Abstract
Uncontrolled diabetes mellitus is associated with a variety of infections which pose management difficulties. Herein, we report a case of diabetic patient who developed combined pulmonary tuberculosis and mucormycosis. The case illustrates management of this rare co-infection which despite being potentially fatal was treated successfully.
Keywords: Diabetes mellitus, pulmonary tuberculosis, mucormycosis
INTRODUCTION
Mucormycosis is a potentially fatal necrotizing fungal infection having propensity to affect immunocompromised hosts. Diabetes has been reported as a predisposing factor in at least 36% cases of mucormycosis.[1] Also, diabetics are 2-3 times more prone to develop pulmonary tuberculosis,[2] with high chances of treatment failure.[3] Herein, we report a case of combined infection of pulmonary tuberculosis and mucormycosis in a diabetic patient. Even though isolated infections have known to occur but such co-existent diseases in diabetes, with successful outcome, has not yet been reported. In view of common clinical and radiological features, this co-infection is a diagnostic dilemma for treating physician.
CASE HISTORY
A-30-year male presented with complaints of right-sided chest pain, progressive shortness of breath, low-grade fever and productive cough of three weeks duration. He was a non-smoker and had poorly controlled diabetes for last three years. He had also taken complete anti-tubercular treatment for pulmonary tuberculosis two years back.
On examination, patient was tachypnoic with respiratory rate of 35/min, hemodynamically stable and afebrile. Chest auscultation revealed decreased breath sounds over right hemithorax with hyper-resonant percussion note. Chest radiograph revealed right-sided pneumothorax along with heterogenous opacity in left mid-zone [Figure 1]. Right intercostal tube drainage was performed which improved patient's distress [Figure 2]. Hematological investigations revealed mild leukocytosis of 12,200 cells/μl with 82% neutrophils. Blood sugar levels were markedly deranged with serial levels between 200-360 mg/dl. He was non-reactive for human immunodeficiency virus (HIV) and sputum was positive for acid-fast bacilli. The KOH wet mount of sputum showed broad sparsely non-septate thin-walled hyphae with right-angle branching, characteristic of mucormycetes. Subsequently, fungal culture showed the growth of Lichtheimia corymbifera [Figure 3].
Figure 1.
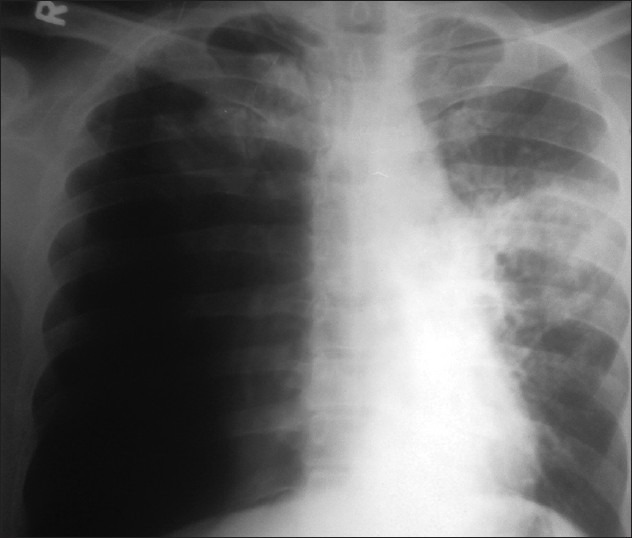
X-ray of the chest showing right side pneumothorax along with left mid-zone non-homogenous opacity undergoing cavitation
Figure 2.
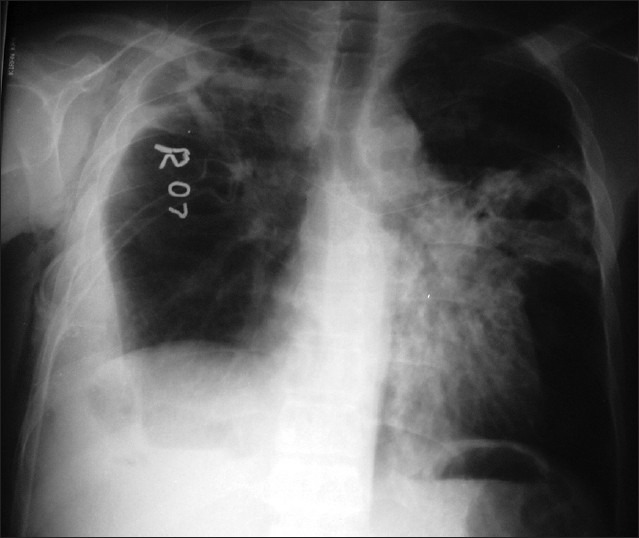
X-ray of the chest shows blunting of right costophrenic angle with intercostal tubein situalong with left mid-zone lung abscess and surrounding consolidation
Figure 3.
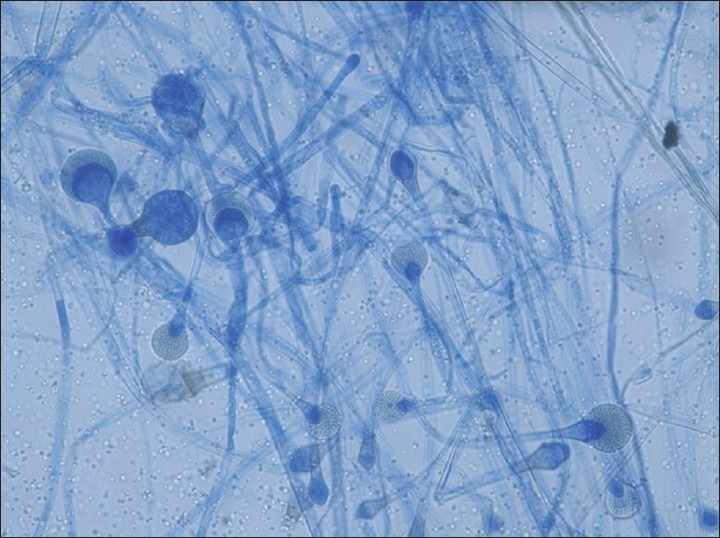
LCB mount showing sporangium, apophyses, conidiophores of Lichtheimia corymbifera(LCB-X 200)
Patient was started on anti-tubercular treatment consisting of five drugs under Revised National Tuberculosis Control Program. Intravenous liposomal amphotericin B (dose - 2 mg/kg/day) was initiated simultaneously along with adequate hydration. Glycemic control was achieved with subcutaneous regular insulin. Patient tolerated the antifungal treatment and started showing gradual improvement. Fever subsided in three weeks time. Amphotericin B was discontinued at the end of 8th week, after obtaining negative sputum culture and ensuring clinical improvement. Patient completed eight months of anti-tubercular treatment and is on regular follow-up with satisfactory improvement [Figure 4].
Figure 4.

X-ray of the chest shows a small pocket of right-sided pneumothorax and thick fibrotic band in left mid-zone, likely healed lesion
DISCUSSION
By impairing innate and adaptive immunity, diabetes mellitus predisposes to a variety of infections, sometimes due to unusual organisms. Mucormycosis is one such uncommon but prognostically important, opportunistic infection caused by ubiquitous filamentous fungus like Rhizopus, Mucor, and Lichtheimia species of the order Mucorales. These vasotropic fungi lead to a wide severity of rhinosinocerebral, pulmonary and disseminated infections,[4,5] causing extensive tissue necrosis. Pulmonary involvement with mucormycosis usually occurs in severe immunosuppression and often mimics aspergillosis[5] and tuberculosis.[6] Understandably, co-infection with mucormycosis and tuberculosis, as in our case, is liable to create management difficulties. This dreaded co-infection has scarcely been reported as isolated case reports in post-stem cell transplantation[7] and acute myeloid leukemia.[8]
Like tuberculosis, pulmonary mucormycosis presents with prolonged and refractory fever, cough, hemoptysis and chest pain.[5] In a tuberculosis endemic country, these non-specific symptoms are very often attributed to pulmonary tuberculosis. Compounding the problem, mucormycosis present as parenchymal infiltrates, consolidation, nodules, cavitation, effusion etc., on imaging, similar to tuberculosis.[9] Microbial culture and/or histopathology is the gold standard for diagnosis of both diseases.[10] However, its usefulness is hampered by factors like time lapse for diagnosis, need for sterile tissue (which necessitates invasive procedure) and low diagnostic yield (less than 50%).[11,12] Sputum or bronchoalveolar lavage fluid cultures are usually non-diagnostic but provide suggestive diagnosis, requiring further confirmation.[13] In our case as well, mucormycosis confirmation could not be done as the patient was unfit to undergo invasive tissue sampling. Considering his underlying condition and the fatality of untreated mycosis, patient was started on antifungal treatment. Quite often, suspected patients of pulmonary mucormycosis fail to undergo invasive diagnostic testing. Subjecting such patients to antifungal therapy is a matter of further discussion and evaluation.
Although, there are no consensus treatment guidelines for mucormycosis, currently, the recommended antifungal therapy includes conventional or liposomal amphotericin B.[14] The duration of therapy is highly individualized and determined by clinical response, normalization of x-ray findings and negative culture/biopsy.[10] Co-infection with tuberculosis should be treated simultaneously, though it may increase likelihood of drug interactions, side-effects and non-compliance to treatment. Recovery from immunosuppression is of utmost importance for successful outcome. Despite medical and surgical treatment, mortality rates as high as 70% are seen in invasive pulmonary mucormycosis.[1] Co-infection with tuberculosis is likely to increase the overall mortality depending on host factors, disease stage and time of initiation of treatment.
In view of rising burden of mucormycosis, incidence of such mixed infections is likely to increase in future.[15] High index of suspicion and comprehensive screening of diabetics and possibly all immunocompromised patients for possible co-infections is pertinent even if a single agent has been isolated. Once considered fatal, diagnosis of mucormycosis should not be considered a lost battle. Early diagnosis and aggressive treatment is the key to successful outcome.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Roden MM, Zaoutis TE, Buchanan WL, Knudsen TA, Sarkisova TA, Schaufele RL, et al. Epidemiology and outcome of zygomycosis: A review of 929 reported cases. Clin Infect Dis. 2005;41:634–53. doi: 10.1086/432579. [DOI] [PubMed] [Google Scholar]
- 2.Jeon CY, Murray MB. Diabetes mellitus increases the risk of active tuberculosis: A systematic review of 13 observational studies. PLoS Med. 2008;5:e152. doi: 10.1371/journal.pmed.0050152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alisjahbana B, Sahiratmadja E, Nelwan EJ, Purwa AM, Ahmad Y, Ottenhoff TH, et al. The effect of type 2 diabetes mellitus on the presentation and treatment response of pulmonary tuberculosis. Clin Infect Dis. 2007;45:428–35. doi: 10.1086/519841. [DOI] [PubMed] [Google Scholar]
- 4.Gonzalez CE, Rinaldi MG, Sugar AM. Zygomycosis. Infect Dis Clin North Am. 2002;16:895–914. doi: 10.1016/s0891-5520(02)00037-5. [DOI] [PubMed] [Google Scholar]
- 5.Petrikkos G, Skiada A, Lortholary O, Roilides E, Walsh TJ, Kontoyiannis DP. Epidemiology and clinical manifestations of mucormycosis. Clin Infect Dis. 2012;54:S23–34. doi: 10.1093/cid/cir866. [DOI] [PubMed] [Google Scholar]
- 6.Garg R, Marak RS, Verma SK, Singh J, Sanjay, Prasad R. Pulmonary mucormycosis mimicking as pulmonary tuberculosis: A case report. Lung India. 2008;25:129–31. doi: 10.4103/0970-2113.59595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sharma SK, Agarwal N, Mukherjee A, Seth T, Mishra P, Xess I, et al. Coexisting pulmonary tuberculosis and mucormycosis in a patient with aplastic anemia post allogenic stem cell transplantation. Mediterr J Hematol Infect Dis. 2011;3:e2011036. doi: 10.4084/MJHID.2011.0036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miyamoto R, Hongo T, Takehiro A, Igarashi Y, Ueyama T, Harada Y, et al. A case of acute myelogenous leukemia complicated with pulmonary tuberculosis and pulmonary mucormycosis (author's transl) Rinsho Ketsueki. 1981;22:903–8. [PubMed] [Google Scholar]
- 9.Kanne JP, Yandow DR, Mohammed TL, Meyer CA. CT findings of pulmonary nocardiosis. AJR Am J Roentgenol. 2011;197:W266–72. doi: 10.2214/AJR.10.6208. [DOI] [PubMed] [Google Scholar]
- 10.Hamilos G, Samonis G, Kontoyiannis DP. Pulmonary mucormycosis. Semin Respir Crit Care Med. 2011;32:693–702. doi: 10.1055/s-0031-1295717. [DOI] [PubMed] [Google Scholar]
- 11.Ribes JA, Vanover-Sams CL, Baker DJ. Zygomycetes in human disease. Clin Microbiol Rev. 2000;13:236–301. doi: 10.1128/cmr.13.2.236-301.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Spellberg B, Edwards J, Jr, Ibrahim A. Novel perspectives on mucormycosis: Pathophysiology, presentation, and management. Clin Microbiol Rev. 2005;18:556–69. doi: 10.1128/CMR.18.3.556-569.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Glazer M, Nusair S, Breuer R, Lafair J, Sherman Y, Berkman N. The role of BAL in the diagnosis of pulmonary mucormycosis. Chest. 2000;117:279–82. doi: 10.1378/chest.117.1.279. [DOI] [PubMed] [Google Scholar]
- 14.Spellberg B, Walsh TJ, Kontoyiannis DP, Edwards J, Jr, Ibrahim AS. Recent advances in the management of mucormycosis: From bench to bedside. Clin Infect Dis. 2009;48:1743–51. doi: 10.1086/599105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gleissner B, Schilling A, Anagnostopolous I, Siehl I, Thiel E. Improved outcome of zygomycosis in patients with hematological diseases? Leuk Lymphoma. 2004;45:1351–60. doi: 10.1080/10428190310001653691. [DOI] [PubMed] [Google Scholar]


