Abstract
Background:
Chronic obstructive pulmonary disease (COPD) is characterized by progressive deterioration of respiratory function along with systemic effects which have a great impact on health-related quality of life (HRQoL). Classification of severity of airflow limitation in COPD does not represent the clinical consequences of COPD. Hence, combined COPD assessment should be preferred. BODE index (Body mass index, Airflow obstruction, Dyspnea and Exercise capacity) has recently been proposed to provide useful prognostic information.
Objectives:
To find out correlations between the BODE index and HRQoL, and between GOLD classification of COPD severity and HRQoL in stable COPD patients, and to compare between these two correlations.
Materials and Methods:
A longitudinal observational study was carried out with 114 stable COPD patients recruited over 10 months at the outpatient clinic of a tertiary care hospital in Kolkata, India. Patients were classified according to GOLD classification of severity of airflow limitation after performing spirometry. BODE index was calculated for each patient. Saint George's Respiratory Questionnaire (SGRQ) was used to assess the HRQoL.
Results:
BODE scores were categorized into four quartiles, quartile one to four with scores of 0-2, 3-4, 5-6 and 7-10, respectively. Higher BODE quartiles were associated with higher total SGRQ scores and SGRQ subscale scores (symptom, activity and impact). Very strong correlations were found between BODE quartiles and total SGRQ scores (P = 0.914; P < 0.01). In contrast, GOLD classes showed moderate correlation with total SGRQ scores (P = 0.590; P < 0.01).
Conclusions:
BODE index was strongly correlated with the HRQoL in stable COPD patients and it was better than GOLD classes of COPD severity to reflect the health status in patients with stable COPD.
Keywords: BODE index, chronic obstructive pulmonary disease, health-related quality of life, Saint George's respiratory questionnaire
INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is a common preventable and treatable disease characterized by persistent airflow limitation that is usually progressive.[1] It is a leading cause of morbidity and mortality worldwide and results in a substantial economic and social burden. It is characterized by progressive deterioration of respiratory function over time and systemic effects that lead to permanent disability in the form of dyspnea, fatigue, limited exercise capacity, and a negative impact on quality of life.[2] The major manifestation of airflow obstruction in COPD is the reduction in forced expiratory volume in first second (FEV1) which form the basis of the classification of COPD severity by the global initiative for chronic obstructive lung disease (GOLD).[3] As COPD is a complex multi-dimensional disease, the disease progression and treatment efficacy are assessed with different parameters like imaging, spirometric assessment of lung function, frequency of exacerbations, exercise capacity, health-related quality of life (HRQoL), social and economic burden, pulmonary and non-pulmonary biomarkers and mortality, etc.[4] The evaluation of lung function by FEV1 alone does not represent the complex clinical consequences of COPD.[5] FEV1 is also known to correlate poorly with patients' symptoms, quality of life, exacerbation frequency and exercise intolerance.[6] Hence, newer approaches to disease assessment are required which can supersede the FEV1 -based GOLD classification of disease severity.
In 2004, Celli et al. created a mortality prediction index, known as BODE index (Body mass index, airway Obstruction, Dyspnea and Exercise capacity) which is a multistage scoring system that provides useful prognostic information in patients with COPD.[7] BODE scores greater than 7, 5-6 and less than 5 are associated with a 2-year mortality of 30%, 15% and 10%, respectively. It has been shown that BODE index is better than the FEV1 at predicting the risk of death among COPD patients.[8] However, it is not well known whether the BODE index is a sensitive tool for predicting the HRQoL in COPD patients. HRQoL is a questionnaire of patient-reported outcome, where the responses are collected directly from the patient via self-administered questionnaires completed by the patient themselves or via interviews. HRQoL is an important clinical outcome in patients with COPD.[9] Recently there has been a substantial increase in the use of developed tools that measure health status as clinicians and researchers realize that improving patients' symptoms, functional status, and quality of life are important goals in the management of COPD.[10] St. George's Respiratory Questionnaire (SGRQ), Chronic Respiratory Questionnaire (CRQ), Clinical COPD Questionnaire (CCQ), Medical Outcomes Study Short Form-36 (SF-36) are such tools commonly used to measure the health-related quality of life.
We have undertaken this study to assess the correlations between the BODE index and HRQoL and between HRQoL and GOLD classification of COPD severity in stable COPD patients and to compare between these two correlations.
MATERIALS AND METHODS
In this longitudinal observational study, 114 consecutive stable COPD patients (patients without any exacerbation in the previous 4 weeks) were recruited from the outpatient clinic of Pulmonary Medicine OPD of Medical College, Kolkata, India over 10 months. The study protocol was approved by the institutional Ethics Committee. Informed consent was obtained from all patients. Following inclusion criteria were used for selection of the patient: (1) Age of 18 years or more, (2) spirometric diagnosis of COPD and (3) clinically stable with no exacerbation within the last 4 weeks. Exclusion criteria used were: (1) Inability to perform the spirometry or 6-min walk test, (2) patients with concomitant other pulmonary diseases like asthma, diffuse parenchymal lung disease, bronchiectasis, pulmonary tuberculosis and lung cancer, (3) patients with history of acute myocardial infarction, unstable angina or congestive cardiac failure within 4 weeks and (4) Previous lung resection surgery.
Detailed history and thorough physical examination were carried out in all patients. Body mass index (BMI) was calculated with the formula: 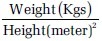 Spirometry was performed as per ATS/ERS recommendation[11] using Spirometer RMS MEDSPIROR (Recorders and Medicare Systems Pvt. Ltd., Chandigarh, India) to measure post bronchodilator FEV1, FVC and the FEV1 /FVC. Severity of dyspnea was assessed with the modified Medical Research Council (mMRC) dyspnea scale. Six minute walk test was performed according to the ATS recommendation.[12]
Spirometry was performed as per ATS/ERS recommendation[11] using Spirometer RMS MEDSPIROR (Recorders and Medicare Systems Pvt. Ltd., Chandigarh, India) to measure post bronchodilator FEV1, FVC and the FEV1 /FVC. Severity of dyspnea was assessed with the modified Medical Research Council (mMRC) dyspnea scale. Six minute walk test was performed according to the ATS recommendation.[12]
BODE index score was calculated by summation of score obtained for each variable (BMI, post bronchodilator FEV1, mMRC dyspnea scale and 6 min walk distance (6MWD)).
HRQoL was measured using the English and vernacular versions of the SGRQ validated to be used in Indian population.[13,14] Statistical analysis was carried out using SPSS 17 for Windows. Data were expressed as mean ± SD. Spearman's correlation coefficient (ρ) and Pearson's correlation coefficient (r) analysis were done to find out the correlation between different variables. Strength of correlation was interpreted according to the value of correlation coefficient ranges from −1 to +1, where ‘−’ denotes negative correlation and ‘+’ denotes positive correlation and weak, moderate, strong and very strong correlation are indicated by ≤0.35, 0.36-0.67, 0.68-0.89 and ≥0.90, respectively.
RESULTS
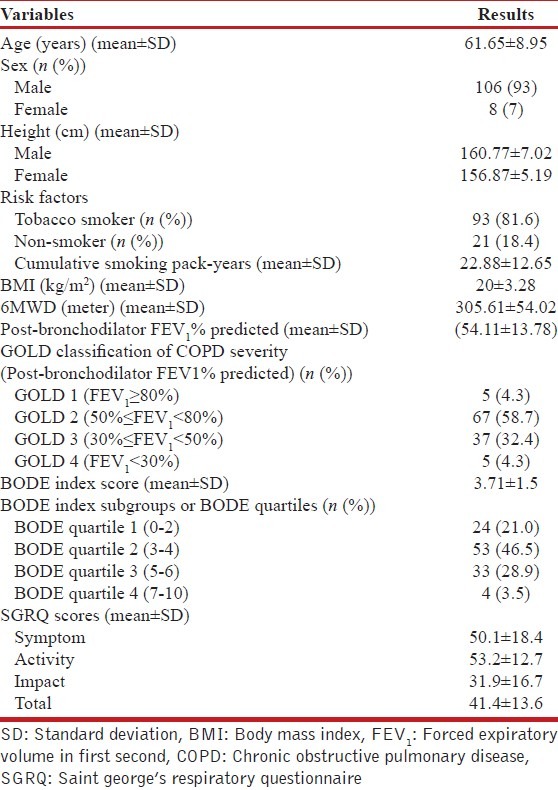
Mean age was 61.65 ± 8.95 years and 93% were male. Cumulative smoking pack-year was 22.88 ± 12.65. BMI was 20 ± 3.28 kg/m2, 6MWD was 305.61 ± 54.02 meter. Mean post-bronchodilator FEV1 % predicted was (54.11 ± 13.78) %. A total of 4.3% of patients were in GOLD class 1, 58.7% in GOLD class 2, 32.4% in GOLD class 3, and 4.3% in GOLD class 4. BODE index score was 3.71 ± 1.5. SGRQ scores were as follows: Symptom 50.1 ± 18.4, activity 53.2 ± 12.7, impact 31.9 ± 16.7 and total 41.4 ± 13.6 [Table 1].
Table 1.
Baseline demographic characteristics of the study population
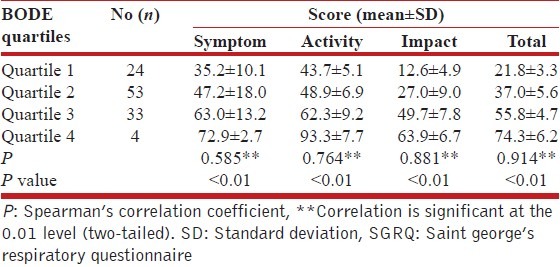
BODE index scores measured were categorized into four quartiles, quartile 1 to 4 with scores of 0-2, 3-4, 5-6 and 7-10, respectively. Mean total SGRQ scores gradually increased with the increase in BODE index quartiles [Table 2]. The mean total SGRQ score was lowest in BODE quartile 1 and highest in BODE quartile 4. Mean symptom, activity and impact scores also increased with the increase in BODE index quartiles. Very strong correlation (P = 0.914; P < 0.01) was found between BODE quartiles and baseline total SGRQ scores. BODE index quartiles also showed strong correlation with the activity (P = 0.764; P < 0.01) and impact (P = 0.881; P < 0.01) domains of SGRQ score, but showed moderate correlation with the symptom domain (P = 0.585; P < 0.01).
Table 2.
Distribution of SGRQ scores according to BODE quartiles
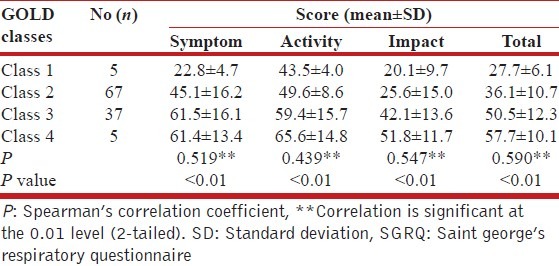
Mean total SGRQ score increased according to increase in GOLD classes [Table 3] being lowest in GOLD class 1 and highest in GOLD class 4. Mean activity and impact scores also increased with the increase in GOLD classes. But mean symptom scores increased with increase in GOLD classes up to class 3 only. Moderate correlation (P =0.590; P < 0.01) was found between GOLD classes and baseline total SGRQ scores.
Table 3.
Distribution of SGRQ scores according to GOLD stages
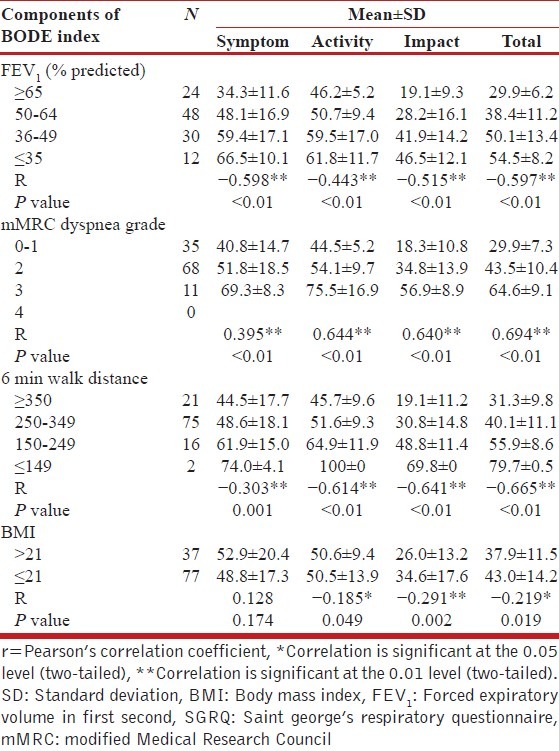
There were increases in mean total SGRQ score and mean scores of SGRQ components (symptom, activity, impact) with the decrease of FEV1 %predicted and 6MWD and with the increase of mMRC dyspnea grade [Table 4]. Moderate negative correlations were found between FEV1 %predicted and total SGRQ score as well as between 6MWD and total SGRQ scores. Moderate positive correlation was found between mMRC dyspnea grade and total SGRQ score. Lower BMI (≤21) was associated with higher total SGRQ score and higher BMI (>21) was associated with lower total SGRQ score. But the correlation between the BMI and total SGRQ scores was weak (r = −0.219; P < 0.05).
Table 4.
Distribution of mean SGRQ scores according to the individual components of BODE index
DISCUSSION
This study intended to find out the correlation among FEV1 -based GOLD classes, BODE index and health-related quality of life as assessed by SGRQ. Studies show that post-bronchodilator FEV1 % predicted correlates weakly or not at all with the quality of life assessed by SGRQ score[15,16] and FEV1 is not identified as a predictor of health-related quality of life in COPD patient.[17] Antonelli-Incalzi et al. in their study found that the GOLD staging of COPD corresponded to important differences in health status between stages II and III, but not between other consecutive stages, and the authors concluded that crossing the boundary of a FEV1 of < 50% of predicted was likely to herald a dramatic decline in health status.[18] Our study shows that GOLD classes correlated modestly with baseline SGRQ score (P = 0.590; P < 0.01).
Higher BODE quartiles were associated with higher (worse) SGRQ scores. The differences among the BODE quartiles in health status indexes were significant for total SGRQ as well as all three of the SGRQ components. BODE index quartiles showed very strong correlation with the total SGRQ score. BODE index quartiles also showed strong correlation with the activity and impact domain of SGRQ score, but showed moderate correlation with the symptom domain. Authors of a previous study also believed that BODE index could correlate significantly with the quality of life questionnaire scores and was shown to be an independent predictor of health-related quality of life.[6] Authors thought that consistent with the GOLD classification, important differences in health status between the highest quartiles (quartiles 3 and 4) of the BODE classification system were observed but not between lower grade consecutive quartiles. This suggested that health status might be relatively preserved in these patients till the disease was very advanced and every effort should thus be made to prevent disease progression even in severe COPD before a dramatic decline of health status occurred.
Among the individual components of BODE index, the decrease of lung function (FEV1 %predicted), and 6MWD, and the increase of MMRC dyspnea grade were associated with corresponding increase in total SGRQ and SGRQ components (symptom, activity, impact). These components correlated modestly with the total SGRQ score.
Lower BMI (≤21 kg/m2) was associated with higher total SGRQ score (worse health status) and higher BMI (>21 kg/m2) was associated with lower total SGRQ score (better health status); but the correlation between the BMI and total SGRQ scores was weak. Similar findings were found in the study done by Lin et al.[19]
Dyspnea leads to limited daily activities and impaired quality of life in COPD patients. MMRC scores are found to be responsible for the SGRQ score variance in different studies which showed that dyspnea perception could explain 25% to 54% of the quality of life score variance in COPD patients[20] with a strong relationship between SGRQ-assessed quality of life and dyspnea perception. Our study established moderate positive correlation between mMRC dyspnea scale and SGRQ score at baseline (r = 0.694; P < 0.01). Some studies have shown a significant correlation between 6MWT distance and quality of life scores, and that exercise intolerance could influence quality of life in COPD patients.[20,21,22] This study shows moderate negative correlation between 6MWD and SGRQ score (r = -0.665; P < 0.01).
Though some authors have found a relationship between low BMI and peripheral muscle impairment and consequently low exercise capacity in individuals with COPD,[23] we found no definite relationship between BMI and exercise capacity as measured by 6MWD.
Several limitations in this study need discussion. First, we did not assess anxiety and depression which are known to affect the quality of life in COPD patients.[14] Second, percentages of female COPD was very less (7%) in our study. This might not represent the overall prevalence of female COPD patients in India.[24] Third, whether the findings in our study are also applicable to other ethnic groups are not well determined. Lastly, it would be better to determine the correlations between the BODE index and HRQOL, and between GOLD classes and HRQoL after a follow-up period along with the baseline correlations. But, patients were not followed up in our study.
CONCLUSION
BODE index was found to be superior to the GOLD class to predict the health status among stable COPD patients. Among the components of BODE index, the decrease in the FEV1 (%predicted) and 6MWD, and the increase of mMRC dyspnea grade were associated with worsening of health status (increase in total SGRQ and SGRQ subscales). Lower BMI (≤21 kg/m2) was associated with higher total SGRQ score (worse health status), but there was weak correlation between the BMI and total SGRQ scores.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. [Last accessed on 9th August, 2013]. Available from: https://www.goldcopd.com .
- 2.Jones PW, Prince M, Wijkstra PJ, Patel V, Saxena S, Maj M, et al. Quality of life in patients with chronic obstructive pulmonary disease. Eur Respir Mon. 2006;38:375–86. [Google Scholar]
- 3.Seemungal TA, Hurst JR, Wedzicha JA. Exacerbation rate, health status and mortality in COPD--a review of potential interventions. Int J Chron Obstruct Pulmon Dis. 2009;4:203–23. doi: 10.2147/copd.s3385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cazzola M, MacNee W, Martinez FJ, Rabe KF, Franciosi LG, Barnes PJ, et al. American Thoracic Society; European Respiratory Society Task Force on Outcomes of COPD. Outcomes for COPD pharmacological trials: From lung function to biomarkers. Eur Respir J. 2008;31:416–69. doi: 10.1183/09031936.00099306. [DOI] [PubMed] [Google Scholar]
- 5.Nici L, Donner C, Wouters E, Zuwallack R, Ambrosino N, Bourbeau J, et al. ATS/ERS Pulmonary Rehabilitation Writing Committee. American Thoracic Society/European Respiratory Society statement on pulmonary rehabilitation. Am J Respir Crit Care Med. 2006;173:1390–413. doi: 10.1164/rccm.200508-1211ST. [DOI] [PubMed] [Google Scholar]
- 6.Ong KC, Lu SJ, Soh CS. Does the multidimensional grading system (BODE) correspond to differences in health status of patients with COPD? Int J Chron Obstruct Pulmon Dis. 2006;1:91–6. doi: 10.2147/copd.2006.1.1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Celli BR, Cote CG, Marin JM, Casanova C, Montes de Oca M, Mendez RA, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004;350:1005–12. doi: 10.1056/NEJMoa021322. [DOI] [PubMed] [Google Scholar]
- 8.Shapiro SD, Reilly JJ, Rennard SI. Chronic bronchitis and emphysema. In: Mason RJ, Broaddus VC, Martin TR, King TE Jr, Schraufnagel DE, Murray JF, editors. Murray and Nadel's Textbook of Respiratory Medicine. 5th ed. Philadelphia: Saunders Elsevier; 2010. pp. 919–76. [Google Scholar]
- 9.Aslani J, Mirzamani SM, AzizAbadi-Farahani M, Moghani Lankarani MM, Assari S. Health-related quality of life in chronic obstructive pulmonary disease: Are disease-specific and generic quality of life measures correlated? Tanaffos. 2008;7:28–35. [Google Scholar]
- 10.Curtis JR, Patrick DL. The assessment of health status among patients with COPD. Eur Respir J Suppl. 2003;41:36–45s. doi: 10.1183/09031936.03.00078102. [DOI] [PubMed] [Google Scholar]
- 11.Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardization of spirometry. Eur Respir J. 2005;26:319–38. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 12.ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: Guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111–7. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 13.Jones PW, Forde Y. St. George Respiratory Questionnaire Mannual. [Last assessed on 2013 Nov 12]. Available from: http://www.healthstatus.sgul.ac.uk .
- 14.Aggarwal AN, Gupta D, Kumar T, Singh N, Jindal SK. Validation of Hindi translation of St. George's Respiratory Questionnaire in Indian patients with chronic obstructive pulmonary disease. Indian J Chest Dis Allied Sci. 2007;49:87–92. [Google Scholar]
- 15.Tsiligianni I, Kocks J, Tzanakis N, Siafakas N, van der Molen T. Factors that influence disease-specific quality of life or health status in patients with COPD: A review and meta-analysis of Pearson correlations. Prim Care Respir J. 2011;20:257–68. doi: 10.4104/pcrj.2011.00029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jones PW. Health status and the spiral of decline. COPD. 2009;6:59–63. doi: 10.1080/15412550802587943. [DOI] [PubMed] [Google Scholar]
- 17.Camelier A, Rosa FW, Jones PW, Jardim JR. Brazilian version of airways questionnaire 20: A reproducibility study and correlations in patients with COPD. Respir Med. 2005;99:602–8. doi: 10.1016/j.rmed.2004.09.022. [DOI] [PubMed] [Google Scholar]
- 18.Antonelli-Incalzi R, Imperiale C, Bellia V, Catalano F, Scichilone N, Pistelli R, et al. Do GOLD stages of COPD severity really correspond to differences in health status? Eur Respir J. 2003;22:444–9. doi: 10.1183/09031936.03.00101203. [DOI] [PubMed] [Google Scholar]
- 19.Lin YX, Xu WN, Liang LR, Pang BS, Nie XH, Zhang J, et al. The cross-sectional and longitudinal association of the BODE index with quality of life in patients with chronic obstructive pulmonary disease. Chin Med J (Engl) 2009;122:2939–44. [PubMed] [Google Scholar]
- 20.Katsura H, Yamada K, Kida K. Both generic and disease specific health-related quality of life are deteriorated in patients with underweight COPD. Respir Med. 2005;99:624–30. doi: 10.1016/j.rmed.2004.09.017. [DOI] [PubMed] [Google Scholar]
- 21.González E, Herrejón A, Inchaurraga I, Blanquer R. Determinants of health-related quality of life in patients with pulmonary emphysema. Respir Med. 2005;99:638–44. doi: 10.1016/j.rmed.2004.09.019. [DOI] [PubMed] [Google Scholar]
- 22.Oga T, Nishimura K, Tsukino M, Sato S, Hajiro T. Analysis of the factors related to mortality in chronic obstructive pulmonary disease: Role of exercise capacity and health status. Am J Respir Crit Care Med. 2003;167:544–9. doi: 10.1164/rccm.200206-583OC. [DOI] [PubMed] [Google Scholar]
- 23.Araujo ZT, Holanda G. Does the BODE index correlate with quality of life in patients with COPD? J Bras Pneumol. 2010;36:447–52. doi: 10.1590/s1806-37132010000400009. [DOI] [PubMed] [Google Scholar]
- 24.Jindal SK. Emergence of chronic obstructive pulmonary disease as an epidemic in India. Indian J Med Res. 2006;124:619–30. [PubMed] [Google Scholar]


