provided written informed consent.
Procedures
Patients were randomized 2:1 to receive weekly subcutaneous romiplostim, starting at a dose of 750 μg, or volume-matched placebo. Randomization was facilitated through the interactive voice response system (IVRS) and was stratified by baseline platelet count (≥20 × 109/L or <20 × 109/L) and IPSS rating (low or intermediate-1). The romiplostim dose could be adjusted in 250-μg increments (from 250 μg every other week to 1000 μg weekly) or volume-matched placebo on the basis of platelet counts. Doses were withheld when the platelet count was >450 × 109/L and were reinitiated at a reduced dose when the platelet count was <200 × 109/L; if patients were receiving 250 μg, then the dose was reinitiated every other week. If the platelet count was <50 × 109/L for the first 3 consecutive weeks, then the dose was increased to 1000 μg on the fourth week. Patients who had their dose reduced could increase to the next highest dose if their platelet count was <50 × 109/L for 3 consecutive weeks.
Supportive care, defined as not including treatments that affected platelet production, aggregation, activation, granulocyte-macrophage–colony-stimulating factors, or any other investigational agents, was allowed throughout the study. In the extended treatment period only, patients could receive any standard-of-care MDS treatments. After completion of the 58-week study period or early discontinuation of study drug, patients entered LTFU.
The primary endpoint was clinically significant bleeding events (CSBEs) (grade ≥2 on the modified WHO bleeding scale16,17). Bleeding for >7 days was counted as a separate event every eighth day. Multiple events from the same organ system on the same day were collapsed into 1 event. Simultaneous bleeding events from unique organ systems were counted as individual events. Protocol-defined platelet transfusion events (PTEs) (ie, platelet transfusions for a bleeding event or platelets ≤10 × 109/L), overall bleeding, and platelet response according to 2006 International Working Group Hematologic Improvement-Platelet (HI-P)18 criteria also were assessed. Overall survival, MDS progression to AML, adverse events, and antibodies to romiplostim or thrombopoietin were assessed during the 58-week study period, which included the time in follow-up for patients who discontinued study drug early.
Romiplostim can be associated with transient blast cell count elevations in the absence of progression to AML. The study-defined criteria for progression to AML included: 1) confirmation of bone marrow or peripheral blast cells ≥20%19,20 at least 4 weeks after the last dose of study drug and at least 2 weeks after the last dose of hematopoietic growth factors; 2) a pathology report confirming extramedullary AML; or 3) initiation of treatment for AML, as designated by the investigator. An independent safety data monitoring committee (DMC) of 3 experts external to Amgen oversaw patient safety and met semiannually to review safety data generated by an independent statistics group.
Statistical Analysis
A sample size of 240 was planned for this study. The estimated event rate of CSBE was predicted to be 0.053 events per patient per week for the placebo group and 0.035 events per patient per week for the romiplostim group in the 26-week treatment period. The sample size was predicted to provide approximately 83% power to detect a difference in the total number of CSBEs between groups at a significance level of .05 (2-sided).
The primary endpoint of total number of CSBEs during the 26-week treatment period was analyzed using the Andersen-Gill model.8 A Poisson regression model was used both for secondary analysis and to calculate the difference between the rates of PTEs and overall bleeding in each group. We summarized time-to-event endpoints using Kaplan-Meier estimates21 and survival curves according to treatment group at 58 weeks. Hazard ratios (HRs) with 2-sided 95% confidence intervals (CIs) were calculated using a Cox proportional-hazards model22 stratified by randomization strata. We summarized the incidence of study-defined progression to AML at 58 weeks. Patient status information was updated with disease progression information obtained from LTFU. Disease progression, as assessed by increases in bone marrow blasts, was summarized as an exploratory analysis. For overall duration of bleeding, the relative risk (RR) was calculated from a Poisson regression model with treatment and stratification factors as covariates. Common odds ratios (ORs), adjusted for stratification factors, were calculated for HI-P. All patients who were randomized and received at least 1 dose of investigational product were included in the analysis. An unblinded interim analysis to review safety and efficacy data occurred when all enrolled individuals had completed the test treatment and interim washout period (week 30) or had terminated the study early. The final unblinding and analyses were performed at Amgen Inc.
RESULTS
Baseline Characteristics
In total, 250 patients were enrolled (romiplostim, n = 167; placebo, n = 83) at 109 sites in the United States, Canada, and Europe. The treatment groups were similar with respect to baseline characteristics, except that the romiplostim group included proportionally more patients with refractory anemia with excess blasts 1 (RAEB-1) (14% vs 11%) and fewer with unclassified MDS (MDS-U) (10% vs 15%) (Table1).
Table 1.
Baseline Demographics and Characteristicsa
| No. of Patients (%) | |||
|---|---|---|---|
| Variable | Placebo, N = 83 | Romiplostim, N = 167 | Total, N = 250 |
| Men | 53 (63.9) | 95 (56.9) | 148 (59.2) |
| Caucasians | 79 (95.2) | 156 (93.4) | 235 (94.0) |
| Age: Median [Q1, Q3], y | 69.0 [61.0, 76.0] | 71.0 [62.0, 77.0] | 70.0 [61.0, 77.0] |
| Platelets: Median [Q1, Q3], ×109/L | 17.7 [11.0, 28.7] | 19.7 [13.3, 31.3] | 19.3 [12.5, 30.3] |
| MDS duration: Median [Q1, Q3], y | 0.58 [0.16, 1.86] | 0.39 [0.13, 1.74] | 0.44 [0.13, 1.74] |
| MDS WHO classification at baselineb | |||
| RA | 5 (6) | 6 (3.6) | 11 (4.4) |
| RARS | 0 (0) | 2 (1.2) | 2 (0.8) |
| RAEB-1 | 9 (10.8) | 24 (14.4) | 33 (13.2) |
| RAEB-2 | 0 (0) | 1 (0.6) | 1 (0.4) |
| RCMD | 55 (66.3) | 114 (68.3) | 169 (67.6) |
| RCMD-RS | 2 (2.4) | 4 (2.4) | 6 (2.4) |
| MDS-U | 12 (14.5) | 16 (9.6) | 28 (11.2) |
| Del 5q | 0 (0) | 0 (0) | 0 (0) |
| IPSS status | |||
| Low: Total score of 0 | 23 (27.7) | 40 (24) | 63 (25.2) |
| Intermediate-1: Total score of 0.5 or 1 | 58 (70) | 120 (71.9) | 178 (71.2) |
| Intermediate-2: Total score of 1.5c | 0 (0) | 1 (0.6) | 1 (0.4) |
| Missing | 2 (2.4) | 6 (3.6) | 8 (3.2) |
| IPSS cytopenias | |||
| 1 | 31 (37.3) | 63 (37.7) | 94 (37.6) |
| 2 | 32 (38.6) | 61 (36.5) | 93 (37.2) |
| 3 | 20 (24.1) | 43 (25.7) | 63 (25.2) |
| IPSS cytogenetics | |||
| Good | 63 (75.9) | 131 (78.4) | 194 (77.6) |
| Intermediate | 18 (21.7) | 26 (15.6) | 44 (17.6) |
| Poor | 0 (0) | 4 (2.4) | 4 (1.6) |
| Unknown | 1 (1.2) | 5 (3) | 6 (2.4) |
| Missing | 1 (1.2) | 1 (0.6) | 2 (0.8) |
| Bone marrow myeloblasts, % | |||
| <5 | 74 (89.2) | 143 (85.6) | 217 (86.8) |
| 5-10 | 9 (10.8) | 24 (14.4) | 33 (13.2) |
| Prior MDS therapy | |||
| No | 70 (84.3) | 133 (79.6) | 203 (81.2) |
| Yes | 13 (15.7) | 34 (20.4) | 47 (18.8) |
Abbreviations: Del 5q, myelodysplastic syndrome associated with isolated 5q deletion; IPSS, International Prognostic Scoring System; MDS, myelodysplastic syndrome; MDS-U, myelodysplastic syndrome, unclassified; Q1, Q3, interquartile range; RA, refractory anemia; RAEB-1, refractory anemia with excess blasts-1; RAEB-2, refractory anemia with excess blasts-2; RARS, refractory anemia with ringed sideroblasts; RCMD, refractory cytopenia with multilineage dysplasia; RCMD-RS, refractory cytopenia with multilineage dysplasia and ringed sideroblasts; WHO, World Health Organization.
Unless stated otherwise, data shown are the number of patients (%).
Diagnoses were according to 2001 WHO criteria.
The enrollment of 1 patient who had an IPSS score of 1.5 was a protocol deviation.
Disposition
In February 2011, based on interim data as of October 2010 from 219 patients, the DMC recommended that all patients discontinue study treatment. The DMC was concerned that transient increases in peripheral blast cell counts associated with romiplostim put patients at risk for diagnosis of and treatment for AML and that the potential benefit of a reduction in bleeding did not outweigh that risk. All patients discontinued treatment by February 24, 2011, but remained on study for follow-up. All patients had received at least 1 dose of investigational product. Seventy patients (41.9%) who received romiplostim and 39 patients (47%) who received placebo completed the 26-week test treatment period and started the extended treatment period. Because of the DMC recommendation, 69 patients (27.6%) discontinued study drug early, including 41 in the test treatment period and 28 in the extended treatment period (Fig. 2). Only 56 patients (36 patients in the romiplostim group and 20 patients in the placebo group) completed the 58-week study (Fig. 2).
Figure 2.
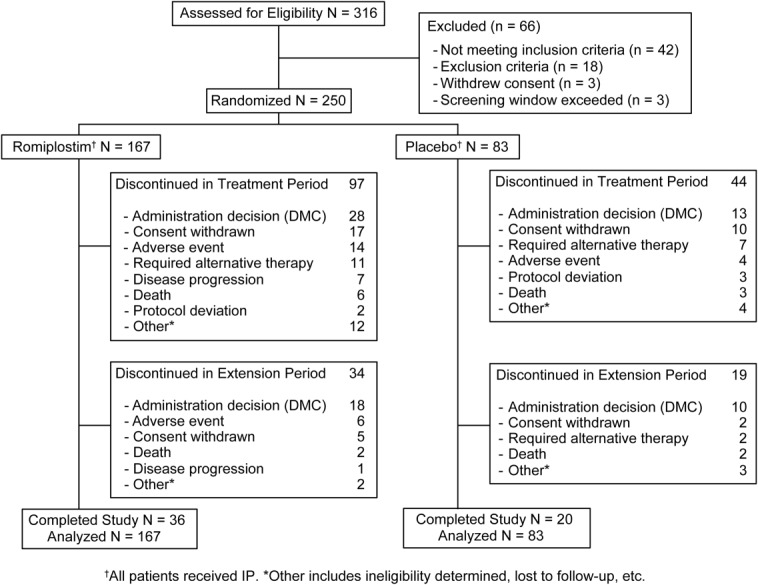
Patient disposition is illustrated. DMC indicates data monitoring committee; IP, investigational product.
Efficacy in the 26-Week Test Treatment Period: Bleeding and Platelet Transfusions
During the 26-week treatment period, the mean incidence of CSBEs per patient was less with romiplostim (1.47) than with placebo (1.94; P = .13) (Table2; Supporting Fig. 1 [see online supporting information]). The number of CSBEs was lower with romiplostim in patients who had baseline low-risk MDS (HR, 0.48; 95% CI, 0.29-0.79) or a platelet count ≥20 × 109/L (HR, 0.34; 95% CI, 0.20-0.58) (Supporting Fig. 2; see online supporting information). The number of all bleeding events was lower with romiplostim (RR, 0.922; 95% CI, 0.86-0.99), as was the overall duration (in days) of all bleeding events (RR, 0.906; 95% CI, 0.87-0.94).
Table 2.
Clinical Outcomes: Bleeding Events and Platelet Transfusions in the 26-Week Test Treatment Period
| Treatment Differencea | ||||
|---|---|---|---|---|
| Variableb | Placebo | Romiplostim | Ratio (95% CI) | P |
| All patientsc | ||||
| CSBE: Mean no. of events per patient at week 26 | 1.94 | 1.47 | HR, 0.83 (0.66-1.05) | .13 |
| All bleeding events per 100 pt-yrs | 3786.4 | 3459.9 | RR, 0.922 (0.86-0.99) | .026 |
| No. of CTCAE grade ≥3 bleeding events per 100 pt-yrs | 133.9 | 101.5 | RR, 0.780 (0.53-1.16) | |
| No. of CTCAE grade 4 bleeding events: Life-threatening | 1/83 | 2/167 | ||
| No. of CTCAE grade 5 bleeding events: Fatal | 3/83 | 0/167 | ||
| Protocol-defined platelet transfusions rate per 100 pt-yrs | 1013.5 | 748.9 | RR, 0.766 (0.66-0.88) | < .001 |
| Total no. of platelet transfusions per 100 pt-yrs | 1195.2 | 983.6 | RR, 0.849 (0.75-0.97) | .013 |
| Total no. of platelet transfusion units per 100 pt-yrs | 3120.2 | 2221.8 | RR, 0.739 (0.68-0.80) | < .001 |
| Baseline platelets <20 × 109/Ld | ||||
| CSBE rate per 100 pt-yrs | 501.2 | 514.9 | RR, 1.03 (0.79-1.35) | |
| No. of platelet transfusions per 100 pt-yrs | 1778.6 | 1250.5 | RR, 0.71 (0.61-0.82) | < .0001 |
| Baseline platelets ≥20 × 109/Le | ||||
| CSBE rate per 100 pt-yrs | 226.4 | 79.5 | RR, 0.35 (0.21-0.59) | < .0001 |
| Platelet transfusion rate per /100 pt-yrs | 179.8 | 251.8 | RR, 1.38 (0.89-2.15) | |
Abbreviations: CI, confidence interval; CSBE, clinically significant bleeding events; CTCAE, Common Terminology Criteria for Adverse Events; HR, hazard ratio; pt-yrs, patient-years; RR, relative risk (used as the Poisson regression model was applied because of the low event incidence).
In addition to treatment effect, the covariates included stratification factors (baseline platelet count and IPSS status).
Data indicate the difference in treatment between romiplostim and versus placebo.
Placebo, n = 83; romiplostim, n = 167.
Placebo, n = 43; romiplostim, n = 87.
Placebo, n = 40; romiplostim, n = 80.
Annualized rates of protocol-defined PTEs, total transfusions, and total platelet transfusion unit use were lower with romiplostim (Table2). The proportions of therapeutic transfusions (romiplostim, 44.5%; placebo, 49.6%) and prophylactic transfusion (romiplostim, 47.2%; placebo, 45.9%) were similar. An examination of bleeding and transfusion events by baseline platelet count indicated that, for patients who had baseline platelet counts ≥20 × 109/L, there were nearly 3-fold fewer CSBEs with romiplostim, without a notable change in the incidence of PTEs (Table2). For patients who had baseline platelet counts <20 × 109/L, the CSBE rate was not different with romiplostim; however, placebo-treated patients had significantly more PTEs (RR, 0.71 for romiplostim-treated patients; 95% CI, 0.61-0.82).
After week 4, median platelet counts were consistently higher with romiplostim (P < .001) (Fig. 3A). Of the patients who were evaluable for HI-P (platelet response), a greater proportion of those receiving romiplostim had an HI-P (61 of 167 patients [36.5%] in the romiplostim group vs 3 of 83 patients [3.6%] in the placebo group). Thirty-seven patients (29 in the romiplostim group and 8 in the placebo group) discontinued treatment before receiving 8 weeks of study drug and, thus, could not be assessed for HI-P. The common OR, which was calculated with all patients included, was 15.6 (95% CI, 4.7-51.8; P < .001). HI-P was increased with romiplostim relative to placebo. Among 64 patients with HI-P (61 in the romiplostim group, 3 in the placebo group), 8 patients (12.5%) had a CSBE, 42 (65.6%) had any bleeding, 14 (21.9%) had a PTE, and 16 (25%) had any platelet transfusion. The proportions of patients who had a platelet response at any point in time quickly diverged for the romiplostim and placebo groups (Supporting Fig. 3; see online supporting information).
Figure 3.
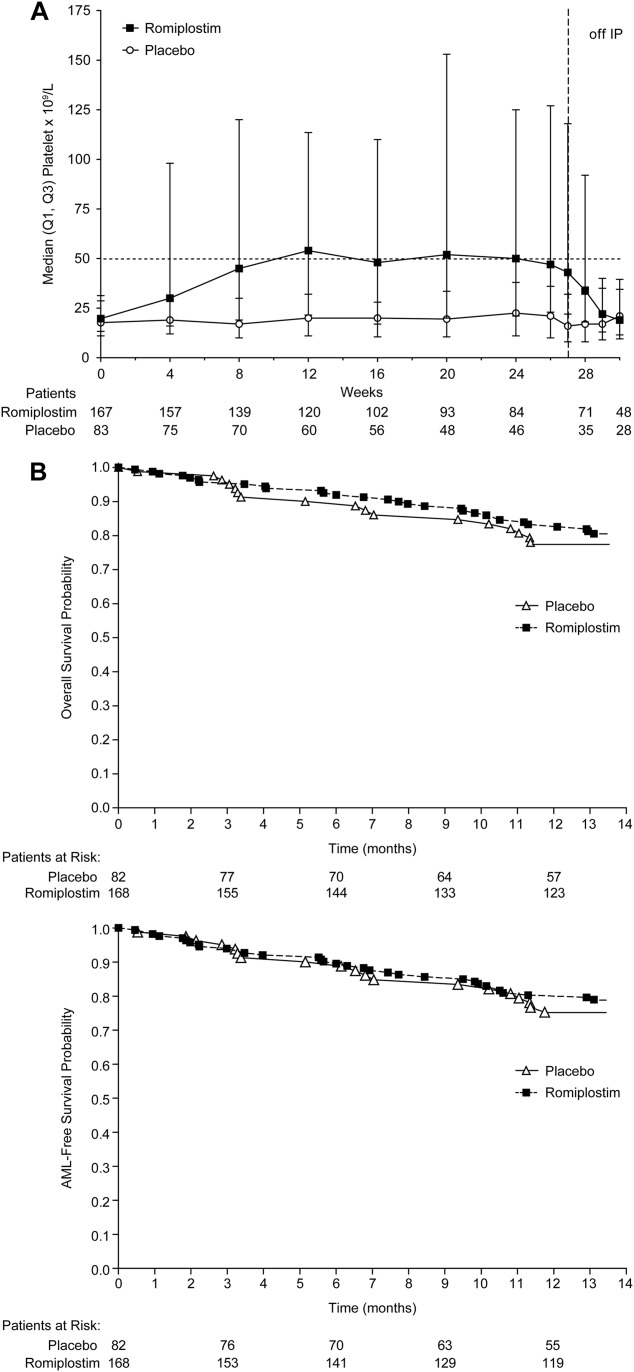
(A) Platelet counts and (B) overall and acute myeloid leukemia-free survival over time are illustrated. IP indicates investigational product; Q1, Q3, interquartile range.
Survival and AML
Similar proportions of patients died on both arms within the 58-week study period, including 18% of patients in the romiplostim and 20.5% of patients in the placebo group (overall survival: HR, 0.86; 95% CI, 0.48-1.56) (Fig. 3B). There was no significant difference in disease progression to AML between treatment groups. Study-defined criteria for progression to AML were met during the 58-week period by 10 (6%) romiplostim-treated patients and by 4 (4.9%) placebo-treated patients (HR, 1.20; 95% CI, 0.38-3.84) (Table3; Supporting Table 1 [see online supporting information]). At the time of the interim data cut upon which the DMC based its recommendation to discontinue study drug, AML was reported in 10 patients who had received romiplostim (6%) and in 2 patients who had received placebo (2.4%; HR, 2.51; 95% CI, 0.55-11.47). AML-free survival rates for the final data were 19.8% (33 patients) for the romiplostim group and 22.9% (19 patients) for the placebo group (HR, 0.86; 95% CI, 0.49-1.51). Of 14 patients who had AML, 9 were patients whose baseline WHO classification was RAEB-1/RAEB-2, and 5 fulfilled criteria for AML by investigator choice to initiate chemotherapy for AML. Patients with RAEB-1/RAEB-2 (14% of the study population) were more likely to progress to AML and comprised 64% of AML cases. MDS disease-modifying therapies were received by 3 patients in the romiplostim group (1.8%) and by 4 patients in the placebo group (4.8%).
Table 3.
Progression to Acute Myeloid Leukemia
| No. of Patients (%) | |||
|---|---|---|---|
| Variable | Placebo, N = 82 | Romiplostim, N = 168 | Total, N = 250 |
| Total no. with study-defined AML | 4 | 10 | 14 |
| Baseline WHO classification | |||
| RAEB-1 or RAEB-2 | 3 (75) | 6 (60) | 9 (64) |
| Non-RAEB | 1 (25) | 4 (40) | 5 (36) |
| AML diagnosis by | |||
| Bone marrow/peripheral blasts ≥20% | 2 (50) | 7 (70)a | 9 (64) |
| Anti-AML therapy alone | 2 (50) | 3 (30) | 5 (36) |
Abbreviations: AML, acute myeloid leukemia; RAEB-1, refractory anemia with excess blasts-1; RAEB-2, refractory anemia with excess blasts-2; WHO, World Health Organization.
In 2 patients, a diagnosis of AML was made after study drug was discontinued for 2 weeks (according to an earlier version of the protocol).
Safety
During the 58-week study period, adverse events were reported for 157 patients (93.5%) who were receiving romiplostim and 76 patients (92.7%) who were receiving placebo. Similar incidences were reported during the 26-week treatment period. Overall, 67 patients (39.9%) who were receiving romiplostim and 22 patients (26.8%) who were receiving placebo had serious adverse events (95% CI, 32.4%-47.7% and 17.6%-37.8%, respectively). Serious adverse events that were considered related to romiplostim were reported for 12 patients (7.1%), including increased myeloblast count, colon cancer, deep vein thrombosis, extramedullary hemopoiesis, leukocytosis, myelofibrosis, pneumonia, pyrexia, splenic infarction, transient ischemic attack, and type 2 diabetes mellitus. The most frequently reported adverse events in both study arms were epistaxis, hematoma, and petechiae (Supporting Table 2; see online supporting information). One romiplostim-treated patient who had disease progression had serious grade 3 bone marrow fibrosis reported on day 35 of romiplostim treatment that had a reasonable possibility of being related to romiplostim. A second patient who had a history of myelofibrosis and had disease progression had grade 2 bone marrow fibrosis noted on day 71 and grade 3 bone marrow fibrosis noted on day 99 of treatment, although neither event was considered related to treatment. No patients were positive for neutralizing antibodies to romiplostim or thrombopoietin.
Elevations in peripheral blast cell counts to >10% occurred in 25 (14.9%) romiplostim-treated patients and 3 (3.7%) placebo-treated patients (95% CI, 9.9%-21.2% and 0.8%-10.3%, respectively). Twenty-four of those patients (85.7%) also had immature white blood cell forms in the peripheral blood. In 14 of 16 romiplostim-treated patients with available follow-up data, blasts decreased after romiplostim discontinuation. The remaining 2 romiplostim-treated patients had persistent blast cell count elevations. Of note, 11 of 14 patients (78.6%) who met the study-defined criteria for AML had an increase in immature white blood cell forms at any time postbaseline, compared with 39% of those who did not develop AML.
DISCUSSION
This study of thrombocytopenic patients with low-risk/intermediate-1–risk MDS demonstrated that romiplostim monotherapy increased platelet counts, decreased platelet transfusions, and decreased overall bleeding. The treatment groups did not differ with respect to the primary endpoint: CSBE. There was no demonstrated effect on survival. The overall incidences of adverse events were similar, although there were more serious adverse events with romiplostim (nonsignificant). Because the DMC recommended early discontinuation of the study drug based on interim data, thereby decreasing the study's statistical power, additional study conclusions are limited. However, platelet count increases and the incidence of platelet response were greater in romiplostim-treated patients. Romiplostim decreased overall bleeding events (P = .026) and CSBEs in patients who had baseline platelet counts ≥20 × 109/L (P < .0001).
The CSBE endpoint is confounded by the significantly greater rate of platelet transfusions received in the placebo group. In patients with baseline platelet counts <20 × 109/L, no difference in CSBEs between treatment groups was observed. However, the percentage of patients with PTEs was significantly lower in the romiplostim group overall (P < .001), particularly among patients with baseline platelet counts <20 × 109/L. It is likely that PTEs in patients with baseline platelet counts <20 × 109/L reduced bleeding events, which may account for the overall lack of difference in CSBEs between the placebo and romiplostim groups.
A composite endpoint of bleeding and platelet transfusions, similar to that comprising both bleeding and rescue medication use developed for patients with immune thrombocytopenia,23,24 might aid in the evaluation of romiplostim in MDS. Additional trials evaluating additional patient populations with endpoints that account for platelet transfusions and bleeding may be worthwhile.
Although the study drug was discontinued because of concern about blast increases and progression to AML with romiplostim, the rates of overall survival and progression to AML-free survival were similar between study arms. However, the study was not designed or powered to evaluate AML risk and was truncated early. Two romiplostim-treated patients who had increases in peripheral blast cell counts initiated treatment for AML without undergoing bone marrow biopsies 4 weeks after discontinuing romiplostim. Such patients were counted as having progressed to AML, which could affect interpretation of the results. In both arms of the study, patients with RAEB-1/RAEB-2 were disproportionately represented among those who developed AML. Romiplostim may stimulate megakaryocytes and other hematopoietic cells,25–27 which may account for the increases in blast cell counts observed more frequently with romiplostim and which often decreased after romiplostim discontinuation. Additional analysis revealed that, in most of these patients, romiplostim induced an increase in immature white blood cell forms and peripheral blood blasts, which could have led to an incorrect diagnosis of and treatment for AML.
One limitation of this study is the early discontinuation of study drug, which led to a smaller data set. This reduced power may have contributed to not meeting the primary endpoint: CSBE. Second, CSBE may have been confounded by platelet transfusions for which there were no set guidelines. Third, standard-of-care MDS treatments were allowed in the extended treatment period and during LTFU. The study was not designed to analyze the impact of those therapies, so their effects on outcomes were not evaluated. Finally, the broad criteria for diagnosing AML, some of which did not require bone marrow evaluation, along with data on transient blast increases, may account in part for the relatively high rate of AML observed in this low-risk population.28 Because this represented a homogeneous population of relatively healthy patients with lower risk MDS, generalization is limited.
Although the data set was affected by the early discontinuation of study drug, the available data indicate that romiplostim monotherapy increased platelet counts and decreased platelet transfusions and all bleeding except CSBEs in thrombocytopenic patients with low-risk/intermediate-1–risk MDS. The rates of AML and survival were similar between study arms. Additional data will be evaluated as LTFU continues, including the effects of romiplostim on the risk of disease progression to AML.
FUNDING SUPPORT
This study was funded by Amgen Inc. Medical writing assistance, supported financially by Amgen, Inc., was provided by Susanna Mac of Amgen Inc.
CONFLICT OF INTEREST DISCLOSURES
Dr. Giagounidis has served on advisory boards and as a speaker for Amgen and GlaxoSmithKline. Dr. Mufti has served as a consultant for and received research funding from Celgene. Dr. Fenaux has received honoraria and research funding from Amgen, Celgene, Janssen Roche, GlaxoSmithKline, and Novartis. Dr. Sekeres has served on advisory boards for Amgen and Celgene. Dr. Szer has been on advisory boards and received honoraria from Amgen, Celgene, Novartis, and Alexion. Dr. Platzbecker has served as a consultant for Amgen, GlaxoSmithKline, Celgene, and Novartis. Dr. Kuendgen has received honoraria from Celgene. Dr. Gaidano has served on advisory boards for Amgen, Celgene, Roche, Onyx, GlaxoSmithKline, and Bristol Myers Squibb, and as a speaker for Amgen, Roche, and GlaxoSmithKline. Dr. Wiktor-Jedrzejczak has served as a consultant for Janssen-Cilag, Amgen, Novartis, Pfizer, and Bayer; on advisory boards for Bristol Myers Squibb; and as a speaker for Celgene, Genzyme, Novartis, Genopharm, and Bristol Myers Squibb. Drs. Hu and Yang are employees of and stockholders in Amgen. Dr. Woodard is a former employee of and stockholder in Amgen. Dr. Kantarjian has received research grants from Amgen.
Additional supporting information may be found in the online version of this article.
REFERENCES
- Garcia-Manero G, Shan J, Faderl S, et al. A prognostic score for patients with lower risk myelodysplastic syndrome. Leukemia. 2008;22:538–543. doi: 10.1038/sj.leu.2405070. [DOI] [PubMed] [Google Scholar]
- Gonzalez-Porras J, Cordoba I, Such E, et al. Prognostic impact of severe thrombocytopenia in low-risk myelodysplastic syndrome. Cancer. 2011;117:5529–5537. doi: 10.1002/cncr.26173. [DOI] [PubMed] [Google Scholar]
- Kantarjian H, Giles F, List A, et al. The incidence and impact of thrombocytopenia in myelodysplastic syndromes. Cancer. 2007;109:1705–1714. doi: 10.1002/cncr.22602. [DOI] [PubMed] [Google Scholar]
- Kantarjian H, O'Brien S, Ravandi F, et al. Proposal for a new risk model in myelodysplastic syndrome that accounts for events not considered in the original International Prognostic Scoring System. Cancer. 2008;113:1351–1361. doi: 10.1002/cncr.23697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sekeres MA, Schoonen WM, Kantarjian H, et al. Characteristics of US patients with myelodysplastic syndromes: results of 6 cross-sectional physician surveys. J Natl Cancer Inst. 2008;100:1542–1551. doi: 10.1093/jnci/djn349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manoharan A, Brighton T, Gemmell R, et al. Platelet dysfunction in myelodysplastic syndromes: a clinicopathological study. Int J Hematol. 2002;76:272–278. doi: 10.1007/BF02982798. [DOI] [PubMed] [Google Scholar]
- Mittelman M, Zeidman A. Platelet function in the myelodysplastic syndromes. Int J Hematol. 2000;71:95–98. [PubMed] [Google Scholar]
- Andersen PK, Gill RD. Cox's Regression model for counting processes: a large sample study. Ann Stat. 1982;10:1100–1120. [Google Scholar]
- Bussel JB, Kuter DJ, George JN, et al. AMG 531, a thrombopoiesis-stimulating protein, for chronic ITP. N Engl J Med. 2006;355:1672–1681. doi: 10.1056/NEJMoa054626. [DOI] [PubMed] [Google Scholar]
- Fenaux P, Kantarjian HM, Muus P, et al. Update of an open-label extension study evaluating the long-term safety and efficacy of romiplostim in thrombocytopenic patients with myelodysplastic syndromes (MDS) Blood (ASH Annual Meeting Abstracts) 2011;118 Abstract 2772. [Google Scholar]
- Greenberg PL, Garcia-Manero G, Moore M, et al. A randomized controlled trial of romiplostim in patients with low- or intermediate-risk myelodysplastic syndrome (MDS) receiving decitabine. Leuk Lymphoma. 2012;54:321–328. doi: 10.3109/10428194.2012.713477. [DOI] [PubMed] [Google Scholar]
- Kantarjian H, Fenaux P, Sekeres MA, et al. Phase 1/2 study of AMG 531 in thrombocytopenic patients (pts) with low-risk myelodysplastic syndrome (MDS): update including extended treatment [abstract] Blood (ASH Annual Meeting Abstracts) 2007;110 Abstract 250. [Google Scholar]
- Kantarjian H, Giles F, Fenaux P, et al. Evaluating safety and efficacy of AMG 531 for the treatment of thrombocytopenic patients with myelodysplastic syndrome (MDS): preliminary results of a phase 1/2 study [abstract] J Clin Oncol. 2007;25(18S) Abstract 7032. [Google Scholar]
- Wang ES, Lyons RM, Larson RA, et al. A randomized, double-blind, placebo-controlled phase 2 study evaluating the efficacy and safety of romiplostim treatment of patients with low or intermediate-1 risk myelodysplastic syndrome receiving lenalidomide [serial online] J Hematol Oncol. 2012;5:71. doi: 10.1186/1756-8722-5-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sekeres MA, Kantarjian H, Fenaux P, et al. Subcutaneous or intravenous administration of romiplostim in thrombocytopenic patients with lower risk myelodysplastic syndromes. Cancer. 2011;117:992–1000. doi: 10.1002/cncr.25545. [DOI] [PubMed] [Google Scholar]
- Heddle NM, Cook RJ, Webert KE, et al. Methodologic issues in the use of bleeding as an outcome in transfusion medicine studies. Transfusion. 2003;43:742–752. doi: 10.1046/j.1537-2995.2003.00418.x. [DOI] [PubMed] [Google Scholar]
- Rebulla P, Finazzi G, Marangoni F, et al. The threshold for prophylactic platelet transfusions in adults with acute myeloid leukemia.-Gruppo Italiano Malattie Ematologiche Maligne dell'Adulto. N Engl J Med. 1997;337:1870–1875. doi: 10.1056/NEJM199712253372602. [DOI] [PubMed] [Google Scholar]
- Cheson BD, Greenberg PL, Bennett JM, et al. Clinical application and proposal for modification of the International Working Group (IWG) response criteria in myelodysplasia. Blood. 2006;108:419–425. doi: 10.1182/blood-2005-10-4149. [DOI] [PubMed] [Google Scholar]
- Vardiman JW, Harris NL, Brunning RD. The World Health Organization (WHO) classification of the myeloid neoplasms. Blood. 2002;100:2292–2302. doi: 10.1182/blood-2002-04-1199. [DOI] [PubMed] [Google Scholar]
- Vardiman JW, Thiele J, Arber DA, et al. The 2008 revision of the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia: rationale and important changes. Blood. 2009;114:937–951. doi: 10.1182/blood-2009-03-209262. [DOI] [PubMed] [Google Scholar]
- Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. [Google Scholar]
- Cox DR. Regression models and life-tables. J R Stat Soc. 1972;34:187–220. [Google Scholar]
- Stasi R, Murali M, Michel M, et al. Evaluation of bleeding-related episodes in patients with immune thrombocytopenia (ITP) receiving romiplostim or medical standard of care. Int J Hematol. 2012;96:26–33. doi: 10.1007/s12185-012-1088-8. [DOI] [PubMed] [Google Scholar]
- Weitz I, Sanz MA, Henry D, et al. A novel approach to the evaluation of bleeding-related episodes in patients with chronic immune thrombocytopenia. Curr Med Res Opin. 2012;28:789–796. doi: 10.1185/03007995.2012.684046. [DOI] [PubMed] [Google Scholar]
- Harker LA, Marzec UM, Hunt P, et al. Dose-response effects of pegylated human megakaryocyte growth and development factor on platelet production and function in nonhuman primates. Blood. 1996;88:511–521. [PubMed] [Google Scholar]
- Harker LA, Hunt P, Marzec UM, et al. Regulation of platelet production and function by megakaryocyte growth and development factor in nonhuman primates. Blood. 1996;87:1833–1844. [PubMed] [Google Scholar]
- Ninos JM, Jefferies LC, Cogle CR, et al. The thrombopoietin receptor, c-Mpl, is a selective surface marker for human hematopoietic stem cells [abstract] J Transl Med. 2006;4:9. doi: 10.1186/1479-5876-4-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg P, Cox C, LeBeau MM, et al. International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood. 1997;89:2079–2088. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


