Abstract
Purpose
To identify sexual function improvement associated with alfuzosin (10 mg daily for 2 years).
Materials and Methods
We enrolled 30 men with lower urinary tract symptom (LUTS) who visited Gyeongsang National University Hospital between 2010 and 2012. At first visit, urinalysis, prostate specific antigen, transrectal ultrasound, and uroflowmetry were performed. The nternational Prostate Symptom Score (IPSS), quality of life (QoL), International Index of Erectile Function (IIEF), and Male Sexual Health Questionnaire Ejaculation Function Domain (MSHQ-EjFD) questionnaires were administered, and the subjects answered the same questionnaires at 1 month, 6 months, 1 year, and 2 years of follow-up.
Results
Twelve men completed of the entire study. After administration of alfuzosin, the median IPSS at first visit, 1 month, 6 months, 1 year, and 2 years was 18.00 (interquatile range [IQR]: 14.00~29.75), 20.00 (IQR: 11.50~30.00), 15.50 (IQR: 8.50~25.25), 14.50 (IQR: 9.25~19.50), and 11.50 (IQR: 5.00~17.75), respectively, which showed an improvement. The median QoL at the same times was 4.50 (IQR: 4.00~5.00), 4.50 (IQR: 4.00~5.00), 3.00 (IQR: 2.00~4.00), 3.50 (IQR: 2.25~4.00), and 3.00 (IQR: 1.00~3.00), respectively, and also showed improvement. Likewise, the median IIEF was 36.50 (IQR: 24.50~46.75), 37.50 (IQR: 26.75~47.25), 45.50 (IQR: 35.00~59.75), 48.50 (IQR: 34.75~62.75), and 47.50 (IQR: 43.25~61.00), while the median MSHQ-EjFD was 19.00 (IQR: 12.0~24.75), 19.50 (IQR: 13.50~27.75), 23.00 (IQR: 19.25~32.25), 26.50 (IQR: 18.25~34.50), 27.00 (IQR: 21.50~32.50), respectively, with both showing improvement.
Conclusions
After administration of alfuzosin (10 mg daily for 2 years), the IPSS, QoL, IIEF, and MSHQ-EjFD all improved significantly. This means long-term administration of 10 mg of alfuzosin daily would be effective not only for LUTS but also erectile function and ejaculation.
Keywords: Alfuzosin, Ejaculation, Penile erection
INTRODUCTION
With age, various physical changes such as lower urinary tract symptoms (LUTS), erectile dysfunction (ED), and a decrease in libido typically occur and cause trouble in daily life [1,2]. The prevalence of LUTS and ED commonly increases with increasing age, and the two diseases frequently coexist. Thus studies investigating a common pathophysiology of the two diseases have been actively conducted [3].
Recent studies have presented several hypotheses on the physiological explanation of the association of LUTS with ED, including the following possible causes: (i) the dysfunction of nitric oxide synthesis in endothelial cells in the corpus cavernosum; (ii) the contraction of smooth muscle in the corpus cavernosum by the increase of sympathicotonia and hyperactivation of the autonomic nervous system due to LUTS; (iii) the contraction of smooth muscle by phosphorylation of myosin light chain due to increase of Rho-kinase activity; and (iv) pelvic atherosclerosis [4].
Currently, the most effective primary treatment for LUTS caused by benign prostate hyperplasia (BPH) is to administer an α-blocker, which is generally noted for its safety and efficacy. However, the outcomes and site of action affecting sexual function appear differently depending on the type of α-blocker used [5,6]. The non-selective α-blockers such as alfuzosin, doxazosin, and terazosin are known to have produce greater improvements in sexual function than α1A-subtype superselective α-blockers [3]. However, to our knowledge, clinical data from long-term follow-up observation of alfuzosin application are not available. Thus, this study was conducted to determine the outcomes with regard to sexual function of continuous daily administration of 10 mg of alfuzosin for 2 years.
MATERIALS AND METHODS
This study enrolled 30 men with LUTS/BPH who visited Gyeongsang National University Hospital between 2010 and 2012. None of the patients had received α-blockers before the study commenced. This open-label, prospective, and non-comparative study was conducted at a single center. The study was approved by the institutional review board of Gyeongsang National University Hospital in Korea.
At the first visit, the following were assessed for all of the patients: urinalysis, prostate specific antigen (PSA), transrectal ultrasound, uroflowmetry, the International Prostate Symptom Score (IPSS), International Index of Erectile Function (IIEF), and Male Sexual Health Questionnaire Ejaculation Function Domain (MSHQ-EjFD). The following patients were included in this study: those who had 1) IPSS ≥8, 2) prostate volume ≥20, and 3) regular sexual intercourse at least once a month. The following patients were excluded from this study: those who 1) had undergone prostate surgery, 2) had sexual dysfunction (IIEF≤17), 3) had a neurologic abnormality, 4) had severe hepatic dysfunction, 5) had severe cardiovascular system abnormality, or 6) had been taking any drugs that could affect sexual function.
All enrolled patients were given an oral alfuzosin dose of 10 mg daily at the first visit, and the IPSS, quality of life (QoL), IIEF, and MSHQ-EjFD were conducted upon follow-up at 1 month, 6 months, 1 year, and 2 years after the initial alfuzosin administration.
Statistical analysis was performed with IBM SPSS Statistics for Windows software version 22.0 (IBM Co., Armonk, NY, USA). Variables were expressed as the median (interquartile range [IQR]) and compared using the Wilcoxon signed-rank test, and p<0.05 was considered statistically significant.
RESULTS
The median age was 56 years (IQR: 52.25~64.75 years) and the median prostate volume was 30 mL (IQR: 20.63~40.95 mL). The median PSA was 0.88 ng/mL (IQR: 0.46~2.56 ng/mL). At the first visit, 30 men were enrolled in this study, but 18 men had dropped out of the study due to incomplete data collection. Consequently, in the end, 12 men had completed the study. Their characteristics are presented in Table 1. No significant adverse events related to alfuzosin administration occurred.
Table 1.
Baseline characteristics of the patients
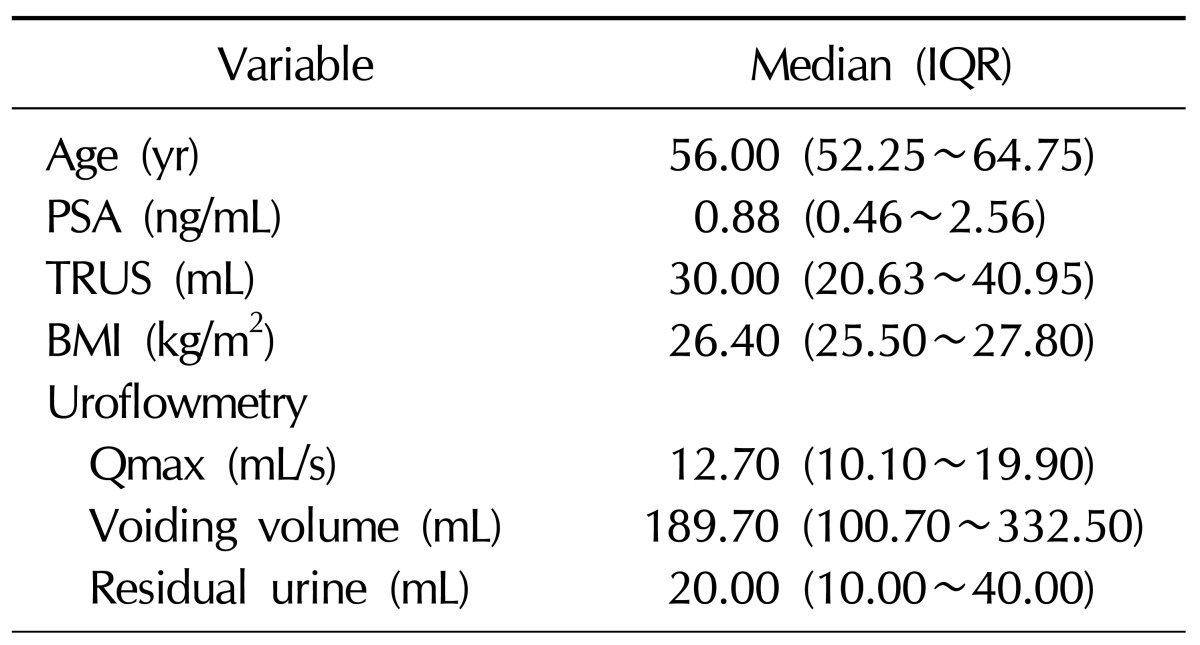
IQR: interquartile range, PSA: prostate specific antigen, TRUS: transrectal ultrasound, BMI: body mass index, Qmax: maximum urinary flow.
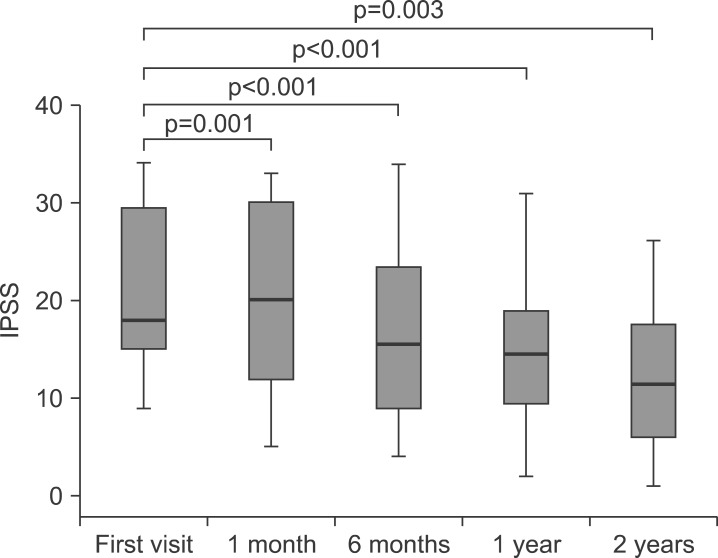
1. Changes in International Prostate Symptom Score and quality of life after treatment with 10 mg alfuzosin
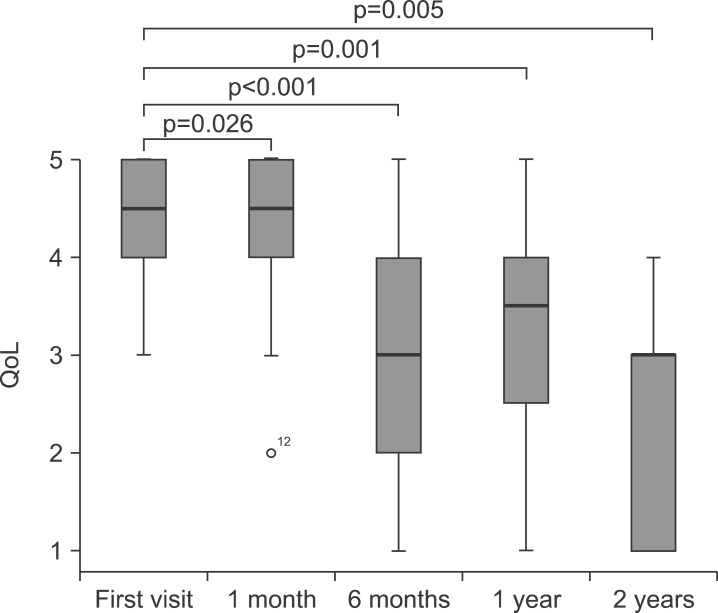
The results showed continuous improvement in the IPSS score during the period of treatment: at first visit, 18.00 (IQR: 14.00~29.75); 1 month later, 20.00 (IQR: 11.50~ 30.00); 6 months later, 15.50 (IQR: 8.50~25.25); 1 year later, 14.50 (IQR: 9.25~19.50); and 2 years later, 11.50 (IQR: 5.00~17.75) (Table 2, Fig. 1). The QoL also appeared to have been improved accordingly: at first visit, 4.50 (IQR: 4.00~5.00); 1 month later, 4.50 (IQR: 4.00~ 5.00); 6 months later, 3.00 (IQR: 2.00~4.00); 1 year later, 3.50 (IQR: 2.25~4.00); and 2 years later, 3.00 (IQR: 1.00-3.00) (Table 2, Fig. 2).
Table 2.
Changes in IPSS, QoL, IIEF, MSHQ-EjFD after treatment with alfuzosin 10 mg
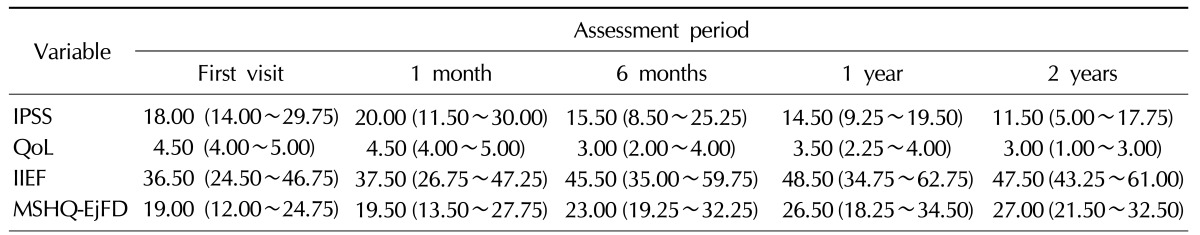
Values are presented as median (interquartile range).
IPSS: International Prostate Symptom Score, QoL: quality of life, IIEF: International Index of Erectile Function, MSHQ-EjFD: Male Sexual Health Questionnaire Ejaculation Function Domain.
Fig. 1.
Changes in the International Prostate Symptom Score (IPSS) after treatment with 10 mg alfuzosin. p value: compared with the first visit.
Fig. 2.
Changes in quality of life (QoL) after treatment with 10 mg alfuzosin. p value: compared with the first visit.
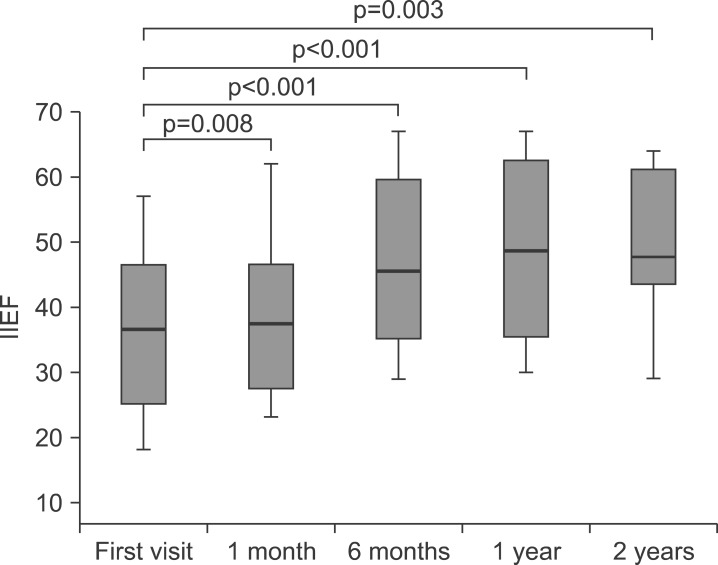
2. Changes in International Index of Erectile Function scores after treatment with 10 mg alfuzosin
Sexual function also showed a continuous improvement in the IIEF: first visit, 36.50 (IQR: 24.50~46.75); 1 month later, 37.50 (IQR: 26.75~47.25); 6 months later, 45.50 (IQR: 35.00~59.75); 1 year later, 48.50 (IQR: 34.75~62.75); and 2 years later, 47.50 (IQR: 43.25~ 61.00) (Table 2, Fig. 3).
Fig. 3.
Changes in the International Index of Erectile Function (IIEF) after treatment with 10 mg alfuzosin. p value: compared with the first visit.
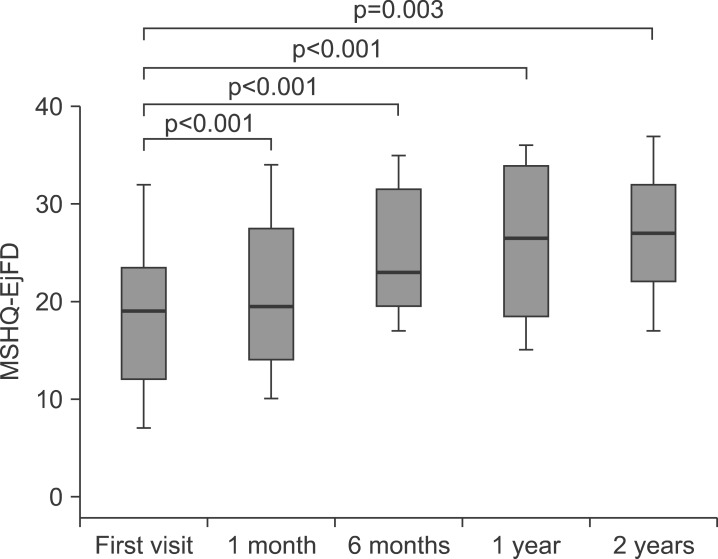
3. Changes in ale Sexual Health Questionnaire Ejaculation Function Domain scores after treatment with 10 mg alfuzosin
Ejaculation function, as measured by MSHQ-EjFD questionnaires, also showed a continuous improvement: first visit, 19.00 (IQR: 12.00~24.75); 1 month later, 19.50 (IQR: 13.50~27.75); 6 months later, 23.00 (IQR: 19.25~ 32.25); 1 year later, 26.50 (IQR: 18.25-34.50); and 2 years later, 27.00 (IQR: 21.50~32.50) (Table 2, Fig. 4).
Fig. 4.
Changes in the Male Sexual Health Questionnaire Ejaculation Function Domain (MSHQ-EjFD) after treatment with 10 mg alfuzosin. p value: compared with the first visit.
DISCUSSION
It was reported that among α-adrenoceptors in the prostate gland, the α1A receptors were mainly distributed in the interstitial cells and the α1B receptors were mainly distributed in the epithelial cells where the α1A-receptors played a major role in keeping the tension of smooth muscle in the prostate gland [7,8]. Three subtypes have been found to exist in the corpus cavernosum; the α1A-receptors are most abundant and the α1B-receptors are most scarce [9,10]. Therefore, studies on the α-blocker, which had been used to treat the BPH, have been actively conducted to determine its impacts on sexual function.
For an erection, the functioning of the central nervous system, peripheral nervous system, and vascular system are all essential. Some studies have reported that α-blockers can help an erection through central nervous system functioning or in the the peripheral vascular system to suppress the contraction of smooth muscle in the corpus cavernosum. The oral administration of phentolamine, the mixed α1/α2-antagonist, induced an improvement in erectile function [11], and it was also reported that the combination of the oral administration of doxazosin and alprostadil injection into the corpus cavernosum had a positive effect on the erection [12]. In this study, where the follow-up for the single administration of 10 mg alfuzosin had been conducted for 2 years also found significant continuous improvement in IIEF after 3 months from the start of the administration. However, another paper reported that the single administration of an α-blocker alone would not improve the erectile function; thus the impacts of the α-blocker upon the erection seem to require further investigation [13].
Recent studies have reported that the efficacy of an α1-blocker was commonly accepted to be effective regardless of the subtypes of the α1-blocker, but the adverse effects in the ejaculation showed many variations depending on the types of the α1-blocker. Wilt et al [14] reported that tamsulosin had a high affinity to the α1A-receptor, which has high adverse effects in ejaculation in overall sexual functioning, and Marks et al [15] reported that silodosin had a high affinity with the α1A-receptor and also had a large number of adverse effects related with the ejaculation function. On the other hand, another study reported that there was no difference in side effects related with the ejaculation between the groups administered non selective α1-blockers such as doxazocin or alfuzosin and the groups who took the placebos [5].
In this study, however, the long-term administration of alfuzosin appeared to have helped the improvement of ejaculatory function. The degree of ejaculatory disturbance of an α-blocker may be related with the amount of the dosage. Lee and Lee [16] found that neither ED nor ejaculatory dysfunction occurred after administering tamsulosin 0.2 mg, and Cho and Lee [17] reported adverse events of decreased sexual desire in 8.1%, ED in 6.6%, and ejaculatory dysfunction in 3.3% were observed. Such results are lower than the frequencies of tamsulosin-induced ejaculatory dysfunction reported in Western Europe, and the researchers interpreted this difference in ejaculatory disturbance frequencies between the East and the West might came from the differences in the amount of tamsulosin dosages.
In this study, the patients were followed-up for 2 years with questionnaires on the IPSS, IIEF, and MSHQ-EjFD by administering alfuzosin 10 mg every day to treat lower unary tract symptoms. The results showed a significant improvement in LUTS including the QoL, and the sexual functions including the premature ejaculation were also identified to have been improved.
However, there were some limitations in this study. Above all, the total number of subjective patients was not sufficient, and furthermore, the number of patients who participated in the study to the completion was also not enough. Finally, the study was conducted without control groups apply placebos, thus the proper assessment of impacts of the alfuzosin upon sexual functions would require further additional studies.
CONCLUSIONS
After the long term administration of alfuzosin 10 mg for 2 years, IPSS, QoL, IIEF and MSHQ-EjFD were all improved significantly. This results means that long-term administration of alfuzosin 10 mg daily would be effective not only on LUTS but also on the erectile and ejaculation functions.
References
- 1.Braun M, Wassmer G, Klotz T, Reifenrath B, Mathers M, Engelmann U. Epidemiology of erectile dysfunction: results of the 'Cologne Male Survey'. Int J Impot Res. 2000;12:305–311. doi: 10.1038/sj.ijir.3900622. [DOI] [PubMed] [Google Scholar]
- 2.Rosen R, Altwein J, Boyle P, Kirby RS, Lukacs B, Meuleman E, et al. Lower urinary tract symptoms and male sexual dysfunction: the multinational survey of the aging male (MSAM-7) Eur Urol. 2003;44:637–649. doi: 10.1016/j.eururo.2003.08.015. [DOI] [PubMed] [Google Scholar]
- 3.Rosen RC, Wei JT, Althof SE, Seftel AD, Miner M, Perelman MA. Association of sexual dysfunction with lower urinary tract symptoms of BPH and BPH medical therapies: results from the BPH Registry. BPH Registry and Patient Survey Steering Committee. Urology. 2009;73:562–566. doi: 10.1016/j.urology.2008.05.034. [DOI] [PubMed] [Google Scholar]
- 4.McVary KT. Sexual dysfunction in men with lower urinary tract symptoms and benign prostatic hyperplasia: an emerging link. BJU Int. 2003;91:770–771. doi: 10.1046/j.1464-410x.2003.04252.x. [DOI] [PubMed] [Google Scholar]
- 5.Roehrborn CG, Van Kerrebroeck P, Nordling J. Safety and efficacy of alfuzosin 10 mg once-daily in the treatment of lower urinary tract symptoms and clinical benign prostatic hyperplasia: a pooled analysis of three double-blind, placebo-controlled studies. BJU Int. 2003;92:257–261. doi: 10.1046/j.1464-410x.2003.04309.x. [DOI] [PubMed] [Google Scholar]
- 6.Lepor H. Phase III multicenter placebo-controlled study of tamsulosin in benign prostatic hyperplasia. Tamsulosin Investigator Group. Urology. 1998;51:892–900. doi: 10.1016/s0090-4295(98)00126-5. [DOI] [PubMed] [Google Scholar]
- 7.Kobayashi S, Tang R, Shapiro E, Lepor H. Characterization and localization of prostatic alpha 1 adrenoceptors using radioligand receptor binding on slide-mounted tissue section. J Urol. 1993;150:2002–2006. doi: 10.1016/s0022-5347(17)35954-2. [DOI] [PubMed] [Google Scholar]
- 8.Walden PD, Durkin MM, Lepor H, Wetzel JM, Gluchowski C, Gustafson EL. Localization of mRNA and receptor binding sites for the alpha 1a-adrenoceptor subtype in the rat, monkey and human urinary bladder and prostate. J Urol. 1997;157:1032–1038. [PubMed] [Google Scholar]
- 9.Dausse JP, Leriche A, Yablonsky F. Patterns of messenger RNA expression for alpha1-adrenoceptor subtypes in human corpus cavernosum. J Urol. 1998;160:597–600. [PubMed] [Google Scholar]
- 10.Goepel M, Krege S, Price DT, Michelotti GA, Schwinn DA, Michel MC. Characterization of alpha-adrenoceptor subtypes in the corpus cavernosum of patients undergoing sex change surgery. J Urol. 1999;162:1793–1799. [PubMed] [Google Scholar]
- 11.Becker AJ, Stief CG, Machtens S, Schultheiss D, Hartmann U, Truss MC, et al. Oral phentolamine as treatment for erectile dysfunction. J Urol. 1998;159:1214–1216. [PubMed] [Google Scholar]
- 12.Kaplan SA, Reis RB, Kohn IJ, Shabsigh R, Te AE. Combination therapy using oral alpha-blockers and intracavernosal injection in men with erectile dysfunction. Urology. 1998;52:739–743. doi: 10.1016/s0090-4295(98)00388-4. [DOI] [PubMed] [Google Scholar]
- 13.Gacci M, Vittori G, Tosi N, Siena G, Rossetti MA, Lapini A, et al. A randomized, placebo-controlled study to assess safety and efficacy of vardenafil 10 mg and tamsulosin 0.4 mg vs. tamsulosin 0.4 mg alone in the treatment of lower urinary tract symptoms secondary to benign prostatic hyperplasia. J Sex Med. 2012;9:1624–1633. doi: 10.1111/j.1743-6109.2012.02718.x. [DOI] [PubMed] [Google Scholar]
- 14.Wilt TJ, Mac Donald R, Rutks I. Tamsulosin for benign prostatic hyperplasia. Cochrane Database Syst Rev. 2003;(1):CD002081. doi: 10.1002/14651858.CD002081. [DOI] [PubMed] [Google Scholar]
- 15.Marks LS, Gittelman MC, Hill LA, Volinn W, Hoel G. Rapid efficacy of the highly selective alpha1A-adrenoceptor antagonist silodosin in men with signs and symptoms of benign prostatic hyperplasia: pooled results of 2 phase 3 studies. J Urol. 2009;181:2634–2640. doi: 10.1016/j.juro.2009.02.034. [DOI] [PubMed] [Google Scholar]
- 16.Lee E, Lee C. Clinical comparison of selective and non-selective alpha 1A-adrenoreceptor antagonists in benign prostatic hyperplasia: studies on tamsulosin in a fixed dose and terazosin in increasing doses. Br J Urol. 1997;80:606–611. doi: 10.1046/j.1464-410x.1997.00411.x. [DOI] [PubMed] [Google Scholar]
- 17.Cho SH, Lee SK. The experience with combination of finasteride and tamsulosin on benign prostatic hyperplasia. Korean J Urol. 2003;44:1110–1115. [Google Scholar]