Abstract
Cough is the most common symptom for which medical treatment is sought in the outpatient setting. Chronic dry cough poses a great diagnostic and management challenge due to myriad etiologies. Chronic cough has been commonly considered to be caused by gastroesophageal reflux, post-nasal drip or asthma. However, recent evidences suggest that many patients with these conditions do not have cough, and in those with cough, the response to specific treatments is unpredictable at best. This raises questions about the concept of a triad of treatable causes for chronic cough. This article discusses the mechanism and etiology of cough, along with recent advances in the field of cough, highlighting some of the diagnostic and management challenges.
Keywords: Cough, chronic cough, diagnosis, guidelines, management
INTRODUCTION
Cough is an important natural defense mechanism of the respiratory tract.[1] It can also be a warning sign of several respiratory and non-respiratory diseases and is one of the most common reasons for adults seeking medical treatment.[1,2] Acute or short-lived cough, which often occurs in association with upper respiratory tract infection, is usually self-limiting and usually resolves within three weeks.[3] However, chronic cough (persisting greater than eight weeks) can lead to considerable morbidity, including exhaustion, disturbance of sleep, cough syncope, urinary stress incontinence, and work absenteeism. Chronic cough, in more severe cases, can also cause rib fractures, pneumothorax, pneumomediastinum (PM), and subcutaneous emphysema. Chronic cough is reported in approximately 10-20% of the general population.[4] Most patients with chronic cough present with a dry or minimally productive cough. It poses a great diagnostic and management challenge, due to the myriad etiologies.
This review will discuss the mechanism and etiology of the cough, along with recent advances in the field of cough, highlighting some of the diagnostic and management challenges. In preparing this section, PUBMED was searched, for studies published in the English language, using medical subject heading terms like ‘cough’, ‘chronic cough’, ‘chronic dry cough’, ‘causes of dry cough’, ‘etiology of dry cough’, ‘mechanism of dry cough’, ‘diagnosis of chronic cough’, and ‘chronic cough management guidelines’. Also, any references from these studies that were pertinent to the topic were obtained.
Mechanisms of chronic cough: Peripheral reflex and brain control
In general, coughing is characterized by a reflex-evoked modification of the normal breathing pattern. However, coughing can also be initiated and suppressed voluntarily. Stimulation of the peripheral sensory nerves is the first step that drives resultant cough. These sensory neurons can be divided into two types:[5] Those with chemosensitive nociceptors-the transmission mechanism in these neurons is controlled by transient receptor potential cation channels, especially the transient receptor potential vanilloid 1 and ankyrin 1 (TRPV1 and TRPA1).[5] The other type of sensory neurons are those that have low-threshold mechanosensors. These receptors react to touch-like mechanical stimuli, but are not chemically reactive, and therefore, do not respond to the capsaicin test.[5] The transmission in these neurons occurs through myelinated nerve fibers. Both these sensory afferent pathways finally terminate at the brainstem, at the nucleus of the solitary tract, and the spinal trigeminal tract. Second-order neurons from the solitary nucleus and the trigeminal nucleus are connected to neurons of the brainstem and the spinal respiratory circuit, which coordinate the efferent cough response.[6]
The causes of cough - The conventional view
Chronic cough can be caused by a myriad of different respiratory or non-respiratory conditions. The common causes of chronic cough include viral infections of the upper respiratory tract, upper airway cough syndrome (UACS; postnasal drip syndrome), gastroesophageal reflux disease (GERD), cough-variant asthma, eosinophilic bronchitis, mediastinal tumors, pleural diseases, early interstitial fibrosis, use of an angiotensin converting enzyme-inhibitor (ACEI), and psychogenic and idiopathic (or unexplained) cough.[4] It has been reported that causes of cough cannot be identified in up to 42% of the patients presenting at a specialized clinic.[7] The latest American College of Chest Physicians (ACCP) Consensus Guidelines, which analyzed the data of 11 studies worldwide, reported that postnasal drip, GERD, and cough-variant asthma were the most common causes of chronic cough, comprising two-thirds of all diagnoses [Figure 1]. On the basis of these findings, ACCP recommends investigation and systematic treatment of this triad of underlying triggers in the absence of other disorders.[8]
Figure 1.
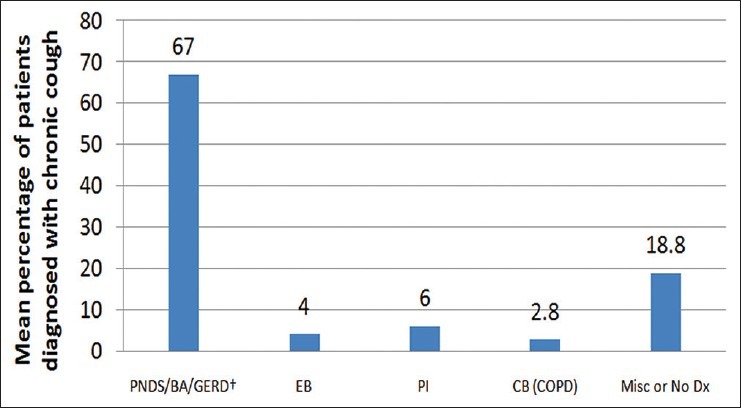
The most common causes of chronic cough reported in the literature
Assessment and management of the common triad of cough etiologies
Upper airway cough syndrome
The ACCP 2006 guidelines has suggested the term ‘UACS’ instead of the previously described ‘postnasal drip syndrome’.[9] This is because UACS more effectively addresses the possibility that cough in these patients occurs not only because of postnasal drip, but can occur as a result of irritation or inflammation of the upper airway structures that directly stimulate the cough receptors independently or in addition to the postnasal drip.[10] Rhinitis or rhinosinusitis commonly appears in the reported causes of cough in these patients.[11] The common clinical signs and symptoms associated with UACS include a feeling of drainage in the posterior pharynx, frequent throat clearing, nasal discharge, cobblestone appearance of the oropharyngeal mucosa, and mucopurulent secretions in the oropharynx. Although these clinical findings are relatively sensitive, they lack specificity.[9]
Part of the lack of specificity of a UACS diagnosis stems from the non-availability of an objective test. In patients with an atypical clinical presentation, the diagnosis is often established only after the response to empirical treatment with oral first-generation antihistamines/decongestants, which are preferred over newer agents.[10] Use of intranasal corticosteroids for two to eight weeks or oral antihistamines or nasal ipratropium bromide is also recommended in selected patients with rhinitis.[9] In case patients do not respond to empirical treatment, sinus imaging, preferably with a CT scan, is indicated.[10]
Asthma/nonasthmatic eosinophilic bronchitis
Chronic dry cough may present as a predominant symptom or even the only symptom (as in the case of cough-variant asthma) in patients with asthma.[9] In a majority of patients with cough-variant asthma, dry cough often occurs at night.[1] The pathophysiology of dry cough in asthma can be explained by two mechanisms:[1]
Sensitization of cough receptors by increased levels of inflammatory mediators, such as, bradykinin, tachykinin, or prostaglandins. These sensitized cough receptors then cause an increased cough reflex
Stimulation of cough receptors through constriction of the bronchial smooth muscle.
Asthma as the cause of chronic dry cough has to be considered in patients who do not respond to empirical treatment for postnasal drip.[12] Spirometry is the most reliable test for establishing the diagnosis of asthma.[13] Bronchoprovocation tests can be considered in patients who may not have demonstrable airflow obstruction on spirometry. Bronchoprovocation tests are most commonly done by direct methods using methacholine or histamine. A negative methacholine challenge test excludes the diagnosis of cough-variant asthma, while the positive predictive value is reported to be 78-88%.[14] Use of objective tests, such as raised sputum eosinophil count or increased exhaled nitric oxide (NO) concentration are important for establishing diagnosis of cough-variant asthma.[1] Non-asthmatic eosinophilic bronchitis (NAEB) also presents in a similar manner. Patients with NAEB present with cough and sputum eosinophilia. However, the major characteristic distinguishing asthma from NAEB is the absence of variable airflow obstruction and bronchial hyperresponsiveness.[10]
In the absence of objective tests, a trial of inhaled corticosteroids should be considered in patients with unexplained chronic cough in order to rule out asthma and NAEB.[10] Additional treatment options for patients with cough-variant asthma include long-acting bronchodilators, antileukotrienes, and/or low-dose theophylline. A trial of oral corticosteroids (30 mg of prednisolone for 14 days) may be an option for selected patients with severe and/or refractory asthmatic cough.[10] Patients with NAEB have a good response to inhaled corticosteroids, but not to bronchodilators.[10] Patients with chronic cough and NAEB may not be diagnosed due to lack of sputum eosinophil testing.
Gastroesophageal reflux disease
Gastroesophageal reflux disease is reported as a cause of chronic cough in as many as 40% of the patients.[15,16] Hence, it is necessary to consider GERD as a cause of chronic cough in patients who also complain of typical and frequent gastrointestinal symptoms, such as, heartburn and regurgitation.[10]
Gastroesophageal reflux disease-associated cough has been postulated to occur through three major mechanisms: (a) Intraesophageal reflux (stimulation of the esophageal-tracheobronchial cough reflex), (b) laryngopharyngeal reflux, and (c) microaspiration. Each of these three mechanisms may act directly by triggering cough events or indirectly by sensitization of the cough reflex.[16] The vagally-mediated esophageal-tracheobronchial cough reflex is the major mechanism responsible for GERD-associated cough.[15] Occurrence of classical reflux symptoms such as heartburn, acid regurgitation, water brash, and so on, are not common in chronic cough patients and cough may be the sole presenting manifestation of GERD.[15] It has been reported that in up to 75% of the cases, patients with GERD-related cough may present with no gastrointestinal symptoms.[17] This makes GERD more difficult to diagnose.
Studies utilizing the impedance-pH monitoring of reflux events and objective cough recording have indicated a temporal relationship between reflux events and cough.[18] Recent studies have reported that in a considerable number of chronic cough patients (20-48%), cough succeeds reflux more frequently than expected by chance.[18,19,20] Furthermore, the pH of the reflux events preceding cough is irrelevant, as events of pH >4 are found to be as important as those with pH <4.[18] Definitive evidence confirming a causal link between cough and reflux events are lacking.[18]
The management of chronic cough associated with GERD includes: anti-reflux diet and lifestyle changes, a prokinetic agent (e.g. metoclopramide), and an acid suppressant with a proton pump inhibitor (PPI).[10] Although the effectiveness of acid-suppressive therapy has been questioned in a meta-analysis and recent studies, the therapeutic benefit of this therapy in patients with chronic cough cannot be dismissed, and hence, use of PPI is still considered for patients with evidence of pathological esophageal acid exposure and/or reflux esophagitis.[18,21]
New considerations in chronic cough management
The growing numbers of patients with unexplained cough, who are resistant to treatment, and evidences of a large number of patients with UACS, GERD, and asthma, who do not complain of cough at all, indicates that these diseases are not fundamental in the etiology of cough.[17] Furthermore, significant progress in the field of cough during the past decade has identified a number of conditions associated with unexplained chronic cough.
Non-acid reflux and chronic cough
The importance of non-acid reflux events in chronic cough has been highlighted in several studies.[22,23,24,25,26] These studies have reported that a subgroup of patients with chronic cough have failed to respond to intense acid suppression treatment and improved chronic cough after antireflux surgery, suggesting the involvement of a non-acidic gastric component in the refluxate. Hence, there is a need for a more careful workup in patients with chronic cough suspected to be due to GERD.[27,28]
Chronic cough due to non-acid reflux causes a hypersensitive cough reflex, possibly by stimulation of the neurogenic airway inflammation and mast cell activation.[29]
Impedance-pH monitoring is a powerful tool that helps in detecting acid and non-acid reflux events in patients on PPI therapy.[28] The current treatment approaches are limited; however, therapeutic options for non-acid GERD are largely dietary modifications, prokinetic drug therapy, and antireflux surgery in selected patients.[30]
Laryngopharyngeal reflux and cough
The concept of laryngopharyngeal reflux (LPR) causing upper airway symptoms has gained increased attention in recent years.[31] Although it is widely considered as a common cause of chronic cough among otolaryngologists, it has yet to gain widespread recognition among pulmonologists.
Laryngopharyngeal reflux does not have any specific pathognomonic symptoms, signs, or endoscopic findings.[30] Generally, the diagnosis of LPR is based on the laryngoscopic findings of erythema, edema, and thickening of the posterior pharynx.[30] However, these findings are also very common in patients with trauma due to cough, and hence, it is difficult to differentiate between these two conditions.[30] Limited evidence supports the use of PPIs in patients with cough due to LPR.[30] However, there is a need to establish a temporal relationship between LPR and cough with pharyngeal impedance monitoring and randomized controlled trials of PPIs.[30,32]
Sleep apnea and chronic cough
In recent times, obstructive sleep apnea (OSA) is being increasingly recognized as a cause of chronic cough.[33] Several recent studies have suggested a possible association between chronic cough and obstructive apnea, with a reported prevalence of 33 and 44%, in two different studies.[34] Although the exact mechanism of cough in patients with OSA is unclear, there are two proposed mechanisms: First is an increase in trans-diaphragmatic pressure during apnea episodes, which causes lower esophageal sphincter insufficiency leading to GERD. Another potential mechanism is cough that results from upper airway inflammation secondary to epithelial injury, associated with snoring and apnea.[35] A trial of continuous positive airway pressure therapy is reported to reduce or resolve the cough in patients with OSA.[35]
Vocal cord dysfunction and chronic cough
Patients with vocal cord dysfunction commonly experience stridor and dysphonia, owing to episodic, uncontrollable narrowing of the cords during inspiration. These patients also occasionally experience dyspnea and cough.[36] The diagnosis of vocal cord dysfunction can be made with the use of direct laryngoscopy and flattening of the inspiratory flow-volume loop on spirometry.[28] In acute cases, continuous positive airway pressure can be used to treat vocal cord dysfunction, while in longer-term voice therapy, psychological counseling along with reassurance, irritant avoidance, and supportive care are useful.[36] Evidences suggest that a number of patients with vocal cord dysfunction are commonly misdiagnosed with asthma, and hence, receive overtreatment with inhaled corticosteroids.[37] Hence, a careful management of vocal cord dysfunction is crucial.
Cough hypersensitivity syndrome: The new paradigm
The term ‘cough hypersensitivity syndrome’ views chronic cough from a more mechanistic standpoint. In this view, chronic cough is considered as a single syndrome with a common intrinsic mechanism of cough hypersensitivity. Furthermore, common diseases, such as rhinitis, eosinophilic bronchitis, asthma or gastroesophageal acidic refluxes are believed to be triggers rather than causes.[27] There is increased expression of cough receptors in the airways of patients with cough.[35] The important features of the cough hypersensitivity syndrome are depicted in Table 1.[35]
Table 1.
Important features of the cough hypersensitivity syndrome
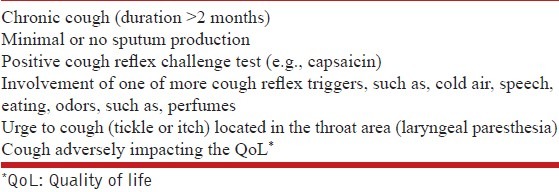
It has been expected that the new concept of ‘cough hypersensitivity’ may be useful in several ways. It may fill a gap that has occurred in the relationships between previous ‘common etiologies’ and chronic cough, help in reducing the unnecessary classifications of overlapping and similar diseases, as well as help in the discovery of biomarkers and develop newer indications for traditional therapeutic agents.[38]
Advances in cough outcome measures
Of late, developments of objective ambulatory cough monitoring systems and subjective quality of life questionnaires, along with well-established tools, such as, cough diary scores and visual analog scales, have improved the assessment of chronic cough.[35]
The three well-validated, cough-specific, quality-of-life questionnaires in adults include: The Leicester Cough Questionnaire (LCQ), the Cough-specific Quality of Life Questionnaire (CQLQ), and the Adverse Cough Outcome Survey (ACOS).[35,39] Several studies have shown that these instruments have fair-to-moderate correlation with other cough measurement tools, such as, cough frequency logs, tussigenic challenges, electronic recordings or other quality-of-life questionnaires.[39] Other cough-specific, quality-of-life questionnaires developed include, the Chronic Cough Impact Questionnaire (CCIQ) and the Cough and Sputum Assessment Questionnaire (CASA-Q). Although these instruments have shown good internal consistency, extensive comparison with objective cough measures have not been made.[39] Another validated instrument specifically developed for the pediatric population includes the Parent Cough-specific Quality-of-Life questionnaire (PC-QOL). It has shown good internal consistency and a strong correlation with the other subjective and objective cough measurement tools.[39]
In recent years, advances in sound recording devices and improved battery life have allowed the development of a number of cough monitoring devices, which include, Leicester Cough Monitor (LCM) and the VitaloJak and coughcount.[35] The Leicester Cough Monitor comprises of an MP3 recorder and a microphone. It measures the 24-hour cough frequency in the patients’ own environment. The reported sensitivity and specificity of LCM are 91 and 99%, respectively, for detecting cough in patients with chronic cough.[40] The VitaloJak is a semi-automated 24-hour ambulatory sound-based cough monitoring system that requires manual analysis of cough recordings.[41] The coughcount is an automated, sound-based cough monitoring system. However, it has not been validated in patients with chronic cough.[35] Several recent clinical trials have shown the feasibility of using this technology to assess outcomes with drug therapy and it is expected that positive cough monitoring data may provide strong support for the efficacy of antitussive drugs in future.[35]
Importance of antitussive agents
Antitussive therapies should be considered in patients with chronic dry cough when the cause of the increased cough reflex is unexplained and treatment against the potential aggravating factors is not satisfactory.[42] Antitussives can be categorized as acting centrally or peripherally. The common centrally acting antitussive agents used in clinical practice include codeine, pholcodine, dextromethorphan, methadone, and morphine. They exhibit their action directly on the cough center in the brain and decrease the nerve impulse discharges to the muscles that produce cough. Peripherally acting antitussives may inhibit the responsiveness of the afferent or efferent nerves of the cough reflex that evoke cough.[43] Peripherally acting agents are further grouped as demulcents, local anesthetics (lidocaine, benzocaine, hexylcaine hydrochloride, and tetracaine), and humidifying aerosols.[44]
In India, several cough formulations are available. Most antitussives are combinations of dextromethorphan or codeine, with antihistamines, expectorants, decongestants, and/or antipyretics. These antitussives are useful in the symptomatic relief of dry or non-productive cough. Codeine is one of the most commonly preferred centrally acting cough suppressants. Its efficacy has been proven in animal models[45,46,47] and also in humans,[48,49] where it suppresses artificially induced, disease-related, and unexplained chronic cough. In addition to its antitussive property, codeine has analgesic and sedative effects, which may be useful in relieving painful cough.[44] Dextromethorphan has also been shown to be effective in suppressing cough in animal models as well as in humans.[44] It is non-addictive and does not depress respiration in the usual doses. However, it has no significant analgesic or sedative properties. Pholcodine has a comparable efficacy to codeine, with a longer duration of action and an equivalent or safer toxicity profile.[50]
CONCLUSION
Chronic cough remains a distressing condition both physically and psychologically and can sometimes lead to serious complications. Chronic cough has been commonly considered to be caused by gastroesophageal reflux, postnasal drip or asthma. However, recent evidence suggests that many patients with these conditions do not have cough, and in those with cough, the response to specific treatments for these conditions is unpredictable at best. In addition, many chronic cough patients do not have an identifiable cause. This raises questions about the concept of a triad of treatable causes for chronic cough. During the past decade, significant progress in the field of cough has identified a number of conditions associated with unexplained chronic cough. Furthermore, it has been found that a heightened cough reflex is the key feature in a majority of the patients with chronic cough, and hence, chronic cough is recognized as a unique entity - ‘cough hypersensitivity’. Development of objective ambulatory cough monitoring systems and subjective quality-of-life questionnaires, along with well-established tools, such as, cough diary scores and visual analog scales have improved the assessment of chronic cough.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Singh S, Singh V. Combating cough-etiopathogenesis. J Assoc Physicians India. 2013;61(Suppl 5):6–7. [PubMed] [Google Scholar]
- 2.Simpson CB, Amin MR. Chronic cough: State-of-the-art review. Otolaryngol Head Neck Surg. 2006;134:693–700. doi: 10.1016/j.otohns.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 3.Rai SP. Chronic cough. J Assoc Physicians India. 2013;61(Suppl 5):28–30. [PubMed] [Google Scholar]
- 4.Iyer RK, Joshi JM. Future drugs for the treatment of dry cough. J Assoc Physicians India. 2013;61(Suppl 5):14–6. [PubMed] [Google Scholar]
- 5.Chung KF, McGarvey L, Mazzone SB. Chronic cough as a neuropathic disorder. Lancet Respir Med. 2013;1:414–22. doi: 10.1016/S2213-2600(13)70043-2. [DOI] [PubMed] [Google Scholar]
- 6.Pacheco A, Cobeta I, Wagner C. Refractory chronic cough: New perspectives in diagnosis and treatment. Arch Bronconeumol. 2013;49:151–7. doi: 10.1016/j.arbres.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 7.McGarvey LP. Does idiopathic cough exist? Lung. 2008;186(Suppl 1):S78–81. doi: 10.1007/s00408-007-9048-4. [DOI] [PubMed] [Google Scholar]
- 8.Pratter MR. Overview of common causes of chronic cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(Suppl 1):59S–62S. doi: 10.1378/chest.129.1_suppl.59S. [DOI] [PubMed] [Google Scholar]
- 9.Pratter MR. Chronic upper airway cough syndrome secondary to rhinosinus diseases (previously referred to as postnasal drip syndrome): ACCP evidence-based clinical practice guidelines. Chest. 2006;129(Suppl 1):63S–71S. doi: 10.1378/chest.129.1_suppl.63S. [DOI] [PubMed] [Google Scholar]
- 10.Bartziokas K, Papadopoulos A, Kostikas K. The never-ending challenge of chronic cough in adults: A Review for the Clinician. Pneumon. 2012;25:164–75. [Google Scholar]
- 11.McGarvey LP, Elder J. Future directions in treating cough. OtolaryngolClin North Am. 2010;43:199–211, xii. doi: 10.1016/j.otc.2009.11.011. [DOI] [PubMed] [Google Scholar]
- 12.Irwin RS, Baumann MH, Bolser DC, Boulet LP, Braman SS, Brightling CE, et al. American College of Chest Physicians (ACCP). Diagnosis and management of cough executive summary: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(Suppl 1):1S–23S. doi: 10.1378/chest.129.1_suppl.1S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yawn BP. Differential assessment and management of asthma vs chronic obstructive pulmonary disease. Medscape J Med. 2009;11:20. [PMC free article] [PubMed] [Google Scholar]
- 14.Morice AH, McGarvey L, Pavord I. British Thoracic Society Cough Guideline Group. Recommendations for the management of cough in adults. Thorax. 2006;61(Suppl 1):i1–24. doi: 10.1136/thx.2006.065144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Makkar RP, Sachdev GK. Chronic unexplained cough and gastroesophageal reflux disease: A quick clinical review. The Internet Journal of Internal Medicine. 2003;4:1–4. [Google Scholar]
- 16.Smith J, Woodcock A, Houghton L. New developments in reflux-associated cough. Lung. 2010;188(Suppl 1):S81–6. doi: 10.1007/s00408-009-9210-2. [DOI] [PubMed] [Google Scholar]
- 17.Woodcock A, Young EC, Smith JA. New insights in cough. Br Med Bull. 2010;96:61–73. doi: 10.1093/bmb/ldq034. [DOI] [PubMed] [Google Scholar]
- 18.Kahrilas PJ, Smith JA, Dicpinigaitis PV. A causal relationship between cough and gastroesophageal reflux disease (GERD) has been established: A pro/con debate. Lung. 2014;192:39–46. doi: 10.1007/s00408-013-9528-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sifrim D, Dupont L, Blondeau K, Zhang X, Tack J, Janssens J. Weakly acidic reflux in patients with chronic unexplained cough during 24 hour pressure, pH, and impedance monitoring. Gut. 2005;54:449–54. doi: 10.1136/gut.2004.055418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Blondeau K, Dupont LJ, Mertens V, Tack J, Sifrim D. Improved diagnosis of gastro-oesophageal reflux in patients with unexplained chronic cough. Aliment Pharmacol Ther. 2007;25:723–32. doi: 10.1111/j.1365-2036.2007.03255.x. [DOI] [PubMed] [Google Scholar]
- 21.Kahrilas PJ, Howden CW, Hughes N, Molloy-Bland M. Response of chronic cough to acid-suppressive therapy in patients with gastroesophageal reflux disease. Chest. 2013;143:605–12. doi: 10.1378/chest.12-1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Allen CJ, Anvari M. Gastro-oesophageal reflux related cough and its response to laparoscopic fundoplication. Thorax. 1998;53:963–8. doi: 10.1136/thx.53.11.963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Irwin RS, Zawacki JK, Wilson MM, French CT, Callery MP. Chronic cough due to gastrooesophageal reflux disease: Failure to resolve despite total/near-total elimination of esophageal acid. Chest. 2002;121:1132–40. doi: 10.1378/chest.121.4.1132. [DOI] [PubMed] [Google Scholar]
- 24.Duffy JP, Maggard M, Hiyama DT, Atkinson JB, McFadden DW, Ko CY, et al. Laparoscopic Nissen fundoplication improves quality of life in patients with atypical symptoms of gastroesophageal reflux. Am Surg. 2003;69:833–8. [PubMed] [Google Scholar]
- 25.Allen CJ, Anvari M. Does laparoscopic fundoplication provide long-term control of gastrooesophageal reflux related cough? Surg Endosc. 2004;18:633–7. doi: 10.1007/s00464-003-8821-6. [DOI] [PubMed] [Google Scholar]
- 26.Mainie I, Tutuian R, Agrawal A, Hila A, Highland KB, Adams DB, et al. Fundoplication eliminates chronic cough due to non-acid reflux identified by impedancepH monitoring. Thorax. 2005;60:521–3. doi: 10.1136/thx.2005.040139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McGarvey LP. Idiopathic chronic cough: A real disease or a failure of diagnosis? Cough. 2005;1:9. doi: 10.1186/1745-9974-1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Storr MA. What is nonacid reflux disease? Can J Gastroenterol. 2011;25:35–8. doi: 10.1155/2011/626752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Qiu Z, Yu L, Xu S, Liu B, Zhao T, Lü H, et al. Cough reflex sensitivity and airway inflammation in patients with chronic cough due to non-acid gastro-oesophageal reflux. Respirology. 2011;16:645–52. doi: 10.1111/j.1440-1843.2011.01952.x. [DOI] [PubMed] [Google Scholar]
- 30.Birring SS. Controversies in the evaluation and management of chronic cough. Am J Respir Crit Care Med. 2011;183:708–15. doi: 10.1164/rccm.201007-1017CI. [DOI] [PubMed] [Google Scholar]
- 31.Smith JA, Houghton LA. The oesophagus and cough: Laryngo-pharyngeal reflux, microaspiration and vagal reflexes. Cough. 2013;9:12. doi: 10.1186/1745-9974-9-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Reimer C, Bytzer P. Management of laryngopharyngeal reflux with proton pump inhibitors. Ther Clin Risk Manag. 2008;4:225–33. doi: 10.2147/tcrm.s6862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Faruqi S, Fahim A, Morice AH. Chronic cough and obstructive sleep apnoea: Reflux-associated cough hypersensitivity? Eur Respir J. 2012;40:1049–50. doi: 10.1183/09031936.00025012. [DOI] [PubMed] [Google Scholar]
- 34.Wang TY, Lo YL, Liu WT, Lin SM, Lin TY, Kuo CH, et al. Chronic cough and obstructive sleep apnoea in a sleep laboratory-based pulmonary practice. Cough. 2013;9:24. doi: 10.1186/1745-9974-9-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Birring SS. New concepts in the management of chronic cough. Pulm Pharmacol Ther. 2011;24:334–8. doi: 10.1016/j.pupt.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 36.Kwan B, Goh C. Managing cough in adults: Is there a serious underlying cause? Med Today. 2012;13:39–46. [Google Scholar]
- 37.Kenn K, Balkissoon R. Vocal cord dysfunction: What do we know? EurRespir J. 2011;37:194–200. doi: 10.1183/09031936.00192809. [DOI] [PubMed] [Google Scholar]
- 38.Song WJ, Chang YS, Morice AH. Changing the paradigm for cough: Does ‘cough hypersensitivity’aid our understanding? Asia Pac Allergy. 2014;4:3–13. doi: 10.5415/apallergy.2014.4.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McCrory DC, Coeytaux RR, Yancy WS, Jr, Schmit KM, Kemper AR, Goode A, et al. Assessment and Management of Chronic Cough. Rockville, MD: Agency for Healthcare Research and Quality (US); 2013. [PubMed] [Google Scholar]
- 40.Birring SS, Fleming T, Matos S, Raj AA, Evans DH, Pavord ID. The leicester cough monitor: Preliminary validation of an automated cough detection system in chronic cough. Eur Respir J. 2008;31:1013–8. doi: 10.1183/09031936.00057407. [DOI] [PubMed] [Google Scholar]
- 41.Smith JA, Decalmer S, Kelsall A, McGuinness K, Jones H, Galloway S, et al. Acoustic cough-reflux associations in chronic cough: Potential triggers and mechanisms. Gastroenterology. 2010;139:754–62. doi: 10.1053/j.gastro.2010.06.050. [DOI] [PubMed] [Google Scholar]
- 42.Pavord ID, Chung KF. Management of chronic cough. Lancet. 2008;371:1375–84. doi: 10.1016/S0140-6736(08)60596-6. [DOI] [PubMed] [Google Scholar]
- 43.Reynolds SM, Mackenzie AJ, Spina D, Page CP. The pharmacology of cough. Trends Pharmacol Sci. 2004;25:569–76. doi: 10.1016/j.tips.2004.09.009. [DOI] [PubMed] [Google Scholar]
- 44.Padma L. Current drugs for the treatment of dry cough. J Assoc Physicians India. 2013;61(Suppl 5):9–13. [PubMed] [Google Scholar]
- 45.May AJ, Widdicombe JG. Depression of the cough reflex by pentobarbitone and some opium derivatives. Br J Pharmacol Chemother. 1954;9:335–40. doi: 10.1111/j.1476-5381.1954.tb01689.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chou D, Wang SC. Studies on the localization of central cough mechanism: Site of action of antitussive drugs. J Pharmacol Exp Ther. 1975;194:499–505. [PubMed] [Google Scholar]
- 47.Bolser DC, Hey JA, Chapman RW. Influence of central antitussive drugs on the cough motor pattern. J Appl Physiol (1985) 1999;86:1017–24. doi: 10.1152/jappl.1999.86.3.1017. [DOI] [PubMed] [Google Scholar]
- 48.Sevelius H, McCoy JF, Colmore JP. Dose response to codeine in patients with chronic cough. Clin Pharmacol Ther. 1971;12:449–55. doi: 10.1002/cpt1971123449. [DOI] [PubMed] [Google Scholar]
- 49.Sevelius H, Colmore JP. Objective assessment of antitussive agents in patients with chronic cough. J New Drugs. 1966;6:216–23. [PubMed] [Google Scholar]
- 50.Blanchard E, Tunon de Lara M. New insights into the role of pholcodine in the treatment of cough in 2013? Therapie. 2013;68:85–91. doi: 10.2515/therapie/2013019. [DOI] [PubMed] [Google Scholar]


