Abstract
Purpose
To evaluate the characteristics of patients who received primary androgen deprivation therapy (PADT) for prostate cancer and the clinical efficacy of this treatment.
Materials and Methods
Two hundred forty patients treated by PADT were reviewed. These patients could not receive definitive therapy owing to old age, patient need, and medical comorbidity. The patients were divided into three groups according to the extent of prostate cancer: localized, locally advanced, and metastatic. Then, prostate-specific antigen (PSA) progression in these groups was analyzed.
Results
The median age of the patients was 73.0 years, and the median pretreatment PSA level was 47.0 ng/mL. Of the patients, 91.7% were treated with combined androgen blockade, and 8.3% were treated with monotherapy. Clinical factors for PSA progression were a PSA nadir and a high clinical stage. Estimated PSA recurrence-free median survival time in each group was 57, 24, and 12 months, respectively. A PSA nadir of >0.2 ng/mL and metastatic stage were independent factors for expecting a poor response to PADT (hazard ratio 4.26, p<0.001; and 2.60, p<0.001).
Conclusions
Patients with localized or locally advanced prostate cancer who did not receive definitive therapy had lower PSA progression rates than those at metastatic stage during PADT. Further, a PSA nadir of ≤0.2 ng/mL showed better progression-free survival. Therefore, PADT can be another therapeutic option in well-selected patients with localized or locally advanced prostate cancer and PSA change should be checked carefully.
Keywords: Androgen antagonists, Prostate, Prostate neoplasms
INTRODUCTION
Huggins and Hodges [1] introduced androgen deprivation therapy (ADT) for prostate cancer based on the concept of androgen sensitivity. Its benefit as adjuvant therapy is well established, particularly in intermediate or high-risk patients [2,3,4,5,6]. ADT is also a treatment option with survival benefits for metastatic or incurable advanced prostate cancer. However, ADT is not definitive therapy for metastatic prostate cancer; therefore, the disease will progress and ultimately become castration resistant [7].
Despite a lack of data on primary androgen deprivation therapy (PADT), the number of patients receiving PADT as an alternative to other local therapies is increasing. In a 1999 to 2001 survey, PADT was the second most common treatment for localized prostate cancer [8]. If patients do not want definite therapy for prostate cancer or are a high operative risk due to advanced age or medical comorbidities, PADT is often used instead of definite local therapy [9,10]. Therefore, this retrospective study examined the clinical characteristics of patients undergoing PADT for prostate cancer and evaluated the factors affecting disease progression while receiving this treatment.
MATERIALS AND METHODS
1. Study population
The study enrolled all prostate cancer patients registered at five centers in Korea (three in Busan, one in Ulsan, and one in Seoul) who had undergone PADT for prostate cancer between 2000 and 2010. In all, 240 patients were studied. The collection and analysis of data were approved by the Institutional Review Board of each medical center. We retrospectively reviewed the PADT therapy data in terms of a comparison with prostate-specific antigen (PSA) progression. The patients were classified into three groups based on clinical stage: localized, locally advanced, and metastatic prostate cancer. Localized prostate cancer was defined as stage T1 to 2 without nodal invasion or distant metastasis. Locally advanced prostate cancer was defined as stage T3a, T3b, or T4 or N1 associated with any T stage if combined with an absence of distant metastasis. Metastatic prostate cancer was defined by the existence of any distant metastasis. All tumor stages were based on the tumor-node-metastasis (TNM) staging system [10].
The PSA nadir was defined as the lowest PSA level while on PADT. PSA progression was defined as three consecutive PSA increases from the PSA nadir while on PADT [9].
2. Statistical analysis
The analysis was performed using IBM SPSS Statistics version 20 (IBM Co., Armonk, NY, USA). The demographic, clinical, and pathological characteristics of the subjects were examined. The data were summarized using the median and range values. Clinical variables-such as age, body mass index (BMI), prostate size, and PSA levels- were compared among the groups by using analysis of variance. Categorical variables were compared using the chi-squared test and Fisher's exact test.
PSA progression was analyzed using a Kaplan-Meier curve, and a Cox regression model was used to identify predictors of PSA progression by univariate and multivariate analyses. A p value of <0.05 was considered to indicate statistical significance.
RESULTS
The clinical and pathological characteristics of the PADT patients are summarized in Table 1. The median follow-up on PADT was 24 months (range: 3~115) months. The median patient age was 73.0 years, and the median pretreatment PSA level was 47.0 ng/mL. Of the patients, 91.7% were treated with combined androgen blockade and 8.3% with monotherapy.
Table 1.
Characteristics of the patients treated with primary androgen-deprivation therapy
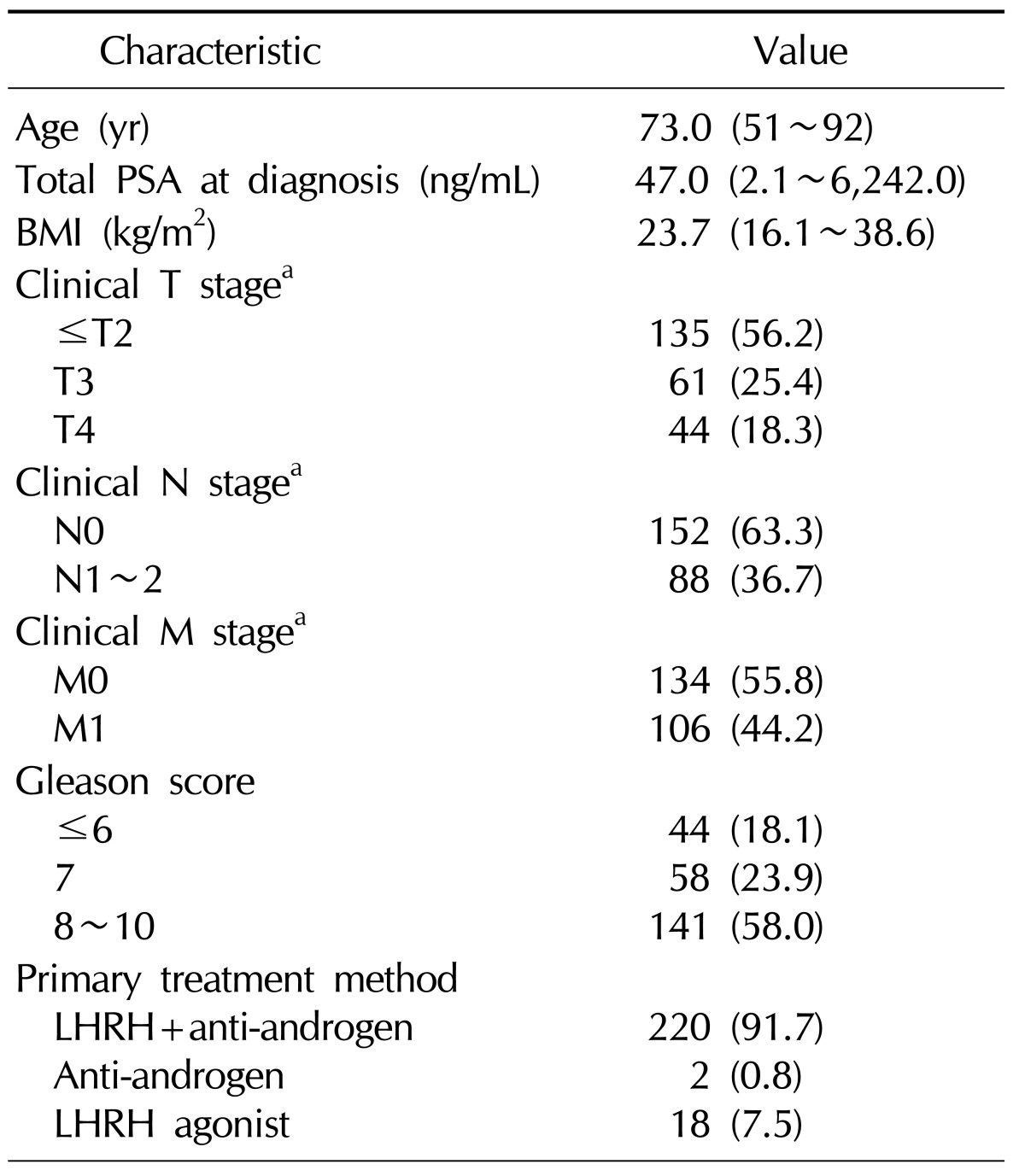
Values are presented as median (range) or number (%).
PSA: prostate-specific antigen, BMI: body mass index, LHRH: luteinizing hormone-releasing hormone.
aAll tumor stages were based on the tumor-node-metastasis (TNM) staging system.
Differences among the three groups according to clinical stage are shown in Table 2. Of the patients, 33.3% had localized, 22.5% had locally advanced, and 44.2% had metastatic prostate cancer. There were no significant differences in follow-up period or age among the groups. The patients with metastatic prostate cancer had the lowest BMI (22.5 kg/m2). The PSA levels at diagnosis were 14.9, 27.8, and 103.9 ng/mL in the localized, locally advanced, and metastatic groups. Of the patients with locally advanced prostate cancer, 48.1% had lymph node metastasis and 87.1% were at a more advanced stage than T3.
Table 2.
Comparison of the patients treated with primary androgen-deprivation therapy according to prostate cancer stage
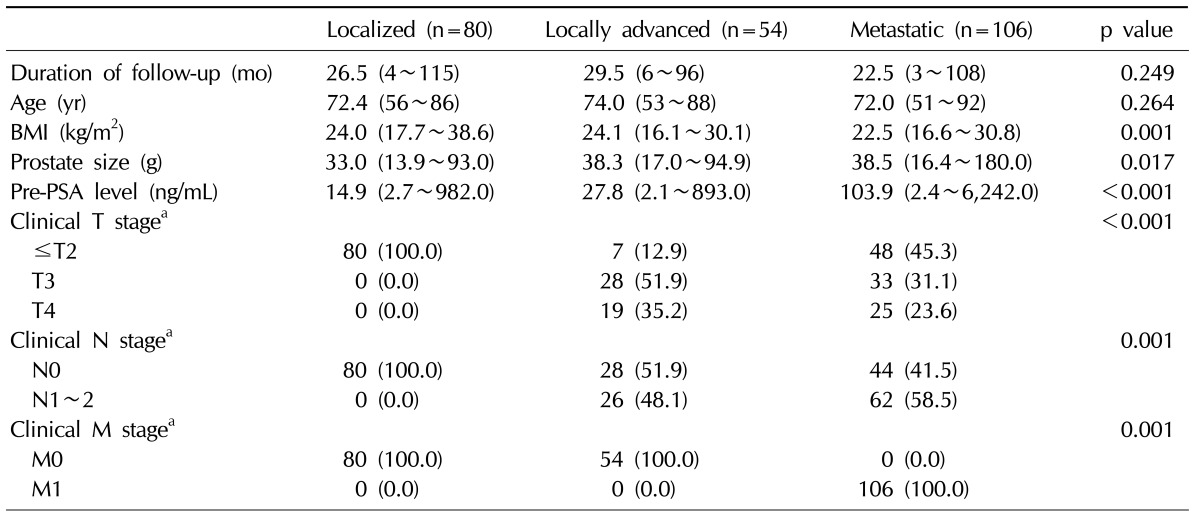
Values are presented as median (range) or number (%).
BMI: body mass index, PSA: prostate-specific antigen.
aAll tumor stages were based on the tumor-node-metastasis (TNM) staging system.
Clinical factors related to PSA progression were identified using Cox regression (Table 3). In the multivariate analysis, PSA nadir and stage significantly affected PSA progression during PADT, with hazard ratios of 4.26 and 2.60 (p<0.001), respectively.
Table 3.
Clinical factors predictive of PSA progression based on a Cox regression analysis
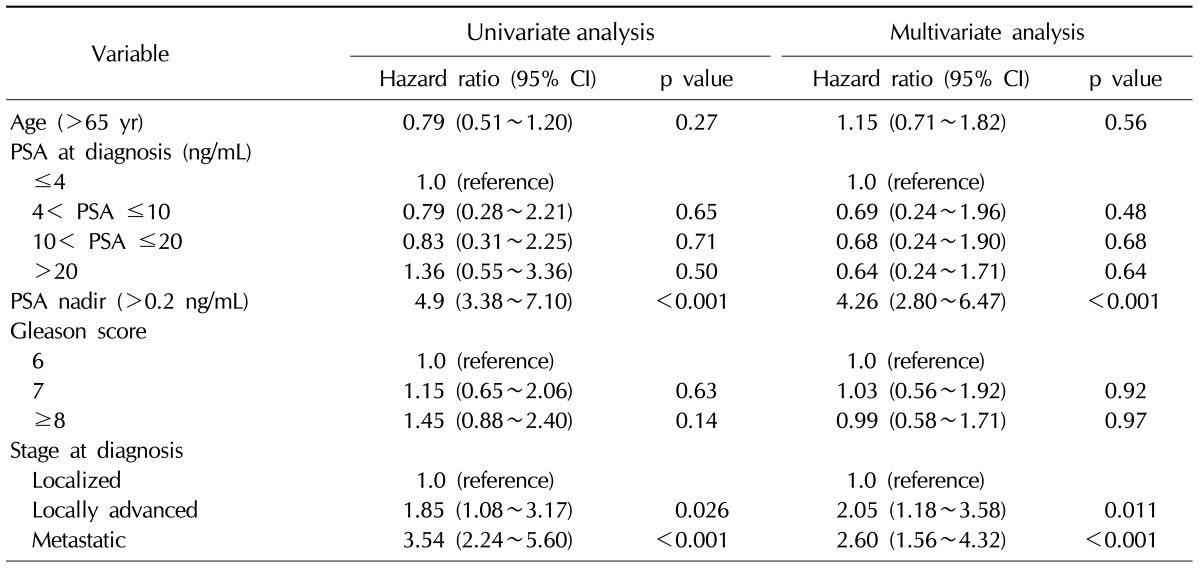
PSA: prostate-specific antigen, CI: confidence interval.
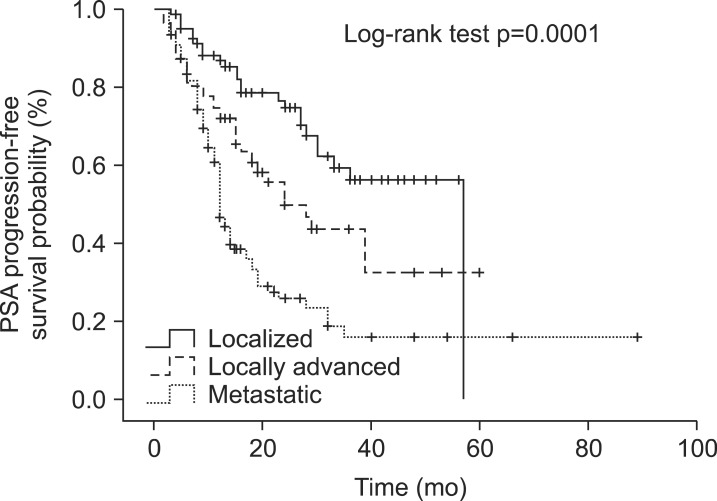
Fig. 1 shows the Kaplan-Meier analysis of the PSA progression- free survival rate after 3 years according to stage; the estimated values were 56.1%, 43.4%, and 16.1% (p=0.001), in the localized, locally advanced, and metastatic groups, respectively. The estimated PSA recurrence- free median survival durations in the respective groups were 57, 24, and 12 months.
Fig. 1.
Prostate-specific antigen (PSA) progression-free survival in prostate cancer patients on primary androgen-deprivation therapy.
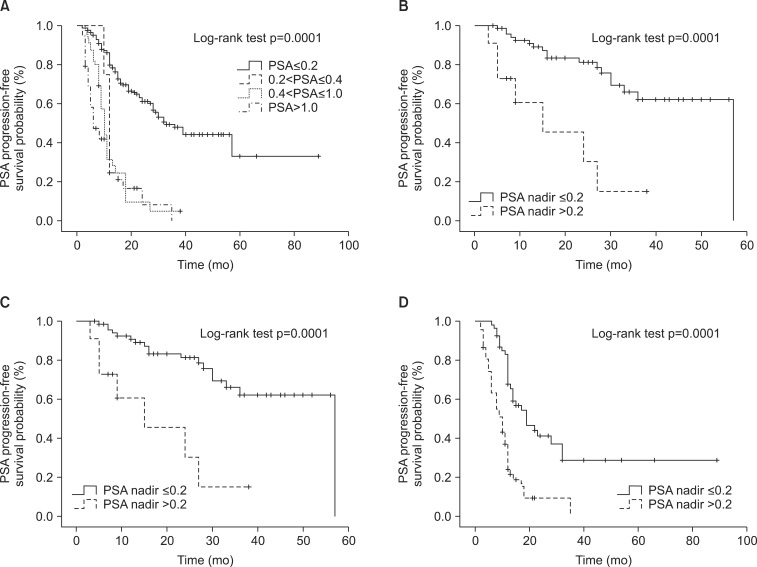
There was a significant difference in the survival rate between a PSA nadir of ≤0.2 and >0.2 ng/mL (Fig. 2A). Therefore, we considered a PSA level of 0.2 ng/mL to be the optimal PSA nadir after PADT. Using a PSA nadir of 0.2 ng/mL, we analyzed the progression-free survival rate in each stage. For the localized stage, the survival rate for a PSA nadir of ≤0.2 ng/mL was 62.1%, and the estimated median survival duration was 57 months, versus 15.1% and 15 months for a PSA nadir of >0.2 ng/mL (Fig. 2B). For locally advanced disease, the PSA progression-free survival rate was 49.3% for a PSA nadir of ≤0.2 ng/mL, and the estimated median survival duration was 29 months (Fig. 2C). In the metastatic stage, the PSA progression- free survival rate was 28.9%, and the estimated median survival duration was 19 months (Fig. 2D).
Fig. 2.
(A) Prostate-specific antigen (PSA) progression according to the PSA nadir. PSA progression-free survival in patients with localized (B), locally advanced (C), and metastatic prostate cancer given primary androgen-deprivation therapy according to the PSA nadir (D).
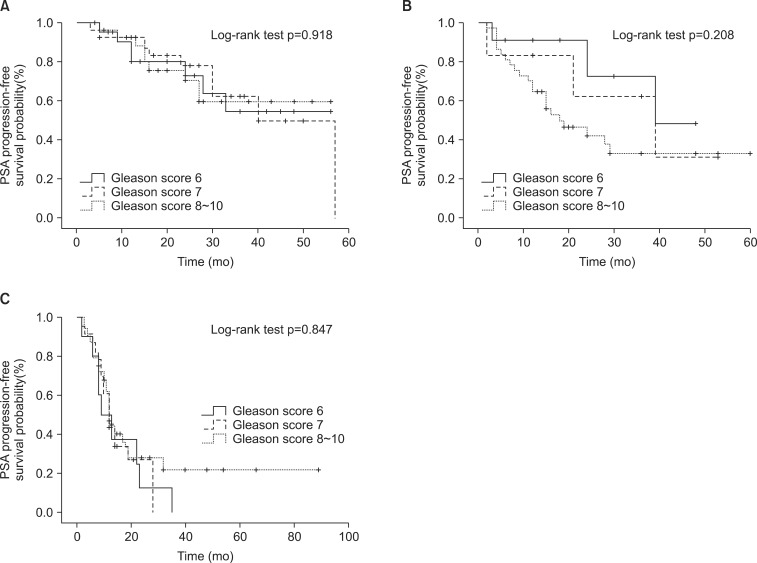
Fig. 3 shows differences in the progression-free survival rate according to Gleason score. There were no significant differences in the progression-free survival rate when analyzed using Gleason scores of 6, 7, and 8 to 10 in localized, locally advanced, and metastatic prostate cancer after PADT.
Fig. 3.
Prostate-specific antigen (PSA) progression-free survival in patients with localized (A), locally advanced (B), and metastatic prostate cancer on primary androgen-deprivation therapy according to the Gleason score (C).
DISCUSSION
No prospective study has compared PADT with control groups (e.g., conservative treatment, surgery, or other local therapy), and bias might affect patient selection. There are also no guidelines for PADT in terms of patient indications, tumor characteristics, life expectancy, starting and stopping times of therapy, and duration of therapy. Therefore, the selection of patients for PADT is important; the tumor characteristics should also be considered. Our study also did not compare the results with the results of any other definitive therapy or active surveillance. However, multicenter data regarding the trends and current state of PADT in Korea might assist clinicians in selecting appropriate PADT therapy.
Although there is insufficient evidence regarding the benefits of PADT in prostate cancer management, several studies have suggested its efficacy or clinical benefits. A retrospective study of the Cancer of the Prostate Strategic Urologic Research Endeavor (CaPSURE) data analyzed 993 males treated with PADT [11]. The 5-year disease-specific survival rate was 95.9%, and only 4.1% died from prostate cancer. In addition, 5 years after starting PADT, the treatment was still being applied to 67.3% of the patients. A long-term (20-year) single-center experience with PADT in localized or advanced prostate cancer reported results similar to those of the CaPSURE study [12]. The 5-, 10-, and 15-year disease-specific survival rates were 95.7%, 91.7%, and 84.9%, respectively. They also compared PADT with salvage ADT-no significant differences in disease-specific survival were evident. In a study comparing radical prostatectomy and PADT, the patients who underwent radical prostatectomy had a higher 10-year overall survival due to their longer expected life span (73% vs. 41%) [13]. However, there was no significant difference in the cancer-specific survival rate (86% vs. 78%). Therefore, PADT is an alternative treatment for prostate cancer, particularly for patients with a short expected life span with localized or locally advanced prostate cancer.
Contrasting these favorable results, a study of The Surveillance, Epidemiology, and End Result (SEER) program of national cancer institute data of patients >65 years of age suggested that a careful approach to PADT is warranted. Early PADT for localized prostate cancer, particularly low-risk cancer, is associated with an increased frequency of chemotherapy use [14]. This result was based on the molecular mechanism associated with an androgen receptor [15,16,17,18,19]. Lu-Yao et al [20] also investigated survival after PADT in localized prostate cancer and found that PADT reduced the 10-year disease-specific survival rate with a hazard ratio of 1.17 and was associated with no benefit in the 10-year overall survival rate compared with conservative treatment. They concluded that elderly patients with T1 to 2 prostate cancer derived no clinical benefit from PADT. However, these results did not show the uselessness of PADT but rather that the early start of PADT had no benefit as compared to conservative treatment in old-age patients.
Compared with the 75% 5-year progression-free survival rate of the Portland Veterans Affairs Medical Center, the survival rate for localized and locally advanced prostate cancer in our study (56.1% and 43.4%, respectively) was relatively low [9]. In 2009, Kim et al [21] reported that the 5-year progression-free survival in Korean patients was 73.6%. The most important reason for the lower progression- free survival rate in our study is the difference in the definition of progression. We defined progression after PADT as any increase in PSA after reaching the PSA nadir, while most studies used a definitive cut-off value for PSA, even if the patient's PSA nadir was lower than the cut-off value, or defined PSA progression as three consecutive PSA increases. For example, if the PSA nadir after PADT is 0.1 ng/mL but the PSA continues to increase, the patient is not considered to be experiencing progression. Only when the PSA level reaches a value above the cut-off, e.g., 4 ng/mL, is the patient classified as experiencing progression. Therefore, we detected patients showing PSA progression after PADT earlier than in other studies. We defined PSA progression as any PSA elevation during PADT to determine when the change in PSA occurs during PADT and to determine the optimal PSA nadir in patients with PADT.
Another possible reason for the difference as compared to other studies is the patient distribution. The median PSA in our series was 47.0 ng/mL, which was considerably higher than the 13.8 in Janoff et al [9] and 13.52 in Kim et al [21]. More advanced prostate cancer patients were selected for PADT in our series; this might have caused the differences in the survival rate. In addition, increasing use of surgery and radiation therapy might contribute to the low progression-free survival rate in PADT patients. Similarly, results of a study of the Japanese population showed a tendency for the survival with PADT to decrease from 50% to 40%, comparing 2004 to 2006 vs. 2007 to 2009 [22]. Despite these differences, the Asian consensus statement on PADT recommends using PADT even in the early stage [23].
The clinical stage and PSA nadir after PADT were independent predictors of PSA progression in our study. A PSA nadir greater than 0.2 ng/mL predicted a poor response to PADT for all clinical stages. In contrast, age at diagnosis and Gleason score were not associated with PSA progression. Young patients or those with a longer expected life span tend to have more aggressive prostate cancer; therefore, cancer progression in such individuals is more frequent than in elderly patients [24,25]. However, we found that age was not associated with cancer progression among the patients who underwent PADT, perhaps because of the relatively young age used as a cut-off in this study. The Gleason score also showed no significant relationship with PSA progression after PADT for any stage, with p values of 0.918, 0.208, and 0.847 for localized, locally advanced, and metastatic cancer, respectively. Therefore, contrary to expectations, cell differentiation in prostate cancer did not influence PSA progression after PADT in our study.
A major limitation of this study was the lack of a control group, such as a group of patients who underwent other local definitive therapy (surgery or radiation) or active surveillance. Another limitation was that no analysis of overall survival or cancer-specific survival was performed. Therefore, the efficacy and clinical benefits of PADT could not be estimated. However, we report the characteristics and trends of PADT in Korea through multicenter experiences for the first time ever, and expect this study to be a foundation for another prospective study on PADT.
CONCLUSIONS
In spite of some limitations and debates, PADT may be another option for prostate cancer control from the perspective of a less invasive treatment. However, the indications for PADT must be considered carefully, including patient age, cancer stage, tumor characteristics, treatment- related comorbidities, and socioeconomic status. Further, the observation for reaching the PSA nadir should be required for a response expectation. After more longterm follow-up data have been obtained, a large-scale comparison study is required to assess the efficacy of PADT.
References
- 1.Huggins C, Hodges CV. Studies in prostate cancer: the effect of castration, of estrogen and of androgen injection on serum phosphatases in metastatic carcinoma of prostate. Cancer Res. 1941;1:293–297. [Google Scholar]
- 2.Chedin M, Filhol O, Duminy C, Bolla M, Benistant C, Roche S, et al. Characterization of two different cytoplasmic protein tyrosine kinases from human breast cancer. Carcinogenesis. 1997;18:1463–1472. doi: 10.1093/carcin/18.8.1463. [DOI] [PubMed] [Google Scholar]
- 3.Bolla M, Collette L, Blank L, Warde P, Dubois JB, Mirimanoff RO, et al. Long-term results with immediate androgen suppression and external irradiation in patients with locally advanced prostate cancer (an EORTC study): a phase III randomised trial. Lancet. 2002;360:103–106. doi: 10.1016/s0140-6736(02)09408-4. [DOI] [PubMed] [Google Scholar]
- 4.Messing EM, Manola J, Sarosdy M, Wilding G, Crawford ED, Trump D. Immediate hormonal therapy compared with observation after radical prostatectomy and pelvic lymphadenectomy in men with node-positive prostate cancer. N Engl J Med. 1999;341:1781–1788. doi: 10.1056/NEJM199912093412401. [DOI] [PubMed] [Google Scholar]
- 5.D'Amico AV, Manola J, Loffredo M, Renshaw AA, DellaCroce A, Kantoff PW. 6-month androgen suppression plus radiation therapy vs radiation therapy alone for patients with clinically localized prostate cancer: a randomized controlled trial. JAMA. 2004;292:821–827. doi: 10.1001/jama.292.7.821. [DOI] [PubMed] [Google Scholar]
- 6.Schröder FH, Kurth KH, Fosså SD, Hoekstra W, Karthaus PP, Debois M, et al. Members of the European Organisation for the Research and Treatment of Cancer Genito-urinary Group. Early versus delayed endocrine treatment of pN1-3 M0 prostate cancer without local treatment of the primary tumor: results of European Organisation for the Research and Treatment of Cancer 30846: a phase III study. J Urol. 2004;172:923–927. doi: 10.1097/01.ju.0000135742.13171.d2. [DOI] [PubMed] [Google Scholar]
- 7.Pagliarulo V, Bracarda S, Eisenberger MA, Mottet N, Schröder FH, Sternberg CN, et al. Contemporary role of androgen deprivation therapy for prostate cancer. Eur Urol. 2012;61:11–25. doi: 10.1016/j.eururo.2011.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cooperberg MR, Grossfeld GD, Lubeck DP, Carroll PR. National practice patterns and time trends in androgen ablation for localized prostate cancer. J Natl Cancer Inst. 2003;95:981–989. doi: 10.1093/jnci/95.13.981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Janoff DM, Peterson C, Mongoue-Tchokote S, Peters L, Beer TM, Wersinger EM, et al. Clinical outcomes of androgen deprivation as the sole therapy for localized and locally advanced prostate cancer. BJU Int. 2005;96:503–507. doi: 10.1111/j.1464-410X.2005.05674.x. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of the Urinary System and Male Genital Organs. Chapter 3. Tumours of the Prostate [Internet] Lyon (France): IARC Press; 2004. [cited 2014 Jul 15]. Available from: http://www.iarc.fr/en/publications/pdfs-online/pat-gen/bb7/bb7-chap3.pdf. [Google Scholar]
- 11.Kawakami J, Cowan JE, Elkin EP, Latini DM, DuChane J, Carroll PR CaPSURE Investigators. Androgen-deprivation therapy as primary treatment for localized prostate cancer: data from Cancer of the Prostate Strategic Urologic Research Endeavor (CaPSURE) Cancer. 2006;106:1708–1714. doi: 10.1002/cncr.21799. [DOI] [PubMed] [Google Scholar]
- 12.DiBlasio CJ, Malcolm JB, Hammett J, Wan JY, Aleman MA, Patterson AL, et al. Survival outcomes in men receiving androgen-deprivation therapy as primary or salvage treatment for localized or advanced prostate cancer: 20-year single-centre experience. BJU Int. 2009;104:1208–1214. doi: 10.1111/j.1464-410X.2009.08593.x. [DOI] [PubMed] [Google Scholar]
- 13.Akaza H, Homma Y, Usami M, Hirao Y, Tsushima T, Okada K, et al. Prostate Cancer Study Group. Efficacy of primary hormone therapy for localized or locally advanced prostate cancer: results of a 10-year follow-up. BJU Int. 2006;98:573–579. doi: 10.1111/j.1464-410X.2006.06349.x. [DOI] [PubMed] [Google Scholar]
- 14.Lu-Yao GL, Albertsen PC, Li H, Moore DF, Shih W, Lin Y, et al. Does primary androgen-deprivation therapy delay the receipt of secondary cancer therapy for localized prostate cancer? Eur Urol. 2012;62:966–972. doi: 10.1016/j.eururo.2012.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koivisto P, Kononen J, Palmberg C, Tammela T, Hyytinen E, Isola J, et al. Androgen receptor gene amplification: a possible molecular mechanism for androgen deprivation therapy failure in prostate cancer. Cancer Res. 1997;57:314–319. [PubMed] [Google Scholar]
- 16.Koivisto PA, Helin HJ. Androgen receptor gene amplification increases tissue PSA protein expression in hormone-refractory prostate carcinoma. J Pathol. 1999;189:219–223. doi: 10.1002/(SICI)1096-9896(199910)189:2<219::AID-PATH423>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 17.Shi Y, Brands FH, Chatterjee S, Feng AC, Groshen S, Schewe J, et al. Her-2/neu expression in prostate cancer: high level of expression associated with exposure to hormone therapy and androgen independent disease. J Urol. 2001;166:1514–1519. doi: 10.1016/s0022-5347(05)65822-3. [DOI] [PubMed] [Google Scholar]
- 18.Ricciardelli C, Jackson MW, Choong CS, Stahl J, Marshall VR, Horsfall DJ, et al. Elevated levels of HER-2/neu and androgen receptor in clinically localized prostate cancer identifies metastatic potential. Prostate. 2008;68:830–838. doi: 10.1002/pros.20747. [DOI] [PubMed] [Google Scholar]
- 19.Jennbacken K, Tesan T, Wang W, Gustavsson H, Damber JE, Welén K. N-cadherin increases after androgen deprivation and is associated with metastasis in prostate cancer. Endocr Relat Cancer. 2010;17:469–479. doi: 10.1677/ERC-10-0015. [DOI] [PubMed] [Google Scholar]
- 20.Lu-Yao GL, Albertsen PC, Moore DF, Shih W, Lin Y, DiPaola RS, et al. Survival following primary androgen deprivation therapy among men with localized prostate cancer. JAMA. 2008;300:173–181. doi: 10.1001/jama.300.2.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim TS, Kang SH, Rhew HY. Efficacy of androgen deprivation therapy in patients with clinically localized prostate cancer. Korean J Urol. 2009;50:1073–1077. [Google Scholar]
- 22.Tanaka N, Hirayama A, Yoneda T, Yoshida K, Shimada K, Konishi N, et al. Trends of risk classification and primary therapy for Japanese patients with prostate cancer in Nara Uro-Oncological Research Group (NUORG): a comparison between 2004-2006 and 2007-2009. BMC Cancer. 2013;13:588. doi: 10.1186/1471-2407-13-588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Akaza H. Asian trends in primary androgen depletion therapy on prostate cancer. Cancer Biol Med. 2013;10:187–191. doi: 10.7497/j.issn.2095-3941.2013.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bill-Axelson A, Holmberg L, Ruutu M, Häggman M, Andersson SO, Bratell S, et al. Scandinavian Prostate Cancer Group Study No. 4. Radical prostatectomy versus watchful waiting in early prostate cancer. N Engl J Med. 2005;352:1977–1984. doi: 10.1056/NEJMoa043739. [DOI] [PubMed] [Google Scholar]
- 25.Situmorang GR, Umbas R, Mochtar CA, Santoso RB. Prostate cancer in younger and older patients: do we treat them differently? Asian Pac J Cancer Prev. 2012;13:4577–4580. doi: 10.7314/apjcp.2012.13.9.4577. [DOI] [PubMed] [Google Scholar]