Abstract
Background and Aim:
Several studies have reported the performance of combining endoscopic ultrasound fine-needle aspiration with an echobronchoscope (EUS-B-FNA), with endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA), for the diagnosis of mediastinal lymphadenopathy. Herein we report our initial experience with this technique.
Patients and Methods:
In this retrospective study, we report the outcome of patients who underwent EUS-B-FNA with or without EBUS-TBNA during the same session. Details of the lymph nodes sampled, number of passes, duration of the procedure, results of the cytological examination, and the final diagnosis of all the patients are presented.
Results:
Eleven patients underwent EUS-B-FNA during the study period. EUS-B-FNA and EBUS-TBNA together yielded a sensitivity and specificity of 72.7 and 100%, respectively. The number of lymph nodes sampled per patient and the number of passes per lymph node were significantly higher with EBUS-TBNA compared to EUS-B-FNA. The mean duration of procedure was also significantly higher in the EBUS-TBNA group. The most common reason (five patients (45.5%)) for resorting to EUS-B-FNA was the patient being unfit for EBUS-TBNA or the inability of the operator to complete the procedure. Sarcoidosis was the most frequent final diagnosis in the study patients (four cases), followed by bronchogenic carcinoma (three cases).
Conclusions:
EUS-B-FNA is a useful additional tool for the diagnosis of mediastinal lymphadenopathy. In combination with EBUS-TBNA, it has a fairly good diagnostic yield and is a good alternative in situations where EBUS-TBNA is not feasible.
Keywords: Bronchoscopy, EBUS, lung cancer, sarcoidosis, TBNA, transbronchial needle aspiration, tuberculosis
INTRODUCTION
Conventional transbronchial needle aspiration and mediastinoscopy have been the traditional methods to access mediastinal lymph nodes.[1,2,3,4] With the advent of the curved-array echoendoscope (endoscopic ultrasound (EUS)) followed by the convex probe echobronchoscope (endobronchial ultrasound (EBUS)), assessment of such lesions is now possible accurately, with minimally invasive techniques.[5,6,7,8] The combination of these procedures (so called complete ‘medical’ mediastinoscopy) has become the standard of care for the staging of lung cancer.[9,10,11] These techniques are complementary to each other in their access to different parts of the mediastinum.[12] However, EBUS-TBNA is mostly performed by pulmonary physicians or thoracic surgeons, while EUS-FNA generally lies in the domain of the gastroenterologist. Therefore, for patients requiring both procedures, waiting times and costs get amplified as they are performed by different physicians individually.
Transesophageal needle aspiration of the mediastinal lymph nodes using an echobronchoscope was first reported in 2007.[13] This procedure can be performed with the same echobronchoscope by the same operator during the same session as EBUS-TBNA, thus potentially reducing the costs and inconvenience to patients. Several studies have reported the utility of this technique, termed ‘endoscopic ultrasound with bronchoscope-guided fine-needle aspiration (EUS-B-FNA)’ for the diagnosis of sarcoidosis and lung cancer and mediastinal staging (and restaging) of bronchogenic carcinoma.[14,15,16,17,18] Only one study from India has described the utility of the transesophageal use of EBUS in children, primarily for performing abdominal procedures.[19] Herein, we describe our experience of EUS-B-FNA in the first eleven patients, focusing on the technique and the reasons for performing this ‘unconventional’ procedure.
PATIENTS AND METHODS
Patients
This is a retrospective study of patients undergoing EUS-B-FNA between 1st January 2013 and 30th April 2014. A written informed consent was obtained from all patients for the performance of the procedure and the study was approved by the Ethics Review Committee. Patients presenting to the bronchoscopy suite of this institute with intrathoracic lymphadenopathy on computed tomography (CT) of the chest, and who underwent EUS-B-FNA (with or without EBUS-TBNA), were enrolled. Patients with any of the following were excluded: Pregnancy, deranged coagulation profile or failure to provide informed consent. All patients underwent detailed clinical evaluation, laboratory tests (complete blood count, coagulation profile, and liver and kidney function tests), chest radiograph, and CT of the chest.
Endobronchial ultrasound transbronchial needle aspiration procedure
The procedure was performed in the supine position, transorally, by pulmonary consultants experienced in the EBUS technique, as previously described.[20] Lymph node stations were categorized according to the International Association for the Study of Lung Cancer classification.[21,22] EBUS-TBNA was performed in spontaneously breathing patients under conscious sedation and analgesia (intravenous midazolam and pentazocine, in doses adequate to maintain sedation and cough suppression). Promethazine (25 mg) and atropine (0.6 mg) were administered intramuscularly, followed by nebulized 4% lignocaine immediately before the procedure. Topical lignocaine (10% solution) was sprayed over the oropharynx along with 2% lignocaine solution instilled over the vocal cords and the airways by the ‘spray-as-you-go’ technique.[2] The pulse rate, blood pressure, respiratory rate, and pulse oximetric saturation were monitored throughout the procedure. The convex probe EBUS scope (BF-UC 180F; Olympus Medical Systems, Japan) with a 7.5 MHz convex transducer and a compatible endoscopic ultrasound scanner (EU-ME1; Olympus Medical Systems, Japan) were used.
The lymph nodes were punctured using a disposable, 21-gauge needle (Vizishot, NA-201SX-4021 Olympus Medical Systems, Japan) under real-time sonographic and endoscopic visualization.[23] The aspirate thus obtained was expressed on to a glass slide by pushing air, using a 10 mL syringe. Both air-dried and fixed (95% ethanol) slides were prepared. On-site cytological assessment for adequacy of the aspirate was not available.
Endoscopic ultrasound fine-needle aspiration with an echobronchoscope procedure
Endoscopic ultrasound with bronchoscope-guided fine-needle aspiration was performed in the supine position by introducing the echobronchoscope through the mouth into the pharynx. After reaching the area posterior to the larynx, the bronchoscope was turned 180° to face the posterior pharyngeal wall, and advanced into the esophagus, with gentle manipulation. The scope was guided using vascular landmarks as there was limited endoscopic visualization due to the collapsed esophagus. The lymph nodes were mapped by their location in relation to the heart and intrathoracic vessels. Puncture of the lymph nodes and specimen processing were performed in a fashion similar to EBUS-TBNA.
Outcome
Details of the lymph nodes sampled, number of passes, and duration of procedure were recorded separately for EBUS-TBNA and EUS-B-FNA. The reason for performing EUS-B-FNA was documented for every patient. The results of cytological examination and final diagnosis of all patients were also noted.
Statistical analysis
Statistical analysis was performed using the commercial statistical package StatsDirect (Version 2.8.0, England, StatsDirect Ltd, 2005. http://www.statsdirect.com). Data were expressed as mean ± standard deviation (SD) or number with percentage. Differences between continuous variables in the two groups were compared using Mann-Whitney U test.
RESULTS
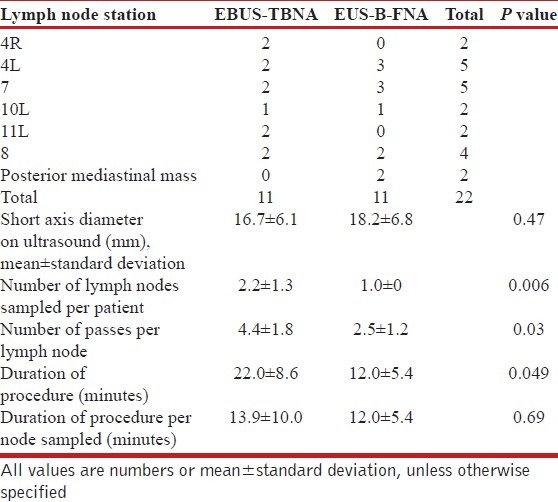
During the study period 257 EBUS-TBNA procedures were performed. Eleven patients (two women) with a mean (SD) age of 39.7 (19.4) years underwent EUS-B-FNA [Table 1]. EBUS was also performed in six of the eleven patients. A total of 11 lymph nodes were assessed by EBUS-TBNA in five patients, whereas, the same number of lesions was assessed in 11 patients by EUS-B-FNA [Table 2]. The left paratracheal (station 4L) and subcarinal (station 7) nodes were the most commonly accessed nodes by EUS-B-FNA. The number of lymph nodes sampled per patient and the number of passes per lymph node were significantly higher with EBUS-TBNA compared to EUS-B-FNA; however, there was no significant difference in the average size of the lymph nodes between the two procedures [Table 2]. The mean duration of the procedure was significantly higher in the EBUS-TBNA group (22 minutes) than in the EUS-B-FNA (12 minutes) group. However, there was no significant difference in the average time of the procedure per lymph node sampled.
Table 1.
Baseline characteristics of study patients (n=11)

Table 2.
Number of lymph nodes sampled according to stations by endobronchial ultrasound-guided transbronchial needle aspiration and endoscopic ultrasound-guided needle aspiration with an echobronchoscope
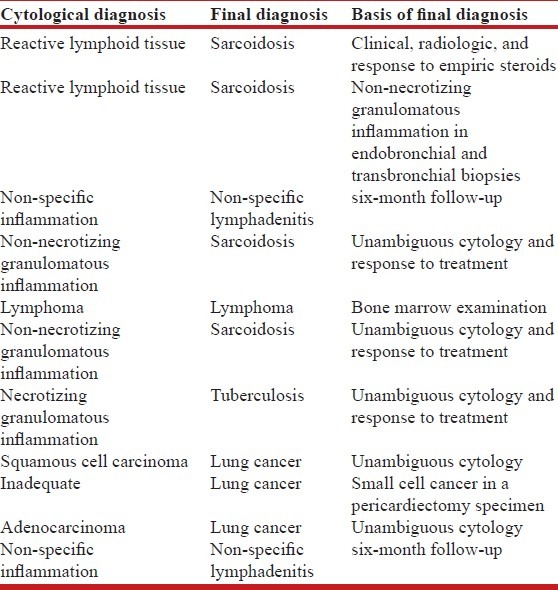
The most common reason (five patients) for resorting to EUS-B-FNA was the patient being unfit for EBUS-TBNA or not allowing the operator to complete the procedure [Table 3]. In three patients, EUS-B-FNA was performed after carrying out an EBUS-TBNA in the same lesion, as all areas of the lesion could not be conveniently accessed by EBUS-TBNA. Sarcoidosis (n = 4) was the most frequent final diagnosis in the study patients [Table 4], followed by bronchogenic carcinoma (three cases). EUS-B-FNA and EBUS-TBNA together helped in making the correct diagnosis in eight out of eleven patients, yielding a sensitivity and specificity of 72.7 and 100%, respectively.
Table 3.
Reasons for resorting to endoscopic ultrasoundguided needle aspiration with an echobronchoscope
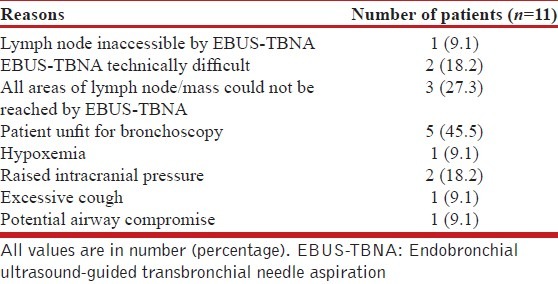
Table 4.
Cytological and final diagnosis of 11 patients subjected to endobronchial ultrasound-guided transbronchial needle aspiration and endoscopic ultrasoundguided needle aspiration with an echobronchoscope
DISCUSSION
This is the first study from India describing the transesophageal use of the EBUS scope for diagnosis of mediastinal lymphadenopathy in adults. We found the technique to be simple and feasible, and when combined with EBUS-TBNA (also called combined endobronchial and endoscopic ultrasound-guided needle aspiration by use of a single ultrasound bronchoscope (CUSb-NA)) it is fairly sensitive and highly specific, similar to the results of other studies.[17,24] The study also demonstrates that EUS-B-FNA provides a good alternative for accessing mediastinal lesions in circumstances where EBUS-TBNA is not feasible.
Endoscopic ultrasound fine-needle aspiration with an echobronchoscope has many advantages over EBUS-TBNA. Similar to EUS-FNA, it reduces patient discomfort as the airway is not obstructed during the procedure and cough is minimized. This makes the use of the esophageal route safer in patients with excessive cough, raised intracranial tension, hypoxemia, and in those with lesions compressing the trachea (with resultant upper airway obstruction) as seen in five of our patients. We found the procedure especially useful for the left lower paratracheal (station 4L) lymph node (three patients), which occasionally becomes difficult to visualize with EBUS-TBNA, due to its proximity to the subaortic area and its location deep in the trachea.[25] Besides, EUS-B-FNA gives additional access to the aortopulmonary window (station 5), paraesophageal (station 8), and pulmonary ligament (station 9) lymph nodes, as well as to lesions located posterior to the esophagus.
Most diseases causing mediastinal lymphadenopathy (lung cancer, sarcoidosis, and tuberculosis) are primarily managed by pulmonary physicians. The most important gain of EUS-B-FNA over EUS-FNA thus lies in making a pulmonary unit self-sufficient in managing such patients. As the procedure can be performed along with EBUS-TBNA in the same session, without the need for additional equipment; it reduces costs, saves time, and decreases the discomfort and inconvenience to the patients.[17] The average cost of EBUS-TBNA procedure approximates to about 15,000 Indian rupees (nearly US$250) and that of EUS-FNA around 16,000 Indian rupees (nearly US$265). Thus, CUSb-NA leads to cost savings of approximately 50% for the patient, in the selected situations.
EUS-B-FNA has certain drawbacks in comparison to EUS-FNA.[26] The sonographic angle of the echobronchoscope is narrower and the image quality inferior compared to the echoendoscope.[27] On account of the shorter length of the EBUS scope, access to the left adrenal (for the purpose of extrathoracic staging of lung cancer) is seldom successful.[28] The ultrasound bronchoscope also has lesser stability in the esophagus on account of its narrow caliber, hence, approach to certain stations like aortopulmonary window (station 5) can be challenging.[26] Contrary to EUS, the needle angle cannot be changed, although bending the EBUS-TBNA needle before insertion can partly overcome this limitation.[18]
There are several peculiarities of the EUS-B-FNA procedure that are to be borne in mind by the pulmonary physician. Endoscopic visualization is limited while maneuvering the scope in the esophagus, because it remains collapsed although instilling oxygen through the working channel of the bronchoscope can partly improve the visibility.[24] As the esophagus is a more contaminated luminal structure than the airways, EBUS should always be performed first followed by EUS-B-FNA. In exceptional circumstances, when EUS needs to be performed first, thorough decontamination of the scope should be achieved before insertion into the trachea. Unlike the case with EBUS, where localization of the various lymph node stations is accomplished by both the bronchial and vascular anatomy, during EUS, nodal stations are localized based on their spatial relationship to the heart and intrathoracic blood vessels. Therefore, it is imperative that the operator is well-acquainted with the vascular anatomy of the thoracic cavity before attempting this procedure. We have also observed that while puncturing the lymph nodes during EUS-B-FNA, they tend to ‘slip’. This is because of the narrower scope and lack of elevation in the EBUS scope; and unlike the airways, the esophageal wall through which the needle is inserted is not a rigid structure due to the absence of cartilaginous rings.[29] Therefore, it is essential to stabilize the scope well and keep the tip of the bronchoscope pushed firmly against the esophageal wall. Thus, it will be necessary to establish methods for training in the EUS-B-FNA technique.
Finally, our study is not without limitations. It is a descriptive study with a small sample size. We did not have availability of on-site cytological examination. We also did not assess the yield of EUS-B-FNA separately in the combined procedures, nor could we compare the technique with EUS-FNA. However, the objective of this study was primarily to assess the feasibility of this unconventional method in a resource-constrained setting like ours.
CONCLUSIONS
The technique of EUS-B-FNA is simple and useful for the diagnosis of mediastinal lymphadenopathy. In combination with EBUS-TBNA, it has a reasonable diagnostic yield. Furthermore, it offers an alternative to the pulmonary physician in circumstances where EBUS-TBNA is not feasible.
ACKNOWLEDGMENTS
The authors wish to thank Dr. VR Pattabhiraman, Director of the Pulmonary Unit at Kovai Medical Center, Coimbatore, and Dr. Malay Sharma, Director of the Gastroenterology Unit at the Jaswant Rai Medical Center, Meerut, for introducing them to the techniques of EUS.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Agarwal R, Aggarwal AN, Gupta D. Efficacy and safety of conventional transbronchial needle aspiration in sarcoidosis: A systematic review and meta-analysis. Respir Care. 2013;58:683–93. doi: 10.4187/respcare.02101. [DOI] [PubMed] [Google Scholar]
- 2.Khan A, Agarwal R, Aggarwal AN, Gupta N, Bal A, Singh N, et al. Blind transbronchial needle aspiration without an on-site cytopathologist: Experience of 473 procedures. Natl Med J India. 2011;24:136–9. [PubMed] [Google Scholar]
- 3.Rami-Porta R, Call S. Invasive staging of mediastinal lymph nodes: Mediastinoscopy and remediastinoscopy. Thorac Surg Clin. 2012;22:177–89. doi: 10.1016/j.thorsurg.2011.12.003. [DOI] [PubMed] [Google Scholar]
- 4.Goyal A, Gupta D, Agarwal R, Bal A, Nijhawan R, Aggarwal AN. Value of different bronchoscopic sampling techniques in diagnosis of sarcoidosis: A prospective study of 151 patients. J Bronchology Interv Pulmonol. 2014;21:220–6. doi: 10.1097/LBR.0000000000000081. [DOI] [PubMed] [Google Scholar]
- 5.Yasufuku K, Chhajed PN, Sekine Y, Nakajima T, Chiyo M, Iyoda A, et al. Endobronchial ultrasound using a new convex probe: A preliminary study on surgically resected specimens. Oncol Rep. 2004;11:293–6. [PubMed] [Google Scholar]
- 6.Vilmann P, Khattar S, Hancke S. Endoscopic ultrasound examination of the upper gastrointestinal tract using a curved-array transducer. A preliminary report. Surg Endosc. 1991;5:79–82. doi: 10.1007/BF00316842. [DOI] [PubMed] [Google Scholar]
- 7.Gupta D, Dadhwal DS, Agarwal R, Gupta N, Bal A, Aggarwal AN. Endobronchial ultrasound guided TBNA vs. conventional TBNA in the diagnosis of sarcoidosis. Chest. 2014 doi: 10.1378/chest.13-2339. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 8.Agarwal R, Srinivasan A, Aggarwal AN, Gupta D. Efficacy and safety of convex probe EBUS-TBNA in sarcoidosis: A systematic review and meta-analysis. Respir Med. 2012;106:883–92. doi: 10.1016/j.rmed.2012.02.014. [DOI] [PubMed] [Google Scholar]
- 9.Wallace MB, Pascual JM, Raimondo M, Woodward TA, McComb BL, Crook JE, et al. Minimally invasive endoscopic staging of suspected lung cancer. JAMA. 2008;299:540–6. doi: 10.1001/jama.299.5.540. [DOI] [PubMed] [Google Scholar]
- 10.Vilmann P, Puri R. The complete “medical” mediastinoscopy (EUS-FNA+EBUS-TBNA) Minerva Med. 2007;98:331–8. [PubMed] [Google Scholar]
- 11.Rintoul RC, Skwarski KM, Murchison JT, Wallace WA, Walker WS, Penman ID. Endobronchial and endoscopic ultrasound-guided real-time fine-needle aspiration for mediastinal staging. Eur Respir J. 2005;25:416–21. doi: 10.1183/09031936.05.00095404. [DOI] [PubMed] [Google Scholar]
- 12.Vilmann P, Krasnik M, Larsen SS, Jacobsen GK, Clementsen P. Transesophageal endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) and endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) biopsy: A combined approach in the evaluation of mediastinal lesions. Endoscopy. 2005;37:833–9. doi: 10.1055/s-2005-870276. [DOI] [PubMed] [Google Scholar]
- 13.Gupta K, Mallery S. Small-caliber endobronchial ultrasonic videoscope: Successful transesophageal and transgastric FNA after failed passage of a standard ultrasonic endoscope. Gastrointest Endosc. 2007;66:574–7. doi: 10.1016/j.gie.2007.02.025. [DOI] [PubMed] [Google Scholar]
- 14.Oki M, Saka H, Kitagawa C, Kogure Y, Murata N, Adachi T, et al. Transesophageal bronchoscopic ultrasound-guided fine needle aspiration for diagnosis of sarcoidosis. Respiration. 2013;85:137–43. doi: 10.1159/000345207. [DOI] [PubMed] [Google Scholar]
- 15.Araya T, Demura Y, Kasahara K, Matsuoka H, Yamamura K, Nishitsuji M, et al. Usefulness of transesophageal bronchoscopic ultrasound-guided fine-needle aspiration in the pathologic and molecular diagnosis of lung cancer lesions adjacent to the esophagus. J Bronchology Interv Pulmonol. 2013;20:121–6. doi: 10.1097/LBR.0b013e31829182a0. [DOI] [PubMed] [Google Scholar]
- 16.Herth FJ, Krasnik M, Kahn N, Eberhardt R, Ernst A. Combined endoscopic-endobronchial ultrasound-guided fine-needle aspiration of mediastinal lymph nodes through a single bronchoscope in 150 patients with suspected lung cancer. Chest. 2010;138:790–4. doi: 10.1378/chest.09-2149. [DOI] [PubMed] [Google Scholar]
- 17.Szlubowski A, Zieliñski M, Soja J, Filarecka A, Orzechowski S, Pankowski J, et al. Accurate and safe mediastinal restaging by combined endobronchial and endoscopic ultrasound-guided needle aspiration performed by single ultrasound bronchoscope. Eur J Cardiothorac Surg. 2014;46:262–6. doi: 10.1093/ejcts/ezt570. [DOI] [PubMed] [Google Scholar]
- 18.Hwangbo B, Lee GK, Lee HS, Lim KY, Lee SH, Kim HY, et al. Transbronchial and transesophageal fine-needle aspiration using an ultrasound bronchoscope in mediastinal staging of potentially operable lung cancer. Chest. 2010;138:795–802. doi: 10.1378/chest.09-2100. [DOI] [PubMed] [Google Scholar]
- 19.Sharma M, Wani ZA, Bansal R, Hari RS. Utility of narrow caliber echo-bronchoscope in pre-school pediatric population: A case series (with video) EndoscUltrasound. 2013;2:96–101. doi: 10.4103/2303-9027.117695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dhooria S, Agarwal R, Aggarwal AN, Bal A, Gupta N, Gupta D. Differentiating tuberculosis from sarcoidosis by sonographic characteristics of lymph nodes on endobronchial ultrasonography: A study of 165 patients. J Thorac Cardiovasc Surg. 2014;148:662–7. doi: 10.1016/j.jtcvs.2014.01.028. [DOI] [PubMed] [Google Scholar]
- 21.Rusch VW, Asamura H, Watanabe H, Giroux DJ, Rami-Porta R, Goldstraw P. Members of IASLC Staging Committee. The IASLC lung cancer staging project: A proposal for a new international lymph node map in the forthcoming seventh edition of the TNM classification for lung cancer. J Thorac Oncol. 2009;4:568–77. doi: 10.1097/JTO.0b013e3181a0d82e. [DOI] [PubMed] [Google Scholar]
- 22.Sharma M, Rameshbabu CS, Mohan P. Standard techniques of imaging of IASLC borders by endoscopic ultrasound. J Bronchology Interv Pulmonol. 2011;18:99–110. doi: 10.1097/LBR.0b013e318207e6d5. [DOI] [PubMed] [Google Scholar]
- 23.Srinivasan A, Agarwal R, Gupta N, Aggarwal AN, Gupta D. Initial experience with real time endobronchial ultrasound guided transbronchial needle aspiration from a tertiary care hospital in north India. Indian J Med Res. 2013;137:803–7. [PMC free article] [PubMed] [Google Scholar]
- 24.Lee KJ, Suh GY, Chung MP, Kim H, Kwon OJ, Han J, et al. Combined endobronchial and transesophageal approach of an ultrasound bronchoscope for mediastinal staging of lung cancer. PLoS One. 2014;9:e91893. doi: 10.1371/journal.pone.0091893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jhun BW, Park HY, Jeon K, Koh WJ, Suh GY, Chung MP, et al. Nodal stations and diagnostic performances of endobronchial ultrasound-guided transbronchial needle aspiration in patients with non-small cell lung cancer. J Korean Med Sci. 2012;27:46–51. doi: 10.3346/jkms.2012.27.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hwangbo B, Lee HS, Lee GK, Lim KY, Lee SH, Kim HY, et al. Transoesophageal needle aspiration using a convex probe ultrasonic bronchoscope. Respirology. 2009;14:843–9. doi: 10.1111/j.1440-1843.2009.01590.x. [DOI] [PubMed] [Google Scholar]
- 27.Sharma M, Arya CL, Somasundaram A, Rameshbabu CS. Techniques of linear endobronchial ultrasound imaging. J Bronchology Interv Pulmonol. 2010;17:177–87. doi: 10.1097/LBR.0b013e3181dca122. [DOI] [PubMed] [Google Scholar]
- 28.Szlubowski A, Soja J, Kocon P, Talar P, Czajkowski W, Rudnicka-Sosin L, et al. A comparison of the combined ultrasound of the mediastinum by use of a single ultrasound bronchoscope versus ultrasound bronchoscope plus ultrasound gastroscope in lung cancer staging: A prospective trial. InteractCardiovascThoracSurg. 2012;15:442–6. doi: 10.1093/icvts/ivs161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sharma M. Combined imaging for benign mediastinal lymphadenopathy: Endoscopic ultrasonography first or endobronchial ultrasonography first? Chest. 2011;140:558–9; author reply 559. doi: 10.1378/chest.11-0455. [DOI] [PubMed] [Google Scholar]


