SUMMARY
Countless disadvantages of the "old" pectoralis major have been listed while the amazing versatility of the free flap armamentarium gives the opportunity to suit the defect deriving from virtually every ablative head and neck surgery with a tailored reconstruction. Nevertheless, pectoralis major is still the "workhorse" for head and neck reconstruction in developing countries thanks to its ease of harvest, and minimal requirements in term of instrumentation. Furthermore, even in facilities with a high volume of reconstructions by free flaps, a certain number of pectoralis major flaps is still raised every year. The history, present role and current indications of the most widely head and neck reconstructive procedure ever has been reviewed.
KEY WORDS: Pectoralis major, Head and neck reconstruction, Regional flaps, Myocutaneous flaps, Fasciocutaneous flaps
RIASSUNTO
Mediante i lembi liberi microlascolari è ad oggi possibile una ricostruzione "su misura" virtualmente di ogni difetto nel distretto testa e collo. I vantaggi delle innumerevoli possibilità ricostruttive offerte dai lembi liberi rispetto al "vecchio" lembo peduncolato di grande pettorale sono ben noti. Tuttavia il lembo di grande pettorale è tuttoggi il workhorse per la ricostruzione della regione testa e collo nei paesi in via di sviluppo, grazie alla relativa semplicità dal punto di vista tecnico, ed al minimo strumentario chirurgico richiesto. Inoltre, anche nelle strutture con un alto volume di procedure ricostruttive mediante lembi liberi, viene sempre indicata in una quota di casi una ricostruzione con lembo di grande pettorale. Nel presente lavoro vengono prese in esame la storia, il ruolo e le attuali indicazioni della procedura ricostruttiva più utilizzata nel testa e collo.
History of the pectoralis major
Evolution of the technique
Pectoralis major myocutaneous (PMMC) flap, based on the thoracoacromial artery, whose first description is commonly attributed to Ariyan in 1979 who exhaustively described the technique and its anatomical basis 1, was however reported in 1977 by at least two authors 2 3. It has been considered for decades the workhorse for head and neck reconstruction, and is still often mentioned as a reliable and easy-to-raise flap 4. Since then, an impressive number of modifications to the original technique have been proposed over the years, with different goals:
to reconstruct different types of defects;
to increase mobility of the flap itself;
to reduce donor site morbidity.
All these modifications and technical refinements have been ultimately aimed at widening the indications for pectoralis major reconstruction.
Since 1984, a variant of the flap called pectoralis major myofascial (PMMF) flap, without the skin paddle overlying the muscle, and intended to reduce the thickness and bulkiness of the original flap, has been described and increasingly used mainly for the reconstruction of hypo/ oropharyngeal defects 5-9. Obviously, while PMMC is more suitable for reconstruction involving skin defects, the PMMF variant better complies with mucosal defects as it is covered early by a substantially normal mucosal layer 10.
Between the 1980s and the 1990s other major variants of the PM flap that incorporated a bony component, potentially very useful for combined mandibular reconstructions, have been described, including a vascularised section of the fifth rib 11 12 or a non-vascularised section of the iliac crest 13 14. A third variant of the osteomyocutaneous flap that included a segment of the outer table of the sternum, sterno-costal joint and rib was reported by Jones and Sommerland who used it for the reconstruction of the zygoma, temporo-mandibular joint and hemi-mandible 15. Maruyama et al. described the transfer of the flap through a midline section of the clavicle 3, a technique that has since been more extensively studied and refined in cadaver models by Freeman et al. who reported a lengthening of the pedicle within the range of 0.5 to 6.5 cm 16. The section of the clavicle is the only way to guarantee greater length and a wider range of movement to the flap: in 2001, Kerawala et al. showed that the subclavicular route was both feasible and safe 17, although later other authors exposed some reservations about the effective advantages offered by this solution 18. Shortly after the report of their first experience with the PMMC, Maruyama et al. proposed a dynamic variant in which the transfer of the flap was combined with selective neuro-anastomoses to provide dynamic muscle action 19. Aesthetical concerns about PMMC in women led to describe "female-friendly" variants with modifications in the harvesting site (as the inframammary paddle described by Ariyan 20) or in the shape of the skin paddle (as the crescentic skin paddle raised medially to the nipple described by Crosher 21).
Since 1980, some authors have reported double paddle variants of the flap for reconstruction of defects involving two separate areas 22-24, which required the preservation of both the thoracoacromial artery and the lateral thoracic arteries, and allowed preservation of the nipple area complex 25 26. With the same aim, many authors have described combinations of the pectoralis major myofascial flap with latissimus dorsi 27, deltopectoral flap both in combination 28 or assembled in a bilobed flap version 29 30, and with free flaps such as radial forearm flap, fibula flap and anterolateral thigh flap 31-33. In 1981, Sharzer et al. reported a parasternal paddle that crossed the midline reaching the contralateral internal mammary perforators 34, and during the same year Dennis and Kashima described a "Janus flap" variant used to repair defects that required two skin surfaces (i.e. cervical oesophagus and pharynx) 35. Later, in the same year, Strawberry et al. described reconstruction with a bilateral PMMC 36. A tubed version of the flap was described by Neifeld et al. in 1983, representing a great advance in oesophageal reconstruction 37. With an eye towards function sparing, in 1985 Morain et al. proposed a medially based segmental transfer of a single intercostal portion of the pectoralis major muscle supplied by a single perforating branch of the internal thoracic artery 38. The same year Lawson described a PMMF flap covered with amnion to prevent partial necrosis in diabetic and elderly patients 39. Katsantonis tried to solve the problem related to function in total glossectomy reconstruction by describing an animal model of neurotisation of PMMC by the hypoglossal nerve 40. In 1988, in an effort to find new ways to reduce thickness, even liposuction of the flap was proposed 41, although this technique, like many others, was most likely never actually employed.
Wei et al., in 1984, described a technique to harvest a muscle-free, longer, and much more movable pedicle by transecting the pectoralis major muscle along its horizontal fibres above the emergence of the thoracoacromial artery 42. Further modifications of this variant have been recently described 43 44, as it remains the most widely used trick, with less risk for the pedicle and patient, to increase the mobility of the flap and reduce undesired bulk in the neck.
It was 1993 when a pectoralis major free flap made its first appearance in the literature, and described by Gateley et al. in a case report that showed a composite variant based on the thoracoacromial artery 45. Chaturvedi et al. have proposed both a sub-mammary approach for women and a flap harvested exclusively through the skin paddle incision 46 47. An endoscopic assisted technique to harvest the pedicle was proposed by Turkmen and Perks in 2005 48. Other innovations involved vascularisation of the flap, which was originally based only on the thoracoacromial artery. In 2006, a technique that preserved the lateral thoracic artery was published 49 and three years later Rikimaru et al. described another way to improve vascularisation and avoid possible complications related to circulation by including the third intercostal perforating branch of the internal thoracic artery 50. The most widely used technique for closure of the donor site is undoubtedly primary closure. Nevertheless, it may be difficult or impossible to achieve when particularly wide skin pads are harvested to accomplish a proper reconstruction, and several authors have described alternative closure techniques for these cases 51-54.
Evolution of indications
In its long history, the pectoralis major flap has seen alternating indications. Since the beginning of the 1980s, until the end of the 1990s, the indications for pectoralis major flaps have progressively broadened, made possible by the unprecedented reconstructive possibilities they offered, which were further increased by the above cited technical refinements. Therefore, many head and neck surgeons worldwide have been trained in these techniques, which became the most widely used reconstructive procedure in the head and neck region to date, the so-called "workhorse of head and neck reconstruction". This reconstructive potential also contributed to enlarging the indications for ablative surgery itself, in cases in which the limitation was related to the possibility to close the defect (i.e. extensive pharyngeal or skin involvement), making many more head and neck malignancies operable.
The preponderance of pectoralis major flaps as a reconstructive option in the head and neck was progressively called into question in the beginning of the XXI century, and pectoralis major is no longer the first option, at least in developed countries, and is often replaced by a wide choice of free flaps that can suit virtually every defect in the head and neck region. Accordingly, reconstruction is no longer an issue for ablative surgery in the head and neck. Nevertheless, many pectoralis major flaps are still harvested, and while its indications have changed and are less extensive, it still remains a very useful tool in several clinical situations.
In 1979, before the development of the techniques that would have pushed this flap to its theoretical limits, Ariyan described his experience with the reconstruction after exenteratio orbitae 55 and temporal bone resection 56. Primary reconstruction of oropharyngeal, hypopharyngeal (including the base of the tongue), pharyngolaryngeal and oral cavity defects (including full thickness cheek defects, hemi- and total glossectomy) after highly invasive oncological surgery 3 5-9 35 57-59; carotid artery protection after radical neck dissection or repair of an orocutaneous, tracheoesophageal and pharyngocutaneous fistula 28 60-62; stomal recurrence after laryngectomy 63; management of osteoradionecrosis of the mandible 64; and salvage of necrotic wounds of the pharynx and neck 65 were among the first indications to be proposed.
The original technique, compared with late variants, allowed only limited mobility of the skin paddle. With the introduction of variants with longer pedicles 16 44 66, tubed 37, split and combined with other flaps 22 23, greater mobility and the possibility to reconstruct larger defects have been achieved, allowing broadening of the indications for reconstruction of nasopharyngeal defects, the anterior skull base 67 and the cervical oesophagus, as well as all skin defects located as far as the forehead 68 and extremely wide as midfacial reconstructions 69. In the 1980s, variants of the flap were also proposed for treatment of facial palsy 70, septic and necrotic wounds 71 and reconstruction of mediastinal trachea 72.
During 1990s, while free flaps were strongly gaining momentum and direct comparisons between free and pedicled flaps were starting to appear in the literature 73-75, the main indications for pectoralis major flaps partially changed in favour of salvage operations. Reconstruction after free flap failure is still one of the major indications for pectoralis major flaps due to the high failure rate of second free tissue transfers 76-79. During the last 10 years, many authors have reported on their experience with this flap, which underlined a shift in the type of subsite reconstructed, with less reconstruction of oral cavity defects over the years, and more hypopharyngeal and oropharyngeal reconstructions 80-82. While the superiority of free flaps over pedicled flaps for tongue and mandibular reconstructions due to functional and esthetical advantages was clearly demonstrated 83-87, due to a higher total failure rate of free flaps other authors tended to still consider the pectoralis major an option when a bone reconstruction is not needed 88, especially in patients with poor overall conditions or in case of unsuccessful microsurgical flaps 89. Other applications that are still valid include management of carotid artery exposure 90, cervical skin defects, dead space filler, infections 78, vessel depleted necks 91, mandible reconstruction when a free flap is not advisable, by rolling the PMMF on a metal plate 88 92 93, pharyngocutaneous fistula 94, closure after total laryngectomies to prevent fistula 95 and reconstruction of full thickness defects of the cheek 96.
The above described evolutions in the indications for pedicled pectoralis reconstruction refers mainly to developed countries, and to settings where patients have access to free flap reconstruction, even though it is noted that the majority of the world population is not in the same condition. In developing densely populated countries, such as India, pectoralis major flaps remain the workhorse for head and neck reconstruction with all of their original indications 97.
Currently adopted techniques
Among the main considerations for currently recommending a pectoralis major reconstruction in a free flap facility in developed countries are shorter operating time, ease of harvest and favourable early and late morbidity profile. For these reasons, the above described complex variants, with multiple paddles, with bone, with a higher rate of failure and/or of donor site complications, or simply with longer operative time, are only seldom raised.
In general, we believe that two main variants: PMMF and PMMC, are by far the most employed techniques. Even if every surgeon has his own way and little tricks for raising a pectoralis major flap, at present most surgeons, to increase the flap mobility while reducing at the same time the bulk in the neck and over the clavicle, prefer the "island" technique described by Wei 42, with successive modifications 43 44, rather than more complex and invasive steps such as cutting the clavicle or passing the flap below the clavicle itself 98 since this increases operative time, morbidity, complications and even causes vascular/pedicle issues for the flap itself. In the same way and for similar reasons, most surgeons in the current literature transfer the flap to the head and neck region through a supraclavicular subplatysmal tunnel, without any incision of the skin overlying the clavicle (which would compromise the vascular supply of a deltopectoral flap (or of its propeller variant internal mammary perforator flap). The only technical differences between the two variants are that the PMMF is harvested without skin, with consequent changes in skin incision and aesthetic outcomes of the donor site, and in operative time (which is even shorter).
Relative advantages and indications
The two variants, even if very similar in terms of the harvesting technique, show many relevant differences for reconstructive potential, postoperative rearrangements and results with clear relative advantages and disadvantages that have an impact on their indications. The PMMC flap was described first and is probably still the most employed variant worldwide. Its advantages lay mostly in the short operative time, ease of harvest, potentially large amount of well-vascularised tissue, relatively low morbidity on the donor site and, most of all, great versatility, as it can close virtually every defect in the head and neck region. The disadvantages and limits should be assessed in comparison with the other reconstructive options available, mainly free flaps, but also the PMMF variant.
Comparison with free flaps, which offer on the whole a huge spectrum of reconstructive options, and are in most situations the gold standard for long-term functional and aesthetic results, which is probably the key issue when evaluating the present role of pectoralis major flaps and will be discussed in detail below.
The skin of the PMMC is not 100% reliable, especially if it is not over the muscle and/or if the skin island is too small. In fact, the vascular supply to the skin comes from musculocutaneous perforators from the pectoralis branches of the thoracoacromial artery, and partial skin losses are relatively frequent (from 5 to 30%) in all series as the perforating vessels are usually not looked for. At any rate, in general, when a skin defect is created, the PMMC variant is always preferable (Figs. 1, 2). The PMMC can be used for mucosal resurfacing with good results as well (Fig. 3).
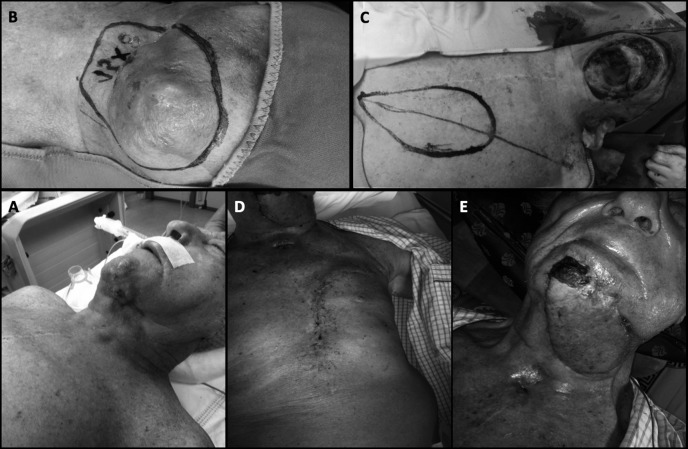
Fig. 1.
A second neck submandibular recurrence with skin invasion (A, B) of a cutaneous SCC in a 92-year-old patient, was treated with a revision of the neck dissection and a wide skin excision (C). The large defect (B, C) was closed with a PMMC flap with a large (15 cm major axis) skin paddle (C, E), partially lying beyond the inferior limit of the pectoralis major muscle (C). For this reason a small distal part of the skin paddle (C), not vascularised enough by muscolocutaneous perforators, has undergone partial necrosis (E). Despite the large dimensions of the skin paddle, a primary closure of the donor site was successfully performed without any complication (D).
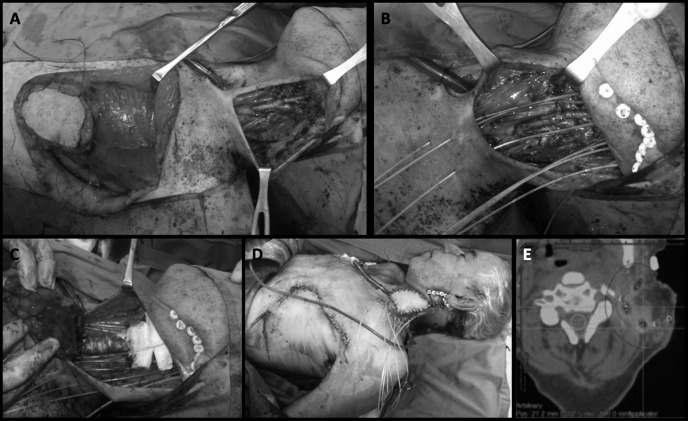
Fig. 2.
A neck recurrence in a patient previously treated with salvage total laryngectomy and neck dissection for a persistent laryngeal cancer after radiochemotherapy, and salvaged again by radical neck dissection (A, B). A pectoralis major myocutaneous flap was raised (A, C, D) to fill the dead space, protect the carotid axis and allow a safe re-irradiation by HDR brachytherapy through the plastic tubes placed during the operation (B, C, D). With this precaution, most of the adjuvant dose is given to the previously non-irradiated pectoralis muscle as shown in the axial image of the treatment plan (E).
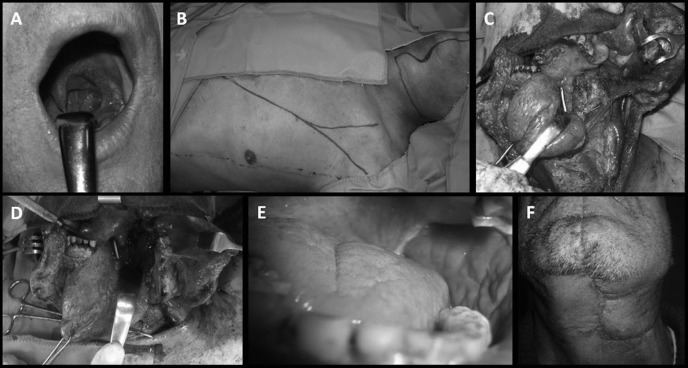
Fig. 3.
(A,B) 75 ys old patient with gum scc invading bone and skin. (C)Wide demolition including skin and mandible was performed. The patient was not suitable for microsurgical recostruction. (D) A titanium plate was inserted in order to reconstruct the mandibular profile. (E,F)Pedicled pectoralis flap was harvested and wrapped on the plate. (H, I, L, M)The coutaneous portion of the flap was used to reconstruct the gum and the skin defect was reconstructed with rotation local flap.
PMMF, in comparison with PMMC, is characterised by an even faster harvest, a wider and more pliable myofascial surface (potentially the entire surface of the pectoralis major muscle) for the closure of the defect. It is thinner, is not covered by hair and is usually resurfaced by the mucosa which normally covers the resected area, whose borders with native mucosa are not usually recognisable in few weeks after insetting (Fig. 4). The shape of the area closed by muscle fascia can be arbitrarily chosen in this case by the surgeon by applying a stitch along the desired suture line.
Fig. 4.
The local recurrence after radiochemotherapy of a SCC of the left posterior faucial pillar (A,C) was salvaged by a partial pharyngectomy through a transmandibular approach (C, D). The defect was restored through a PMMF flap (B, D), with complete re-epithelialisation and acceptable aesthetic results (E, F). The patient was able to feed with a normal diet at 3 weeks after the salvage surgery and did not report dysphagia.
The reduced thickness and the coverage with normal, not hairy, mucosa are undoubtedly a relevant argument supporting the use of PMMF in reconstructions of the oroand hypopharynx (Figs. 4, 5), as the bulk and the hair of the PMMC variant (and also most free flaps) can cause a functional impairment and complaints from patients. On the other hand, one of the main issues considering the functional results of pectoralis major reconstructions, also deriving in pedicled flaps from muscle denervation, is muscle fibrosis and consequent retraction. This is much more evident in the PMMF variant in which it involves the surface of the defect: in pharyngeal defects involving a wide angle of the circumference in the axial plane, it is associated with a high rate of long-term dysphagia, stricture and dependence on PEG 99 100 even in our personal experience (Fig. 5).
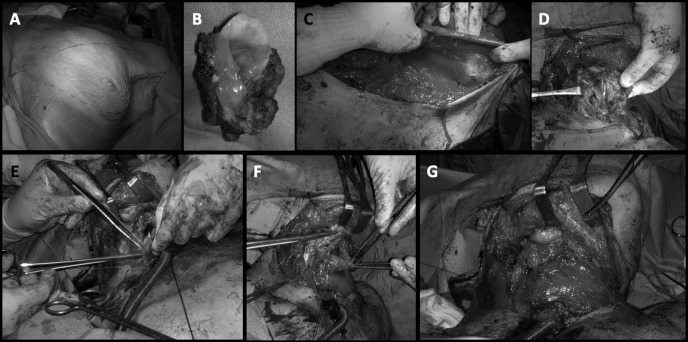
Fig. 5.
Local recurrence after radiochemotherapy of a hypopharyngeal postcricoid SCC was salvaged by total laryngectomy and subtotal pharyngectomy (B). The pharyngeal tube was restored suturing the superficial fascia of a PMMF flap (A, C) to the residual posterior hypopharyngeal mucosa (D, E, F, G). The portion of the hypopharyngeal circumference restored with the procedure was more than 50% (D) and the patient, after the recovery of a normal swallowing without complications, showed progressive dysphagia after 4 months. A recurrent hypopharyngeal stricture was diagnosed, and after two endoscopic dilatations a gastrostomy tube was placed endoscopically (PEG).
On the other hand, the wide pliable myofascial surface can be very useful to be rolled around a reconstruction plate in case of a segmental mandibular defect (Fig. 3). Even in these cases, if no skin area is resected, PMMF may be an alternative to PMMC 93 97 101 102. Considering that most free bony tissue transfers, characterised by relevant donor site morbidity, surgical complexity and duration and complications, are not followed by restoration of dentition through osteointegrated implants, they remain a undeniably valuable option for reconstruction of mandibular defects, especially if lateral, with less aesthetic and functional issues 102.
Salvage total laryngectomies after irradiation are characterised by a high rate of fistulas 103; in these cases, pectoralis major flaps may work as dead space fillers, bring well-vascularised tissue in the irradiated field, reinforce the pharyngeal suture and have been demonstrated to markedly reduce the risk of this complication. For this reason, in post- radiation laryngectomies several authors propose to electively reinforce the suture line and the pharyngeal wall with a pectoralis major 95 104 105. If a skin island is not needed for a skin defect, better results have been shown with a thin, well vascularised PMMF 95. For the same reason, many authors use the pectoralis major to protect the carotid axis after a salvage radical neck dissection following radiotherapy failure 8 78 106. At the same time, the well vascularised muscular tissue fills the dead space, and the vascular supply reduces post-irradiation neck fibrosis. If a PMMC is raised, its well vascularised skin reduces the tension and retraction of the suture line and later of the scar (Fig. 2). The inset of the PMMC flap in vessel depleted necks after salvage neck dissection has allowed us in some cases to place plastic tubes to administer further adjuvant perioperative brachytherapy (Fig. 2).
The protective and trophic effect of pectoralis muscle on neck vessels and tissues is an advantage in all cases after radiotherapy and neck dissection, even if the reconstructed defect is in the pharynx, oral cavity, or other head and neck sites: in fact, the humeral end of the raised muscle always tends to remain in the neck (Figs. 1-5). Many free flap surgeons use both the variants of the pectoralis flap in combination with free tissue transfer, based upon these considerations and with similar indications, also for coverage and protection of microanastomosis 83 115.
Complications and morbidity
PMMC and PMMF are both related to some complications that have partially changed both in type and frequency, thanks to evolution of the technique. The very first report of complications in 42 cases of reconstruction with PMMC 57 did not show any major necrosis, while minor necrosis was present in three cases (7%). appeared later report documented a wider range of complications including those involving the donor site, such as chest wall haematoma and infections, the reconstructed areas, including fistula and neck abscess, or the flap itself with partial and total necrosis 108.
Later, in 1983, two interesting and larger reports provided deeper insight into the actual complication rates. Mehrhof et al. 109, describing their experience on 67 patients treated with 73 PMMC, reported a complication rate of 54%. Major complications were total flap necrosis (4%) and partial flap necrosis (12%). The vast majority were minor complications that did not require second procedures for correction: orocutaneous fistulas (16.5%), suture line dehiscence (12%), neck wound complications (11%), donor site complication (1.3%) and sequelae related to mandibular replacement (not a complication of the flap itself but related to a metal device used by the authors to restore mandibular continuity in 10 patients included in this series) (11%). In the same year, Ossoff et al. 110, while reporting an overall complication rate similar to those previously reported, warned other authors about the insidious possibility of a delayed detection of recurrence hidden by the flap itself, which occurred three times in their experience (86 patients, 95 PMMC). In 1984, Donegan et al. reported another rare complication, namely osteomyelitis of the rib in the donor area of the PMMF 111. Even if unusual, this complication gave rise to a number of publications discussing its treatment, with the use of a vertical rectus abdominis myocutaneous flap proposed by Nagarjuna et al. being the latest 112. Other reported complications include exposure of the plate covered by the flap in reconstructions of the mandible 91 and cervical contracture leading to severe functional impairment 113. Cervical contracture has been specifically addressed by some authors by secondary myectomy and subclavicular route 17 114, but a certain amount of contracture is unavoidable, deriving from the fibrotic retraction of the denervated muscle, even in the "island" technique.
In 1990, an interesting report on 168 cases of PMMC and PMMF performed at MD Anderson Cancer Center in Texas by Kroll et al. was published 115 in which the rate of overall complications was 63%, but with a flap loss rate of only 2.4%, with a relatively higher complication rate in smokers and patients with larger tumours. Later, in the same year, Shah reported his experience 116 which consisted of 211 patients treated with PMMC. Similar to that seen at MD Anderson, he reported an overall complication rate of 63%. On the other hand, despite the apparently high complication rate, he reported only 2 cases in which a second flap was required (1%), and 33 cases in which reoperation was required to resolve complications. Such a low rate of major complications was substantially confirmed in the 1990s by other authors 117. A correlation between complications and some variables was also shown, namely: age over 70 years, female sex, overweight, albumin less than 4 g/dl, oral cavity reconstruction after total glossectomy and systemic disease. Some of these correlations had been previously reported by Kroll et al. and later by other authors with the adjunct of prior chemotherapy and secondary reconstructions 117-119. The higher rate of flap necrosis seen in women by those authors was attributed to the interposition of breast tissue between muscle and the skin paddle. In fact, the authors noted that only PMMC were involved by this phenomena, while in their series PMMF had the same complication rates between men and women 115. Both Shah and later Keidan et al. outlined the absence of a significant correlation between prior radiation therapy and complication rates 120.
Starting from 2000, reports in literature from both wealthy and poor-developing countries, substantially confirm a slight drop in complications, with very few to no total flap losses recorded and an overall complication rate around 20–50% as seen in many papers published during this period 7 91 113 119 121 122. At present such complications rates are probably even lower, at least in developed countries. A rare complication of PMMC with very few reports in literature published in the last 15 years is metastasis at the flap donor site, for which some possible mechanisms have been proposed based on anatomical and physiological considerations 123.
Comparison with free flaps
Since the development of reconstructive techniques involving free flaps 124, we participated in a lively debate on the advantages and disadvantages of both pedicled and free flap techniques applied to head and neck sites. In an attempt to summarise the data from the literature, it should be kept in mind that pectoralis major is often confronted to different types of free flaps and in different types of reconstructions, thus making it impossible to make any general statements. Each type of reconstruction would ideally require a separate discussion to come to definitive conclusions. During the last 30 years, the three main topics of discussion have been functional results, morbidity and costs of the two techniques. In all these areas, when comparing free flap with pectoralis major patients, several biases can be seen, the most important being in our opinion that in the free flap era many patients were recommended pedicled flaps when they are in poor general conditions, with the preference for an option with short operative time, technical ease and low morbidity. As a result, radically different groups, at least in terms of comorbidities, are often compared. For this reasons, we believe that comorbidity, or at least age, should be considered and matched in every attempt at comparison.
Functional results
Each subsite would ideally deserve a separate discussion, even if not all the papers in the literature analytically evaluate the functional differences according site and size of the defect. Paradoxically, despite the amount of publications evaluating reconstructive techniques in the head and neck, there is still a lack of evidence-based data about the functional differences between free and pedicled flaps, and no definitive conclusions can be made at present. Actually, the concept of function in head and neck cancer patients is controversial and consensus about the objective evaluation of functional results is lacking. The most used tools are questionnaires, which are not specific and sensitive in evaluating the functional aspects addressed by the different reconstructive techniques. Nonetheless, a few investigations give some clues with which to initiate definite functional comparison site by site.
An impressive series was presented by Hsing et al. in 2011 125. They reported their experience with 491 patients treated for oral cavity cancer, 100 of which completed a quality of life questionnaire. They found no significant difference in overall quality of life between patients treated with PMMC versus free flaps, nor did they find differences in the domains regarding pain, appearance, activity, recreation, swallowing, chewing, taste, saliva, or anxiety. Nevertheless, they reported significant differences between the free flap and PMMC flap groups in speech, shoulder mobility and mood domains with better outcomes for the free flap group.
Xiao et al., also focusing specifically on oral cavity cancer and analysing two groups, one characterised by reconstruction performed with an anterolateral tight (ALT) flap and the other by PMMC, found no significant differences between groups for pain, activity, recreation, swallowing, chewing, speech, taste, saliva, or mood and anxiety domains. However, significant differences were seen between the PMMC and ALT groups for the shoulder and appearance domains, and a higher emotional impact left by the scar and the aesthetic appearance left by PMMC 126. A similar study with similar results was presented in 2014 by Zhang et al., with the only difference being slightly worse speech outcome for patients treated by ALT 127.
O'Neill et al., in 2010, published an interesting comparison between radial forearm free flaps and PMMC in reconstruction of oral and oropharyngeal defects 128. In their report, they outlined that while no differences in deformity, diet, or socialisation were found, only 22.2% of patients reconstructed with PMMC were satisfied with their speech compared with 53.1% of patients reconstructed with RFFF. Deganello et al. noted a difference in diet with all PMMC in their series able to feed only by soft or liquid diet postoperatively 99 129.
As free flaps show a predisposition to better performance in functional outcomes 86, many authors have tried to close the gap by developing variants of the PMMC/PMMF meant to improve functional results, such as the dynamic variant 19 and attempts of neurotisation of the flap with the hypoglossal nerve 40. These complex techniques, however, are associated with loss of the renowned advantages of pectoralis flaps in terms of ease and speed.
Morbidity
Pectoralis major has a rate of complications that is not to be underestimated, and the rate of overall complications raised some concerns in the past. An interesting comparison of complications rate between the free tissue transfer option and the PMMC were made by Mallet et al. in 2009 130 who analysed the results of 70 consecutive patients treated alternatively with both techniques (25 FTT and 45 PMMC). They outlined a similar rate of postoperative complications and the same duration of use of tracheostomy tube and feeding tube. Similar results, prone to a substantially similar morbidity of free flaps and PMMF/ PMMC, have been reported by other groups 125 131, some of which also highlighted a similar failure rate 78. O'Neill, reporting on a series of 114 patients treated alternatively with PMMC or radial forearm free flap (RFFF) reported that the only significant differences in complications were suture dehiscence, which were more frequent in PMMC, and atelectasis, which was more frequent in RFFF; major flap complications, leading to another surgery, were more frequent in the RFFF group 128.
In a similar study, de Bree et al. reported a higher rate of medical complications, flap failures and admissions to intensive care units in the radial forearm group, but more overall surgical complications (partial flap necrosis, dehiscence, wound abscesses and fistula) with PMMC 132, as seen in other studies 73 133, thus leading to a longer postoperative hospitalisation for treatment of complications.
Costs
In the last years, in light of spending reviews and rationalisations
of resources, especially in Italy, the costs of reconstructive procedures must be taken into account. The main factors contributing to the increase in costs, in our experience, are the time spent in the hospital postoperatively (heavily influenced by the complication rate), time spent in the operating room and number of surgeons required. PMMC is often recognised as a faster technique considering operating time 125 126 129-132 134-136, and most reports outline that free flap surgery requires more surgeons at the same time 129 130 137. In many departments, FFT in the head and neck are performed by two teams at the same time, thus reducing the operative time, but not the overall costs. Data regarding discharge time after surgery seems to be uniform in the literature with most authors outlining a similar if not shorter time needed after a procedure involving free flaps 128-132. Nevertheless, when it comes to costs estimated in single experiences, data are rather conflicting. Some authors reported higher costs with free flaps 91 129 134 136 138, while others have documented that overall costs for PMMC are either higher 115 132 or not significantly different 131 139. In particular, Funk et al. hypothesised that although surgical costs were higher for free flaps, postoperative hospitalisation due to treatment of complications, which is higher in PMMC, balanced the costs and abolished any economic advantages 139.
While a generally acceptable, definitive statement about respective costs is probably not possible at present, according to the literature we can at least definitely accept that, even with highly significant differences between various reports, the time spent in the operating room for reconstruction with a pedicled flap is undeniably shorter. Importantly, as outlined by de Bree et al. 132, most studies on costs have selection biases, and do not consider differences in age and comorbidity, thus probably complicating any possible evaluation on discharge time and complication rates.
Notably, in settings where resource constraints are a matter of fact, along with the lack of available technologies and expertise, such as in developing countries, extensive use of pectoralis major at the expense of free flaps remains a reality 91 97 138.
Our experience
Our 20-year clinical experience in pectoralis major reconstructions at the main big facilities in Italy performing a high volume of free flap procedures is shown in Table I. Virtually every defect in the head and neck region has been addressed, with a very low rate of complications (less than 5% of patients experienced any kind of procedure- related sequelae). Such complication rate is lower than what reported in most paper in the literature, nevertheless in our opinion it reflects the state of the art as for pectoralis major reconstruction and appears the main general argument supporting the use of pectoralis major regional flaps in most cases. The 274 cases (Table I) have been operated along 20 years, in this long period several changes in the use and indications for pectoralis major reconstructions have been occurred, mostly reflecting the above cited literature evidences. In fact the number of pectoralis major flaps raised per year has on the whole decreased, and in particular it is now only seldom used for tongue and skin defect. The median age of the patient has increased together with their comorbidities. Interestingly, in recent years pectoralis major inset has been also useful for allow safe further irradiation by brachytherapy in a few cases, by protecting neck vessels and bringing nonpreviously irradiated tissue (Fig. 2).
Table I.
Descriptive statistics of the main variables concerning patients, primary sites and defects.
| Characteristic | N = 274 |
|---|---|
| Age at diagnosis | |
| Median | 70 |
| Range | 29-92 |
| Sex [N (%)] | |
| Male | 199 (72.6%) |
| Female | 75 (27.4%) |
| Variant (PMMC vs. PMMF) [N (%)] | |
| PMMC | 237 (86.5%) |
| PMMF | 37 (13.5%) |
| Primary site [N (%)] | |
| Larynx and Hypopharynx | 21 (7.7%) |
| Mandible | 19 (7%) |
| Oropharynx | 85 (31%) |
| Skin | 5 (1.8%) |
| Occult primary | 1 (0.3%) |
| Oral cavity | 143 (52.2%) |
| Retromolar | 56 (20.4%) |
| Tongue | 87 (31.8%) |
| Hystotype | N (%) |
| SCC | 255 (93%) |
| Salivary histotypes | 17 (6.2%) |
| Malignant ameloblastoma | 1 (0.4%) |
| Osteosarcoma | 1 (0.4%) |
| Type of defect | |
| Mucosa | 141 (51.5%) |
| Mucosa+bone | 112 (40.9%) |
| Mucosa+skin | 11 (4%) |
| Skin | 10 (3.6%) |
| Previous treatments for HNSCC | |
| None | 209 (76.3%) |
| Radio±chemotherapy | 48 (17.5%) |
| Surgery | 3 (1.1%) |
| Surgery+ radio±chemotherapy | 14 (5.1%) |
| Adjuvant /perioperative treatments | |
| None | 154 (56.2%) |
| Radiotherapy | 102 (37.2%) |
| Brachytherapy | 4 (1.5%) |
| Radio±chemotherapy | 14 (5.1%) |
| Timing | |
| Immediate | 265 (96.7%) |
| Delayed (management of radiotherapy sequelae) | 9 (3.3%) |
| Early and late complications of the procedure | |
| Partial skin necrosis | 8 (2.9%) |
| Total necrosis | 2 (0.7%) |
| Donor site dehiscence | 2 (0.7%) |
| Late hypopharyngeal stricture/ gastrostomy | 1 (0.4%) |
| Death | 1 (0.4%) |
| None | 261 (95.3%) |
Conclusions
We are definitely in the era of free flap surgery. In developed countries, in excellence centres, and in patients with good general conditions, the amazing versatility of the free flap armamentarium gives the opportunity to suit the defect deriving from virtually every ablative head and neck surgery with a tailored reconstruction. Such possibilities, even in the absence of definitive evidence-based data on better functional outcomes compared with pectoralis major flaps, make free tissue transfer the standard for head and neck reconstruction. Countless disadvantages of the "old" pectoralis major have been listed, such as flap thickness, functional and cosmetic defects, excessive bulk in obese or muscular patients, poor reliability of the skin in PMMC, difficulty in obtaining reliable bone tissue and long-term fibrotic muscle retraction.
Nevertheless, even in facilities with a high volume of reconstructions by free flaps, a certain number of pectoralis major flaps is still raised every year in the head and neck. The easier indication is reconstruction after a free flap failure due to the high failure rate of second free tissue transfers 76 77. Other indications, which are much more common, are probably controversial, and therefore more interesting to discuss. They can be driven by the setting in which patients are cured, by clinical status and comorbidities of patients and perhaps, in very selected cases, by the type of the defect.
The healthcare system and the facilities in which patients are cured are also key considerations in determining epidemiology and death rates for cancer worldwide. Raising a pectoralis major just requires a knife, forceps and retractors as surgical instrumentation, few hours of operative time, shorter training time and less surgical skills. Mainly for these reasons in developing countries such as India the pectoralis major remains the workhorse for head and neck reconstruction 97. Nevertheless, in forthcoming years, the public discussion about health system resources and spending reviews may bring these arguments to many Western countries in recession. As previously outlined, another reason why pectoralis major can still be indicated is related to patient conditions, which may require ease of harvest and shorter operative times (and therefore, especially in the elderly, a lower perioperative complication rate).
Finally, there are some situations in which pectoralis major still appears as a valuable option even in facilities performing free flaps and for patients in good general conditions 78. One such situation is prevention of pharyngocutaneous fistula in case of salvage total laryngectomies after irradiation. In these cases, several authors have proposed to electively reinforce the suture line and pharyngeal wall with a PMMF 95 104 105. In the same way, PMMF/PMMC can be used to protect the carotid axis after salvage radical neck dissection following radiotherapy failure 8 78 106, and in these cases a further adjuvant perioperative brachytherapy can be safely administered (Fig. 2). Lastly, recent reports stress 7 80 99 100 140 the utility of pectoralis major flaps for reconstruction of pharyngeal defects. In case of circumferential defects, long-term stricture due to muscle fibrotic retraction is probably frequent (Fig. 5), but in lateral defects (less than 50% of pharyngeal circumference) the reduced thickness and coverage with normal, not hairy, mucosa are relevant advantages supporting the use of PMMF (Fig. 4). In case of a segmental lateral mandibular defect, if restoration of dentition is not planned, a PMMC or PMMF rolled around a reconstruction plate may be a valid option characterised by low morbidity 93 97 101 102.
References
- 1.Ariyan S. The pectoralis major myocutaneous flap. A versatile flap for reconstruction in the head and neck. Plast Reconstr Surg. 1979;63:73–81. doi: 10.1097/00006534-197901000-00012. [DOI] [PubMed] [Google Scholar]
- 2.Brown RG, Fleming WH, Jurkiewicz MJ. An island flap of the pectoralis major muscle. Br J Plast Surg. 1977;30:161–165. doi: 10.1016/0007-1226(77)90015-7. [DOI] [PubMed] [Google Scholar]
- 3.Maruyama Y, Fujino T, Aoyagi F, et al. One stage reconstruction of oral cavity by use of pectoralis major myocutaneous island flap. Keio J Med. 1978;27:47–52. doi: 10.2302/kjm.27.47. [DOI] [PubMed] [Google Scholar]
- 4.El-Marakby HH. The reliability of pectoralis major myocutaneous flap in head and neck reconstruction. J Egypt Natl Canc Inst. 2006;18:41–51. [PubMed] [Google Scholar]
- 5.Robertson MS, Robinson JM. Pharyngoesophageal reconstruction. Is a skin-lined pharynx necessary? Arch Otolaryngol. 1985;111:375–376. doi: 10.1001/archotol.1985.00800080061006. [DOI] [PubMed] [Google Scholar]
- 6.Phillips JG, Postlethwaite K, Peckitt N. The pectoralis major muscle flap without skin in intra-oral reconstruction. Br J Oral Maxillofac Surg. 1988;26:479–485. doi: 10.1016/0266-4356(88)90069-1. [DOI] [PubMed] [Google Scholar]
- 7.Montemari G, Rocco A, Galla S, et al. Hypopharynx reconstruction with pectoralis major myofascial flap: our experience in 45 cases. Acta Otorhinolaryngol Ital. 2012;32:93–97. [PMC free article] [PubMed] [Google Scholar]
- 8.Shindo ML, Costantino PD, Friedman CD, et al. The pectoralis major myofascial flap for intraoral and pharyngeal reconstruction. Arch Otolaryngol Head Neck Surg. 1992;118:707–711. doi: 10.1001/archotol.1992.01880070037007. [DOI] [PubMed] [Google Scholar]
- 9.Righi PD, Weisberger EC, Slakes SR, et al. The pectoralis major myofascial flap: clinical applications in head and neck reconstruction. Am J Otolaryngol. 1998;19:96–101. doi: 10.1016/s0196-0709(98)90102-8. [DOI] [PubMed] [Google Scholar]
- 10.Johnson MA, Langdon JD. Is skin necessary for intraoral reconstruction with myocutaneous flaps? Br J Oral Maxillofac Surg. 1990;28:299–301. doi: 10.1016/0266-4356(90)90101-p. [DOI] [PubMed] [Google Scholar]
- 11.Cuono CB, Ariyan S. Immediate reconstruction of a composite mandibular defect with a regional osteomusculocutaneous flap. Plast Reconstr Surg. 1980;65:477–484. doi: 10.1097/00006534-198004000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Green MF, Gibson JR, Bryson JR, et al. A one-stage correction of mandibular defects using a split sternum pectoralis major osteo-musculocutaneous transfer. Br J Plast Surg. 1981;34:11–16. doi: 10.1016/0007-1226(81)90087-4. [DOI] [PubMed] [Google Scholar]
- 13.Bell MS, Barron PT. The rib-pectoralis major osteomyocutaneous flap. Ann Plast Surg. 1981;6:347–353. doi: 10.1097/00000637-198105000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Phillips JG, Falconer DT, Postlethwaite K, et al. Pectoralis major muscle flap with bone graft in intra-oral reconstruction. Br J Oral Maxillofac Surg. 1990;28:160–163. doi: 10.1016/0266-4356(90)90079-z. [DOI] [PubMed] [Google Scholar]
- 15.Jones NF, Sommerlad BC. Reconstruction of the zygoma, temporo-mandibular joint and mandible using a compound pectoralis major osteo-muscular flap. Br J Plast Surg. 1983;36:491–497. doi: 10.1016/0007-1226(83)90138-8. [DOI] [PubMed] [Google Scholar]
- 16.Freeman MS, Thomas JR, Zipper JA. Clavicular division technique. A new approach for lengthening the pectoralis flap. Arch Otolaryngol Head Neck Surg. 1989;115:224–227. doi: 10.1001/archotol.1989.01860260098022. [DOI] [PubMed] [Google Scholar]
- 17.Kerawala CJ, Sun J, Zhang ZY, et al. The pectoralis major myocutaneous flap: Is the subclavicular route safe? Head Neck. 2001;23:879–884. doi: 10.1002/hed.1127. [DOI] [PubMed] [Google Scholar]
- 18.Vanni CM, Pinto FR, Matos LL, et al. The subclavicular versus the supraclavicular route for pectoralis major myocutaneous flap: a cadaveric anatomic study. Eur Arch Otorhinolaryngol. 2010;267:1141–1146. doi: 10.1007/s00405-010-1203-5. [DOI] [PubMed] [Google Scholar]
- 19.Maruyama Y, Nakajima H, Fujino T. A dynamic reconstruction of a facial defect with a pectoralis major myocutaneous flap. Br J Plast Surg. 1980;33:145–149. doi: 10.1016/0007-1226(80)90002-8. [DOI] [PubMed] [Google Scholar]
- 20.Ariyan S. The donor site of the pectoralis major myocutaneous flap. Plast Reconstr Surg. 1980;66:165–166. [PubMed] [Google Scholar]
- 21.Crosher R, Llewelyn J, Mitchell R. A modification of the pectoralis major myocutaneous flap that reduces the defect at the donor site. Ann R Coll Surg Engl. 1995;77:389–391. [PMC free article] [PubMed] [Google Scholar]
- 22.Morain WD, Geurkink NA. Split pectoralis major myocutaneous flap. Ann Plast Surg. 1980;5:358–361. doi: 10.1097/00000637-198011000-00005. [DOI] [PubMed] [Google Scholar]
- 23.Freeman JL, Gullane PJ, Rotstein LM. The double paddle pectoralis major myocutaneous flap. J Otolaryngol. 1985;14:237–240. [PubMed] [Google Scholar]
- 24.Ord RA, Avery BS. Side-by-side double paddle pectoralis major flap for cheek defects. Br J Oral Maxillofac Surg. 1989;27:177–185. doi: 10.1016/0266-4356(89)90141-1. [DOI] [PubMed] [Google Scholar]
- 25.Freeman JL, Walker EP, Wilson JS, et al. The vascular anatomy of the pectoralis major myocutaneous flap. Br J Plast Surg. 1981;34:3–10. doi: 10.1016/0007-1226(81)90086-2. [DOI] [PubMed] [Google Scholar]
- 26.Espinosa MH, Phillip JA, Khatri VP, et al. Double skin island pectoralis major myocutaneous flap with nipple-areola complex preservation: a case report. Head Neck. 1992;14:488–491. doi: 10.1002/hed.2880140612. [DOI] [PubMed] [Google Scholar]
- 27.Maruyama Y, Nakajima H, Fujino T. One-stage reconstruction of a esophagostome with a latissimus dorsi myocutaneous flap and a pectoralis major myocutaneous flap (case report) Acta Chir Plast. 1980;22:80–85. [PubMed] [Google Scholar]
- 28.Maisel RH, Liston SL. Combined pectoralis major myocutaneous flap with medially based deltopectoral flap for closure of large pharyngocutaneous fistulas. Ann Otol Rhinol Laryngol. 1982;91:98–100. doi: 10.1177/000348948209100122. [DOI] [PubMed] [Google Scholar]
- 29.Meyer R, Kelly TP, Abul Failat AS. Single bilobed flap for use in head and neck reconstruction. Ann Plast Surg. 1981;6:203–206. doi: 10.1097/00000637-198103000-00005. [DOI] [PubMed] [Google Scholar]
- 30.Weaver AW, Vandenberg HJ, Atkinson DP, et al. Modified bilobular ("gemini") pectoralis major myocutaneous flap. Am J Surg. 1982;144:482–488. doi: 10.1016/0002-9610(82)90429-9. [DOI] [PubMed] [Google Scholar]
- 31.Harii K, Iwaya T, Kawaguchi N. Combination myocutaneous flap and microvascular free flap. Plast Reconstr Surg. 1981;68:700–711. doi: 10.1097/00006534-198111000-00006. [DOI] [PubMed] [Google Scholar]
- 32.Chen HC, Demirkan F, Wei FC, et al. Free fibula osteoseptocutaneous- pedicled pectoralis major myocutaneous flap combination in reconstruction of extensive composite mandibular defects. Plast Reconstr Surg. 1999;103:839–845. doi: 10.1097/00006534-199903000-00009. [DOI] [PubMed] [Google Scholar]
- 33.Choi JO, Choi G, Chae SW, et al. Combined use of pectoralis major myocutaneous and free radial forearm flaps for reconstruction of through-and-through defects from excision of head and neck cancers. J Otolaryngol. 1999;28:332–336. [PubMed] [Google Scholar]
- 34.Sharzer LA, Kalisman M, Silver CE, et al. The parasternal paddle: a modification of the pectoralis major myocutaneous flap. Plast Reconstr Surg. 1981;67:753–762. [PubMed] [Google Scholar]
- 35.Dennis D, Kashima H. Introduction of the Janus flap. A modified pectoralis major myocutaneous flap for cervical esophageal and pharyngeal reconstruction. Arch Otolaryngol. 1981;107:431–435. doi: 10.1001/archotol.1981.00790430033009. [DOI] [PubMed] [Google Scholar]
- 36.Strawberry CW, Fries HO, Deeb ZE. Reconstruction of the hypopharynx and cervical esophagus with bilateral pectoralis major myocutaneous flaps. Head Neck Surg. 1981;4:161–164. doi: 10.1002/hed.2890040213. [DOI] [PubMed] [Google Scholar]
- 37.Neifeld JP, Merritt WA, Theogaraj SD, et al. Tubed pectoralis major musculocutaneous flaps for cervical esophageal replacement. Ann Plast Surg. 1983;11:24–30. doi: 10.1097/00000637-198307000-00004. [DOI] [PubMed] [Google Scholar]
- 38.Morain WD, Colen LB, Hutchings JC. The segmental pectoralis major muscle flap: a function-preserving procedure. Plast Reconstr Surg. 1985;75:825–830. doi: 10.1097/00006534-198506000-00010. [DOI] [PubMed] [Google Scholar]
- 39.Lawson VG. Pectoralis major muscle flap with amnion in oral cavity reconstruction. Aust N Z J Surg. 1986;56:163–166. doi: 10.1111/j.1445-2197.1986.tb01875.x. [DOI] [PubMed] [Google Scholar]
- 40.Katsantonis GP. Neurotization of pectoralis major myocutaneous flap by the hypoglossal nerve in tongue reconstruction: clinical and experimental observations. Laryngoscope. 1988;98:1313–1323. doi: 10.1288/00005537-198812000-00007. [DOI] [PubMed] [Google Scholar]
- 41.Cueva R, Thomas JR, Davidson TM. Liposuction to debulk the pectoralis major myocutaneous flap. Am J Otolaryngol. 1988;9:106–110. doi: 10.1016/s0196-0709(88)80015-2. [DOI] [PubMed] [Google Scholar]
- 42.Wei WI, Lam KH, Wong J. The true pectoralis major myocutaneous island flap: an anatomical study. Br J Plast Surg. 1984;37:568–573. doi: 10.1016/0007-1226(84)90151-6. [DOI] [PubMed] [Google Scholar]
- 43.Kasler M, Banhidy FG, Trizna Z. Experience with the modified pectoralis major myocutaneous flap. Arch Otolaryngol Head Neck Surg. 1992;118:931–932. doi: 10.1001/archotol.1992.01880090047014. [DOI] [PubMed] [Google Scholar]
- 44.Palmer JH, Batchelor AG. The functional pectoralis major musculocutaneous island flap in head and neck reconstruction. Plast Reconstr Surg. 1990;85:363–367. doi: 10.1097/00006534-199003000-00004. [DOI] [PubMed] [Google Scholar]
- 45.Gateley DR, Moss AL, Blenkinsopp P. Reconstruction of the anterior lower third of the face using a composite pectoralis major free flap. J R Soc Med. 1993;86:731–732. doi: 10.1177/014107689308601220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chaturvedi P, Prabhudesai SG, Kanitkar G, et al. Sub-mammary approach for pectoralis major myocutaneous flap in females. J Surg Oncol. 2003;84:255–256. doi: 10.1002/jso.10324. [DOI] [PubMed] [Google Scholar]
- 47.Chaturvedi P, Pathak KA, Pai PS, et al. A novel technique of raising a pectoralis major myocutaneous flap through the skin paddle incision alone. J Surg Oncol. 2004;86:105–106. doi: 10.1002/jso.20048. [DOI] [PubMed] [Google Scholar]
- 48.Turkmen A, Perks AG. Endoscopic assisted harvest of the pedicled pectoralis major muscle flap. Br J Plast Surg. 2005;58:170–174. doi: 10.1016/j.bjps.2004.10.019. [DOI] [PubMed] [Google Scholar]
- 49.Po-Wing YA. Preservation of lateral thoracic artery to improve vascular supply of distal skin without compromising pedicle length in harvesting pectoralis major myocutaneous flap. J Plast Reconstr Aesthet Surg. 2006;59:1433–1435. doi: 10.1016/j.bjps.2006.02.007. [DOI] [PubMed] [Google Scholar]
- 50.Rikimaru H, Kiyokawa K, Watanabe K, et al. New method of preparing a pectoralis major myocutaneous flap with a skin paddle that includes the third intercostal perforating branch of the internal thoracic artery. Plast Reconstr Surg. 2009;123:1220–1228. doi: 10.1097/PRS.0b013e31819f2967. [DOI] [PubMed] [Google Scholar]
- 51.Belt PJ, Emmett J. Local transposition flap repair of the pectoralis major myocutaneous flap donor site. Plast Reconstr Surg. 2004;114:732–737. doi: 10.1097/01.prs.0000131237.23717.98. [DOI] [PubMed] [Google Scholar]
- 52.Chan YW, Ng RW, Yuen AP. Lateral thoracic flap for donor site repair of pectoralis major myocutaneous flap. J Plast Reconstr Aesthet Surg. 2009;62:1004–1007. doi: 10.1016/j.bjps.2008.02.009. [DOI] [PubMed] [Google Scholar]
- 53.Kruse AL, Luebbers HT, Gratz KW, et al. A new method for closure of large donor side defects after raising the pectoralis major flap. Oral Maxillofac Surg. 2011;15:251–252. doi: 10.1007/s10006-010-0245-6. [DOI] [PubMed] [Google Scholar]
- 54.Benech A, Arcuri F, Poglio G, et al. Vacuum-assisted closure therapy in reconstructive surgery. Acta Otorhinolaryngol Ital. 2012;32:192–197. [PMC free article] [PubMed] [Google Scholar]
- 55.Ariyan S. Further experiences with the pectoralis major myocutaneous flap for the immediate repair of defects from excisions of head and neck cancers. Plast Reconstr Surg. 1979;64:605–612. [PubMed] [Google Scholar]
- 56.Arlyan S, Cuono CB. Use of the pectoralis major myocutaneous flap for reconstruction of large cervical, facial or cranial defects. Am J Surg. 1980;140:503–506. doi: 10.1016/0002-9610(80)90200-7. [DOI] [PubMed] [Google Scholar]
- 57.Biller HF, Krespi YP, Lawson W, et al. A one-stage flap reconstruction following resection for stomal recurrence. Otolaryngol Head Neck Surg. 1980;88:357–360. doi: 10.1177/019459988008800407. [DOI] [PubMed] [Google Scholar]
- 58.Theogaraj SD, Merritt WH, Acharya G, et al. The pectoralis major musculocutaneous island flap in single-stage reconstruction of the pharyngoesophageal region. Plast Reconstr Surg. 1980;65:267–276. doi: 10.1097/00006534-198003000-00001. [DOI] [PubMed] [Google Scholar]
- 59.Evans PH, Das Gupta AR. The use of the pectoralis major myocutaneous flap for one-stage reconstruction of the base of the tongue. J Laryngol Otol. 1981;95:809–816. doi: 10.1017/s0022215100091453. [DOI] [PubMed] [Google Scholar]
- 60.Withers EH, Franklin JD, Madden JJ, Jr, et al. Pectoralis major musculocutaneous flap: a new flap in head and neck reconstruction. Am J Surg. 1979;138:537–543. doi: 10.1016/0002-9610(79)90415-x. [DOI] [PubMed] [Google Scholar]
- 61.Lee YT. Carotid artery protection by pectoralis major muscle flap. Am J Surg. 1980;140:464–464. doi: 10.1016/0002-9610(80)90191-9. [DOI] [PubMed] [Google Scholar]
- 62.Siu KF, Wei WI, Lam KH, et al. Use of the pectoralis major muscle flap for repair of a tracheoesophageal fistula. Am J Surg. 1985;150:617–619. doi: 10.1016/0002-9610(85)90449-0. [DOI] [PubMed] [Google Scholar]
- 63.Sisson GA, Goldman ME. Pectoral myocutaneous island flap for reconstruction of stomal recurrence. Arch Otolaryngol. 1981;107:446–449. doi: 10.1001/archotol.1981.00790430048013. [DOI] [PubMed] [Google Scholar]
- 64.Baker SR. Management of osteoradionecrosis of the mandible with myocutaneous flaps. J Surg Oncol. 1983;24:282–289. doi: 10.1002/jso.2930240409. [DOI] [PubMed] [Google Scholar]
- 65.Price JC, Davis RK, Koltai PJ. The pectoralis myocutaneous flap for salvage of necrotic wounds. Laryngoscope. 1985;95:146–150. doi: 10.1288/00005537-198502000-00004. [DOI] [PubMed] [Google Scholar]
- 66.Krespi YP, Sisson GA. Reconstruction after total or subtotal glossectomy. Am J Surg. 1983;146:488–492. doi: 10.1016/0002-9610(83)90237-4. [DOI] [PubMed] [Google Scholar]
- 67.Sasaki CT, Ariyan S, Spencer D, et al. Pectoralis major myocutaneous reconstruction of the anterior skull base. Laryngoscope. 1985;95:162–166. doi: 10.1288/00005537-198502000-00007. [DOI] [PubMed] [Google Scholar]
- 68.Deganello A, Gitti G, Struijs B, et al. Palliative combined treatment for unresectable cutaneous basosquamous cell carcinoma of the head and neck. Acta Otorhinolaryngol Ital. 2013;33:353–356. [PMC free article] [PubMed] [Google Scholar]
- 69.Morgan RF, Sargent LA, Hoopes JE. Midfacial and total nasal reconstruction with bilateral pectoralis major myocutaneous flaps. Plast Reconstr Surg. 1984;73:824–826. doi: 10.1097/00006534-198405000-00019. [DOI] [PubMed] [Google Scholar]
- 70.Milroy BC, Korula P. Vascularized innervated transfer of the clavicular head of the pectoralis major muscle in established facial paralysis. Ann Plast Surg. 1988;20:75–81. doi: 10.1097/00000637-198801000-00012. [DOI] [PubMed] [Google Scholar]
- 71.Joseph CA, Fayman MS, Kadwa MA, Gregor RT. The pectoralis major flap for reconstruction of septic wounds. S Afr J Surg. 1988;26:107–109. [PubMed] [Google Scholar]
- 72.Fleischer A, Khafif R. Reconstruction of the mediastinal trachea with a tubed pectoralis major myocutaneous flap. Plast Reconstr Surg. 1989;84:342–346. doi: 10.1097/00006534-198908000-00025. [DOI] [PubMed] [Google Scholar]
- 73.Schusterman MA, Kroll SS, Weber RS, et al. Intraoral soft tissue reconstruction after cancer ablation: a comparison of the pectoralis major flap and the free radial forearm flap. Am J Surg. 1991;162:397–399. doi: 10.1016/0002-9610(91)90157-9. [DOI] [PubMed] [Google Scholar]
- 74.Kroll SS, Reece GP, Miller MJ, et al. Comparison of the rectus abdominis free flap with the pectoralis major myocutaneous flap for reconstructions in the head and neck. Am J Surg. 1992;164:615–618. doi: 10.1016/s0002-9610(05)80719-6. [DOI] [PubMed] [Google Scholar]
- 75.Cordeiro PG, Hidalgo DA. Soft tissue coverage of mandibular reconstruction plates. Head Neck. 1994;16:112–115. doi: 10.1002/hed.2880160203. [DOI] [PubMed] [Google Scholar]
- 76.Wei FC, Demirkan F, Chen HC, et al. The outcome of failed free flaps in head and neck and extremity reconstruction: what is next in the reconstructive ladder? Plast Reconstr Surg. 2001;108:1154–1160. doi: 10.1097/00006534-200110000-00007. [DOI] [PubMed] [Google Scholar]
- 77.Bozikov K, Arnez ZM. Factors predicting free flap complications in head and neck reconstruction. J Plast Reconstr Aesthet Surg. 2006;59:737–742. doi: 10.1016/j.bjps.2005.11.013. [DOI] [PubMed] [Google Scholar]
- 78.Schneider DS, Wu V, Wax MK. Indications for pedicled pectoralis major flap in a free tissue transfer practice. Head Neck. 2012;34:1106–1110. doi: 10.1002/hed.21868. [DOI] [PubMed] [Google Scholar]
- 79.Colletti G, Autelitano L, Tewfik K, et al. Autonomized flaps in secondary head and neck reconstructions. Acta Otorhinolaryngol Ital. 2012;32:329–335. [PMC free article] [PubMed] [Google Scholar]
- 80.Spriano G, Piantanida R, Pellini R. Hypopharyngeal reconstruction using pectoralis major myocutaneous flap and prevertebral fascia. Laryngoscope. 2001;111:544–547. doi: 10.1097/00005537-200103000-00030. [DOI] [PubMed] [Google Scholar]
- 81.Saussez S, Cuno A, Urbain F, et al. Reconstruction of circumferential oro- and hypopharyngeal defects with U-shaped pectoralis major myocutaneous flap. Otolaryngol Head Neck Surg. 2006;134:823–829. doi: 10.1016/j.otohns.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 82.Liu HL, Chan JY, Wei WI. The changing role of pectoralis major flap in head and neck reconstruction. Eur Arch Otorhinolaryngol. 2010;267:1759–1763. doi: 10.1007/s00405-010-1271-6. [DOI] [PubMed] [Google Scholar]
- 83.Talesnik A, Markowitz B, Calcaterra T, et al. Cost and outcome of osteocutaneous free-tissue transfer versus pedicled soft-tissue reconstruction for composite mandibular defects. Plast Reconstr Surg. 1996;97:1167–1178. doi: 10.1097/00006534-199605000-00011. [DOI] [PubMed] [Google Scholar]
- 84.Giordano L, Bondi S, Ferrario F, et al. Radial forearm free flap surgery: a modified skin- closure technique improving donor-site aesthetic appearance. Acta Otorhinolaryngol Ital. 2012;32:158–163. [PMC free article] [PubMed] [Google Scholar]
- 85.Pellini R, Mercante G, Spriano G. Step-by-step mandibular reconstruction with free fibula flap modelling. Acta Otorhinolaryngol Ital. 2012;32:405–409. [PMC free article] [PubMed] [Google Scholar]
- 86.Tarsitano A, Vietti MV, Cipriani R, et al. Functional results of microvascular reconstruction after hemiglossectomy: free anterolateral thigh flap versus free forearm flap. Acta Otorhinolaryngol Ital. 2013;33:374–379. [PMC free article] [PubMed] [Google Scholar]
- 87.Baj A, Beltramini GA, Demarchi M, et al. Extended-pedicle peroneal artery perforator flap in intraoral reconstruction. Acta Otorhinolaryngol Ital. 2013;33:282–285. [PMC free article] [PubMed] [Google Scholar]
- 88.IJsselstein CB, Hovius SE, Have BL, et al. Is the pectoralis myocutaneous flap in intraoral and oropharyngeal reconstruction outdated? Am J Surg. 1996;172:259–262. doi: 10.1016/S0002-9610(96)00161-4. [DOI] [PubMed] [Google Scholar]
- 89.Croce A, Moretti A, D'Agostino L, et al. Continuing validity of pectoralis major muscle flap 25 years after its first application. Acta Otorhinolaryngol Ital. 2003;23:297–304. [PubMed] [Google Scholar]
- 90.Leemans CR, Balm AJ, Gregor RT, et al. Management of carotid artery exposure with pectoralis major myofascial flap transfer and split-thickness skin coverage. J Laryngol Otol. 1995;109:1176–1180. doi: 10.1017/s0022215100132360. [DOI] [PubMed] [Google Scholar]
- 91.Kekatpure VD, Trivedi NP, Manjula BV, et al. Pectoralis major flap for head and neck reconstruction in era of free flaps. Int J Oral Maxillofac Surg. 2012;41:453–457. doi: 10.1016/j.ijom.2011.12.029. [DOI] [PubMed] [Google Scholar]
- 92.Kiyokawa K, Tai Y, Inoue Y, et al. Reliable, minimally invasive oromandibular reconstruction using metal plate rolled with pectoralis major myocutaneous flap. J Craniofac Surg. 2001;12:326–336. doi: 10.1097/00001665-200107000-00005. [DOI] [PubMed] [Google Scholar]
- 93.Salvatori P, Motto E, Paradisi S, et al. Oromandibular reconstruction using titanium plate and pectoralis major myocutaneous flap. Acta Otorhinolaryngol Ital. 2007;27:227–232. [PMC free article] [PubMed] [Google Scholar]
- 94.Cordova A, Corradino B, Pirrello R, et al. Surgical treatment of pharyngostomes in irradiated patients. Our experience with musculocutaneous pectoralis major flap and hyperbaric oxygen therapy. Acta Otolaryngol. 2005;125:759–764. doi: 10.1080/00016480510027556. [DOI] [PubMed] [Google Scholar]
- 95.Gilbert MR, Sturm JJ, Gooding WE, et al. Pectoralis major myofascial onlay and myocutaneous flaps and pharyngocutaneous fistula in salvage laryngectomy. Laryngoscope. 2014;124:2680–2686. doi: 10.1002/lary.24796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bhola N, Jadhav A, Borle R, et al. Is there still a role for bilobed/bipaddled pectoralis major myocutaneous flap for single-stage immediate reconstruction of post ablative oncologic full-thickness defects of the cheek? Oral Maxillofac Surg. 2014 Aug 17; doi: 10.1007/s10006-014-0458-1. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 97.Gadre KS, Gadre P, Sane VD, et al. Pectoralis major myocutaneous flap--still a workhorse for maxillofacial reconstruction in developing countries. J Oral Maxillofac Surg. 2013;71:2005–2005. doi: 10.1016/j.joms.2013.07.016. [DOI] [PubMed] [Google Scholar]
- 98.Vartanian JG, Carvalho AL, Carvalho SM, et al. Pectoralis major and other myofascial/myocutaneous flaps in head and neck cancer reconstruction: experience with 437 cases at a single institution. Head Neck. 2004;26:1018–1023. doi: 10.1002/hed.20101. [DOI] [PubMed] [Google Scholar]
- 99.Mura F, Bertino G, Occhini A, et al. Advanced carcinoma of the hypopharynx: functional results after circumferential pharyngolaryngectomy with flap reconstruction. Acta Otorhinolaryngol Ital. 2012;32:154–157. [PMC free article] [PubMed] [Google Scholar]
- 100.Mura F, Bertino G, Occhini A, et al. Surgical treatment of hypopharyngeal cancer: a review of the literature and proposal for a decisional flow-chart. Acta Otorhinolaryngol Ital. 2013;33:299–306. [PMC free article] [PubMed] [Google Scholar]
- 101.Wada T, Nakatani K, Hiraishi Y, et al. Usefulness of myofascial flap without skin in contemporary oral and maxillofacial reconstruction. J Oral Maxillofac Surg. 2011;69:1815–1825. doi: 10.1016/j.joms.2010.07.069. [DOI] [PubMed] [Google Scholar]
- 102.Deleyiannis FW, Rogers C, Lee E, et al. Reconstruction of the lateral mandibulectomy defect: management based on prognosis and location and volume of soft tissue resection. Laryngoscope. 2006;116:2071–2080. doi: 10.1097/01.mlg.0000240858.88538.e1. [DOI] [PubMed] [Google Scholar]
- 103.Galli J, Valenza V, Parrilla C, et al. Pharyngocutaneous fistula onset after total laryngectomy: scintigraphic analysis. Acta Otorhinolaryngol Ital. 2009;29:242–244. [PMC free article] [PubMed] [Google Scholar]
- 104.Oosthuizen JC, Leonard DS, Kinsella JB. The role of pectoralis major myofascial flap in salvage laryngectomy: a single surgeon experience. Acta Otolaryngol. 2012;132:1002–1005. doi: 10.3109/00016489.2012.672768. [DOI] [PubMed] [Google Scholar]
- 105.Righini C, Lequeux T, Cuisnier O, et al. The pectoralis myofascial flap in pharyngolaryngeal surgery after radiotherapy. Eur Arch Otorhinolaryngol. 2005;262:357–361. doi: 10.1007/s00405-004-0827-8. [DOI] [PubMed] [Google Scholar]
- 106.McLean JN, Carlson GW, Losken A. The pectoralis major myocutaneous flap revisited: a reliable technique for head and neck reconstruction. Ann Plast Surg. 2010;64:570–573. doi: 10.1097/SAP.0b013e3181c51f4a. [DOI] [PubMed] [Google Scholar]
- 107.Blackwell KE, Buchbinder D, Biller HF, et al. Reconstruction of massive defects in the head and neck: the role of simultaneous distant and regional flaps. Head Neck. 1997;19:620–628. doi: 10.1002/(sici)1097-0347(199710)19:7<620::aid-hed10>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 108.Maisel RH, Liston SL, Adams GL. Complications of pectoralis myocutaneous flaps. Laryngoscope. 1983;93:928–930. doi: 10.1288/00005537-198307000-00015. [DOI] [PubMed] [Google Scholar]
- 109.Mehrhof AI, Jr., Rosenstock A, Neifeld JP, et al. The pectoralis major myocutaneous flap in head and neck reconstruction. Analysis of complications. Am J Surg. 1983;146:478–482. doi: 10.1016/0002-9610(83)90235-0. [DOI] [PubMed] [Google Scholar]
- 110.Ossoff RH, Wurster CF, Berktold RE, et al. Complications after pectoralis major myocutaneous flap reconstruction of head and neck defects. Arch Otolaryngol. 1983;109:812–814. doi: 10.1001/archotol.1983.00800260034008. [DOI] [PubMed] [Google Scholar]
- 111.Donegan JO, Gluckman JL. An unusual complication of the pectoralis major myocutaneous flap. Head Neck Surg. 1984;6:982–983. doi: 10.1002/hed.2890060514. [DOI] [PubMed] [Google Scholar]
- 112.Nagarjuna M, Patil BR, Nagraj N, et al. Use of superiorly based vertical rectus abdominis myocutaneous flap for the correction of costal osteomyelitis at the pectoralis major myocutaneous flap donor site. J Oral Maxillofac Surg. 2013;71:e132–e136. doi: 10.1016/j.joms.2012.10.011. [DOI] [PubMed] [Google Scholar]
- 113.Liu R, Gullane P, Brown D, et al. Pectoralis major myocutaneous pedicled flap in head and neck reconstruction: retrospective review of indications and results in 244 consecutive cases at the Toronto General Hospital. J Otolaryngol. 2001;30:34–40. doi: 10.2310/7070.2001.21011. [DOI] [PubMed] [Google Scholar]
- 114.Rossen ME, Verduijn PV, Mureau MA. Survival of pedicled pectoralis major flap after secondary myectomy of muscle pedicle including transection of thoracoacromial vessels: does the flap remain dependent on its dominant pedicle? J Plast Reconstr Aesthet Surg. 2011;64:323–328. doi: 10.1016/j.bjps.2010.05.026. [DOI] [PubMed] [Google Scholar]
- 115.Kroll SS, Goepfert H, Jones M, et al. Analysis of complications in 168 pectoralis major myocutaneous flaps used for head and neck reconstruction. Ann Plast Surg. 1990;25:93–97. doi: 10.1097/00000637-199008000-00003. [DOI] [PubMed] [Google Scholar]
- 116.Shah JP, Haribhakti V, Loree TR, et al. Complications of the pectoralis major myocutaneous flap in head and neck reconstruction. Am J Surg. 1990;160:352–355. doi: 10.1016/s0002-9610(05)80541-0. [DOI] [PubMed] [Google Scholar]
- 117.Mehta S, Sarkar S, Kavarana N, et al. Complications of the pectoralis major myocutaneous flap in the oral cavity: a prospective evaluation of 220 cases. Plast Reconstr Surg. 1996;98:31–37. doi: 10.1097/00006534-199607000-00006. [DOI] [PubMed] [Google Scholar]
- 118.Castelli ML, Pecorari G, Succo G, et al. Pectoralis major myocutaneous flap: analysis of complications in difficult patients. Eur Arch Otorhinolaryngol. 2001;258:542–545. doi: 10.1007/s004050100389. [DOI] [PubMed] [Google Scholar]
- 119.You YS, Chung CH, Chang YJ, et al. Analysis of 120 pectoralis major flaps for head and neck reconstruction. Arch Plast Surg. 2012;39:522–527. doi: 10.5999/aps.2012.39.5.522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Keidan RD, Kusiak JF. Complications following reconstruction with the pectoralis major myocutaneous flap: the effect of prior radiation therapy. Laryngoscope. 1992;102:521–524. doi: 10.1288/00005537-199205000-00009. [DOI] [PubMed] [Google Scholar]
- 121.Avery CM, Gandhi N, Peel D, et al. Indications and outcomes for 100 patients managed with a pectoralis major flap within a UK maxillofacial unit. Int J Oral Maxillofac Surg. 2014;43:546–554. doi: 10.1016/j.ijom.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 122.Jena A, Patnayak R, Sharan R, et al. Outcomes of pectoralis major myocutaneous flap in female patients for oral cavity defect reconstruction. J Oral Maxillofac Surg. 2014;72:222–231. doi: 10.1016/j.joms.2013.06.205. [DOI] [PubMed] [Google Scholar]
- 123.Bansal R, Patel TS, Bhullar C, et al. Metastases to the donor site of the pectoralis major myocutaneous flap following reconstructive surgery: a rare complication. Plast Reconstr Surg. 2004;114:1965–1966. doi: 10.1097/01.prs.0000143923.36209.08. [DOI] [PubMed] [Google Scholar]
- 124.Seidenberg B, Rosenak SS, Hurwitt ES, et al. Immediate reconstruction of the cervical esophagus by a revascularized isolated jejunal segment. Ann Surg. 1959;149:162–171. doi: 10.1097/00000658-195902000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Hsing CY, Wong YK, Wang CP, et al. Comparison between free flap and pectoralis major pedicled flap for reconstruction in oral cavity cancer patients - a quality of life analysis. Oral Oncol. 2011;47:522–527. doi: 10.1016/j.oraloncology.2011.03.024. [DOI] [PubMed] [Google Scholar]
- 126.Xiao Y, Zhu J, Cai X, et al. Comparison between anterolateral thigh perforator free flaps and pectoralis major pedicled flap for reconstruction in oral cancer patients- -a quality of life analysis. Med Oral Patol Oral Cir Bucal. 2013;18:e856–e861. doi: 10.4317/medoral.19276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Zhang X, Li MJ, Fang QG, et al. A comparison between the pectoralis major myocutaneous flap and the free anterolateral thigh perforator flap for reconstruction in head and neck cancer patients: assessment of the quality of life. J Craniofac Surg. 2014;25:868–871. doi: 10.1097/SCS.0000000000000443. [DOI] [PubMed] [Google Scholar]
- 128.O'Neill JP, Shine N, Eadie PA, et al. Free tissue transfer versus pedicled flap reconstruction of head and neck malignancy defects. Ir J Med Sci. 2010;179:337–343. doi: 10.1007/s11845-010-0468-4. [DOI] [PubMed] [Google Scholar]
- 129.Deganello A, Gitti G, Parrinello G, et al. Cost analysis in oral cavity and oropharyngeal reconstructions with microvascular and pedicled flaps. Acta Otorhinolaryngol Ital. 2013;33:380–387. [PMC free article] [PubMed] [Google Scholar]
- 130.Mallet Y, El BS, Penel N, et al. The free vascularized flap and the pectoralis major pedicled flap options: comparative results of reconstruction of the tongue. Oral Oncol. 2009;45:1028–1031. doi: 10.1016/j.oraloncology.2009.05.639. [DOI] [PubMed] [Google Scholar]
- 131.Smeele LE, Goldstein D, Tsai V, et al. Morbidity and cost differences between free flap reconstruction and pedicled flap reconstruction in oral and oropharyngeal cancer: Matched control study. J Otolaryngol. 2006;35:102–107. doi: 10.2310/7070.2005.5001. [DOI] [PubMed] [Google Scholar]
- 132.Bree R, Reith R, Quak JJ, et al. Free radial forearm flap versus pectoralis major myocutaneous flap reconstruction of oral and oropharyngeal defects: a cost analysis. Clin Otolaryngol. 2007;32:275–282. doi: 10.1111/j.1365-2273.2007.01466.x. [DOI] [PubMed] [Google Scholar]
- 133.Chepeha DB, Annich G, Pynnonen MA, et al. Pectoralis major myocutaneous flap vs revascularized free tissue transfer: complications, gastrostomy tube dependence, and hospitalization. Arch Otolaryngol Head Neck Surg. 2004;130:181–186. doi: 10.1001/archotol.130.2.181. [DOI] [PubMed] [Google Scholar]
- 134.Tsue TT, Desyatnikova SS, Deleyiannis FW, et al. Comparison of cost and function in reconstruction of the posterior oral cavity and oropharynx. Free vs pedicled soft tissue transfer. Arch Otolaryngol Head Neck Surg. 1997;123:731–737. doi: 10.1001/archotol.1997.01900070075012. [DOI] [PubMed] [Google Scholar]
- 135.Petruzzelli GJ, Brockenbrough JM, Vandevender D, et al. The influence of reconstructive modality on cost of care in head and neck oncologic surgery. Arch Otolaryngol Head Neck Surg. 2002;128:1377–1380. doi: 10.1001/archotol.128.12.1377. [DOI] [PubMed] [Google Scholar]
- 136.McCrory AL, Magnuson JS. Free tissue transfer versus pedicled flap in head and neck reconstruction. Laryngoscope. 2002;112:2161–2165. doi: 10.1097/00005537-200212000-00006. [DOI] [PubMed] [Google Scholar]
- 137.Rosenthal E, Carroll W, Dobbs M, et al. Simplifying head and neck microvascular reconstruction. Head Neck. 2004;26:930–936. doi: 10.1002/hed.20076. [DOI] [PubMed] [Google Scholar]
- 138.Metgudmath RB, Metgudmath AR, Metgudmath VV, et al. Versatility of pectoralis major myocutaneous flap in oncosurgery and its role in developing countries. Indian J Otolaryngol Head Neck Surg. 2013;65:80–84. doi: 10.1007/s12070-012-0535-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Funk GF, Karnell LH, Whitehead S, et al. Free tissue transfer versus pedicled flap cost in head and neck cancer. Otolaryngol Head Neck Surg. 2002;127:205–212. doi: 10.1067/mhn.2002.127591. [DOI] [PubMed] [Google Scholar]
- 140.Putten L, Spasiano R, BR, et al. Flap reconstruction of the hypopharynx: a defect orientated approach. Acta Otorhinolaryngol Ital. 2012;32:288–296. [PMC free article] [PubMed] [Google Scholar]