Abstract
Pirfenidone is an anti-fibrotic drug which has been approved for the management of patients with Idiopathic Pulmonary Fibrosis (IPF). However, its role in interstitial lung disease (ILD) due to other causes such as systemic sclerosis (SSc) is not clear. We present a case of a patient with SSc associated ILD who showed a subjective as well as objective improvement in lung function with pirfenidone.
Keywords: Interstitial lung disease, pirfenidone, systemic sclerosis
INTRODUCTION
Pirfenidone is an anti-fibrotic agent that has been approved for idiopathic pulmonary fibrosis (IPF) in Europe, Japan and India so far. There are scarce reports of its use in other fibrotic lung diseases, particularly other interstitial lung disease (ILD) associated with known causes like systemic sclerosis (SSc). We report the case of a patient with long-standing SSc-ILD who showed symptomatic and functional improvement after pirfenidone treatment.
CASE
Our patient is a 44-year-old lady who was diagnosed with systemic sclerosis (SSc) 15 years ago with tightening of facial skin, thickening of skin over the fingers and pitting of finger tips. She also had difficulty in swallowing. An anti-Scl-70 antibody was done which was positive. ANA was also strongly positive with a speckled pattern at a 1:1000 dilution. As per the 1980 American College of Rheumatology guidelines for diagnosing systemic sclerosis, the patient was diagnosed as having SSc (1 major and 2 minor criteria). In 2006, she presented with worsening breathlessness. In 2006, she was also diagnosed to have systemic sclerosis-interstitial lung disease (SSc-ILD) on the basis of bibasal crackles and an HRCT scan of the chest which was suggestive of a non-specific interstitial pneumonia (NSIP) pattern. Despite treatment with corticosteroids, cyclophosphamide and azathioprine for 5 years, there was a relentless worsening in her dyspnea. Her lung function gradually worsened as shown in Table 1 and Figure 1. The six minute walk distance (6MWD) also declined from 350 m in 2006 to 200 m in January 2011. The oxygen desaturation also increased with the oxygen saturation at the end of the 6 minutes’ walk dropping from 91% in 2006 to 85% in January 2011. Given the lack of response to “standard” treatment, and after discussion with the patient about off-label use of the drug, other treatments were stopped and pirfenidone (200 mg three times a day) was commenced as a compassionate use in March 2011. Treatment was well tolerated and lung function stabilized over the next year (forced vital capacity (FVC) 45%, diffusing capacity of lung for carbon monoxide (DLCO) 27% predicted). After 20 months of pirfenidone therapy, the patient was less symptomatic with improved effort tolerance and lung function showed a trend towards improvement (FVC 58% and DLCO 54% predicted) [Ref Table 1 and Figure 1]. The 6MWD in November 2012 improved up to 300 meters. The oxygen saturation at the end of six minutes' walk also improved to 90%. Serial chest HRCT scans also showed no further progression [Ref Figures 2–4]. Serial two-dimensional echocardiography over the past 6 years did not suggest the presence of pulmonary hypertension. The patient is currently on clinical and functional follow-up.
Table 1.
FVC and DLCO before and after starting pirfenidone
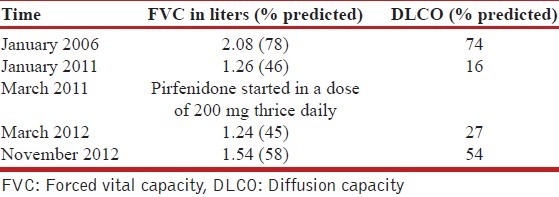
Figure 1.
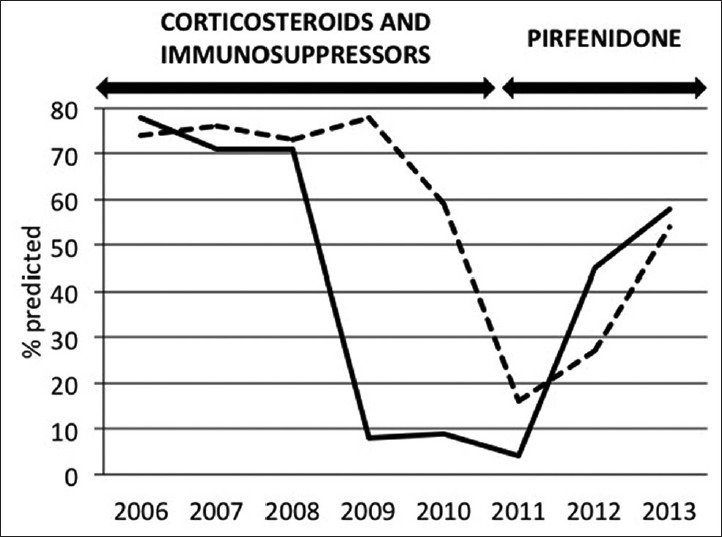
Lung function as measured by % predicted FVC (dotted line) and DLCO (solid line) -yearly measurements
Figure 2.
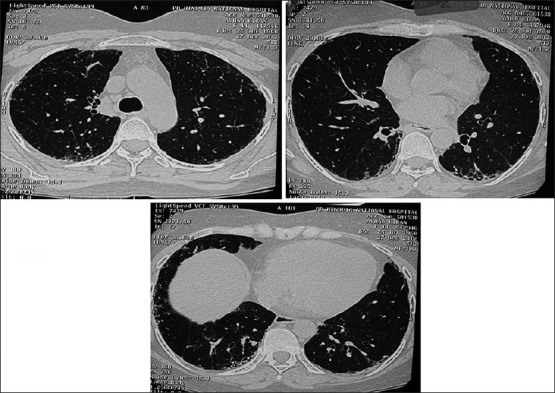
Pre-pirfenidone HRCT chest image 2008
Figure 4.
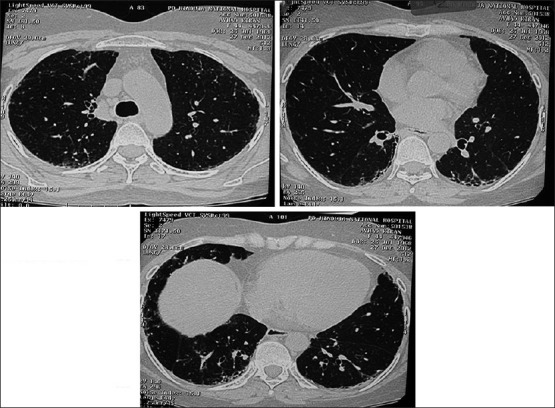
Post-pirfenidone HRCT chest image 2012
Figure 3.
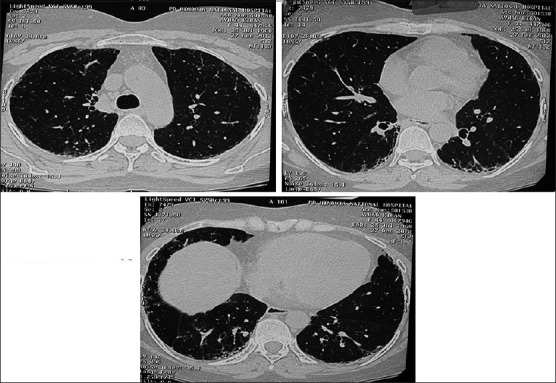
Pre-pirfenidone HRCT chest image 2010
DISCUSSION
Pulmonary fibrosis is the most common cause of mortality in patients with SSc surpassing scleroderma renal crisis, which has become a rarity following the advent of angiotensin-converting-enzyme (ACE) inhibitors. A number of pro-inflammatory and pro-fibrotic extracellular mediators which have been implicated in the pathogenesis of IPF may also play a role in SSc-ILD. The pivotal mediator of fibrosis is the multifunctional cytokine transforming growth factor-beta (TGF-β). Substantial evidence implicates TGF-β, along with platelet-derived growth factors, endothelin 1 and cytokines, in the pathogenesis of SSc.[1] Hence, targeting the TGF-β activated pathway may be a rational strategy in the treatment of SSc-ILD. Pirfenidone, which has known anti-inflammatory, anti-fibrogenic and antioxidant properties, has been shown to reduce fibroblast proliferation and inhibit TGF-β-stimulated collagen production.[2]
We describe here an SSc-ILD patient, who clearly showed a reversal in lung function deterioration after initiation of pirfenidone. Miura and colleagues reported improvement of lung function after pirfenidone treatment in three Japanese patients with SSc-ILD. They suggested that pirfenidone might be a useful treatment option in such patients.[3] Nagai and colleagues also showed that pirfenidone had a stabilizing effect on the course of 10 patients with chronic progressive pulmonary fibrosis, 2 of which were SSc-ILD cases.[4]
There is no consensus on the appropriate dose of pirfenidone in IPF. The CAPACITY trials[5] showed that 2403 mg/day of pirfenidone was the most effective although a smaller dose of 1197 mg/day also slowed the decline in FVC. In Nagai's study[4] the dose of pirfenidone used was about 40 mg/kg/day. In our patient, we used a lower dose of pirfenidone of 200 mg three times a day and continued the same without increasing as the patient had stabilized clinically and functionally on that dose.
The above-mentioned reports, together with the present one, suggest that pirfenidone should be investigated in properly designed prospective trials as a treatment for patients with progressive SSc-ILD.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Varga J, Abraham D. Systemic sclerosis: A prototypic multisystem fibrotic disorder. J Clin Invest. 2007;117:557–67. doi: 10.1172/JCI31139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Oku H, Shimizu T, Kawabata T, Nagira M, Hikita I, Ueyama A, et al. Antifibrotic action of pirfenidone and prednisolone: Different effects on pulmonary cytokines and growth factors in bleomycin-induced murine pulmonary fibrosis. Eur J Pharmacol. 2008;590:400–8. doi: 10.1016/j.ejphar.2008.06.046. [DOI] [PubMed] [Google Scholar]
- 3.Miura Y, Tsunoda Y, Tanaka T, Takoi H, Yatagai Y, Rin S, et al. The efficacy of pirfenidone in scleroderma related interstitial lung disease. Eur Respir J. 2012;40(Suppl 56):P3652. [Google Scholar]
- 4.Nagai S, Hamada K, Shigematsu M, Taniyama M, Yamauchi S, Izumi T. Open-label compassionate use one year-treatment with pirfenidone to patients with chronic pulmonary fibrosis. Intern Med. 2002;41:1118–23. doi: 10.2169/internalmedicine.41.1118. [DOI] [PubMed] [Google Scholar]
- 5.Noble PW, Albera C, Bradford WZ, Costabel U, Glassberg MK, Kardatzke D, et al. CAPACITY Study Group. Pirfenidone in patients with idiopathic pulmonary fibrosis (CAPACITY): Two randomised trials. Lancet. 2011;377:1760–9. doi: 10.1016/S0140-6736(11)60405-4. [DOI] [PubMed] [Google Scholar]


